All published articles of this journal are available on ScienceDirect.
Examination of Herbal-drug Interactions: Implications for Patient Safety and Healthcare Practice in Lebanon: A Cross-sectional Study
Abstract
Background
The lack of regulation of herbal products in Lebanon, and potential risks associated with herbal-drug interactions potentiates the need for increasing awareness and understanding of herbal-drug interactions among patients and athletes in Lebanon. This study highlights the need for increased awareness and understanding of herbal-drug interactions among healthcare professionals and patients in Lebanon.
Objective
The study aims to investigate the level of knowledge and understanding of herbal interactions and conventional medications among Lebanese patients. Moreover, the study will examine the Lebanese patients’ awareness, perception towards Herbal Drug Interactions (HDIs) and the role of pharmacists in patient education and information provided about herbal medicine.
Methods
A cross-sectional, descriptive study was performed from March to May 2023 consisting of Lebanese outpatients (General Population and Athletes) aged 20 years and older at Lebanese community pharmacies who agreed to respond to the survey questionnaire from medications, sociodemographic and clinical characteristics were collected from patients via face-to-face Interviews, and a well-structured survey questionnaire administered to a representative sample of Lebanese patients to gather data via Online Google Platform Surveys. All these calculations are performed using Statistical Package for the Social Sciences Software (SAS), SAS Institute. Descriptive statistics are used to describe independent variables. One-Way ANOVA analysis followed by a t-test (binary logistic regression) was performed to identify factors associated with HDI(s).
Results
The results of this study provide valuable insights into the current state of awareness and highlight areas for improving patient education regarding herbal-drug interactions, which included 501 patients, with a mean age of 50.248 years, 53.1% of them being female 58.9% and males 41.1%. The category of Lebanese patients who consumed Herbal medications during the last 12 months accounted for 46.7% and advising others to take herbal medication, 47.9%, versus patients who don’t consume herbal medications 53.3%. Lebanese patients get their recommendation for herbal medication use from mass media such as TV, ads, social media (32.3%), pharmacist (21.6%), family members with friends and neighbours (19%), personal reading/ Internet search (13.6%), didn’t get any recommendation (10.8%), Herbalist (9.8%), and Physician (7.4%).
Conclusion
The study provides valuable insights into the awareness of herbal-drug interactions and the need for understanding these interactions among professionals and patients where various factors affect negatively the unauthorized use of herbal products such as the economic crisis in Lebanon which negatively affected the purchasing power of Lebanese patients to buy their conventional medications, the affordable prices of herbal medications, and the reputation of folk medicine practiced by ancestors.
1. INTRODUCTION
Herbal medicine is considered the oldest type of therapy for preventing or treating diseases [1]. Medicine history was initiated from herbal medicine itself, and this initial study and knowledge bloomed from the Middle East and Europe [2]. Nowadays, this type of medicine is known as complementary and alternative medicine (CAM) in most countries [3]. Recently, the use of CAM has increased worldwide in the past decade. Herbal medicine presents a crucial healthcare methodology in various traditional cultures [4], where the use of herbal medicine maybe the only form of medicine that is available for such a population [5]. Recently, the World Health Organization estimated that 80% of people worldwide rely on herbal medicines as part of their primary health care [6]. Despite the high prevalence of public use of herbs, still, fewer than half of patients who use CAM typically discuss it with their clinician or even seek a pharmacist’s advice [7, 8].
Many reasons have led to the tremendous use of herbal medicine among Lebanese patients [8]. It has vast availability in the market as an over-the-counter product, it is cost-effective and is safe and effective. Excessive consumption of herbal medicine was also reported in Gulf countries, where 74% of respondents in Saudi Arabia sought a herbalist, spiritual healers, or honeybee providers for medical reasons [9]. Kuwaiti population in similar studies has shown a very high prevalence of natural herbal medicine use, even without a doctor’s consultation [10]. Patients are usually convinced that herbal products are safer than synthetic products “if herbs are not effective, at least they are non-toxic” [11, 12]. Still, this is not 100% guaranteed, where herbal products are not regulated by quality control validations [13], and the dispensed active ingredient is not pure in case the extraction of the raw plant is not efficient or complete [12]. In addition to this issue, the Lebanese market lacks the regulatory process of herbal medicine distribution, where many products may contain additives, excipients, and contaminants that are not labelled on the product [14].
Previously, many articles have assessed the inter- actions between herbal medicine and conventional drugs [1]. These articles have revealed that concurrent use of herbal products with conventional medications can lead to interactions that may affect drug efficacy and safety [15]. The word Herb-drug interaction (HDI) was found in the year 2000, which includes examples such as bleeding occurring due to combining Gingko with warfarin or cardiac arrhythmia upon mixing digoxin with St. John’s wort and so many other unlimited fatal sequala [16]. The Phyto vigilance of drug-plant interactions is complicated due to numerous factors like the patient’s comorbid conditions, pharmacogenomic variations, and poly- pharmacy [11]. On the other hand, Phyto vigilance studies have elaborated on several causes of drug-plant interactions, such as multiple botanical constituents, mis- identification of therapeutic dose, mislabelling, and contamination [17, 18]. Thus, information regarding herb–drug interactions is potentially problematic, especially in critical cases such as cardiovascular illness, breast cancer and patients with kidney diseases [19-21]. Yet, as we move toward integrating patient-centered treatment, a detailed understanding of herb-drug interactions is required to optimize the benefits of favorable interactions while avoiding the dangers of potentially dangerous combination [22].
Although many studies have indicated a high degree of interest in alternative medicine among the public worldwide, the level of herbal knowledge and skills concerning the interactions is not adequately discovered in patients and pharmacists. The pharmacist’s role in providing the proper counselling and educating the patient about the appropriate administration, dosing, and specific herbal drug requirements was not stated before. The objective of this study was to determine the Lebanese patients’ awareness, perception towards HDIs and the role of pharmacists in giving full consultation and information on herbal medicine use. This study addresses the potential risks associated with the concurrent use of herbal medicines and conventional drugs, and it emphasizes the need for effective strategies and a comprehensive database to predict and understand herb-drug interactions.
