All published articles of this journal are available on ScienceDirect.
Factors Influencing the Uptake of Isoniazid Tuberculosis Preventive Therapy among Eligible HIV Patients in Africa: A Systematic Review
Abstract
Background
This review employs a non-empirical research design, specifically a systematic review, to investigate evidence-based factors influencing the adoption of isoniazid Preventive Therapy (IPT) among eligible HIV patients. The objective is to contextualize these factors within an African setting, facilitating their accessibility for policymakers.
Material and Methods
This review followed the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines. A comprehensive search across various databases, including Google Scholar, Africa-wide information, APA PsycInfo, CINAHL Plus (EBSCO), Education Sources, Health Sources – Consumer Edition, Health Sources: Nursing/Academic Edition, Humanities and Social Sciences Index Retrospective Humanities Sources, MasterFILE Premier, MEDLINE, and SociINDEX was conducted. The inclusion criteria were met by a total of n=11 full-text articles from accredited peer-reviewed journals. Utilizing a quality assessment research instrument tool, the gathered data were synthesized and analyzed. The review spanned African sources from January 2019 to April 2023, revealing diverse factors affecting IPT uptake, encompassing influences from health workers, patients, and health system-related aspects.
Results
The study revealed the interplay of various factors categories into four themes that influence IPT intake mostly at the facility level and include: Patient-related factors, healthcare care providers, and health facility factors and strategies to improve IPT uptake.
Discussion
The study's findings underscore the significance of implementing Quality Improvement (QI) interventions comprising three essential components delivered as a cohesive package. Moreover, the study advocates for the incorporation of m-Health technology to send reminders to patients, thereby enhancing completion rates for IPT.
Conclusion
The papers revealed patient, health care workers, and health system challenges that requires the adoption of strategies such as quality improvement interventions, coupled with data monitoring, improving supply chain management, supportive supervision, enhanced health care infrastructure, healthcare workers capacity building, Partnership, Community and patient engagement and the integration of m-health technology as effective strategies to improve IPT uptake.
1. INTRODUCTION
Tuberculosis (TB) and Human Immune Virus (HIV) make up a dead synergy of infectious diseases, and the combined effect is apparent in many low- and middle-income countries (LMICs) [1]. According to the World Health Organisation (WHO) [2], TB remains a main global public health problem and a leading cause of death, even with the recent advancement of intensive global TB control efforts to end TB by the end of 2035. Tuberculosis is the most common Opportunistic Infection (OIs) and the major cause of mortality among people living with HIV (PLHIV) globally, as it possibly increases the rate of disease progression and mortality [3]. There are 10.6 million incident cases of TB, out of which an estimated 187,000 cases occurred in HIV-positive patients [4]. The risk of developing active TB in PLHIV is 16 (uncertainty interval 14–18) times higher than the rest of the world population. The international community has committed to eradicating the TB epidemic by 2030. Key objectives to achieve this ambitious aim encompass a 90% decrease in TB-related fatalities and an 80% decline in TB incidence rates by 2030, relative to the statistics recorded in 2015 [5].
In 2018, Africa represented a quarter (25%) of new TB cases among PLHIV and accounted for 44% of global TB-related deaths. This statistic is alarming, considering that most countries in Africa have adopted the WHO recommendations for TB isoniazid preventive therapy (IPT) [6]. However, the uptake is still low. IPT uptake measures the proportion or rates of eligible individuals, especially PLHIV, who start and adhere to TB preventive therapy to reduce the risk of developing active TB infection. The high uptake signaling effective implementation of IPT, and the low uptake highlights barriers that need to be addressed for improved access and adherence [7].
Africa consists of diverse countries and regions, each with its own unique characteristics and healthcare systems. Developing countries, on the other hand, encompass a broader range of countries across different continents with advanced technologies. Nevertheless, general differences that are often observed in the African context compared to other developing countries encompass a range of interconnected factors that shape the overall implementation and adoption of IPT and can be influenced by various factors such as availability and accessibility of Isoniazid, geographical location, affordability, the presence of healthcare facilities, the quality of healthcare infrastructure, levels of knowledge and awareness, cultural or social barriers, and the support of relevant policies [8]. The emergence of the COVID-19 pandemic in 2019 had a significant impact on Africa, particularly in the Southern, Northern, and Western regions, where varying numbers of cases were reported. The pandemic caused disruptions in the progress made in TB prevention and control efforts, exacerbated by the clinical similarities between COVID-19 and TB, which made it challenging to diagnose the two conditions in African countries without access to the required technology. This challenge hindered the effective management and control of TB in these regions [9]. Consequently, it is crucial to conduct further studies to investigate and document the lessons learned from the factors that impact IPT uptake during and in the aftermath of the COVID-19 pandemic within the African context.
Tuberculosis Isoniazid Preventive Therapy reduce the burden of TB among HIV-infected persons by lowering TB transmission in a high risk population contributing to the broader public health goal of controlling and eventually eliminating TB as a public health threat (14), especially in the Sub-Saharan African (SSA) region [10]. In contrast to developed countries, many African nations encounter obstacles in the implementation of IPT for PLHIV. These barriers include limited research on IPT, a lack of innovative diagnostic tests, policy gaps, and challenges in program implementation. Despite the established effectiveness of IPT in reducing tuberculosis among PLHIV, these factors hinder its widespread adoption in developing nations [11, 12, 13]. Therefore, it is crucial to conduct a thorough investigation and review into the factors contributing to this situation in Africa and identify strategies to address these gaps effectively.
