All published articles of this journal are available on ScienceDirect.
Midwives’ Experience with the 2020 WHO Labor Care Guide in Rural Hospital Settings: Usability, Feasibility, Acceptability, and Satisfaction
Abstract
Introduction
It is recommended by the World Health Organization (WHO) that partographs be used to monitor every delivery. A partograph is a low-cost and simple tool designed to provide continuous data on the labor process and is used to predict the progress of labor and improve results. The next-generation partograph, known as The WHO Labor Care Guide (LCG), was released by the WHO in December 2020. The new highlights of LCG were documentation using numerical figures, specific threshold limits that would initiate intervention, and supportive maternal care.
Objectives
This study aimed to evaluate the usability, feasibility, acceptability, and satisfaction of midwives using WHO LCG in rural practice.
Methods
This study adopted a mixed-method design, with the quantitative phase using a questionnaire and the qualitative phase using interviews, to evaluate midwives' usability, feasibility, acceptability, and satisfaction with the WHO LCG. During February to April 2024, research data were gathered from three rural hospitals. The distribution and characteristics of midwives and patients were identified using descriptive data analysis, and the results are presented in the tables. Data from the interviews are also reported.
Results
Data were collected from 41 midwives in three rural hospitals. Midwives observed labor in 123 patients using LCG. According to the questionnaire, 49.6% of the midwives were satisfied with the use of LCG, 65% were satisfied with how LCG was designed, and 68.3% thought LCG was useful. According to the midwives' interviews, the LCG design was detailed; however, in its implementation, the midwives agreed that more time, information, and effective communication were needed to complete it.
Conclusion
The LCG design is perceived as more detailed and easier to complete; however, midwives are still adjusting to the new format, thus requiring frequent training. In addition, prompt cooperative decision-making requires excellent communication between obstetricians, midwives, patients, and families.
1. INTRODUCTION
Delivery complications account for almost one-third of maternal deaths, half of stillbirths, and over a quarter of newborn mortalities [1]. The majority of these can be avoided or minimized if women have access to adequate prenatal, intrapartum, and postpartum care. Enhancing early detection and management of labor monitoring can prevent unfavorable outcomes [2, 3].
In Indonesia, midwives currently handle 68.6% of maternity services provided during childbirth. According to the midwife's scope of practice, a midwife must be accountable and responsible for giving respect, guidance, and support to women throughout their pregnancies, deliveries, and postpartum period. Midwives have a critical role in lowering maternal and neonatal mortality as well as enhancing the health of expectant mothers, newborns, and children [4, 5].
A partograph is a low-cost and simple tool for observing the labor process. It includes important details regarding fetal, maternal, and labor status. The World Health Organization (WHO) recommends that all laboring mothers utilize the partograph as a monitoring tool. Despite that recommendation, partograph is still not widely used in developing countries because of several challenges, including a shortage of human resources, time limitations, partograph paper shortages, and the know- ledge, attitude, and skills of midwives [3, 6-8].
The next generation partograph, known as the WHO Labor Care Guide (LCG), was released by WHO in 2020. The LCG is different from previous partograph designs in that it focuses on the mother's safety, concerns the duration of labor, and indicates when clinical interventions are required. The LCG sections include identity infor- mation and labor characteristics on admission, supportive care, care for the baby, care for the woman, labor progress, medication, and shared decision-making. The tool aims to promote collaborative decision-making between women and healthcare professionals to enhance women-centered care [9-12].
It is expected that medical practitioners may become uncomfortable with the new partograph, considering that the previous form of the partograph has been used in Indonesia for quite a long time. Therefore, the acceptance of Indonesian health workers, especially midwives, regarding WHO LCG needs to be considered. This study aimed to evaluate the usability, feasibility, acceptability, and satisfaction of midwives using WHO LCG in rural practice. The results of this study can depict the obstacles to WHO LCG implementation and provide inputs regarding improvements that can be made based on rural practices in Indonesia.
2. METHODS
This study adopted a mixed-method design: a quantitative phase that used a questionnaire and a quali- tative phase that used interviews. This project was conducted from February 2024 to April 2024 in the Maternity Room and Emergency Room of Obstetrics and Gynecology at three rural hospitals. The study was conducted in humans according to the Helsinki Decla- ration of 1975, as revised in 2013. This study was approved by the Ethical Committee of the Faculty of Medicine, Universitas Indonesia (ethics number KET-346/ UN2.F1/ETIK/PPM.00.02/2024) and all the participants provided informed consent. A research flowchart is shown in Fig. (1).
