All published articles of this journal are available on ScienceDirect.
Spatial Heterogeneity in Determinants of No Condom Use at First Sex in South Africa
Abstract
Background
Condom use, especially at first sex for unmarried people, is an important behaviour that reduces the risk of HIV transmission, and other Sexually Transmitted Diseases (STDs), as well as unwanted pregnancies. In reviewing the literature, little information was found to elucidate the spatial context of condom use among people who had an early sexual debut. Understanding factors that influence no condom use at first sex in different local or geographical areas can add value in addressing these risky first-sex practices and minimise the risk of getting HIV, STDs, and unwanted pregnancies in South Africa, especially among young people. Therefore, this paper aimed to determine the spatial heterogeneity of factors associated with no condom use at first sex in South Africa using Geographically Weighted Regression (GWR) with Poisson distribution and local bivariate relationships.
Methods
This article used data from the fifth South African National HIV Prevalence, HIV Incidence, Behaviour and Communication Survey (SABSSM V) of 2017. Spatial autocorrelation, GWR using Poisson distribution, and local bivariate relationships were undertaken using ArcGIS Pro.
Results
Geographically weighted regression using Poisson distribution results highlighted being female, being young, having never married, being unemployed, having sexual debut at a younger age, having two or more sexual partners, having no risk of being infected with HIV, and having good Self-perceived Health (SPH) to be significant factors influencing no condom use at first sex, with pseudo R2 = 0.96 and AICc = 692. Local bivariate relationships showed the relationship between no condom use at first sex and most explanatory variables to exhibit a positive linear relationship in most districts with the exception of having never married, which showed a positive linear relationship in only 18 districts, while 33 districts showed a concave relationship. These relationships were all significant with p < 0.05.
Conclusion
This localised analytical approach may contribute to the development of geo-targeted interventions and policies tailored to specific regions within South Africa, thereby improving the effectiveness of efforts to promote safe first sexual practices. Educational programs targeting youth should be developed to further raise awareness of the risks associated with unprotected sex and the importance of condom use. More efforts should be made to break the barriers, such as sexual relationship power, gender, and sociocultural and religious influences, which tend to put young, never-married, and unemployed women at risk of no condom use at first sexual debut. It is further recommended that the type of relationship between no condom use at first sex and each explanatory factor at the local region be considered during geo-targeted interventions as this will assist in the type of intervention and duration of intervention.
1. BACKGROUND/INTRODUCTION
Condoms are considered safe for sex partners who tend to pose a higher risk of contracting Human Immunodeficiency Virus (HIV), notably extramarital partners. Just 30% of women and 47% of men reported using condoms with their most recent non-spouse/non-regular partner in Malawi [1]. Ntshiqa et al. [2] linked various aspects to condom use, including higher levels of education, the conviction that condoms do not diminish sexual pleasure, the conviction that condoms are safe, and having several sexual partners. On the contrary, condom use has also been associated with several connotations, such as lack of willingness to use condoms, access to condoms, gender inequality, social norms that forbid condom usage, and transactional sexual encounters [3]. The significance of using condoms at sexual debut is highlighted by national public campaigns that promote condom usage and the availability of free condoms in both public and private places [4]. The use of condoms is still one of the best behavioural strategies for preventing HIV, STDs, and unintended pregnancies [5-10]. Recently, there has been speculation in South Africa that the lack of condoms in the Gauteng province may have contributed to the rise in STDs. For example, cases of male urethritis syndrome were reported to have increased from 5,486 in February 2022 to 6,035 in February 2023 [11]. In addition, Bolarinwa [12] reported that during the COVID-19 pandemic in South Africa, there was limited access to condoms and that the preferred source of condoms was skewed towards public sources.
Although condom usage may be considered appropriate and even necessary at the beginning of a sexual relationship, Beksinska et al. [13] reported a decline in its usage over time in most relationships due to the build-up of trust. Overall the UNAIDS expressed concerns regarding the low rates of condom use in African nations, especially among young people who are particularly susceptible to the acquisition of HIV [14, 15]. In South Africa, consistent condom usage has been reported as difficult to achieve since definitions of what consistent condom use actually entails vary widely [13]. Before the spread of HIV/AIDS, the use of condoms in Sub-Saharan Africa (SSA) was reported to be low; only sex workers and casual, unreliable partners were allowed to use them [16]. Notably, in European nations, HIV prevalence has been reported to be less than 0.2% among the 15–49 age group in contrast to SSA countries, i.e., Swaziland, South Africa, Lesotho, and Botswana, with estimations of around 15% [10]. Malema et al. [16], in the results of a study conducted at the University of Ibadan in Nigeria with 422 students, whose average age was 17.6 years, found condom use to be low among the 64 sexually active students, with 33% of men and 11% of women saying that they had never used condoms. Izudi et al. [17] reported that among university students in SSA, there was low condom use at the last sexual intercourse. They further indicated that out of 14778 sexually active students, 8744 had used a condom at the last sexual intercourse. They also reported that the pooled proportion of condom use at the last sexual intercourse was 52.9%. In Tanzania, Katikiro and Njau [18] found that 87.8% out of 260 sexually active out-of-school youth who participated in the study in Dar es Salaam reported no condom use in the past 3 months prior to the study.