Isoniazid Preventive Therapy (IPT) reduce the burden of TB among HIV-infected persons by lowering TB transmission in a high risk population contributing to the broader public health goal of controlling and eventually eliminating TB as a public health threat [14]. The most common global regimen of daily isoniazid for ≥6 months has been demonstrated to prevent TB disease among persons who might be infected with TB and are at risk for TB disease [15]. The WHO advises that providing a course of IPT to all PLHIV and to all household contacts of persons with bacteriologically confirmed pulmonary TB disease can reduce the incidence of TB awfully however, the uptake of IPT is still low [16]. WHO further recommends IPT to treat tuberculous infections in high-risk populations, such as PLHIV, household contacts of persons with bacteriologically confirmed pulmonary TB disease, including all children aged 5 years who are close contacts of patients with infectious TB [1]. Tuberculosis preventive therapy involves administering one or more anti-tuberculosis drugs, such as isoniazid, to individuals with latent M. tuberculosis infection to prevent progression to active TB disease [2]. IPT not only alleviates individuals from the burden of TB-associated morbidity and mortality but also lessens the economic impact of the disease on the health system [17]. For over a decade, IPT has been a prioritized recommendation by the WHO for PLHIV and has been consistently included in subsequent guidelines. It is therefore important to document IPT completion as there is evidence that the adequate use of IPT lowers the risk of progression of TB disease and TB-related mortality for PLHIV [10].
The IPT implementation in many high TB burden countries is sub-optional, where only a few people who are initiated on IPT complete their regimen [18]. There are several factors that hamper IPT implementation. Hence it is imperative to explore and obtain evidence-based information regarding factors influencing IPT uptake and strategies employed to deal with such globally and share it with policymakers, programme managers, and implemen- ters to develop targeted interventions [19]. There are medication-related factors that are likely to account for a small fraction of the reasons why medication is dis- continued or deferred, including potential pill burden, side effects, and overlapping side effects with ART medications. Another factor is the attitude of healthcare workers towards IPT provision related to concerns with uncertainty in ruling out TB disease, including healthcare workers’ fear of patients developing TB disease while taking IPT, which they believe leads to drug resistance [20]. National Quality Improvement (NQI) collaborative was used to address multiple healthcare delivery, patient, and provider level barriers to IPT completion using the Continuous Quality Improvement (CQI) approach [21]. This literature review synthesizes both qualitative and quantitative studies to thematically present multiple factors and strategies that have been identified as influencing the uptake of IPT. It is believed that most countries, especially LMICs, can learn evidence-based practices from these findings and can be applied to an African context by making it accessible to policymakers.
Acknowledging the existing gaps in the cascade of care before initiating IPT, it is noteworthy that certain countries are currently documenting elevated levels of IPT coverage. For instance, South Africa reported that 53% of individuals newly enrolled in HIV care in 2017 received IPT [1]. Up to 50% of individuals who commence IPT fail to complete it. Nonetheless, as highlighted by a previous study [22], policymakers acknowledge that increasing initiation rates alone are inadequate. Consequently, they have recommended IPT completion as an additional indicator for monitoring and evaluation.
To better understand factors influencing the uptake of PT among eligible HIV patients in Africa, researchers investigated the following nested subquestion: What are the evidence-based factors and strategies that impact the uptake of IPT among eligible HIV patients? By systematically reviewing both qualitative and quantitative studies, the researcher aimed to identify common themes and trends in factors influencing IPT uptake among eligible HIV patients in Africa. The findings of this study were expected to provide valuable insights that can inform the development of targeted interventions to improve IPT uptake and TB prevention efforts among PLHIV in LMICs, particularly in the African context. Ultimately, by bridging the gap between research and practice, this study aimed to contribute to the global goal of ending the TB epidemic by 2030 [5].
2. MATERIALS AND METHODS
In this review, the Preferred reported Systematic Reviews and Meta-Analyses (PRISMA) framework was employed while it is commonly used for reporting reviews and evaluating randomized trials, it can also serve as a basis for reporting systematic reviews. PRISMA offers an evidence-based, standardized set of reporting elements for systematic reviews and meta-analyses [23]. Furthermore Moher et al., [23], elucidated that a systematic review endeavors to comprehensively aggregate all pertinent evidence meeting predetermined eligibility criteria to address a specific research question. To achieve this, it employs explicit, systematic methodologies to minimize bias during the processes of identifying, selecting, synthesizing, and summarizing relevant studies. In a related context [24], expounded on how systematic reviews and meta-analyses present their findings by amalgamating and analyzing data from various studies conducted on similar research topics.
2.1. Planning Phase: Search Strategy
An experienced librarian assisted in a manual search of the research articles from Africa-wide information APA PsycInfo, CINAHL Plus (EBSCO), Education Sources, Health Sources – Consumer Edition, Health Sources: Nursing/Academic Edition, Humanities and Social Sciences Index Retrospective: 1907-1984 (H.W. Wilson), Humanities Sources, MasterFILE Premier, MEDLINE, SociINDEX search engines. Search expressions were developed for factors and strategies influencing the uptake of IPT among eligible HIV patients that were published in the English language from January 2019 to April 2023 (Fig. 1). Four search strategies were used, as indicated in Table 1.
2.2. Scholarly Documents Selection Phase: Screening
The researchers curated peer-reviewed scholarly sources from accredited journals to address the research questions. Fig. (1) outlines the sequential steps taken during the scholarly document search process. Initially, 100 records were identified. However, 34 records were excluded due to information duplication or failure to meet the inclusion criteria, resulting in the 66 remaining records that underwent further screening. Subsequently, 32 records were eliminated for containing irrelevant information, leaving a total of 34 records. The eligibility of these 34 records was assessed, and 23 scholarly documents were subsequently removed as they contained extraneous information pertaining to other countries. Ultimately, only 11 scholarly documents met the criteria and were utilized in this study.