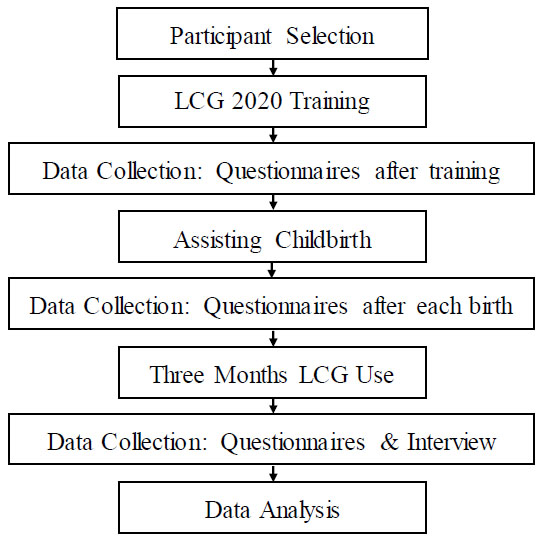
Research flow chart.
2.1. Participants
The participants in this study were midwives who provided childbirth care to low-risk mothers. A consecutive sampling procedure was used to select participants with a minimum sample size of 31.
2.2. Data Collection
Midwives who participated in this study received training in utilizing LCG. Following the training, they provided the first questionnaire to explore their perceptions of the training and the Labor Care Guide training manual. Midwives were then requested to use LCG when assisting childbirth in low-risk mothers, and they were given questionnaires after each birth regarding their satisfaction with using the LCG. After three months of using LCG, the midwives will be given questionnaires regarding their satisfaction and their opinions of each component in the LCG, and then they will be interviewed by SI regarding their perspectives on the LCG 2020.
3. RESULTS
3.1. Quantitative Findings
This study involved 41 midwives from three rural hospitals as participants (Table 1). In addition to the training instructions on how to complete the LCG, participants were also given a questionnaire regarding their responses to the training and their readiness to use the LCG after the training. Of the 41 participants, 70.8% indicated that they thought the training was helpful, and 51.2% claimed they were ready to use LCG in assisting childbirth. In addition, it was discovered from the questionnaire that 65.8% of participants thought the training manual helped them understand the LCG (Table 2).
| Characteristics | Hospital A | Hospital B | Hospital C | Total | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| Professional role | ||||||||
| Midwife | 15 | 36.5 | 17 | 41.5 | 9 | 22 | 41 | 100 |
| Number of years of clinical care provision in labor | ||||||||
| ≤1 year | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1-5 years | 1 | 6.7 | 4 | 23.5 | 0 | 0 | 5 | 12.2 |
| ≥5 years | 14 | 93.3 | 13 | 76.5 | 9 | 100 | 36 | 87.8 |
| Gender | ||||||||
| Male | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Female | 15 | 100 | 17 | 100 | 9 | 100 | 41 | 100 |
| Variable | Hospital A | Hospital B | Hospital C | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| I found overall the training using the Labor Care Guide to be useful | Strongly disagree | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Disagree | 2 | 13.3 | 2 | 11.8 | 0 | 0 | 4 | 9.8 | |
| Neutral | 3 | 20 | 3 | 17.6 | 2 | 22.2 | 8 | 19.4 | |
| Agree | 9 | 60 | 10 | 58.8 | 6 | 66.7 | 25 | 61 | |
| Strongly agree | 1 | 6.7 | 2 | 11.8 | 1 | 11.1 | 4 | 9.8 | |
| I feel capable of using the Labor Care Guide in the labor ward | Strongly disagree | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Disagree | 2 | 13.3 | 2 | 11.8 | 1 | 11.2 | 5 | 12.2 | |
| Neutral | 5 | 33.3 | 6 | 35.2 | 4 | 44.4 | 15 | 36.6 | |
| Agree | 7 | 46.7 | 8 | 47.1 | 4 | 44.4 | 19 | 46.3 | |
| Strongly agree | 1 | 6.7 | 1 | 5.9 | 0 | 0 | 2 | 4.9 | |
| I found the Labor Care Guide training book useful | Strongly disagree | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Disagree | 1 | 6.7 | 1 | 5.9 | 1 | 11.1 | 3 | 7.4 | |
| Neutral | 4 | 26.7 | 4 | 23.5 | 3 | 33.3 | 11 | 26.8 | |
| Agree | 7 | 46.6 | 8 | 47.1 | 4 | 44.5 | 19 | 46.3 | |
| Strongly agree | 3 | 20 | 4 | 23.5 | 1 | 11.1 | 8 | 19.5 | |
Table 3.