The data from the 2017 SABSSM report indicated a relatively high proportion of adolescents to start their sexual lives early, have several partners, and use condoms inconsistently [2, 7, 19]. The most effective way to prevent HIV infection in adolescents having their first sexual experience has been reported to be condom use, which may help to lower HIV infection rates in South Africa and other nations [4]. In addition, Kincaid et al. [20] found condom use at sexual debut to be associated with lower subsequent HIV risk. Data among South African teenagers and young women showed condom use to be underutilized in this important cohort [2]. Due to first-sex practices that are risky and unprotected, South Africa was reported to have one of the highest rates of HIV prevalence among adolescents in the world, at 11.2% in 2015 [4]. The majority of South African youth have indicated to be aware that condoms are effective at preventing STIs, HIV, and unwanted pregnancies, and that condoms are widely available and free of charge in South Africa [21]. However, both men and women in South Africa have reported using fewer condoms in their most recent relationships, with women reporting fewer casual partners than men [16]. Findings from the South African Demographic and Health Survey indicated 50% of young females and 66% of young males to have sex before the age of 18, and 4.6% of young females and 20.7% of young males to have more than two sexual partners in the year prior to the survey [9].
Factors associated with no condom use or condom use are of importance in order to address this HIV behavioural risk. The available studies have explored these factors at a global level rather than at the local level. For instance, Calazans et al. [22] assessed factors related to the lack of condom use by young people at last sexual intercourse with a steady or casual partner in Brazil. They found being female, having low education attainment, having no work history, and having per capita family income above the minimum wage to be associated with not using condoms in the group of young people who had their last sexual encounter with steady partners. In contrast, they found first sex at 9–16 years of age, a positive history of alcohol use, and inadequate knowledge of AIDS treatability as well as bereavement related to violence to be significant factors among those with casual partners. In South Africa, Phora [4] determined factors associated with condom use at first sex among adolescents in 2012. A number of variables, including sociodemographic factors, beliefs or attitudes concerning HIV/AIDS, behavioural characteristics, and exposure to media content, have been found to be predictive of first-time condom usage among adolescents [4]. Phora [4] further reported that geographical location (either urban or rural residence) can be a significant predictor of condom use with urban residents being twice as likely to use condoms compared to rural residents.
Due to the significance of condom use in preventing HIV, STDs, and unintended pregnancies, this phenomenon needs to be explored at the local level using geostatistical modelling. Although some studies have explored no condom use or condom use, no studies have explicitly explored this geographically. Geographically Weighted Regression (GWR) was considered to explore this research gap. Brunsdon et al. [23] pioneered GWR, which allowed coefficient values to vary at various spatial sites. Local spatial regression uses GWR to provide parameters that are disaggregated by the geographic units of study. The GWR model permits coefficient values to vary at various spatial locations and has the ability to display a local relationship between the dependent variable and the independent variable, indicating that it is capable of identifying spatial data instability [24]. Geographically weighted regression models have been utilised to study phenomena related to no condom use, such as the use of modern contraception, HIV prevalence, HIV incidence, and their covariates. For instance, using GWR, Khan and Harris [25] examined regional differences in Bangladesh's use of modern contraception. The absence of modern contraceptive use at the cluster level was evaluated using a geographically weighted regression model. With a large geographic variance, 42.8% of respondents in Bangladesh reported not using modern contraception. Geographical differences existed in the prevalence of risk factors for not using modern contraception in Bangladesh.
Gelibo et al. [26] analysed subpopulation-level hotspot locations and spatial clustering of HIV infections in order to inform targeted treatments with the limited resources available in Ethiopia. The GWR analysis and the Pearson correlation coefficient were both employed to examine the relationships between variables and HIV prevalence. The analysis used socioeconomic, demographic, as well as biological characteristics, and one of the independent variables used was no condom use. The results showed that divorced or widowed people in hotspot towns and uncircumcised men in some hotspot towns may have contributed to the average rise in HIV prevalence in the hotspot locations [26].
