All published articles of this journal are available on ScienceDirect.
Association between Health Literacy and Self-care Behaviors with Traditional Thai Medicine during the COVID-19 Pandemic
Abstract
Background
Health literacy is a multidimensional concept that can lead to changing self-care behaviors.
Objective
This study aimed to assess health literacy, self-care behaviors, and factors related to self-care behaviors in traditional Thai medicine during the COVID-19 pandemic.
Methods
This cross-sectional study included 422 participants. The questionnaire consisted of sociodemographic characteristics, health literacy of traditional Thai medicine with COVID-19, and self-care behavior with traditional Thai medicine in relation to COVID-19. The data were analyzed using descriptive statistics, independent-sample test, one-way ANOVA, and Pearson's correlation coefficient.
Results
The mean score for communication to promote health was high (34.6±8.4). The mean score of overall health literacy was moderate (156.8±20.7), followed by self-care behavior (45.6±6.0), access to health information and services (30.5±5.2), and health knowledge and understanding (26.7±2.6). Pearson correlation coefficient analysis showed that there were significantly positive self-care behaviors, namely, access to health information and services (P-value < 0.001), communication to promote health (P-value < 0.001), media and information literacy (P-value < 0.043), and overall health literacy (P-value < 0.003), while informed decision-making was significantly negatively associated with self-care behaviors (P-value < 0.004).
Conclusion
Increasing overall health literacy and each dimension was associated with self-care behaviors. The findings suggest that interventional programs to develop health literacy are required to improve self-care behaviors.
1. INTRODUCTION
The Coronavirus Disease 2019 (COVID-19) affected public health and caused social and economic crises worldwide [1]. According to the World Health Organi- zation (WHO), approximately 774,771,942 individuals worldwide have cumulatively had the number of COVID-19 in 2024 [2]. COVID-19 is transmitted by the spread of aerosols or droplets containing the virus, such as sneezes or cough droplets, and by touching each other [3]. During the outbreak of COVID-19, WHO established public health and social measures, such as maintaining a distance of 1-2 meters from others, wearing a face mask in public, handwashing, and personal hygiene [4, 5]. Moreover, patients with COVID-19 are cared for using a holistic approach, such as modern medicine and traditional Thai medicine (TTM) treatments [6-8]. TTM is used to take care of one's own health to strengthen the immune system and help prevent COVID-19, such as through the use of andrographis paniculate and Thai herbs, which are the concepts of self-care behavior (SCB) and health literacy (HL) [7, 8].
According to WHO, HL is defined as the cognitive and social skills that determine the ability and skills to access information, knowledge, and understanding, including being able to advise on personal, family, and community health [9]. According to Nutbeam, HL is divided into 3 levels: Level 1: basic/functional HL; Level 2: communi- cative/interactive HL; and Level 3: critical HL [10]. Previous studies found a negative relationship between HL and the rate of frequent hospital admissions [11]. HL is also associated with good health outcomes, such as a lower prevalence rate of chronic diseases, reduced hospital admissions, and reduced healthcare expenditures [11, 12].
TTM has a concept of holistic health care that refers to health promotion, disease prevention, and rehabilitation using activities, such as herbal medicine usage, herbal steam, herbal compress, Thai massage, and traditional Thai exercise (Ruesi dadton) [13-15]. Importantly, SCB with TTM consists of three components: (1) a healthy body, which focuses on maintaining good physical health by exercising, healthy foods, and Thai massage to promote health; (2) a healthy mind, which focuses on maintaining good mental health; and (3) healthy behavior, which focuses on changing to healthier behaviors [16, 17]. Nonetheless, previous studies found that there was a lack of knowledge, attitudes, and practice toward COVID-19 [18, 19]. Therefore, the present study aimed to evaluate HL and SCB and factors related to SCB with TTM during the COVID-19 pandemic.