| Characteristics | N | % |
|---|---|---|
| Maternal age (years) | ||
| 18-24 | 54 | 43.9 |
| 25-30 | 35 | 28.5 |
| 31-34 | 26 | 21.1 |
| Others | 8 | 6.5 |
| Parity | ||
| 0 | 57 | 46.3 |
| 1-2 | 56 | 45.5 |
| ≥3 | 10 | 8.2 |
| Mode of delivery | ||
| Vaginal delivery | 114 | 92.7 |
| Assisted vaginal delivery | 0 | 0 |
| Cesarean section | 9 | 7.3 |
| Sex of baby | ||
| Male | 41 | 33.3 |
| Female | 82 | 66.7 |
| Vital status at birth | ||
| Live birth | 123 | 100 |
| Stillbirth | 0 | 0 |
| Apgar score at 5 minutes | ||
| <7 | 29 | 23.6 |
| ≥7 | 94 | 76.4 |
| Birthweight | ||
| <2500 gram | 14 | 11.4 |
| 2500-4000 gram | 109 | 88.6 |
Table 4.
| Variable | Hospital | ||
|---|---|---|---|
|
A N (%) |
B N (%) |
C N (%) |
|
| I was able to use LCG to manage labor and childbirth | |||
| Strongly disagree | 0 (0) |
2 (3.9) |
0 (0) |
| Disagree | 3 (6.8) |
2 (3.9) |
3 (11.1) |
| Neutral | 11 (24.4) |
18 (35.4) |
14 (41.9) |
| Agree | 29 (64.4) |
25 (49) |
9 (33.3) |
| Strongly agree | 2 (4.4) |
4 (7.8) |
1 (3.7) |
| I was able to complete LCG correctly | |||
| Strongly disagree | 0 (0) |
0 (0) |
0 (0) |
| Disagree | 1 (2.2) |
6 (11.7) |
2 (7.4) |
| Neutral | 14 (31.1) |
18 (35.3) |
8 (29.6) |
| Agree | 26 (57.8) |
24 (47.1) |
15 (55.6) |
| Strongly agree | 4 (8.9) |
3 (5.9) |
2 (7.4) |
| I was satisfied with the LCG in this woman’s labor and childbirth management. | |||
| Strongly disagree | 0 (0) |
1 (2) |
0 (0) |
| Disagree | 3 (6.7) |
2 (3.9) |
2 (7.4) |
| Neutral | 18 (40) |
23 (45.1) |
12 (44.4) |
| Agree | 18 (42.2) |
17 (33.3) |
12 (44.4) |
| Strongly agree | 5 (11.1) |
8 (15.7) |
1 (3.8) |
| The LCG was helpful in managing this woman’s labor and childbirth | |||
| Strongly disagree | 0 (0) |
0 (0) |
0 (0) |
| Disagree | 1 (2.2) |
3 (5.9) |
2 (7.4) |
| Neutral | 13 (28.9) |
23 (45.1) |
8 (29.6) |
| Agree | 27 (60) |
24 (37.1) |
16 (59.3) |
| Strongly agree | 4 (8.9) |
1 (2) |
1 (3.7) |
| Overall, I am satisfied with the current LCG design. | |||
| Strongly disagree | 0 (0) |
0 (0) |
0 (0) |
| Disagree | 2 (4.4) |
4 (7.8) |
2 (7.4) |
| Neutral | 18 (40) |
19 (37.3) |
9 (33.4) |
| Agree | 32 (46.7) |
26 (51) |
13 (48.1) |
| Strongly agree | 4 (8.9) |
2 (3.9) |
3 (11.1) |
Over a three-month period, 41 midwives observed 123 low-risk births using LCG. Most of them were primiparas (46.3%), and those aged 18–24 years had the highest average maternal age (43.9%). In most cases, 92.7% of births were vaginally delivered, while 7.3% required a cesarean section. No maternal or newborn deaths occurred during the study period. Up to 76.4% of newborns had an Apgar score of greater than seven, and up to 88.6% weighed >2500 grams (Table 3).
From the questionnaire that was completed each time a participant assisted in delivering a baby using LCG, the majority of midwives (56.9%) believed they could manage labor with LCG, and 60.2% thought that they could complete the LCG correctly. Up to 49.6% of participants reported satisfaction with LCG use, and 59.3% thought it helped to observe childbirth. Additionally, it was discovered through this questionnaire that 65% of the participants were satisfied with the LCG design (Table 4).