2. METHODS
The study protocol was approved by the Institutional Review Board of the Lebanese International University (2023RC-006-LIUSOP). The collection and processing of the data in this study complied with data protection and privacy. This cross-sectional descriptive study was performed from March until May 2023.
Participants who accepted to fill the questionnaire were interviewed during their visit to a community pharmacy. Patients who are eligible to fill the questionnaire should be older than 20 years of age. Each participant should report any medical condition and must specify the conventional medications they are taking. This latter section was demonstrated to assess the participants’ knowledge about herbal medicine, the practice they adopt, especially with respect to their conventional therapies, and their attitudes towards safety, efficacy, and herbal products' effectiveness in treating diseases and relieving clinical symptoms.
The questionnaire included several sections: socio- demographic status, past medical history, past medication history, and herbal products section. The first carried the details about the patient’s gender, age, height and weight, nationality, area of residence, educational level, work status, marital status, monthly income, and the availability of health insurance contracts. In the past medical history, the questions were asked to collect data about the surgical history, comorbidities, reason for clinical visits or physician’s call, numbers of clinical visits over a year, lab evaluation’s documents in the last 12 months, and the medications prescribed by the physician or even taken as over the counter remedies. The herbal products section has included all the details about patient’s knowledge and competence towards herbal products benefits, adverse effects, risks of toxicity, herbal-drug interactions, and disease-herbs interactions. It also included the patient’s perspectives and attitude towards herbal products, their use, the purpose for the use, their proper administration, their accurate dose measurement, the need for spacing between herbal products and conventional therapy, along with any specific considerations. By the end of the questionnaire, the participants were asked if the prescriber or the pharmacist had educated them about the use, the benefits, and the expected onset of action or the expected side effects.
The statistical analysis and the calculations were performed using Statistical Package for the Social Sciences Software (SPSS), SAS Institute. Descriptive statistics used to describe independent variables. One-Way ANOVA analysis followed by t-test (binary logistic regression) was performed to identify factors associated with HDI(s). Estimating the Lebanese Population size in 2023 is around 5,353,930 [23], with the power to provide a 95% confidence interval [24]. So, for all the previous clues, it has been shown that the recommended minimal sample size we should consider is 384. Categorical variables were reported using numbers and percentages, whereas continuous variables were presented using means (M) and standard deviations (SD). The association of HIDs with each Lebanese patient’s demographic and clinical characteristics was tested using Tukey’s range test to find means that are significantly different from each other, Pearson’s test for categorical variables, One-Way ANOVA analysis followed by T-test for continuous variables. All variables in the bivariate analysis with a p-value <0.05 were included in the logistic regression model unless they were strongly correlated. Therefore, the binary logistic regression allowed the assessment of relationships between binary dependent variable (consuming herbal medications use/not consuming herbal medications), the usage patterns of different types of herbal products or supplements and the current usage of conventional treatment. Thus, it was possible to identify the significant contributing factors to HDIs.
| Characteristic | Frequency (%) |
|---|---|
| Ages | - |
| 20-30 | 183 (36.5%) |
| 30-40 | 80 (15.9%) |
| 40-50 | 76 (15.1%) |
| +50 | 96 (19.1%) |
| Sex | - |
| Male | 206 (41.1%) |
| Female | 295 (58.9%) |
| Nationality | - |
| Lebanese | 444 (88.6%) |
| Non-Lebanese | 57 (11.4%) |
| Area of residence | - |
| Bekaa | 61 (12.2%) |
| Mount Lebanon | 133 (26.5%) |
| Beirut | 178 (35.5%) |
| South | 76 (15.2%) |
| North | 53 (10.6%) |
| Type of residence | - |
| Urban | 363 (72.5%) |
| Rural | 138 (27.5%) |
| Educational level | - |
| Primary Education | 23 (4.6%) |
| High School | 57 (11.4%) |
| University | 421 (84%) |
| Work Status | - |
| Healthcare provider | 180 (35.9%) |
| Non-healthcare provider | 321 (64.1%) |
| Marital status | - |
| Single | 285 (56.9%) |
| Married | 166 (33.1%) |
| Divorced | 41 (8.2%) |
| Widowed | 9 (1.8%) |
| Monthly income | - |
| Less than $ 100 | 171 (34.1%) |
| $100-$500 | 199 (39.7%) |
| $600-$1000 | 87 (17.3%) |
| More than $1000 | 44 (8.8%) |
| Health insurance | - |
| NSSF | 134 (26.7%) |
| COOP | 48 (9.6%) |
| Private | 150 (29.9%) |
| Army | 28 (5.6%) |
| None | 132 (26.3%) |
| Smoking status | - |
| Yes, current smoker | 280 (55.9%) |
| Yes, previous smoker | 41 (8.2%) |
| No, not a smoker | 180 (35.9%) |
| Alcohol consumption | - |
| Yes, current alcohol consumer | 114 (22.8%) |
| Yes, Previous alcohol consumer | 34 (6.8%) |
| No, I don't consume alcohol | 353 (70.5%) |
| Lifestyle | - |
| Healthy and Active | 192 (38.3%) |
| Sedentary | 309 (61.7%) |
| Do you have difficulty in sleeping? | - |
| Yes | 274 (54.7%) |
| No | 227 (45.3%) |
| Are you athletic? | - |
| Yes | 210 (41.9%) |
| No | 291 (58.1%) |
| Do you have Frequent visits to Physicians? | - |
| When needed | 323 (64.5%) |
| Periodically | 62 (12.4%) |
| Never | 323 (64.5%) |
| Do you have Frequent visits to pharmacies? | - |
| When needed | 346 (69.1%) |
| Periodically | 60 (12%) |
| Never | 95 (19%) |
| How many times you do lab tests? | - |
| When needed | 323 (64.5%) |
| Periodically | 94 (18.8%) |
| Never | 84 (16.8%) |
| Have you ever been tested for herbal substance in your blood tests? | - |
| Yes | 106 (21.2%) |
| No | 395 (78.8%) |
3. RESULTS
The questionnaire was filled by 501 Lebanese participants and was distributed over 5 governates of Lebanon (Beirut, Mount Lebanon, South, North, and Beqaa). Most of the participants were females 58.9%, 45.9% of participants aged between 20 and 30 years of age, 55.9% were smokers and 70.5% were non-alcoholic consumers. 35.5% of participants live in the Capital of Beirut, Lebanon, and 61.7% of participants reported a sedentary lifestyle and 54.7% had difficulty in sleeping. Other subjective data were included in the sociodemographic domain, such as monthly income and marital status (Table 1).