The review incorporated both qualitative and quantitative research articles published in English between January 2019 and April 2023 to include articles that were recently published within 5 years. The publication time frame of January 2019 to April 2023 was chosen to ensure the inclusion of the most recent and relevant research, reflecting the latest advancements and trends in the field. This period captures up-to-date evidence while maintaining the review’s focus on current developments. Extending the timeframe might dilute the review's relevance by incorporating outdated studies. These articles were specifically conducted to analyze and explore evidence-based factors and strategies influencing the uptake of IPT among eligible HIV patients. Excluded from the review were studies lacking a detailed methodology, abstracts, duplicates, newspaper articles, magazines, and studies not written in English. Additionally, studies published before 2019 or after April 2023, as well as those not published in peer-reviewed journals, were excluded from upholding quality standards, as outlined in the protocol depicted in Fig. (1).
2.3. Selection Criteria
The selection process adhered to the summarized inclusion and exclusion criteria outlined in Table 2. During this phase, the researchers meticulously validated the retrieved documents to ensure the study's overall quality. As outlined in Appendix A, Table A1, the study centered on eleven scholarly documents. Consequently, each article underwent a thorough review by the researcher to ascertain compliance with the established inclusion and exclusion criteria. The specific details of these criteria are illustrated in Table 2 below. Studies conducted during the COVID-19 pandemic were instrumental in identifying gaps in IPT and understanding the evolving situation. They also provided valuable lessons for effective recovery and planning for future pandemics. These studies offered insights and guidance to policymakers, aiding them in managing TB and preparing for potential future pandemics.
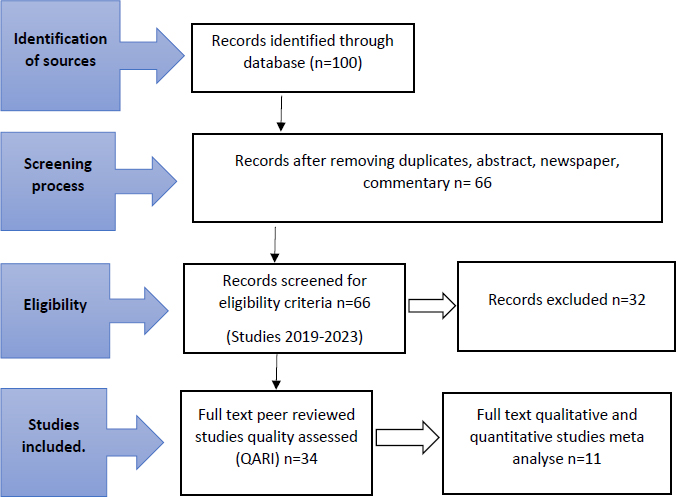
Systematic review flow chart adapted from preferred reporting items for systematic review-PRISMA (author’s own work).
| Isoniazid prophylaxis” OR “Tuberculosis preventive therapy” OR “IPT” OR “INH therapy |
|---|
| AND (“Uptake” OR “Adherence” OR “Utilization” OR “Uptake factors”) AND (“HIV-positive”) |
| OR “People living with HIV” OR “HIV patients” OR “HIV/AIDS” |
| AND (“Africa” OR “Sub-Saharan Africa” OR “African countries” OR “African context”) |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Scholarly documents in the English language. | Scholarly documents not published in the English language. |
| Scholarly documents covering the variables of the study. | Scholarly documents that did not cover the variables of the study. |
| Scholarly documents published from 2019 to March 2023. | Studies published before 2019 or after March 2023. |
| Studies that were published in peer-reviewed journals. | Studies that were not published in peer-reviewed journals. |
2.4. Data Analysis and Synthesis
The data analysis and synthesis process for the 11 qualified sources in this study involved several steps. This comprehensive approach ensured that the selected sources wereof high quality, and the data synthesis was conducted in a systematic and rigorous manner, meeting the standards set for the study as follows:
A quality assessment research Instrument (QARI) adapted from Joanna Briggs institute (JBI) critical appraisal tool or checklist for systematic reviews was used to assess the quality of the selected sources, ensuring adherence to the inclusion criteria. Data were extracted from the selected sources using an Excel template, including author, year, region, sample size, study design, population, and major findings. The extracted data were sorted and arranged alphabetically by the first author's name, and any duplicates were identified and removed. A scoring system based on the quality of each study was established. Studies with 5 points or fewer were excluded from the quality review. The two researchers independently reviewed and screened each record based on the specified inclusion and exclusion criteria. Full-text studies that passed the abstract-level screening were included in a full-text review and analyzed following thematic qualitative analysis methods. Any disagreements between the two reviewers or researchers were resolved through consensus during a meeting between the two reviewers. Factors and strategies influencing the uptake of IPT among eligible HIV patients were extracted from both quantitative and qualitative studies.
2.5. Thematic Data Analysis
Thematic data analysis was utilized to synthesize the data, involving eight stages. Initially, researchers familiarized themselves with the data by thoroughly reviewing selected sources that met the inclusion criteria, taking notes, and highlighting pertinent information on IPT uptake in the African context. In the second stage, a coding framework was developed, outlining potential themes and sub-themes based on the research review question. Four themes emerged and were summarized in Table 3. In stage three, researchers coded the data by assigning relevant codes to corresponding text segments, resolving differences through consensus. Stage four involved identifying patterns, connections, and relation- ships within and across the codes, while stage five entailed reviewing, critiquing, refining, and revising the themes to capture the content accurately. In stage six, an experienced researcher assessed and validated the themes for relevance, coherence, and comprehensiveness in addressing the research questions. In stage seven, the researchers interpreted and synthesized the themes, considering implications, patterns, and underlying meanings. They examined consistencies, inconsistencies, and possible explanations across the sources. Finally, the findings were documented in the systematic review report, including clear interpretations, key insights, and supporting evidence summarized in Table 3. Quality assurance was ensured by having an experienced researcher review the synthesis process for compliance with inclusion criteria. Prior to data synthesis, rigorous quality assessments and risk-of-bias evaluations were conducted to ensure the validity and reliability of the findings [25, 26].