Feldacker et al. [1] used GWR to investigate the spatial relationships between neighbourhood-level variables, individual risk behaviours, and HIV status in rural Malawi. One of the individual-level variables was the use of condoms. In South Africa, Wabiri et al. [27] used a GWR model to map the spatial relationships between social variables and HIV infection in people over the age of 15. Survey-weighted proportions of non-regular condom users made up the study's metrics. The weighted HIV prevalence in each district formed the dependent variable. A set of demographic and socio-economic variables in the 2007 Community Survey and the 2005 and 2006 General Household Surveys were obtained and used [27]. Covariates of interest that were selected included race, sex, intergenerational sex, socioeconomic quantiles, and locality in characterizing the observed patterns of HIV hotspots in the districts. The results showed the population in high prevalence areas to be relatively homogeneous and characterized by the following traits: Black origin, an unfavourable sex ratio (high proportion of females), low socioeconomic status, being single or low marriage rates, having several sexual partners and intergenerational sex [27]. The maps showed spatial non-stationarity in the relationship between local occurrences of HIV prevalence and the social covariates across South Africa [27].
The findings obtained from these various studies shed light on the complex dynamics influencing condom use behaviour among diverse populations. These findings collectively highlight the multifaceted nature of condom use behaviour and the intersecting influences of trust, socioeconomic factors, geography, and demographic characteristics. Understanding these complexities is essential for designing effective public health interventions aimed at promoting safer sexual practices and reducing the transmission of sexually transmitted infections in South Africa and similar contexts.
This study's academic value stems from its addition to the expanding corpus of research on sexual health behaviour and epidemiology. Prior research [28-30] has brought attention to the fact that condom use is influenced by a variety of factors, including individual, cultural, and socioeconomic determinants. Still, there is a lack of knowledge regarding the spatial variations of these elements in South Africa. Additionally, by utilizing GWR, this work contributes to the advancement of methodological techniques in public health research by providing an understanding of spatial variations in the determinants of no condom use at first sex.
The practical implications of the study's findings extend to healthcare professionals, policymakers, and community organizations that promote sexual health at the local level. The specific factors linked to not using a condom during one's first sexual encounter can be identified so that interventions can be customized to meet the particular requirements of various South African demographics and geographical regions. Such targeted interventions have the potential to mitigate the spread of HIV/AIDS and other STIs, thereby contributing to improved public health outcomes.
The use of GWR and the investigation of the no condom use as a variable have been important contributions provided by previous studies [1, 26]. However, these studies are not without limitations. For example, Gelibo et al. [26] might have missed significant distinctions in rural or semi-urban settings because their study was limited to urban areas. This constraint highlights the necessity for research that includes both urban and rural communities and captures the range of socioeconomic and cultural situations within South Africa. Additionally, Feldecker et al. [1] highlighted the challenge of sparse geographic information in developing countries, leading to potential errors in location allocation. This limitation is relevant in the context of South Africa, where disparities in data availability and quality may affect the accuracy of spatial analysis.
Despite these drawbacks, earlier research has paved the way for our understanding of the factors that contribute to condom non-use. Nonetheless, there remains a clear research gap in understanding the spatial variations in these determinants across diverse geographic regions within South Africa. This study aimed to close this gap by addressing these limitations and expanding on earlier research by utilizing rigorous methodological techniques, like GWR, to account for potential errors in geographic information and more accurately capture spatial variations in determinants. This study also aimed to address this gap by investigating the following research questions: what are the determinants of no condom use at first sex in South Africa, and how do they vary spatially across different geographic regions within the country?
Therefore, this study sought to determine the spatial heterogeneity of the factors influencing no condom use at first sex in South Africa using GWR and local bivariate relationships. By incorporating the spatial dimension, the local or geographical areas where no condom use is particularly high can be identified and the local factors associated with this behaviour can be explored explicitly. This localised approach can contribute to the development of geo-targeted interventions and policies tailored to specific regions within South Africa, thereby improving the effectiveness of efforts to promote safe sexual practices.
2. METHODS
2.1. Data
This paper used district-level data from the SABSSM V of 2017, conducted by the Human Sciences Research Council [7, 31]. Briefly, a multi-stage stratified random cluster sampling approach was employed to select 15 Visiting Points (VPs) or households from 1457 Small Area Layers (SALs), which were sampled from national 84 907 SALs. The sample included 13 high-priority districts due to their HIV prevalence. The strata were nine provinces and three geotypes or localities [7]. This secondary analysis focused on eligible people who completed the ≥15 years questionnaire and reported no condom use (either male or female condom) at sexual debut among sexually active people. The 2017 SABSSM V survey was the fifth wave, and therefore, previous survey series used validated questionnaires.
2.2. Measures
The primary outcome variable, no condom use at first sex, was based on the question “Did you use a condom the first time you had sex?” with response options being 1 = yes, 2 = no and 3 = cannot remember. The second option (2 = no) was considered for the final spatial modelling.