Participants were given a questionnaire regarding their opinions on each component in the LCG design at the end of the study period (Table 5). Sections one and three had the highest values among the eight current components (73.2%). Meanwhile, the labor progress section (Section 5) has the lowest value (53.7%). Additionally, a questionnaire called the System Usability Score (SUS) was distributed after the study to evaluate the usability score of the LCG. The results showed that 68.3% of participants thought that LCG was helpful.
3.2. Qualitative Findings
Midwives from the three hospitals were questioned about their thoughts on the use of LCG. In the midwives' opinion, the LCG sheet had a more detailed design than the preceding partograph. This facilitates observation, allowing for more stringent monitoring and quicker decision-making if obstacles are discovered. Additionally, consensus among obstetricians, midwives, patients, and families is paramount; decisions are made collaboratively and harmoniously. Overall, midwives felt that the LCG design was simpler to complete than earlier partographs because it employed numbers instead of graphs or images. The LCG design helps in the process of changing duty hours between birth attendants because the patient's condition and the therapy they have received are listed on a single sheet.
However, midwives also mentioned the challenges they encountered when utilizing LCG. Despite becoming accustomed to the new structure and acknowledging the need for ongoing training, midwives still encounter difficulties completing the LCG. While decisions can be made more rapidly when patient concerns are discovered, in practice, midwives handle an unpredictable number of patients at once, which makes close monitoring and real-time LCG sheet filling challenging.
In addition, it was discovered that decision-making necessitated communication through an intermediary. This involved the transmission of decisions from the patient to the midwife, from the midwife to the obstetricians, and the provision of advice from the obstetricians to the family via the midwife, preceding the family’s deliberation on whether to accept or reject the proposed treatment plan. Given that a typical patient is accompanied by multiple family members, deliberation time is essential for reaching a decision. While midwives’ competence has traditionally been used to assist with normal childbirths without complications, in reality, many patients admitted to the hospital for delivery already present with complications and often require immediate intervention. In the absence of any danger or action thresholds on the LCG sheet, all interventions are dependent on real-time monitoring findings and shared decision-making, which is why the completion of LCG truly requires effective communication between midwives and obstetricians.
| Variable | N | % | |
|---|---|---|---|
| I am satisfied with the Identification section (Section 1) of the Labor Care Guide | Strongly disagree | 0 | 0 |
| Disagree | 0 | 0 | |
| Neutral | 11 | 26.8 | |
| Agree | 22 | 53.7 | |
| Strongly agree | 8 | 19.5 | |
| I am satisfied with the Supportive Care section (Section 2) of the Labor Care Guide. | Strongly disagree | 0 | 0 |
| Disagree | 0 | 0 | |
| Neutral | 12 | 29.3 | |
| Agree | 24 | 58.5 | |
| Strongly agree | 5 | 12.2 | |
| I am satisfied with the Baby section (Section 3) of the Labor Care Guide | Strongly disagree | 0 | 0 |
| Disagree | 0 | 0 | |
| Neutral | 11 | 26.8 | |
| Agree | 25 | 61 | |
| Strongly agree | 5 | 12.2 | |
| I am satisfied with the Mother section (Section 4) of the Labor Care Guide | Strongly disagree | 0 | 0 |
| Disagree | 0 | 0 | |
| Neutral | 14 | 34.1 | |
| Agree | 23 | 56.1 | |
| Strongly agree | 4 | 9.8 | |
| I am satisfied with the Labor Progress section (Section 5) of the Labor Care Guide | Strongly disagree | 0 | 0 |
| Disagree | 0 | 0 | |
| Neutral | 19 | 46.3 | |
| Agree | 20 | 48.8 | |
| Strongly agree | 2 | 4.9 | |
| I am satisfied with the Medication section (Section 6) of the Labor Care Guide | Strongly disagree | 0 | 0 |
| Disagree | 0 | 0 | |
| Neutral | 13 | 31.7 | |
| Agree | 22 | 53.7 | |
| Strongly agree | 6 | 14.6 | |
| I am satisfied with the Shared Decision-making section (Section 7) of the Labor Care Guide | Strongly disagree | 0 | 0 |
| Disagree | 0 | 0 | |
| Neutral | 11 | 26.8 | |
| Agree | 24 | 58.5 | |
| Strongly agree | 6 | 14.7 | |
| I am satisfied with the Birth Outcome section (Section 8) of the Labor Care Guide | Strongly disagree | 0 | 0 |
| Disagree | 0 | 0 | |
| Neutral | 13 | 31.7 | |
| Agree | 25 | 61 | |
| Strongly agree | 3 | 7.3 | |
| Overall, I am satisfied with the current design of the Labor Care Guide | Strongly disagree | 0 | 0 |
| Disagree | 0 | 0 | |
| Neutral | 9 | 22 | |
| Agree | 24 | 58.5 | |
| Strongly agree | 8 | 19.5 | |
4. DISCUSSION
In this study, quantitative and qualitative data were collected from 41 midwives in three rural hospitals. For three months, midwives observed labor in 123 patients using a new partograph sheet called LCG, with 92.7% delivering their babies normally. According to the results of this study, 51.2% of participants believed they could utilize LCG to assist with childbirth after receiving training, and 70.8% of participants found the training helpful. Insights from using older partograph designs can guide WHO LCG implementation. Understanding varied implementation approaches in diverse contexts is crucial for success [13-16].