2.6. Ethical Considerations
Ethical approval was not required for this review, as the information gathered was obtained from publicly available sources, and no human participants were involved. However, ethical considerations remain important in systematic review studies. The researchers conducted the review with transparency and impartiality, adhering to inclusion criteria and proper reporting of the included studies. Researchers followed appropriate citation and referencing protocols to acknowledge the contributions of other researchers and avoid plagiarism. The methods and protocols were described in detail, and data and analysis were made available for review and verification by an experienced researcher. The reporting of the systematic review methods and findings complied with relevant guidelines, such as the PRISMA statement, ensuring a clear and comprehensive presentation.
| Theme | Sub-theme |
|---|---|
| 1. Patient factors | 1.1. High rate of side effects 1.2. Poor adherence to appointments 1.3. Poor adherence to IPT 1.4. Unemployment and poverty |
| 2. Healthcare workers' factors | 2.1. Poor training on IPT/ HIV guideline 2.2. Low or irregularities in screening and irregular timing of IPT 2.3. Clinical misconception/ misperception 2.4. Poor documentation |
| 3. Health system factors | 3.1. Shortage of Isoniazid 3.2. Poor supportive supervision 3.3. Poor monitoring and tracking system. |
| 4. Strategies to improve IPT uptake | 4.1. Quality improvement project 4.2. Routine monitoring and file review 4.3. Capacity building 4.4. M-health electronic tracking system |
3. RESULTS AND DISCUSSION
3.1. The Reviewed Source's Characteristics
A total of 100 research articles underwent screening, with 11 studies meeting the inclusion criteria for this literature review. All 11 articles were derived from quantitative studies, encompassing diverse methodologies: 1 cluster-randomized controlled trial, 1 prospective cohort, and longitudinal study, 3 cross-sectional surveys, 1 observational longitudinal study, 1 quasi-experimental study, 1 retrospective cohort study, 1 randomized trial, 1 longitudinal study, and 1 retrospective study.
The studies were geographically diverse, spanning Nigeria (3), Namibia (1), Tanzania (1), Malawi (1), Ethopia (1), South Africa (3), and Uganda (1). Notably, three studies applied a quality improvement approach to enhance IPT uptake, while one study aimed at improving the quality of HIV and TB services. Two studies focused on assessing the knowledge and adherence of healthcare workers to IPT guidelines. Additionally, one study explored the impact of m-health on IPT adherence among patients, another delved into the effects of IPT on TB incidence and identified risk factors among HIV patients, one study evaluated the efficiency and safety of IPT for TB prevention, and the last study concentrated on the assessment of IPT uptake among HIV patients. Detailed insights into the factors and strategies influencing IPT uptake from these individual studies are presented in Appendix A, Table A1.
3.2. Thematic Results
The study identified and summarized four major themes, as presented in Table 3.
3.2.1. Theme 1: Patient Factors
3.2.1.1. High Rate of Side Effects
The literature indicates that patients often struggle with adherence to IPT due to side effects, significantly impacting the completion of treatment, which serves as the endpoint of the IPT initiation strategy. Isoniazid therapy commonly causes side effects such as vitamin B6 deficiency, peripheral neuropathy, and hepatotoxicity. Vitamin B6 deficiency and peripheral neuropathy can be prevented or treated with pyridoxine supplementation, while hepatotoxicity requires regular liver function monitoring [21]. Moreover, the literature highlights that patients who do not report any side effects associated with IPT are twice as likely to successfully complete their treatment [21]. In one study, it was noted that numerous healthcare workers expressed a lack of familiarity with isoniazid dosing and counseling regarding potential adverse treatment effects, especially in special populations such as children and pregnant women [27].
3.2.1.2. Poor Adherence to Appointments
The literature indicates that patients exhibited non-adherence to their IPT appointments at healthcare facilities. A specific study addressing healthcare workers' perspectives on the IPT program revealed their heightened concern about patient behavior. Healthcare workers identified patient behavior as problematic, citing its impact on general resistance and its role in causing patients to miss their appointments [8].
3.2.1.3. Poor Adherence to IPT
The literature uncovered instances where patients demonstrated non-adherence to their treatment, either by occasionally missing doses or not following the prescribed daily drug regimen recommended by healthcare providers. Emphasizing the importance of counseling before initiating IPT and incorporating adherence monitoring for ART emerged as a key approach to assess patients' preparedness to initiate and successfully complete IPT [21]. One study identified a notable challenge in implementing IPT specifically highlighting poor adherence to treatment [28].
3.2.1.4. Unemployment and Poverty
In a study conducted in South Africa [29], the findings revealed that patients faced challenges related to unemployment, with some also contending with low income. These economic constraints restricted their access to health facilities, particularly in settings where facilities were not centrally located and easily accessible, primarily due to the associated high travel costs.
3.2.2. Theme 2: Health Care Workers Factors
3.2.2.1. Poor Training on IPT/ HIV Guideline
A deficiency in (HCWs) training emerged as a significant factor influencing the implementation of IPT. Particularly noteworthy was the insufficient training among HCWs in TB screening and the initiation of preventive therapy [30]. This lack of training may be a contributing factor to the suboptimal uptake of (IPT) services for People Living with HIV (PLHIV) [21].
3.2.2.2. Low or Irregularities in Screening and Timing of IPT
This study brought to light that the implementation of IPT is hindered by inadequate TB screening in numerous resource-limited settings. Notably, healthcare workers reported low rates of routine TB screening in HIV-positive patients. This practice stands in stark contrast to the recommendations of both the (WHO) and National Guidelines, which advocate for regular screening of all PLHIV during every healthcare visit [8].
3.2.2.3. Clinical Misconception/misperception
The study also highlighted that clinical misperception significantly impacts (IPT) programs. This influence extends to (HCWs) capacity to conduct accurate clinical assessments of HIV-infected clients for (TB) disease during each clinic visit. This process involves the utilization of (WHO) recommended symptom-based screening, where symptomatic patients undergo diagnostic tests such as clinical evaluation, sputum smear microscopy, and chest radiography [8].