3.1. Herbal Usage and Herbal- Drug Interactions (HDIs) related Knowledge
46.7% of the population documented that they consumed herbal medications during the last 12 months. These medications were used as supplements, remedies and prophylaxis. 33% individuals used herbal medications as cold remedies, 30% used other herbal products for gastrointestinal disorders such as abdominal cramps, flatulence, and nausea, 20% of respondents used herbal products to boost energy or to improve sexual desire and libido. Some medications were prescribed during a physician’s visit, while other drugs were recommended as OTC products for self-treatable illnesses such as constipation and diarrhea. Whereas, 27% of participants have consumed herbal products for constipation and 29% have taken herbal products to treat diarrhea. In this study, we have categorized the answers of the patients between consumers of herbal products available in community pharmacies with precise doses and labelled instructions from patients who consider herbal products can be consumed from natural food products found in Lebanese kitchens such as flavourings and spices (Table 2).
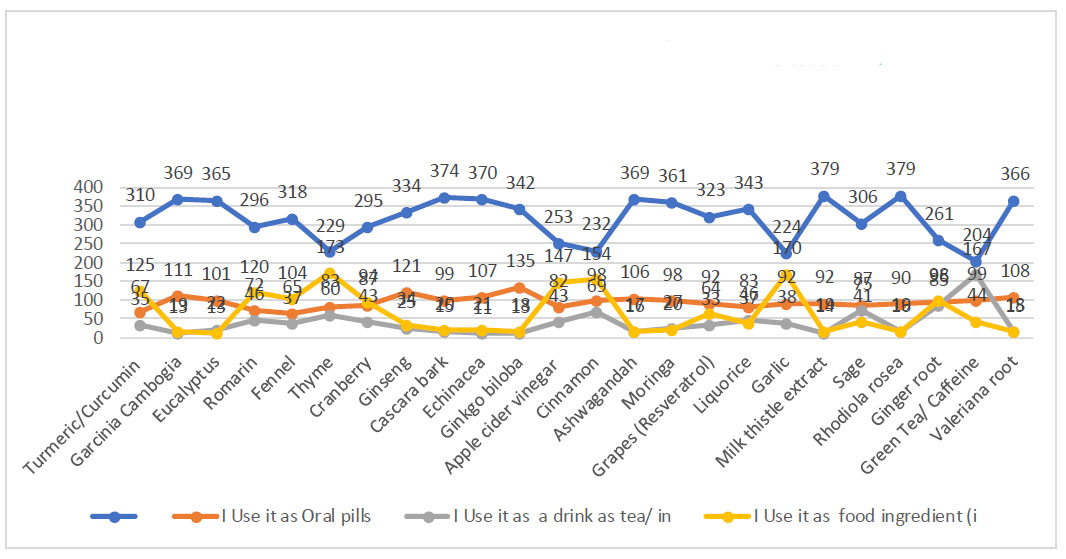
While questioning the participants about the source of information regarding the use of herbal supplements or herbal products used in food, 32.3% of them considered that social media (TV, Instagram, Facebook, and reels) is the best resource of information, and only 7.4% participants take herbal medicine or natural flavourings if recommended by the physician. Herbal products used in preparing food were plenty. The participants documented the use of variable types of flavourings and seasonings such as thyme (Thymus vulgaris, 34.53%), garlic (Allium sativum, 33.93%), cinnamon (Cinnamomum verum, 30.73%), Apple Cider Vinegar (Acetic acid, 30.73%), Curcumin or Turmeric (Curcuma longa, 24.95%), Romarin or Rosemary (Salvia Rosmarinus, 23.95%), while herbal medications as oral pills used by them were Ginkgo biloba (26.94%), Panax Ginseng (Panax quinquefolius L, 24.15%), Garcinia cambogia (Garcinia gummi-gutta, 22.15%), Valeriana (Valeriana officinalis, 21.55%), Echinacea (Echinacea purpurea, 21.35%), and Ashwagandha (Withania somnifera, 21.15%) (Figs. 1-4).