Explanatory variables included in this study were sex (female), young age (15-34 years old), marital status (never married), employment (unemployed), younger age at sex debut (19 years old or younger), sexual partners (two or more partners), HIV risk (no risk of being infected with HIV), and self-perceived health status (good health). The selection of these explanatory variables was based on a review of findings of previous studies [4, 7, 22, 27, 32]. In addition, some behavioural explanatory variables, such as sexual debut, multiple sexual partners, and HIV risk perception, have been found to be key drivers of the HIV epidemic in South Africa [7]. Table 1 highlights the summary statistics of the outcome variable and independent variables cumulatively within 52 districts.
2.3. Spatial Analysis
Global Moran’s Index spatial autocorrelation was performed to determine whether the spatial distribution of no condom use at first sex at the district level was dispersed, clustered, or random [33]. Moran’s I values range between -1 and +1, with positive values indicating spatial clustering of similar values (+1), 0 indicating no spatial autocorrelation, and negative values (-1) indicating perfect spatial dispersion or clustering of dissimilar values. The Moran’s I formula is given below:
 |
(1) |
Where, N is the number of observations, So is the sum of all elements in the spatial weights matrix, y^' yI are the observations from the mean, W refers to the spatial weights, and Wy is the associated spatial lag [33].
| Variables | Number of Districts | Min | Max | Mean | SD | Sum |
|---|---|---|---|---|---|---|
| No condom use at first sex | 52 | 40 | 1369 | 377 | 368 | 19609 |
| Female | 52 | 66 | 2432 | 696 | 670 | 36181 |
| Youth | 52 | 33 | 1554 | 422 | 418 | 21931 |
| Never married | 52 | 42 | 2062 | 483 | 521 | 25130 |
| Unemployed | 52 | 43 | 1493 | 400 | 404 | 20800 |
| Younger sexual debut | 52 | 41 | 1322 | 409 | 375 | 21268 |
| Having two or more partners | 52 | 33 | 1269 | 381 | 347 | 19820 |
| No HIV risk | 52 | 27 | 1513 | 367 | 346 | 19099 |
| Good SPH | 52 | 73 | 2241 | 591 | 584 | 30746 |
2.3.1. GWR
Geographically weighted regression that allows coefficient values to vary at different spatial areas or regions was considered to explore the relationship between no condom use at first sex and the selected explanatory variables [23, 24, 27, 34-36]. Global models are not able to capture differences at the local level, hence only GWR was considered in this study. Using a dataset similar to the one utilised in this study, Fundisi et al. [36] further proved a GWR local model to outperform the global model. The Poisson distribution method is usually applied for count data, and this was the case for this study as well. Geographically weighted regression with Poisson distribution, also known as Geographically Weighted Poisson Regression (GWPR), allows for each parameter to vary across different local areas or regions, hence being able to spatially recognise level variations in the relationship between the outcome variable and explanatory variables [36-40]. The GWPR model is built on Generalised Linear Models (GLM), such as Generalized Linear Regression (GLR), which are spatially rigid and assume fixed effects for various locations in space [36, 37]. The GWR brings into play the spatial component, for instance, how areas are related to their neighbouring areas. Further details on how the GWPR model integrates GLM and GWR are highlighted in the study by Fundisi et al. [36]. For model type, the count (Poisson) type was selected as the outcome variable for this study was discrete and represented the number of occurrences or counts of no condom use at first sex. All other parameters were left at default.
The GWPR formula is given below:
 |
(2) |
Where, Yi is the observed count data at district locations i; E(Yi) is no condom use at first sex at district locations i; β0(s), β1(s), β2(s), ..., βk(s) are the spatially varying coefficients, which may vary across different districts; x1i, x2i, ..., xki are the predictor variables at district locations i; and ln() is the natural logarithm.
2.3.2. Local Bivariate Relationships
Local spatial analysis is necessary to understand the exact nature of the relationship between the outcome variable and explanatory variables and how they change over different spatial areas or points. Existing local spatial analysis techniques assume a linear relationship for all spatial areas and focus only on the change in parameter values [41]. Local bivariate relationship is a technique that employs local entropy map, and is the solution to this challenge. This is a nonparametric method that does not assume a prior relationship form and it is able to detect the existence of different relationships regardless of their forms [41, 42]. Gou [41] found that the local entropy map was at least as powerful as the GWR in finding multivariate linear relationships, while it could also detect other types of relationships at the same time. A local entropy map usually calculates an approximation of the Rényi entropy for the multivariate data in each local area [41-43]. Each local entropy value gets converted to a p-value by matching to a distribution of permutation entropy values for the same area, and all p-values are processed by various statistical measures to control the multiple-testing problem [41]. The higher the local entropy mean value, the less predictable the variable is [42]. All spatial analysis, modelling, and maps were undertaken using ArcGIS Pro 3.0 (ESRI, Redlands, CA).
The local entropy map formula is given below:
 |
(3) |
Where, λ=(d-α)/d, 0<α<d, and c is a constant that depends only on α and d. Mα(x1, x2, ... ,xn) is the shortest-spanning tree in possible spanning trees.