3.2.2.4. Poor Documentation
Inadequate documentation of IPT commencement in patients' care cards and IPT registers by clinicians emerged as a significant hindrance to IPT implementation. This deficiency in documentation also exerts substantial adverse effects on the ability to monitor and track patients' treatment adherence [31].
3.2.3. Theme 3: Health System Factors
3.2.3.1. Shortage of Isoniazid Drug
The scarcity of isoniazid emerged as a hurdle in implementing IPT within resource-limited settings. A particular study revealed that the observed low level of IPT uptake in their investigation mirrored documented challenges in various Sub-Saharan African countries. These challenges primarily revolved around recurrent stockouts and other issues within the supply chain of isoniazid during the program's rollout [31].
3.2.3.2. Poor Supportive Supervision
The study recognized that inadequate support for patient supervision significantly affects the IPT program. A specific study highlighted that the heavy workload borne by healthcare providers can frequently lead to a decline in both the quality of care and the support provided, underscoring the need for organizational context reforms to enhance support for IPT program [31].
3.2.3.3. Poor Monitoring and Tracking System
As indicated in a previos study [31], on a global scale, challenges such as inadequate monitoring and an ineffective tracking system for clients eligible for IPT have been identified as significant impediments to the implementation of IPT in resource-limited settings.
3.2.4. Theme 4: Strategies to Improve IPT Intake
3.2.4.1. Quality Improvement Project
A study conducted in Uganda initiated a national quality improvement collaborative in January 2019 as part of a comprehensive, large-scale, continuous quality improvement effort. The findings reveal a noteworthy improvement in the completion rate of IPT, reaching 89%. Consequently, the study strongly advocates for the implementation of quality improvement strategies within healthcare facilities to enhance both the uptake and completion of IPT [21].
3.2.4.2. Routine Monitoring and File Review
A single study highlighted the significance of consistent, supportive supervision, regular audits of patients' medical records, and routine monitoring and evaluation of the IPT program as crucial elements for reaching the IPT initiation and completion targets [28].
3.2.4.3. Capacity Building
In a study conducted in Nigeria [28], suggested that regular training and re-training sessions for all clinical staff in the relevant clinics should be conducted, particularly following the review of guidelines. The study emphasized the importance of incorporating constant reminders, in the form of text messages, into the clinic's routine activities. This measure was deemed essential to ensure the effective and consistent implementation of the IPT program.
3.2.4.4. M-health Electronic Tracking System
In their study [28], demonstrated the effectiveness of m-health technology in enhancing knowledge and adherence to IPT guidelines among health workers. Furthermore, it was observed to improve knowledge among patients. As a result, the study recommends that program implementers should actively contemplate the incorporation of text message reminders into the regular activities of TB/HIV programs. This inclusion is proposed to contribute to heightened awareness among health workers, thereby fostering improved implementation of IPT.
4. DISCUSSION OF FINDINGS
4.1. Patient Factors as a Barrier to IPT Uptake among Eligible HIV Patients
The review clearly demonstrates that a combination of different patient factors obstructs an IPT uptake. Inadequate adherence significantly contributes to low completion rates as a result of interruptions in IPT, primarily driven by the considerable side effects associated with both IPT and ART medications [32]. Adolescents and young adults living with HIV tend to have significantly lower rates of IPT uptake, as reported in studies [33]. A scoping review conducted across 36 countries, including South Africa, supported these findings and identified patient-specific obstacles to medication and IPT adherence, such as experiencing side effects, dealing with pill burden, lacking comprehension of the reasons for taking the medication, disruptions in routines due to busyness or changes, feelings of stress, helplessness, guilt, and disappointment associated with the disease, leading to forgetting to take the treatment at designated times [34]. Additionally, poor health literacy, particularly when instructions are not provided in the individual's native language, further contributes to the challenges [34]. Another study conducted in South Africa examined the challenges impacting Nurse-Initiated Management of Antiretroviral Therapy (NIMART) and found that patient-related factors, including low socioeconomic status and reluctance to disclose their HIV status, significantly affect treatment adherence [35].
Furthermore, another study on why do patients struggle with their medicines shed the light on matters where some patients expressed a desire to experiment with not taking medication despite the potential life threatening consequences [36]. In contrast, others viewed medication adherence as a crucial and ongoing aspect of their lives, considering it a lifesaving measure. Hence, it is important to engage in discussions with patients regarding the seriousness of their condition and the importance of medication in order to raise awareness and understanding. Furthermore, another study [36] highlighted that patients face challenges such as the mental burden of managing multiple medications, mistrust in the efficacy of the medication due to experiencing side effects that worsen their condition, and the need to make lifestyle adjustments such as abstaining from alcohol. Additionally, time constraints during healthcare appointments often limit their ability to raise their concerns and address their questions with healthcare providers. The study conducted in spain, emphasized the importance of simplifying treatments to enhance adherence. They also recommended regular reviews of treatment plans [37]. Furthermore, the study suggested that training in motivational clinical interviews for healthcare workers should be provided during the pre-placement phase of newly graduated professionals.
This review further highlights the correlation between poor adherence to appointments and low IPT uptake in numerous countries. This is supported by a previous study [38], as well as the findings of another study [39], which emphasized the significance of pre-IPT counseling and aligning appointment dates for both ART and IPT to enhance adherence. Failing to adhere to appointments exacerbates the burden of chronic diseases [40].
The uptake of IPT is significantly influenced by unemployment and poverty, particularly in (LMICs) like South Africa. In 2023, South Africa had a high unemployment rate of 32.9%, with a significant impact on the youth population and a considerable number of individuals living below the poverty line [41]. Financial constraints prevent people from affording necessities such as food and transportation expenses required to attend scheduled clinical reviews and appointments. The COVID-19 pandemic further exacerbated these challenges. This is corroborated by a study conducted by [42] regarding the experiences of patients with chronic diseases. The study revealed that many patients faced difficulties in accessing health services and keeping their appointments due to a lack of financial resources for transportation and purchasing food, as they were required to eat before taking their treatment. This issue raises significant concerns and highlights the need for outreach programs and mobile services to improve access to healthcare services. On the other hand, the WHO End TB Strategy aims to achieve 90% coverage of IPT among (PLHIV) and close contact with infectious TB patients by 2035. However, the progress made is low and should be addressed [43].