| Uses of Herbal Products by Lebanese Patients | Yes, I use it as a herbal supplement medication N (%) |
Yes, I use it in food N (%) |
No, I don’t use it N (%) |
|---|---|---|---|
| Treatment of dermatologic conditions | 133 (26.54%) | 92 (18.36%) | 276 (55.08%) |
| Treatment of hypertension | 104 (20.75%) | 91 (18.16%) | 306 (61.07%) |
| Treatment of diabetes | 77 (15.36%) | 127 (25.34%) | 297 (59.28%) |
| Treatment of kidney diseases | 119 (23.75%) | 84 (16.76%) | 298 (59.48%) |
| Treatment of gynecological diseases or sexual problems | 109 (21.75%) | 107 (21.35%) | 285 (56.88%) |
| Treatment of gastric problems | 154 (30.73%) | 128 (25.54%) | 219 (43.71%) |
| Supportive for weight gain | 108 (21.55%) | 111 (22.15%) | 282 (56.28%) |
| Supportive for weight loss | 123 (24.55%) | 130 (25.94%) | 248 (49.50%) |
| Supportive as aphrodisiac | 100 (19.96%) | 104 (20.75%) | 297 (59.28%) |
| Supportive for constipation relief issues | 141(28.14%) | 132 (26.34%) | 228 (45.50%) |
| Supportive for diarrhea relief issues | 129 (25.74%) | 145 (28.94%) | 227 (45.30%) |
| Supportive for relieving or killing pain | 141 (28.14%) | 130 (25.94%) | 230 (45.90%) |
| Protection from common cold/flu | 165 (32.93%) | 134 (26.74%) | 202 (40.31%) |
| Protection from alopecia or dandruff | 136 (27.14%) | 116 (23.15%) | 249 (49.70%) |
| Protection from infections | 134 (26.74%) | 121 (24.15%) | 246 (49.10%) |
| Protection from dyslipidemia and cardiovascular disease | 129 (25.74%) | 100 (19.96%) | 272 (54.29%) |
| Protection from osteoporosis | 125 (24.95%) | 105 (20.95%) | 271 (54.09%) |
| Relaxation from insomnia | 137 (27.34%) | 124 (24.75%) | 240 (47.90%) |
| Relaxation from depression | 137 (27.34%) | 107 (21.35%) | 257 (51.29%) |
| Relaxation from muscle spasms | 142 (28.34%) | 109 (21.75%) | 250 (49.90%) |
| Energy booster: increase energy and endurance | 145 (28.94%) | 114 (22.75%) | 242 (48.30%) |
| Energy booster: improving athletic performance | 129 (25.74%) | 114 (22.75%) | 258 (51.49%) |
| Energy booster: not being detected in blood tests | 120 (23.95%) | 116 (23.15%) | 265 (52.89%) |
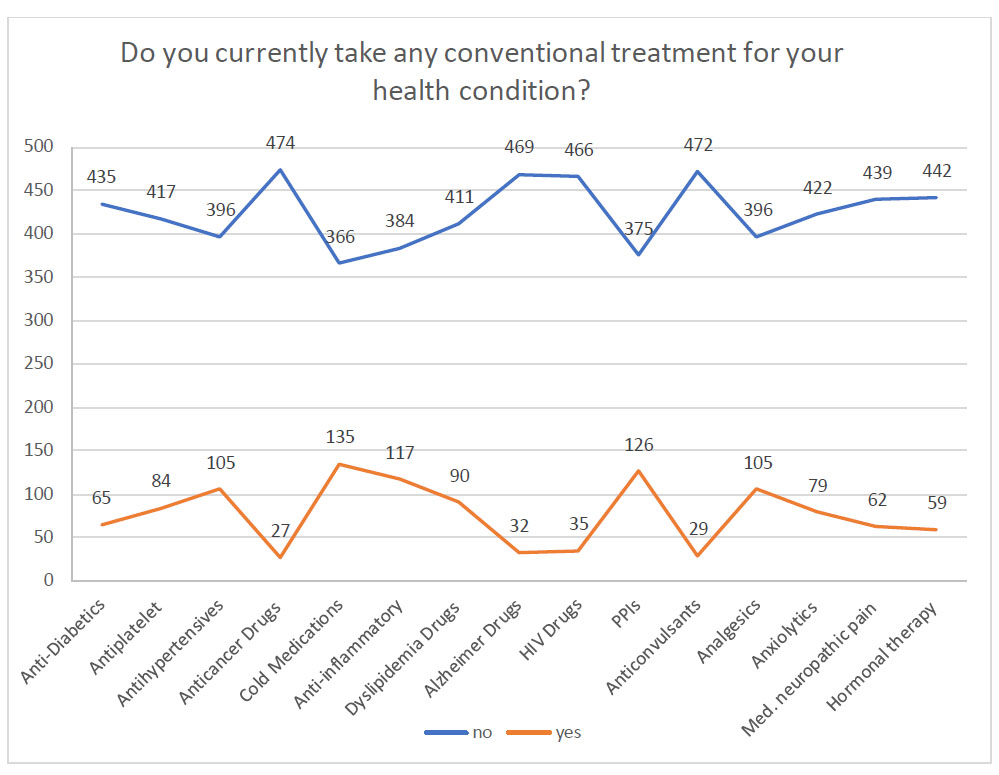
Distribution of Lebanese patients according to their conventional medical treatment
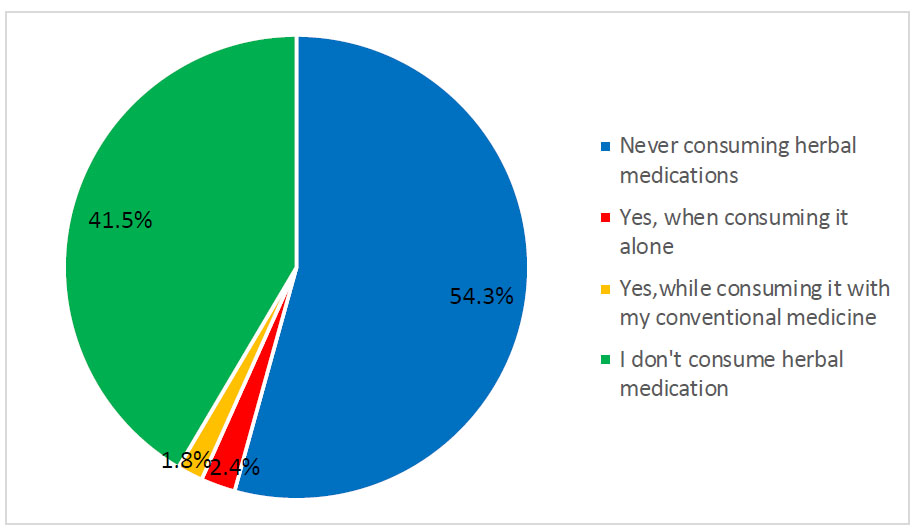
Adverse events after consuming herbal medications by Lebanese patients during the last 12 months.