3. RESULTS
3.1. Spatial Autocorrelation
Spatial autocorrelation was tested using the Global Moran’s I index and the results showed Moran’s I = 0.281, Z-score = 3.418, and p-value = 0.000631. This indicated no condom use at first sex to have spatial clustering of similar values. Fig. (1) depicts the spatial distribution of people who reported no condom use at first sex across the country. The neighbouring districts of eThekwini, iLembe, King Cetshwayo, Umzinyathi, and Uthukela fell under the highest category of 1012-1369 number of people aged ≥15 years who did not use a condom at sexual debut. Adjacent districts of Ekurhuleni, Sedibeng, Gert Sibande, and Ehlanzeni, with the exception of the isolated City of Cape Town, fell under the second category of 599-1011 people who reported no condom use at first sex or sexual debut.
3.2. GWR
Geographically weighted regression using Poisson distribution results highlighted being female, being young, having never married, being unemployed, having sexual debut at a younger age, having two or more sexual partners, having no risk of being infected with HIV, and having good Self-perceived Health (SPH) to be significant factors influencing no condom use at first sex among respondents across the country, with pseudo R2 = 0.96 and AICc = 692.
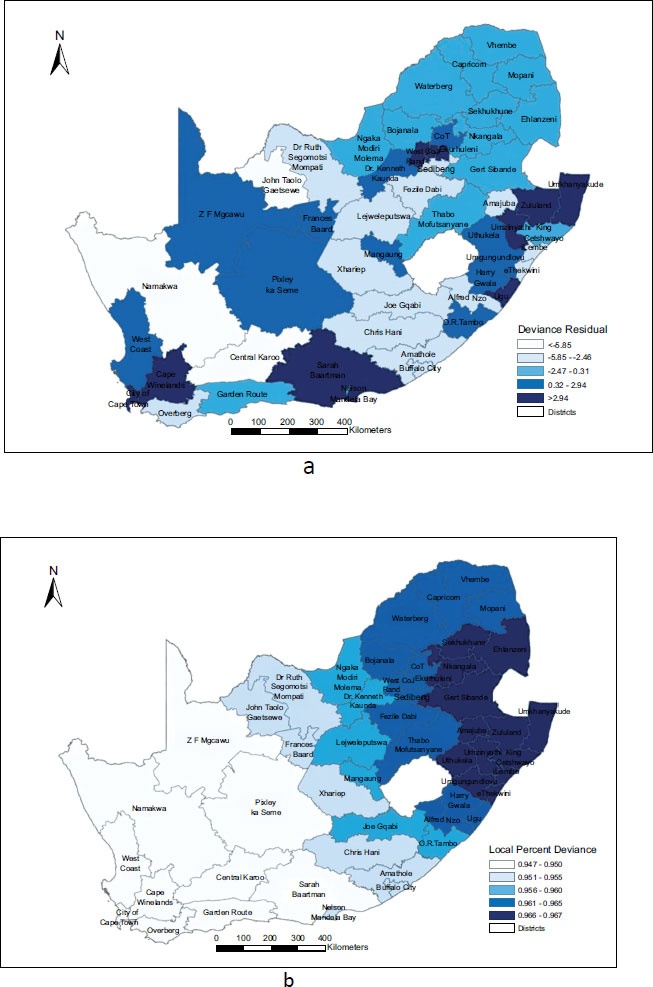
Fig. (2a) highlights the spatial distribution of deviance residuals across the country. The results showed that deviance residuals were randomly spread across the country. The deviance residual of <-5.85 was observed in Central Karoo, Namakwa, and John Taolo Gaetsewe districts. City of Johannesburg, West Rand, Ugu, Umkhanyakude, Umzinyathi, Zululand, Sarah Baartman, Nelson Mandela Bay, City of Cape Town, and Cape Winelands recorded the highest deviance residual category of >2.94.

| Variable | Positive Linear | Concave | Convex | Total | Entropy | p-value |
|---|---|---|---|---|---|---|
| Female | 43 | 0 | 9 | 52 | 1.126 | 0.005 |
| Youth | 41 | 2 | 9 | 52 | 1.163 | 0.005 |
| Never married | 18 | 33 | 1 | 52 | 1.193 | 0.005 |
| Unemployed | 52 | 0 | 0 | 52 | 1.176 | 0.005 |
| Younger sexual debut | 46 | 0 | 6 | 52 | 1.205 | 0.005 |
| Having two or more partners | 47 | 0 | 5 | 52 | 1.267 | 0.005 |
| No HIV risk | 29 | 10 | 13 | 52 | 1.173 | 0.005 |
| Good SPH | 47 | 3 | 2 | 52 | 1.184 | 0.005 |
Fig. (2b) shows the spatial distribution of the local percent deviance across the country. Local percent deviance is regarded as a measure of goodness of fit of the GWR model at the local level, with values ranging from 0.0 to 1.0, whereby higher values are more preferred. The results showed that local percent deviance values ranged from 0.947 to 0.967, which indicated the strength of the GWR model in predicting no condom use at first sex at the local level in South Africa. The model was better fitted in districts located in the eastern part of the country with a local percent deviance range of 0.961 to 0.967 and less fitted in the western part of the country as most of the districts had local percent deviance ranging from 0.947 to 0.950.