4.2. Health Care Providers' Factors as a Barrier to IPT Uptake
This review highlights the apparent gap in knowledge and skills among healthcare providers (HCPs) when it comes to screening, identifying, and implementing IPT guidelines [35] supporting the notion that pre-service training should be offered to undergraduate (HCWs) to equip them with the necessary knowledge and skills for implementing national guidelines on HIV and TB management, including IPTs, at the Primary Healthcare (PHC) level. This training should also focus on enhancing adherence counseling skills. This is supported by a study conducted in Kenya which found that caregivers reported they lack awareness that their children required IPT, as well as a lack of education and counseling on the topic [32]. This indicates that the uptake of IPT among children is also low, and even among those who initiated IPT, the completion rate falls below 90% [32]. Moreover, the study uncovered that (HCWs) exhibit reluctance in prescribing IPT due to concerns about potential side effects, particularly hepatotoxicity and hepatic failure, and drug resistance, especially in individuals with previous instances of such adverse reactions [32]. This factor may contribute to the low and inconsistent screening and timing of IPT. Addressing this issue requires the implementation of robust clinical mentoring programs led by experts in HIV and TB management, as well as providing continuous professional development and in-service training to keep HCWs updated on current developments. These measures aim to enhance their confidence in effectively implementing IPT guidelines [35]. Additionally, another study [32] emphasized that inadequate recording, insufficient health information systems, and deficiencies in monitoring and evaluation systems within healthcare facilities, as observed among clinicians and pharmacy staff, contribute to the low uptake and completion rates of IPT. Therefore, an appropriate data management system that will facilitate collaboration and reporting by these HCWs should be strengthened to ensure effective and quality information management [35]. Poor documentation also contributes to low IPT, while in an actual sense, this was conductedand mostly disappointed those who are managing the programme. In the healthcare system, anything that is not recorded is often considered as not having beenperformed. These findings are supported by a study conducted in Germany which demonstrated that proper documentation could enhance reporting and the quality of care. Therefore, conducting file audits becomes essential in identifying gaps and developing improvement plans to address them effectively [43].
An additional factor recognized is the insufficient communication between health workers and patients, impacting adherence [28]. Another health system-related issue involves recurrent stockouts and challenges within the supply chain of isoniazid during the rollout [44]. The observed low level of IPT uptake in our study mirrors findings documented in other Sub-Saharan Africa.
In September 2018, the United Nations (UN) High-Level Meeting on TB underscored the need to enhance the implementation of IPT, setting a target for 30 million people to receive IPT by 2022. Although ample evidence supports the use of IPT in reducing the risk of progression to TB disease and TB-related mortality for individuals with HIV, it is crucial to document completion rates [10].
Acknowledging the existing gaps in the cascade of care before initiating IPT, it is noteworthy that certain countries are currently documenting elevated levels of IPT coverage. For instance, South Africa reported that 53% of individuals newly enrolled in HIV care in 2017 received IPT [2]. Up to 50% of individuals who commence IPT fail to complete it. Nonetheless, another systematic review study highlighted that policymakers [22] acknowledge that increasing initiation rates alone are inadequate. Consequently, they have recommended IPT completion as an additional indicator for monitoring and evaluation.
4.3. Healthcare Facility Factors as Barriers to IPT Uptake
This was supported by a study conducted in Nigeria, where quality improvement projects involving members from various departments were undertaken to delve deeper into the issues hindering IPT performance at the facility level [31]. These quality improvement projects also facilitated the strengthening of frequent and consistent file audits to identify gaps as soon as possible before reporting deadlines.
Acknowledging health system barriers as barriers to IPT uptake underscores their significant impact on TB prevention efforts, particularly among PLHIV [38]. These factors not only influence individual patient outcomes but also have broader implications for public health outcomes at the community and global levels [32]. One crucial aspect of this discussion is addressing systemic issues within healthcare facilities that hinder IPT uptake. These issues range from the limited availability of IPT supplies to the absence of standardized screening protocols and insufficient training for healthcare providers [45, 46]. Without adequate resources and support, healthcare facilities may struggle to effectively identify and initiate IPT for eligible individuals, leading to missed opportunities for TB prevention among PLHIV.
Integration of TB and HIV services within healthcare facilities is another critical consideration. When TB and HIV services are not well-integrated, PLHIV may not receive comprehensive care that includes screening for TB and access to IPT [47]. Strengthening referral systems and improving communication between different departments can help ensure that PLHIV is routinely screened for TB and offered IPT as part of their HIV care, thereby enhancing uptake and adherence to IPT regimens [2].
Insufficient supportive supervision significantly affects the quality of care provided to patients receiving IPT [48]. Healthcare providers, burdened with heavy workloads, may struggle to offer adequate support and supervision, leading to potential gaps in care delivery [49]. This highlights the need for organizational reforms within healthcare settings to address workload issues and implement supportive supervision mechanisms. By providing healthcare workers with the necessary support and resources, such as training and guidance, healthcare systems can enhance the effectiveness of IPT programs and ensure better patient outcomes [50].
In addition, the current study further found that inadequate monitoring and tracking systems pose significant challenges to IPT implementation, particularly in resource-limited settings [38]. Without proper systems in place, it becomes difficult to identify and follow up with individuals eligible for IPT, resulting in missed opportu- nities for TB prevention. Improving monitoring and tracking mechanisms is essential for ensuring the timely delivery of IPT to eligible individuals and for evaluating the effectiveness of IPT programs. By implementing robust monitoring tools and enhancing data management systems, healthcare systems can better track IPT uptake and outcomes, ultimately improving TB prevention efforts [51].