Furthermore, 54.3% of Lebanese patients did not experience any of adverse events or side effects when consuming herbal plants or medication alone, while 2.4% admit that they experienced adverse events when consuming herbal plants or medication alone. On the other hand, 1.8% experienced adverse events when consuming it with their conventional medication.
Finally, 38.52% of Lebanese patients agree that natural and herbal medicine have side effects, 35.12% of Lebanese patients neither agree nor disagree that natural medicine is more effective than conventional therapy, while 33.93% agree that natural medicine is more effective than conventional therapy, as illustrated in Fig. (2).
In addition, 46.10% of Lebanese patients agree that herbal medicines are beneficial in healthcare management, and 40.71% of Lebanese patients agree that herbal supplements should be used as a substitute for medications after proper sports training, nutrition, and recovery practices. 37.32% of Lebanese patients agree, while 30.73% neither agree nor disagree that herbal supplements can interact with other medications and supplements that you may be taking, 44.51% of Lebanese patients agree that there is scientific research that supports the use of herbal supplements. 37.52% of Lebanese patients agree and 35.92% neither agree nor disagree that there are potential long-term health effects of taking herbal supplements, with 32.93% agreeing that the use of herbal supplements or herbal plants should be limited only to patients who have failed conventional therapy.
Furthermore, 32.93% agree that herbal medicine is safer than conventional medicine, 39.32% of Lebanese patients agree that they are aware of the potential risks and side effects associated with herbal supplements or plants they used, 36.72% of Lebanese patients agree that they know which exact daily amount or dose of herbal plant or herbal supplement they should take for their condition, 40.51% of Lebanese patients agree that when taking any conventional medication along with herbal supplement, the herbal supplement and conventional medication may interact together, 41.91% of Lebanese patients agree that herbal supplements should be regulated and controlled by the Ministry of Health and regulatory bodies to ensure safety and efficacy, 40.71% of Lebanese patients agree that there is a need for education about the risks and benefits of herbal addressed to the general population, 41.51% of Lebanese patients agree that herbal supplements got a health protective effect, 43.71% of Lebanese patients agree that herbal supplements got a disease curative effect, 38.32% of Lebanese patients agree that herbal supplements or herbal plants do not provide treatment, but can only be supportive and treatment is provided only with conventional medicines.
Moreover, 29.34% agree that herbal supplements or herbal plants have no side effects, 38.72% of Lebanese patients agree that herbal supplements or herbal plants do not interact with drugs and can be used at the same time. 38.12% of Lebanese patients agree that the use of herbal supplements or herbal plants can be dangerous, as they will affect the action of existing drug therapy. 37.12% of Lebanese patients agree that herbal supplements or herbal plants can be used as a last option to treat diseases, 33.53% of Lebanese patients agree that it is worth trying herbal supplements or herbal plants before visiting the physician, 37.32% agree that herbal supplements or herbal plants should not be used in the treatment of serious diseases, 41.71% of Lebanese patients agree that herbal supplements can be taken as a desire to boost energy and endurance. 31.73% agree that herbal supplements can help increase sports performance without being detected in blood tests, 42.51% of Lebanese patients agree that they should ask any pharmacist or physician about any herbal supplement or herbal plant before using it alone or with conventional treatment. 41.12% of Lebanese agree that they should investigate the ingredients and dosage of herbal supplements on the internet before taking them, and 44.11% of Lebanese patients agree that they should purchase their herbal supplements from a source, like a certified sports coach or a pharmacy. 44.51% of Lebanese patients agree that they would like to receive consultancy on herbal supplements or herbal plants to know more about how they act and interact in their bodies. 35.52% of Lebanese patients neither agree nor disagree that they would purchase herbal supplements from an online source or herbalist.
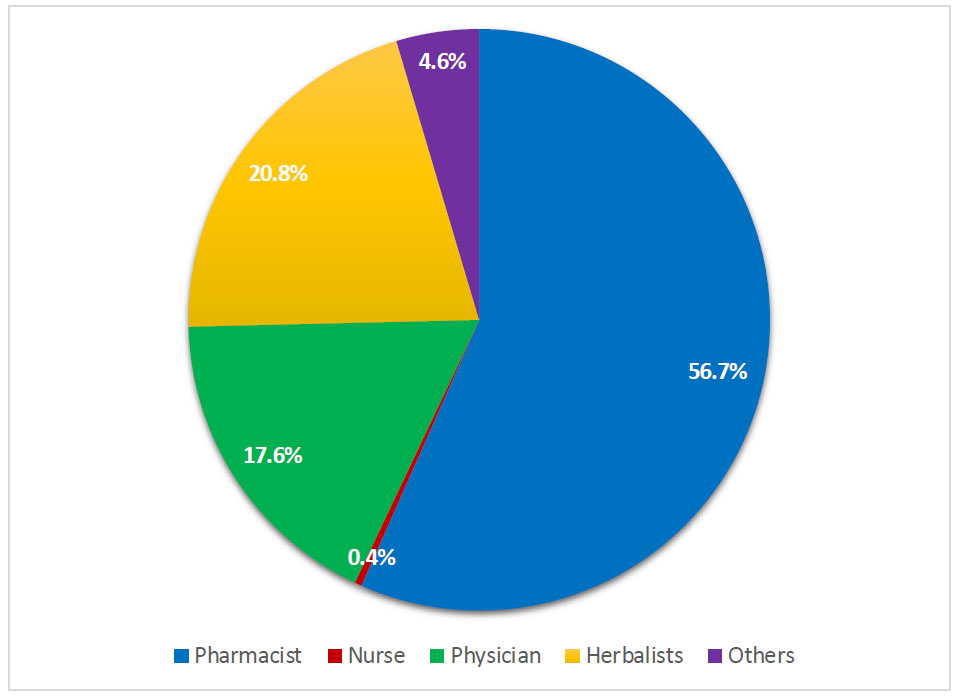
These results show that 56.7% of Lebanese patients consider that the pharmacist should provide complete information about herbal plant or herbal supplement and its usage with conventional medication While 20.8% of Lebanese patients consider the herbalist as the provider source of information about herbal plant or herbal supplement and its usage with conventional medication, 17% consider the physician and 0.4% consider the nurse, while 4.6% consider others, as illustrated by Fig. (3).