3.3. Local Bivariate Relationships
Table 2 highlights the local bivariate relationships between no condom use at first sex and explanatory variables. The relationship between no condom use at first sex and most explanatory variables exhibited a positive linear relationship in most districts with the exception of having never married, which showed a positive linear relationship in only 18 districts, while 33 districts showed a concave relationship. Having no risk of being infected with HIV had the second least number of districts showing a positive linear relationship with the no condom use at first sex in 29 districts, followed by 13 districts with a convex relationship, and lastly 10 districts with a concave relationship. With regards to local entropy, having two or more partners and a younger sexual debut had the highest values of 1.267 and 1.205, respectively. This indicates that these two explanatory variables had the least effect on the lack of condom use. The explanatory variable that had the highest effect on no condom use at first sex across 52 districts was being female with an entropy value of 1.126.
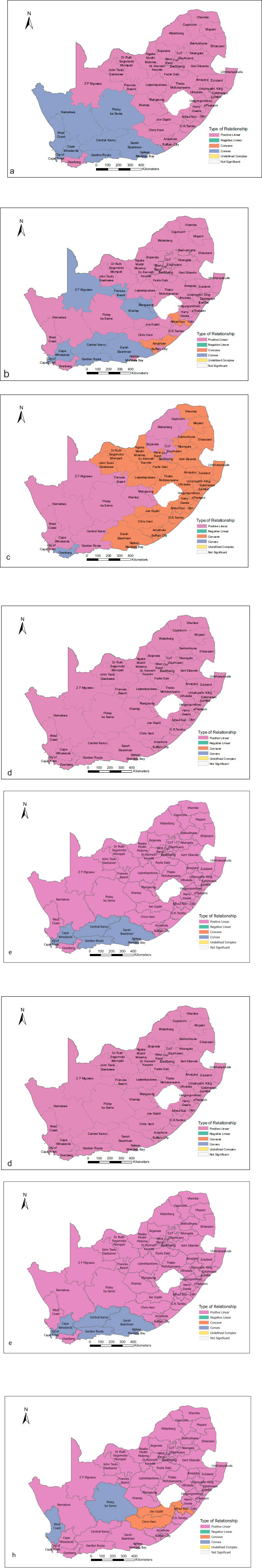
Fig. (3a-f) shows the type of relationship between no condom use at first sex and the explanatory variables across 52 districts. Fig. (3a) shows a positive linear relationship between no condom use at first sex and being female in most districts of the country and a convex relationship in some districts located in the south-western part of the country, with the exception of the Overberg district, which exhibited a positive linear relationship. Fig. (3c) shows a concave relationship between no condom use at first sex and having never married in most districts, especially in the eastern region of the country. There was some evidence of a positive linear relationship in the northern part of the country and a dominant positive linear relationship in the southwestern part of the country, with the exception of the Overberg district having a convex relationship. Fig. (3g) shows a concave relationship between no condom use at first sex and no risk of being infected with HIV in districts located in the northeastern part of the country and a convex relationship in districts located in the central northern part of the country. In general, the types of relationship between no condom use at first sex and the explanatory variables suggest clustering around neighbouring districts with some few cases whereby a district with a different relationship can be found among neighbouring districts with the same relationship type.
4. DISCUSSION
Geographically weighted regression using Poisson distribution results indicated a significant gender disparity in lack of condom use at sexual debut. Females were most vulnerable to lack of condom use at first sex or sexual debut within most districts in South Africa. This supports the findings of the study by Wabiri et al. [27], which reported females to have a high HIV prevalence within South Africa’s districts. Furthermore, Calazans et al. [22] also found being female to be one of the factors associated with the lack of condom use among young people who had their last sexual encounter with steady partners in Brazil. A review of male condom use among women in South Africa found that male dominance in sexual relationships restricted women’s ability to negotiate condom use [44]. Several social and cultural determinants have been associated with the high HIV prevalence among females, particularly among Adolescent Girls and Young Women (AGYW). Prior studies have noted that more AGYW engage in early sexual debut over time, and this occurs in the context of risky HIV-related behaviours, such as condomless sex at early sexual debut. Analyses of the same 2017 SABSSM dataset for AGYW aged 15–19 years found that sexual debut at ages younger than 15 years increased over time, from 12.7% in 2005 to 14.4% in 2017 [45]. Another study on AGYW aged 10 to 24 years conducted during 2016–2019 in ten South African districts found that those who had engaged in early sexual debut were highly likely to have been coerced at first sex, and had condomless first sex, compared to those who had a sexual debut at an older age [46]. A 2003 household-based survey conducted in South Africa among young people aged 15–24 years found that around half or fewer males and AGYW used a condom at sexual debut [47].