4.4. Strategies that can be Employed to Improve IPT Uptake
As highlighted in a study conducted in Uganda [21], IPT has demonstrated efficacy in reducing the risk of active (TB) by up to 60% among individuals living with HIV who exhibit evidence of latent TB infection. IPT stands as a crucial element within the (WHO) End TB strategy. The WHO advocates universal ART for all PLHIV, irrespective of their CD4+ cell count, following the Test and Treat strategy. Additionally, the WHO conditionally recommends a minimum of 36 months of IPT for PLHIV in regions characterized by high TB transmission.
For PLHIV, the optimal period to commence IPT is either before, during, or shortly after initiating ART, as this timeframe corresponds to a heightened risk of TB development (Karanja et al., 2020). The promotion of IPT adherence and the provision of support to patients play crucial roles in realizing the anticipated benefits of the ongoing global scale-up of IPT for high-risk individuals with HIV [18].
A study conducted in resource limited settings revealed that Quality Improvement (QI) interventions effectively enhanced HIV Testing Services (HTS) and the initiation of IPT [19]. Regular monitoring and evaluation were key in preventing possible relapse. The implementation of the QI approach, encompassing three essential components delivered as a 'package': (1) training and capacity building of healthcare workers; (2) in-person QI mentorship of clinic staff; and (3) data quality improvement (DQI) activities to enhance the reliability of routine clinic data, demonstrated the potential to improve both coverage and completion rates of IPT among eligible HIV patient. The recommendation is for government and health programmers to support facilities in applying QI approaches to enhance health service delivery [31]. In a previous study [28], it was demonstrated that m-health technology effectively enhanced knowledge and adherence to IPT guidelines among health workers while also improving knowledge among patients. Based on these findings, we advocate for the inclusion of text message reminders as a routine component in TB/HIV activities. This integration is envisaged to heighten health workers' awareness and commitment to IPT implementation. Additionally, regular training sessions are recommended to continually enhance health workers' knowledge, ensuring they stay abreast of updated recommendations in IPT guidelines [50]. This proactive approach is crucial for keeping health workers well-informed and aligned with any guideline changes. Keeping patients well informed of the purpose and benefits of IPT to take responsibility for their care plan through actively participating and being involved in decision-making. Patient-centred care is key to improving health outcomes [52]. Transitioning from traditional care to telemedicine, mHealth to send reminders, mobile and outreach services, and medical buddy systems, including appointment systems and home medication delivery, can significantly enhance access to healthcare services and medication [53-56].
5. LIMITATIONS OF THE STUDY AND FUTURE RESEARCH DIRECTION
Several limitations of this study are acknowledged. The primary focus was on investigating the factors and strategies influencing the uptake of IPT, rendering the study specific to this context. The inclusion criteria restricted the examination to full-text, peer-reviewed studies, excluding other sources that were not peer-reviewed or published in journals. This exclusion was guided by adherence to the predetermined criteria. Additional studies are warranted to address the identified gaps in the IPT program and provide a more comprehensive understanding.
CONCLUSION
The study aimed to comprehensively analyze factors and strategies influencing the uptake of IPT within an African context. Findings revealed that healthcare workers, health systems, and patient factors significantly impacted the accessibility and success of the IPT program. Challenges included socio-economic factors, substance abuse, adherence, pill burden, side effects, and lack of knowledge. Health system-related factors included healthcare worker attitudes, training gaps, screening irregularities, prescribing uncertainties, and clinical misperceptions. The study emphasizes implementing strategies to enhance IPT effectiveness, such as strengthening clinical mentorship to improve the capacity of HCWs, improving data management, enhancing healthcare infrastructure I underserved areas, promoting community engagement, fostering partnerships, advocating for integration with HIV services, and improving the supply chain, QIP, and monitoring processes. Consideration of m-Health for patient reminders is also recommended to improve IPT completion rates.
RECOMMENDATION
Enhance Adherence Support
Implement comprehensive programs with patient education, counseling, and regular follow-ups. Address IPT and ART side effects through personalized treatments to improve adherence, especially among adolescents and young adults.
Improve Health Literacy and Communication
Create educational materials in local languages to boost health literacy and ensure understanding of IPT's importance. Use tailored communication and motivational interviewing to address emotional and mental burdens, enhancing patient engagement.
Address Socioeconomic Barriers
Launch outreach programs and mobile clinics to tackle financial and logistical obstacles. Provide support for transportation and food security to ensure patients can attend appointments and adhere to treatment.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| CQI | = Continuous Quality Improvement |
| DQA | = Data Quality Improvement |
| QI | = Quality Improvement |
| PLWHA | = People Living with HIV/AIDS |
| IPT | = Isoniazid Preventative Therapy |
| IPT | = TB Preventive Treatment |
| TB | = Tuberculosis |
AVAIALABILITY OF DATA AND MATERIALS
All the data and supportive information are provided within the article.
ACKNOWLEDGEMENTS
The authors would like to thank the University of South Africa for paying the page fees for article publication. The librarian is also thanked for his support. The experienced researcher is thanked for her tireless efforts and guidance in quality assurance.
SUPPLEMENTARY MATERIALS
Indentation PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.
Supplementary material, along with the published article, is available on the publisher’s website.