According to the questionnaire administered to participants after each birth, 49.6% of midwives were satisfied with the utilization of LCG, and 65% were satisfied with their design. These findings align with those of a study in Uganda, which shows that healthcare professionals are eager to use LCG. These are detailed, comprehensive, and tailored to their needs. It can reduce over documentation and also requires minimal additional training [17].
The LCG consists of eight filling sections. Based on the questionnaire that was distributed, it was discovered that the identification section (Section 1) and the baby monitoring section (Section 3) received the highest scores (73%), while the progress section (Section 5) received the lowest scores (53.7%). Upon completion of the trial, midwives were provided with the SUS questionnaire that assessed the utility of the LCG. The results indicated that 68.3% of midwives thought that LCG was useful. The LCG made them more able to provide individualised care, a finding that is similar to a qualitative study from Sub-Saharan Africa [18-20].
Although 68.3% of midwives found the LCG useful, the satisfaction rates with its usage (49.6%) and design (65%) indicated room for improvement. This suggests that the tool's practical application may not fully meet the midwives' expectations, leading to mixed levels of acceptance.
Following the collection of survey data, interviews were conducted with several midwives to learn more about their perspectives, benefits, and challenges related to the use of the LCG sheets. Midwives thought that the LCG sheet was easier to fill out and more detailed overall than the partograph sheet. However, this poses a challenge. More time is needed to complete more thorough monitoring, and there are situations when there are insufficient midwives to handle the burden in the field. In line with the previous mixed-methods study by Vogel et al., eliminating the alert and action line demands that midwives acquire more knowledge and requires continuous communication with obstetricians, patients, and their families when making decisions based on problems encountered [10].
According to midwives' feedback, the implementation of the LCG required additional time, which could be a significant limitation, especially in busy rural settings where midwives are already overburdened with patient care responsibilities. This study indicated that midwives needed more information and support to use LCG effectively. This finding suggests that inadequate training on how to use the tool may hinder its successful adoption.
This is the first study to evaluate midwives’ experiences with the 2020 WHO Labour Care Guide in a rural hospital setting in Indonesia. Although we included 41 midwives from three rural hospitals with a minimum sample size of 31, we realized that a larger and more diverse sample from different geographical areas would provide a broader understanding of midwives' acceptance and application of the WHO LCG. This study also relied on interviews for qualitative data, which are subjective and may be influenced by individual bias. Midwives’ perspectives could be shaped by personal preferences or experiences, which might not reflect broader trends in rural healthcare settings.
Future studies should consider the role of training in improving LCG use. Effective communication has been highlighted as a barrier to the successful implementation of LCG. Communication issues between healthcare teams can affect the tool's usability and patient care outcomes. This limitation highlights the need for better communication protocols in healthcare settings where LCG is used.
CONCLUSION
The LCG design is perceived as more detailed and easier to complete; however, midwives are still adjusting to the new format, thus requiring frequent training. In addition, prompt cooperative decision-making requires excellent communication between obstetricians, midwives, patients, and families.
AUTHORS’ CONTRIBUTIONS
S.A, B.S: Contributed to study conception and design; S.I: Contributed to data collection; S.A., S.I., B.S., and O.A.M: Contributed to analysis and interpretation of results; S.A., S.I., I.P.G, and A.P.: Drafted the manuscript.
LIST OF ABBREVIATIONS
| WHO | = World Health Organization |
| LCG | = Labor Care Guide |
| SUS | = System Usability Score |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethical Committee of the Faculty of Medicine, Universitas Indonesia (ethics number KET-346/UN2.F1/ETIK/PPM.00.02/2024).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.