A study conducted in the United States during 1994–2002 among school-going adolescents found the average age of sexual debut to be 15.2 years and that those who used condoms at their sexual debut were more likely to engage in subsequent protective behaviours, such as using condoms [48]. Analyses of data from the 2005 SABSSM survey reported that people who used condoms at sexual debut were more likely to have remained HIV-negative [20]. A comparison of condom use at sexual debut from three surveys data conducted in 2005, 2009, and 2012 showed the uptake of condom use at sexual debut to be increased over time, suggesting a “generational effect” of condom use at sexual debut [20]. By 2005, condom use at sexual debut was estimated at 6%, whilst it remained stable at 5% in 1995, and its uptake increased by 2012 to 55% [20]. This has been attributed to HIV awareness communication programs.
In the current study, being young influenced no condom use at first sex. Similarly, Katikiro and Njau [18] found that out of 260 sexually active out-of-school youth, the majority (87.8%) reported no condom use in the past 3 months prior to the study in Dar es Salaam, Tanzania. Secondary analyses of condom use at the last sex were lower among HIV-positive young women aged 15-19 years (48.2%) compared to HIV-negative young women (60.6%) [45]. Ntshiqa et al. [2] reported that condom use is underutilized among teenagers and young women in South Africa. Chimoyi et al. [49] found that sub-optimal condom use increases with age and after being married, before and after adjusting for spatial random effects. They also reported that there were clusters with sub-optimal condom use in Ekurhuleni, an urban and semi-urban district in the Gauteng province, South Africa [49]. The youth or young people have also been reported to be particularly susceptible to HIV, and the low rates of condom use or no condom use in this age cohort in Africa have been observed [14, 15].
Having never married was found to be one of the significant factors influencing no condom use at first sex among respondents in South Africa, with a positive linear relationship in 18 districts and a concave relationship in 33 districts. Studies on marital status and the risk of HIV acquisition in the general population of South Africa have highlighted complexities pertaining to demographic, behavioural, and cultural practices [50-52]. In some contexts, being married suggests couples have a stable sexual network, which may confer a protective effect against HIV acquisition [51, 52]. As alluded to by Farrington et al. [6], condom use at first sex, especially for people who have never married, remains one of the important resources to reduce the transmission of HIV and other STDs. Wabiri et al. [27] also found high HIV prevalence to be associated with being single or low marriage rates.
Despite having lower rates of consistent condom use than any other relationship group, across all ages, married people had the lowest HIV incidence at 0.61% [7]. However, marriage rates were reported to be declining in South Africa with about 28,3% of married people aged 15+ years in 2016, and the existence of differential marriage rates by age, locality type (urban/non-urban), and population group [53]. Thus, more people in South Africa have been reported as opting to cohabit over time [53]. Cohabiting people in South Africa have been identified as one of the high-risk groups for HIV acquisition, and indeed, single people had the highest HIV incidence of 1.07% in 2017 [7] and contributed to high district-level HIV prevalence in 2008 [27].
Unemployed people were more likely to report no condom use at first sex in the current study. Low socioeconomic status tends to be associated with high HIV rates in South Africa [27], whereas Calazans et al. [22] found having no work history to be related to not using condoms among young people in Brazil. Having a sexual debut at a younger age exhibited a significant contribution to no condom use at first sex among different districts in South Africa. Calazans et al. [22] and Phora [4] also found first sex at 9–16 years of age and younger than 15 years old, respectively, as one of the factors related to not using condoms among young people.
Furthermore, the current study indicated that having two or more sexual partners also influenced no condom use at first sex among respondents at the district level. Wilson and Sathiyasusuman [54] also found a relationship between multiple sexual partners and condom use. However, other studies have found no significant relationship between multiple sexual partners and condom use [55, 56]. Gender dynamics have also been reported to be at play with respect to having multiple sexual partners. More males tended to engage in multiple sexual partnerships compared to females [7]. Notably, based on data from the 2005 SABSSM survey for youth aged 15-24 years, having multiple sexual partners has been noted more commonly among those who had early sexual debut compared to their counterparts who had sexual debut at older ages [57]. Although a declining trend over time in reported multiple sexual partnerships occurred among males aged 15–24 and 25–49 years, engaging in these types of relationships was still higher among males compared to females [7].