2. MATERIALS AND METHODS
2.1. Study Design
A cross-sectional study design was conducted in Phayao Province, Northern Thailand. Data were collected through face-to-face interviews between December 2021 and February 2022. The inclusion criteria were age 18 years or older, having been living in the area for more than 6 months, and being able to communicate in the Thai language. The sample size was calculated according to Krejcie and Morgan [20] with 464,333 (N) as the population, 48.7% (P) as the proportion of preventive behavior in residents [21], 3.841 as the chi-square value (X2) with degrees of freedom (df) of 0.95, and 0.05 as the degree of accuracy expressed as a proportion (d), as the formula of Krejcie and Morgan [20]:
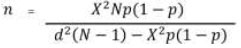 |
The sample size was set to 421.9 individuals, and an additional 10 percent was added to account for expected dropouts. The estimated sample size was 422 individuals. A multistage sampling method was used, and randomly selected communities were recruited.
2.2. Measures
The questionnaire was developed based on the HL and SCB concepts with TTM in relation to COVID-19. The questionnaire consisted of sociodemographic character- istics, the HL concept with TTM with COVID-19, and the SCB concept with TTM in relation to COVID-19. The content validity of the HL and SCB questionnaires was verified by three experts. The reliability of the questionnaire was 0.70 for HL and 0.80 for SCB. The structured questionnaires were divided into three parts as follows:
2.2.1. Part 1
Sociodemographic characteristics, including sex, age, income, marital status, education level, occupation, and underlying disease, were involved.
2.2.2. Part 2
The 71-item health literacy questionnaire consisted of six dimensions: Health knowledge and understanding (13 items); Access to health information and services (12 items); Communication to promote health (13 items); Media and information literacy (10 items); Management of self-condition (12 items); and Informed decision-making (11 items). The dimensions were as follows:
1) The health knowledge and understanding dimension included 13 items. Responses were measured based on a 3-point Likert scale: true = 3, false = 2, and never = 1. The scores ranged from 13 to 39: low = 13–22, moderate = 23–32, and high = 33–39.
2) The dimension of access to health information and services included 12 items. Responses were measured based on a 5-point Likert scale: 5 = always, 4 = often, 3 = sometimes, 2 = rarely, and 1 = never. The scores ranged from 12 to 60: low = 12–28, moderate = 29–45, and high = 46–60.
3) The communication to promote health dimension included 13 items. Responses were measured based on a 5-point Likert scale: 5 = always, 4 = often, 3 = sometimes, 2 = rarely, and 1 = never. The scores ranged from 13 to 39: low = 13–22, moderate = 23–32, and high = 33–39.
4) The media and information literacy dimensions included 10 items. Responses were measured based on a 5-point Likert scale: 5 = always, 4 = often, 3 = sometimes, 2 = rarely, and 1 = never. The scores ranged from 10 to 50: low = 10–24, moderate = 25–39, and high = 40–50.
5) The management of the self-condition dimension included 12 items. Responses were measured based on a 5-point Likert scale: 5 = always, 4 = often, 3 = sometimes, 2 = rarely, and 1 = never. The scores ranged from 12 to 60: low = 12–28, moderate = 29–45, and high = 46–60.
6) The informed decision-making dimension included 11 items. Responses were measured based on a 3-point Likert scale: agree = 3, disagree = 2, and never = 1. The scores ranged from 11 to 33: low = 11–19, moderate = 20–28, and high = 29–33.
The total score range of the 61-item HL questionnaire, including all the above six dimensions of HL, ranged from 61 to 281: low = 61–135, moderate = 136–210, and high = 211–281.
2.2.3. Part 3
A 14-item SCB questionnaire with TTM consisted of three components: healthy body, healthy mind, and healthy behavior. Responses were measured based on a 5-point Likert scale: 5 = always, 4 = often, 3 = sometimes, 2 = rarely, and 1 = never. The scores ranged from 14 to 60: low = 14–30, moderate = 31–47, and high = 48–60.
2.3. Data Analysis
The frequencies, percentages, means, and standard deviations of the data are presented. The mean differences between variables were evaluated using the independent sample test and one-way ANOVA. Pearson's correlation coefficient was used to test the relationships between dependent and independent variables. The significance level was set at a P-value < 0.05.