Source of herbal medicine recommendation.
Types of herbal products used by Lebanese out patients.
4. DISCUSSION
The results of this study have shown that 46.7% of participants consume herbal products and herbal supplements. In this study, we noticed that approximately half of the participants are more aware of the risks and the benefits of herbal supplements, and they can be an efficient part of the healthcare strategies to prevent HIDs in the Lebanese population.
29.1% of Lebanese patients didn’t ask a healthcare provider about herbal product usage and side effects [25, 26] as manyparticipants in this study were younger ageing between 25 and 30 years. Patients at high risk for HDIs who also take drugs with low therapeutic efficiency should be monitored more closely for herb-drug interactions, especially when a new drug is added or discontinued [27].
The overall prevalence of HDIs among Lebanese patients can occur due to the use of herbal products either in food, such as thyme-anticoagulants or antiplatelet drugs, which slows blood clotting and causes a risk of bruising and bleeding [28], Garlic-Anticoagulant/ Antiplatelet (warfarin/ aspirin) developed platelet disorders and/or hemorrhage [29] Figs. (1 and 3). So, patients using warfarin should be extremely cautious regarding the possible risk of increased bleeding with ingestion of garlic. Garlic-analgesics (paracetamol) causes changes in paracetamol pharmacokinetics [30]. Cinnamon-antihypertensives interaction which potentiates the effect of antihypertensive drug and causes hypotension [31], Cinnamon-analgesics/dyslipidaemia drugs can increase the risk of liver damage [32], Cinnamon-antidiabetics can cause hypoglycaemia [33], Apple cider vinegar can cause Antihypertensive (Furosemide) which increases the effect of Furosemide causing a decrease in potassium levels [34]. Curcumin/turmeric-anticoagulant (Fluindione) increases the risk of bleeding [35], and Romarin/rosemary-antihypertensives (Hydrochlorothiazide/ furosemide) increases hydrochlorothiazide and furosemide clearance [36]. The use of immunity/energy boosters with various medications can present various HDIs such as Ginkgo biloba - PPIs (Omeprazole), which decrease omeprazole blood concentration [37], Ginkgo biloba - Ibuprofen causes death due to cerebral haemorrhage (Inhibition of platelet aggregation) [38], and Ginkgo biloba - anticoagulant (warfarin) increases warfarin levels [39]. Ginseng-Anticoagulant (warfarin) increases anticoagulant effect [40], Ginseng- Insulin which has a synergistic action, increases insulin effects [41]. Ginseng- anxiolytic (Midazolam) reduces the effect of midazolam [37], Garcinia Cambogia -Antidiabetics causes hypoglycaemia [42], and Garcinia Cambogia- anticoagulants/antiplatelet drugs slows blood clotting that increases the risk of bruising and bleeding [43].
Oral herbal products, which are mainly used due to their sedative and relaxant effects may also interact extensively. Such oral herbal products are Valeriana root- Alprazolam/Benzodiazepines/Narcotics which increase sedative effects of Alprazolam [44], Ashwagandha-Benzodiazepines/Anticonvulsants/Barbiturates which increase sedative effects of benzodiazepines and narcotics [45], and Ashwagandha-Warfarin, clopidogrel which increases the risk of bleeding [16, 28]. Other herbal drinks such as Caffeine/Green tea may reduce Folic acid absorption and plasma levels [46]. Green tea may increase the risk of bleeding in patients taking warfarin [47]. Moreover, green tea/EGCG interacts with boronic acid-based agents such as the anticancer drug bortezomib, an approved proteasome inhibitor, where the therapeutic effect of bortezomib and other boronic acid-based proteasome inhibitors involve inhibiting the transport of irinotecan and its metabolite SN-38 during biliary elimination, leading to prolonged half-life and a potential increase in toxicity. Additionally, these inhibitors reduce the absorption of OATP drugs/substrates (such as etoposide and irinotecan) and enhance the bioavailability of tamoxifen [48].
Ginger root- antihypertensives (Nifedipine), which potentiates antiplatelet effects of nifedipine [49], Sage- anticoagulant/antiplatelet (Warfarin/ Clopidogrel), which increases anticoagulant effect of warfarin and reduces plasma levels of clopidogrel [50].
There are studies investigating the awareness and knowledge of herbal products by patients and pharmacists in various medical branches and health records [51, 52]. However, there is no study in Lebanon evaluating the use of herbal products by Lebanese patients in terms of the examination of Pharmacokinetics and Pharmacodynamics of HDIs. In addition, this study will contribute to the development of effective strategies for patient education and healthcare professionals to enable healthcare providers to deliver better guidance and advice regarding HDIs for their patients. This can positively affect the treatment process of the patients, as well as lead to lower dangerous consequences in terms of drug interactions and side effects. Considering herbal products as completely safe and self-management without health care provider guidance may cause negative consequences as some plants may have toxic components, and many herbal products also interact with drugs.
The most commonly known Herb-drug interaction by Lebanese participants is garlic or green tea with warfarin, in which both can alter blood haemostasis and anticoagulation of warfarin. This interaction can be obviously observed with Lebanese patients since 33.33% of Lebanese patients consume caffeine/ green tea and 33.93% consume garlic as herbal product in food, and 16.76% use anticoagulant or platelet as a conventional treatment. For this reason, it is necessary to raise awareness among Lebanese patients and pharmacists in order to provide the best treatment conditions and to prevent possible damages. It is extremely important for healthcare professionals to have comprehensive training in phytotherapy and to have sufficient knowledge and skills to enhance treatment effectiveness and prevent unwanted adverse effects. One of the most important issues regarding the use of herbal products is the information source through which the patients can obtain their knowledge about these products. In general, it is observed that 29.1% of Lebanese patients do not consult their doctors about this issue. In our study, 41.12% of the patients stated that they did research before using herbal products. So, by this step, they consider that the internet and social media are fast and reliable resources of information.