In the current study, people’s perception of no risk of being infected with HIV was also related to no condom use at first sex across different districts, which is contrary to Phora’s [4] findings. Furthermore, people who had good SPH also reportedly engaged in condomless sex at sexual debut. In reviewing the literature, to our knowledge, little is known about the impact of early sexual debut on well-being and self-reported health in South Africa. A study by Appollis et al. [46] found that young women aged 20–24 years who had an early sexual debut were more likely to report regretting their first sexual encounter together with lower well-being, compared to their counterparts who had their sexual debut at older ages.
The GWR and local bivariate relationship approaches utilised in this study allowed for the examination of spatially heterogenous relationships as local percent deviance differed across different districts and different relationship types were identified between the no condom use at first sex and the explanatory variables across districts. Similar sentiments were alluded to by Cheruiyot [35] and Fundisi et al. [36]. In accordance with Shacham et al. [58] that identifying predictors that contribute to geographic disparities in STIs is necessary to reduce such disparities, the findings of this paper have shown similar sentiments that determining factors influencing no condom use or lack of condom usage at different geographic areas or regions can lead to the matter being addressed at the local level.
The strength of this study is that it applied different local spatial analysis methods to understand the association between no condom use at first sex among respondents and related covariates at the local or neighbourhood level across the country. These different local spatial analysis methods complemented each other; for instance, the local bivariate relationships complemented the GWR model by further detecting other types of relationships, such as concave or convex relationships, which could not be detected by GWR. The GWR model was able to determine factors significantly associated with no condom use at first sex in different districts. The same factors were further explored to determine the type of relationship between each of them and the outcome variable using local bivariate relationships analysis. One of the lessons learned in this study is that different explanatory factors have different relationship types with no condom use at first sex at different spatial regions. The practical implication of this finding is that interventions should not always assume that there is a linear relationship between the outcome variable and the explanatory variable. Thus, for instance, in cases where there is a concave or convex relationship, the type of intervention that will be introduced will have to be revised or amended when the relationship direction changes. Also, to our knowledge, this is the first district-level analysis of no condom use at early sexual debut. Concerning limitations, the data used in this paper were obtained from a self-reported survey, and thus may be prone to social desirability bias. In addition, the accuracy of no condom use at first sex for older respondents was subject to good recall memory. Kincaid et al. [20] reported that memory of one’s first sexual experience with regard to condom use was expected to be good. Even though this recall bias might have an effect on the actual reporting of no condom use at first sex among older respondents, this did not have an impact on the final results of this article as those aged 35 and older (adults) did not have a significant influence on no condom use at first sex and were excluded from the final GWR model and further analysis.
CONCLUSION
Being female, young, never married, unemployed, having sexual debut at a younger age, having two or more sexual partners, having no risk of being infected with HIV, and having good Self-perceived Health (SPH) were significant factors associated with no condom use at first sex among respondents across the country, with pseudo R2 = 0.96 and AICc = 692. Local bivariate relationships showed the relationship between no condom use at first sex and most explanatory variables to be positively linear in most districts with the exception of having never married, which showed a positive linear relationship in 18 districts, while 33 districts showed a concave relationship. This localised approach highlights similarities and differences in no-condom use among districts, and thereby supports the evidence base for geo-targeted interventions and precision planning tailored to these areas.
The development of educational initiatives aimed at youth is necessary to raise knowledge of the dangers of unprotected sex as well as the significance of condom use. It is important to provide access to condoms and other kinds of contraception, particularly for young people and the unemployed. Comprehensive sexual education programs should be put into place in communities and schools to teach students about safe sexual behaviour, contraception, and how to avoid STDs. Therefore, more awareness campaigns should be organized to break the barriers, such as sexual relationship power, gender, and sociocultural and religious influences, which tend to put young, never married, and unemployed women at risk of no condom use at first sexual debut. Additionally, condom use should be highly encouraged and the stigma behind its usage among young people should be eliminated. It is also recommended that the type of relationship between no condom use at first sex and each explanatory factor at the local region be considered during geo-targeted interventions as this will assist in the type of intervention and duration of intervention. Policymakers, healthcare professionals, relevant stakeholders, and communities should endeavour to work together to lower the incidence of unprotected first sexual encounters and, in turn, lower the spread of HIV and STDs, in South Africa, by implementing these recommendations.
LIST OF ABBREVIATIONS
| STDs | = Sexually Transmitted Diseases |
| GWR | = Geographically Weighted Regression |
| SPH | = Self-perceived Health |
| VPs | = Visiting Points |
| SALs | = Small Area Layers |
| AGYW | = Adolescent Girls and Young Women |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethics approval was received from the Human Science Research Council Research Ethics Committee with protocol approval number REC:4/18/11/15. Approval was also granted by the Associate Director for Science, Center for Global Health (CGH), Centers for Disease Control and Prevention (CDC).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.