3. RESULTS
The demographic characteristics of the participants were as follows: 65.5% were female (n=277), had a mean age of 30.6 years, were single (76.5%), had a bachelor's degree or had a higher education level qualification (73.0%), had a mean monthly income of 12614.7 Thai baht, were students (53.6%), and had no underlying diseases (77.3%). There were statistically significant differences between SCB in terms of sex (P-value < 0.001), age (P-value < 0.001), marital status (P-value < 0.001), and occupation (P-value = 0.001). There was a significant positive association between SCB and age (p < 0.001) (Table 1).
| Variables | N (%) | P-value |
|---|---|---|
|
Sex Male Female |
145 (34.4) 277 (65.6) |
<0.001**a |
|
Age (years), mean±SD <40 ≥40 |
30.6±12.8 344 (81.5) 78 (18.5) |
<0.001**b 0.002a |
| Income (Thai baht), mean±SD | 12614.7±12820.0 | 0.069b |
|
Marital status Single Married Divorce |
323 (76.5) 80 (19.0) 19 (4.5) |
<0.001**c |
|
Education <Bachelor's degree ≥Bachelor's degree |
114 (27.0) 308 (73.0) |
0.495a |
|
Occupation State enterprise and governance officials Student Own bussiness Housewife and unemployed Others (agriculture, and others) |
66 (15.6) 226 (53.6) 46 (10.9) 44 (10.4) 40 (9.5) |
0.001*c |
|
Underlying diseases No Yes |
326 (77.3) 96 (22.7) |
0.146a |
| Variables | Mean±SD | Scores | r | P-value |
|---|---|---|---|---|
| Health knowledge and understanding | 26.7±2.6 | Moderate | -0.024 | 0.622 |
| Access to health information and services | 30.5±5.2 | Moderate | 0.182 | <0.001*** |
| Communication to promote health | 34.6±8.4 | High | 0.296 | <0.001*** |
| Media and information literacy | 21.5±5.7 | Low | 0.099 | 0.043* |
| Management of health conditions | 27.1±6.3 | Low | -0.094 | 0.054 |
| Informed decision-making | 16.4±2.6 | Low | -0.141 | 0.004** |
| Overall | 156.8±20.7 | Moderate | 0.144 | 0.003** |
| SCB | 45.6±6.0 | Moderate | - | - |
The mean score for communication to promote health was high (34.6±8.4). The mean score of overall HL was moderate (156.8±20.7), followed by SCB (45.6±6.0), access to health information and services (30.5±5.2), and health knowledge and understanding (26.7±2.6). The mean score for management of health conditions was low (27.1±6.3), followed by media and information literacy (21.5±5.7) and informed decision-making (16.4±2.6). Pearson correlation coefficient analysis showed that there were significantly positively associated with SCB, namely, access to health information and services (P-value < 0.001), communication to promote health (P-value < 0.001), media and information literacy (P-value < 0.043), and overall HL (P-value < 0.003). In addition, informed decision-making was significantly negatively associated with SCB (P-value < 0.004) (Table 2).
4. DISCUSSION
This study identified HL, SCB, and factors related to SCB with TTM during the COVID-19 pandemic. Previous studies found that HL has been associated with changes in health behaviors. Importantly, HL is also a multi- dimensional concept and is defined as cognitive and social skills. The results of the present study show significant differences in SCB by sex, age, marital status, and occupation. In this study, a significant positive association was found between SCB and age.
The study findings indicate significant differences between sex and SCB. Similarly, Rehman et al. (2018) found that females had more healthcare behaviors than men [22]. Moreover, female genders often have health care due to health concerns during the COVID-19 pandemic [23]. A previous study found that men still have risk factors, such as smoking and a poor diet, while females tend to consume high-fiber foods and avoid foods with high cholesterol and fat [22]. A study found several confounding factors that cause risk behaviors and can result in serious health problems related to COVID-19, such as smoking, alcohol consumption, and decreased physical activity [24].
The findings of the present study indicate significant differences between age and SCB. The results are similar to a previous study that found that older individuals may have better healthcare experiences for rapidly advancing diseases [25]. In addition, older people may have higher risk factors than younger people and are especially vulnerable to COVID-19, aging-related physiological changes in all organ systems, such as weak immune systems and severe chronic diseases [25, 26].