In this study, 28.14% of the Lebanese patients stated that herbal supplements or herbal plants do not interact with drugs and can be used at the same time, but 11.57% of the remaining patients disagreed with this view and 38.72% of them remained undecided. These results actually suggest that patients do not have enough information about toxic plants or their inappropriate use. Similarly, in the present study, 32.93% of the participants agreed with the aspect that the use of herbal supplements or herbal plants should be limited only to patients who have failed conventional therapy, while 12.17% of them disagreed and 33.93% of them were ignorant. These results suggest that some patients consider herbal products quite safe and ignore the possible side effects. However, the use of complementary therapies and herbal products in patients taking conventional medications for long term or chronic diseases should be used under medical supervision.
Regarding participants’ positive attitudes towards the knowledge of pharmacokinetics and pharmacodynamics of herbal products, most of them have shown a good knowledge of this issue (Table 3). The results of our study have shown that 39.32% of respondents are aware of the potential risks and side effects associated with herbal supplements or plants they use, 36.72% of Lebanese patients know the daily amount or dose of herbal plant or herbal supplement should be taken for their condition, 40.51% of Lebanese patients are knowledgeable of the effects occurring with the use of other conventional medication, 41.91% of the study respondents have agreed that herbal supplements should be regulated and controlled by the Ministry of Public Health (MOPH) and regulatory bodies to ensure safety and efficacy. On the other hand, 38.12% of participants agree that herbal supplements or herbal plants do not provide treatment but can only be supportive and treatment is provided only with conventional medicines. Whereas, 38.12% agree that the use of herbal supplements or herbal plants can be dangerous, as they will affect the current drug medical treatments, 37.32% of participants agree that herbal supplements or herbal plants should not be used in the treatment of serious diseases.
| General Attitudes and Behaviors towards Herbal Medications | Strongly Agree n (%) | Agree n (%) | Neutral n (%) |
Disagree n (%) |
Strongly Disagree n (%) |
|---|---|---|---|---|---|
| Natural and herbal medicine have side effects | 119 (23.75%) | 193 (38.52%) | 147 (29.34%) | 31 (6.18%) | 11 (2.19%) |
| Natural medicine is more effective than conventional therapy. | 89 (17.76%) | 170 (33.93%) | 176 (35.12%) | 46 (9.18%) | 20 (3.99%) |
| Herbal medicines are beneficial in healthcare management. | 117 (23.35%) | 231 (46.10%) | 133 (26.54%) | 15 (2.99%) | 5 (0.99%) |
| Herbal supplements should be used after sports and physical training | 99 (19.76%) | 204 (40.71%) | 136 (27.14%) | 42 (8.38%) | 20 (3.99%) |
| Herbal supplements interact with conventional medications and vitamins | 128 (25.54%) | 187 (37.32%) | 154 (30.73%) | 20 (3.99%) | 12 (2.39%) |
| There are potential long-term health effects of taking herbal supplements. | 97 (19.36%) | 188 (37.52%) | 180 (35.92%) | 23 (4.59%) | 13 (2.59%) |
| Herbal medicine is given only if patient’s failed conventional therapy | 78 (15.56%) | 165 (32.93%) | 170 (33.93%) | 61 (12.17%) | 27 (5.38%) |
| Herbal medicine is safer than conventional medicine. | 100 (19.96%) | 165 (32.93%) | 176 (35.12%) | 40 (7.98%) | 20 (3.99%) |
| I know the side effects of herbal medicine and their potential risk | 94 (18.76%) | 197 (39.32%) | 178 (35.52%) | 21 (4.19%) | 11 (2.19%) |
| I know the correct dose, administration of herbal products and supplements | 85 (16.96%) | 184 (36.72%) | 179 (35.72%) | 33 (6.58%) | 20 (3.99%) |
| Herbal-conventional interactions always occur even with spacing | 106 (21.15%) | 203 (40.51%) | 164 (32.73%) | 16 ((3.19%) | 12 (2.39%) |
| Herbal supplements are regulated by the government | 157 (31.33%) | 210 (41.91%) | 112 (22.35%) | 12 (2.39%) | 10 (1.99%) |
| Pharmacist education about herbal medicine is necessary | 172 (34.33%) | 204 (40.71%) | 107 (21.35%) | 10 (1.99%) | 8 (1.59%) |
| Herbal therapy is always beneficial with no adverse effects | 100 (19.96%) | 208 (41.51%) | 166 (33.13%) | 18 (3.59%) | 9 (1.79%) |
| Herbal supplements got a disease curative effect. | 87 (17.36%) | 219 (43.71%) | 162 (32.33%) | 24 (4.79%) | 9 (1.79%) |
| Herbal medicine has synergistic effect along with conventional therapy | 97 (19.36%) | 192 (38.32%) | 164 (32.73%) | 39 (7.78%) | 9 (1.79%) |
| Herbal-conventional interaction may be fatal and life threatening | 97 (19.36%) | 191 (38.12%) | 165 (32.93%) | 30 (5.98%) | 18 (3.59%) |
| I try herbal medicine before visiting the doctor | 89 (17.76%) | 168 (33.53%) | 160 (31.93%) | 58 (11.57%) | 26 (5.18%) |
| Herbal medicine is not used in critical ill patients or series illness | 96 (19.16%) | 187 (37.32%) | 159 (31.73%) | 38 (7.58%) | 21 (4.19%) |
| Herbal supplements may boost immunity, energy, and libido | 92 (18.36%) | 209 (41.71%) | 171 (34.13%) | 20 (3.99%) | 9 (1.79%) |
| Herbal medicine has no plasma level detecting test | 96 (19.61%) | 159 (31.73%) | 188 (37.52%) | 37 (7.38%) | 21 (4.19%) |
| I ask the pharmacist or the physician about herbal medicine profile | 136 (27.14%) | 213 (42.51%) | 126 (25.14%) | 19 (3.79%) | 7 (1.39%) |
| I search for the benefits and the risk of herbal medicine by internet | 105 (20.95%) | 202 (41.12%) | 152 (30.33%) | 27 (5.38%) | 15 (2.99%) |
| I purchase herbal supplements from an online source, pharmacy, sports coach, herbalist | 76 (15.16%) | 148 (29.54%) | 178 (35.52%) | 52 (10.37%) | 47 (9.38%) |
Lebanese patients are willing to be more educated about herbal products use since 40.71% of Lebanese patients agree that there is a need for education about the risks and benefits of herbal supplements, and 42.51% of Lebanese patients ask pharmacists or physicians about herbal supplements or herbal plant before buying, 41.12% of Lebanese patients research the ingredients and dosage of herbal supplements on the internet before taking them, 44.51% of Lebanese patients like to receive consultancy on herbal supplement or herbal plants.