APPENDIX A
Indentation the current study included eleven scholarly documents published in various databases. In this regard, Table A1 depicts a representation of the entire process of the researcher’s search.
| Author and Year/Refs. | Country | Purpose | Participants |
Methodology (Data Collection and Analysis) |
Key Findings | QARI Score |
|---|---|---|---|---|---|---|
| Gengiah et al., 2020 [19] | South Africa | A cluster-randomized controlled trial to improve the quality of integrated HIV-tuberculosis services in primary healthcareclinics in South Africa. | Nurse supervisors | Cluster‐randomized controlled trial. | QI improved HIV testing and IPT initiation compared to SOC. TB screening, ART initiation, and VL testing remained similar. Incorporating QI methods into routine supervision and support activities may strengthen integrated HIV‐TB service delivery. | 8 |
| Sensalire et al., 2020 [21] | Uganda | To document retention, adherence, development of active TB disease, possible side effects, and completion. | HIV patients without TB disease initiated on a dosage of isoniazid 300 mg/day for adults and 150 mg/day for children for a period of 6 months. | A prospective cohort and longitudinal study. The patients initiated on INH were monitored consecutively for 6 months for retention, adherence, development of active TB disease, possible adverse drug reactions, and completion. Data for all patients initiated on IPT in the January cohort was captured and continuously updated monthly by health workers up to 7 months | The completion of IPT was at 89%, patients adhered to treatment (89%) and kept their appointment schedules retention (89%). All patients (100%) received IPT at each appointment visit. Only 4% of patients experienced side effects of isoniazid (INH), but none of them developed active TB at the end of the 6 month | |
| Kendall et al., 2020 [18] | South Africa | A cluster-randomized controlled trial to improve the quality of integrated HIV-tuberculosis services in primary healthcare clinics in South Africa. | Patients attending HIV clinics with active prescriptions for isoniazid preventive therapy | Cross-sectional surveys. The Isoscreen (GFC Diagnostics) point-of-care test, a colorimetric test based on the Arkansas method to test Urine for isoniazid metabolites. Poisson regression was used to analyze risk factors for nonadherence. | Adherence to isoniazid preventive therapy among patients with HIV in South Africa is inadequate, is overestimated by self-report, and declines with time on treatment. | |
| Yirdaw et al., 2019 [54] | Ethiopia | To assess the magnitude and determinants of breakthrough tuberculosis. | All newly enrolled PLHIV in chronic HIV care who started IPT. | Retrospective, observational, longitudinal study. Cox regression analysis was used to study factors associated with breakthrough TB. | Breakthrough TB was uncommon among those receiving IPT in the study setting. | |
| Nabity et al., 2021 [27] | Malawi | To measure the frequency and timeliness of early-phase IPT implementation to inform quality improvement processes. | PLHIV newly enrolled in ART care. | A cross-sectional, two-stage cluster medical record review was used. | Early-phase IPT uptake among adults at ART centers in Malawi was high. Child uptake needed improvement. | |
| Akamike et al., 2021 [55] | Nigeria | To determine the effect of m-health on health worker knowledge and adherence to isoniazid preventive therapy (IPT) guidelines and on patient knowledge and adherence to isoniazid treatment. | All eligible health workers and HIV infected patients were recruited. | Quasi-experimental study. Chi-square test was carried out at p < 0.05 and 95% confidence interval. | At baseline, 54.5% and 63.4% of health workers in the intervention and control arms, respectively, had good knowledge, which improved significantly to 90.2% in the intervention arm after the intervention. There was no significant difference in adherence among patients in both arms. | |
| Sabasaba et al., 2019 [10] | Tanzania | To ascertaining the effect of IPT on TB incidence and to determine risk factors for TB among HIV positive adults in Dar es Salaam region. | HIV positive adults (≥15 years) who were enrolled in CTCs for the first time between January 2011 to December 2014 | Retrospective cohort study and data analysis was performed using Stata version 13.1. | Isoniazid preventive therapy (IPT) has shown to be effective in reducing TB incidence among HIV infected adults in Dar es Salaam. More efforts are needed to increase the provision and coverage of IPT. | |
| Ahmed et al., 2021 [56] | South Africa. | To identify factors associated with low IPT prescription rates among health care workers (HCWs) in rural South Africa. | Healthcare workers were included in the study | Quantitative design and data were collected using self-reported questionnaire. | Among 160 HCWs, 44% had experience prescribing IPT. On multivariable analysis, prescribers (n = 71) who believed their patients would not disclose IPT use to others were significantly less likely to prescribe IPT (aOR 4.19 95% CI 1.35–13.00; p = 0.01). Inadequate isoniazid supplies trended towards significance (aOR 10.10 95% CI 0.95–106.92; p = 0.06) in association with low prescription rates. | |
| Roscoe et al., 2020 [8] | Namibia | To evaluate the uptake of tuberculosis Preventive therapy for people living with HIV in Namibia. | HIV patients and health care workers | Retrospective study quantitative patient chart review using facility data sources. Qualitative survey of health care workers (HCWs) to evaluate provider perspectives on IPT practices and challenges. | Only 1 in 5 eligible PLHIVS completed the IPT cascade in Namibia. Lack of training, irregularities with TB screening and timing of IPT, unclear prescribing and recording responsibilities, and clinical misperception may have contributed to the suboptimal programmatic implementation | |
| Ogunsola et al., 2019 [31] | Nigeria | To improve IPT coverage using quality improvement approaches that help identify the root cause and improve coverage of isoniazid preventive therapy | Adherence counsellor, a pharmacist, a record officer and two other clinic staff | Longitudinal study. Data were collected over a six month period with a learning sessions at the end of every two-month PDSA cycle. Data was analyzed using Microsoft Excel 2010 | The two most contributory factors to low IPT initiation and completion in the facility with prioritization matrix scores of 30 and 25, respectively, were poor tracking system for IPT-eligible clients and poor documentation of IPT commencement in the patients' care cards and IPT registers. | |
| Akamike et al., 2022 [28] | Nigeria | To assess health workers’ knowledge and adherence to Isoniazid Preventive Therapy guidelines | Health workers working in HIV clinics, and patients’ treatment cards. | A cross-sectional study was conducted in six health facilities providing HIV care in Ebonyi State using a semi-structured, self-administered questionnaire. Data analysis was carried out using SPSS version 20 software. | There was good knowledge and practice of the guideline from health worker self-reports, however, review of the treatment cards showed the prescription was low. |