The findings of the present study indicate significant differences between marital status and SCB. This finding is consistent with the findings of Peng et al. (2022) and Saisanan Na Ayudhaya et al. (2023) [21, 27]. A previous study found that married women are likely to have lower self-care than married men [27]. Married people have easier access to social support, which was a protective factor for mental health during the COVID-19 pandemic [27, 28]. Another study indicated that single people often have decreased physical activity and increased alcohol consumption, which lead to unhealthy lifestyles [29].
The present study found significant differences between occupational status and SCB. Similarly, Li et al. (2020) and Combs et al. (2023) revealed that high-status occupation and employment status were also associated with preventive behavior through access to better health outcomes [30, 31]. Another study found that pensioners or retired individuals are likely to have better healthcare behaviors than those who are unemployed [32]. However, previous studies found that lower socioeconomic status may increase the risk of certain behaviors [33, 34].
The results of this study show that the overall HL of the participants was moderate. Similarly, Intara- kamhanget et al. indicated that Thai people had a fair or moderate HL level (58.9%) [35]. In the present study, it was found that HL dimensions in access to health information and services, communication to promote health, media and information literacy, and overall HL are positively associated with SCB to COVID-19.
Yodmai et al. (2021) revealed that 58.2% of participants had easy access to health information [36]. The results of this study also showed that there was a relationship between SCB and access to health information and services. Access to health information and services is a basic humanitarian principle that can provide rapid and effective support to prevent and control diseases, including reducing the risks of spreading the illness to others [37, 38]. In the past, access to COVID-19 vaccines and treatment could reduce the risk of illness or death [38, 39].
The present study shows a relationship between SCB and communication in promoting health. The study demonstrated that communicating reliable health information can help people engage in self-health promotion and self-care, including preventing and rapidly controlling disease [40]. Moreover, people can access reliable educational information through the media, on the internet, and through social media, such as wearing a mask, social distancing behavior, and vaccination [40-42].
However, the HL dimension in informed decision-making has a negative association with self-care behavior and COVID-19. Previous studies found that decision-making was associated with HL and SCB [43, 44]. However, low decision-making in HL may have multiple factors contributing to poor health outcomes, such as perception, self-efficacy, and knowledge [45]. Other studies indicated that there were fewer self-protective measures among younger individuals due to several factors, including low health literacy, students' age, and perceived vulnerability [45, 46]. The limitation of this study was that it was a cross-sectional study describing HL and SCB and factors related to SCB with TTM during the COVID-19 pandemic. Future studies should be focused on long-term predictions. Interestingly, TTM is indeed a comprehensive system that encompasses physical well-being, mental wellness, and behavioral health. Aligning these aspects with health literacy concepts can indeed facilitate behavior changes and promote overall wellness within the framework of TTM.
CONCLUSION
Demographic characteristics and socioeconomic status, including sex, age, marital status, and occupation, are risks or/and protective factors of fundamental causes of physical and mental health and wellbeing. Further, increasing overall HL and each dimension is found to be associated with SCB. The findings suggest that interventional programs for HL are required to improve SCB.
AUTHORS’ CONTRIBUTIONS
Pongsaton Silangirn, Sarinthorn Thummayot, and Sakesun Thongtip made substantial contributions to the conception and design of the study. Pongsaton Silangirn, Sarinthorn Thummayot, Uratcha Sadjapong, and Sakesun Thongtip conducted the material preparation, data collection, and data analysis. The first draft of the manuscript was written by Pongsaton Silangirn and Sakesun Thongtip. The final manuscript was read and approved by all authors.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus Disease 2019 |
| WHO | = World Health Organization |
| TTM | = Traditional Thai Medicine |
| SCB | = Self-Care Behaviors |
| HL | = Health Literacy |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol was approved by the University of Phayao Human Ethics Committee, University of Phayao, Thailand (UP-HEC 1.3/058/64).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
All participants provided written informed consent to participate in this study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be made available upon request through the corresponding author [S.T].