Another study concerning the knowledge of athletes about herbal products shows that 17% of college female athletes have used herbal supplements such as” “Guarana”, “Ashwagandha”, “Caffeine”, “Purple Willow Bark”, “Cayenne”, “Pepper”, and “Ginger root”. These products were believed to increase mental vigilance, stimulate fat-burning metabolism, and improve muscle performance [53]. Other plants such as Tribulus terrestris, Ginkgo biloba, Rhodiola rosea, and Cordyceps sinensis have demonstrated benefits on muscle growth and strength in active men, while others have shown no effect on muscle performances. Whereas, in this study, 28.94% Lebanese patients and especially the athletes, use these herbal supplements, mostly the Ashwagandha (21.15%), ginger root (16.96%), caffeine/green tea (33.33%) as energy boosters in order to increase energy and endurance, and 28.34% for relaxation from muscle spasms after sport exercises and 41.71% agree that herbal supplements can be taken as a desire to boost energy and endurance. Also 31.73% agree that herbal supplements can help increase sports performance without being detected in blood tests. Moreover, Ashwagandha can cause false positive results in benzodiazepine, thyroxine, digoxin drug tests, which can trigger false positive results that may affect certain lab test results [54].
Moreover, in the literature, the authors discuss the pharmacists’ knowledge, their experience of patient - reporting adverse reactions and their awareness of these reactions could play a vital role in identifying and reporting these reactions [51, 55]. The results of our study have shown significant similarities with previous studies and literature. Community pharmacists were not aware of potential herb–drug interactions, and an even larger majority did not receive complaints from the patients about herbal medicines. Thus, we recommend strategies taken by the Lebanese Ministry of Public Health (MOPH), Lebanese Hospitals, and Lebanese Pharmaceutical Companies to prevent or minimize the incidence of HIDs in society by raising awareness of pharmacists which will positively affect patients’ knowledge and correct herbal medicine practice.
In contrast to the literature, 56.7% of Lebanese patients get their source of information about herbal plants or supplements and their usage with conventional medication, while only 20.7% of Lebanese patients refer to the herbalist. Moreover, in this study, 44.11% of patients’ first choice was to purchase herbal supplements from pharmacies or certified sports coaches. Meanwhile, a lower percentage were inclined to purchase from an online source or herbalist as a second and alternate choice. Take into consideration that previous studies have shown that the primary consultant for herbal medicine use is the pharmacist only [56]. This reflects the trust of Lebanese patients towards their pharmacists, so pharmacists need enhanced education on pharmacokinetic and pharmacodynamics mechanisms, drug metabolizing enzymes, and transporters playing significant roles in herb-drug mechanisms in order to provide objective and evidence-based information on the benefits and risks of herbal medicines which might affect the general knowledge and awareness of the targeted population for better patient care and benefit in the future. Patient education and healthcare professionals play a crucial role in raising awareness and providing guidance on herb-drug interactions. The study highlights the high prevalence of herbal product use in Lebanon, driven by factors such as the unaffordability of synthetic medications and the economic crisis. The research aims to assess Lebanese patients' awareness and perception of herb-drug interactions and the role of pharmacists in providing consultation and information on herbal medicine use.
CONCLUSION
The study provides valuable insights into the awareness of herbal-drug interactions and the need for understanding these interactions among professionals and patients. Where various factors negatively affect the unauthorized use of herbal products, such as the economic crisis in Lebanon, which negatively affected the purchasing power of Lebanese patients to buy their conventional medications, the affordable prices of herbal medications, and the reputation of folk medicine practiced by ancestors. This study addresses athlete’s mindsets about herbal product use as well as shed light on developing effective strategies taken by the Lebanese Ministry of Public Health (MOPH), Lebanese Hospitals, and Lebanese Pharmaceutical Companies to prevent or minimize the incidence of HIDs among Athletes and Lebanese Population. Therefore, it is important to give credit to patient education and healthcare professionals in order to enable healthcare providers to deliver better awareness, guidance and advice regarding HDIs for their patients. Finally, more comprehensive studies should be conducted examining the benefit and harm profiles of herbal products among the Lebanese population.
AUTHORS’ CONTRIBUTION
M.A., R.B.: Study conception and design; R.Al-M.: Data collection: R.Al-M., M.A.: Analysis and interpretation of results; S.N., J.A.: Draft manuscript:
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol was approved by the Institutional Review Board of the Lebanese International University, Lebanon (2023RC-006-LIUSOP).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The collection and processing of the data in this study complied with data protection and privacy. This cross-sectional descriptive study was performed from March until May 2023 from participants who accepted to fill the questionnaire and were interviewed during their visit to a community pharmacy.
ACKNOWLEDGEMENTS
We would like to thank all the Lebanese pharmacists in community pharmacies for their help in passing the surveys and data entry. We would also like to thank all the doctors in the School of Pharmacy at Lebanese International University for their vital assistance throughout this study.


