All published articles of this journal are available on ScienceDirect.
Parental Perspectives on Childhood Fever and Antipyretics: A Cross-sectional Study on Knowledge, Attitudes, and Beliefs in Bekaa Valley
Abstract
Background
Fever in children is one of the most common reasons for seeking pediatric medical care. Many parents believe that elevation in body temperature is an immune response to illness, while others perceive it as a disease requiring immediate attention. The use of drugs (antipyretics and antibiotics) often presents a significant challenge for parents when assessing the condition of their child. Most of the parents, regardless of their education level, medical background, or previous experience in treating a child with fever, feel very intimidated by underdiagnosed or untreated fever.
Objective
The purpose of this study was to assess parental knowledge and attitude towards fever in children aged 3-5 years and their practice during assessment and treatment.
Methods
A cross-sectional observational study was carried out among Bekaa elementary schools. This study targeted parents through a questionnaire sent to them at home. They were asked to fill out the questionnaire, which included participants’ demographics, knowledge, attitude, and practice regarding fever and drugs. The practice score was calculated using 13 different variables to evaluate the knowledge.
Results
Out of 1300 parents, a total of 808 parents participated in this study; 42.7% of them recognized fever as a body temperature above 38.5ºC, and 28% believed that fever reflects a healthy immune response. Moreover, 65.5% of parents were found to give their children antipyretics when body temperature was below the defined threshold. The calculated median knowledge score was 8. According to bivariate analysis, parents with higher education levels or with medical specialties demonstrated no difference in treating fever from non-educated parents or parents who did not belong to the medical field (P-value: 0.268 and 1, respectively), whereas the age of parents positively affected the knowledge.
Conclusion
In this study, parental knowledge regarding fever was generally acceptable, but it failed to evaluate the impact of knowledge on attitudes and practices. Still, parental awareness regarding fever assessment and management must be carefully addressed by primary caregivers and community pharmacists.
1. INTRODUCTION
Previous studies have established the word fever phobia. Since 1980, parents reported their fright about fever and its consequences if left untreated [1]. Fever is defined as body temperature, by rectal route, exceeding 38.3°C. It is the most common sign of illness that a child represents in the first five years of age and the first reason for pediatrics consultation [2]. Investigators have found that fever phobia ranges from fever that leads to irritability and weakness to major neurological conse- quences like brain damage and convulsions [3].
Some previous literature has documented that all parents, regardless of their health literacy or level of education, face problems in dealing with their feverish child. It is very difficult to know whether a child needs rest and a healthy environment to get better or needs an immediate medical referral [1]. Although parents who have medical specialty answered all the knowledge domains in the surveys correctly, they have reported that they feel powerless towards the illness of their children [1, 2]. This kind of parents may feel that the medication is an unnecessary exposure to drugs, and failure to respond indicates a serious underlying disease [3].
Parents have reported their confusion in treating their child’s condition: when to start with self-treatment and give the medication, when to refer to the physician, and when they can consider treatment failure. All these questions and tens more have raised the conflict towards fever practice and behaviour and widened the definition of fever phobia [2, 3]. Parental behaviour in assessing their children’s condition has been a major concern, in addition to the uncertainty, since parents lack accurate knowledge in recognizing body temperature thresholds and providing the appropriate treatment. On the other hand, dealing with antipyretics and education about the dosing, administration, and available dosage forms have also been addressed [4].
Signs and symptoms accompanied by fever are chills, myalgia, fatigue, anorexia, excessive sleep, tachycardia, tachypnea, headache, and delirium. If left untreated, the patient may develop dehydration, febrile seizures, or even hyperpyrexia [5]. All of these signs have worsened the parental challenge against fever and magnified their fear of it. Underdiagnosed or untreated fever may aggravate the condition. This rests on several factors like a child’s age, diet status and caloric intake, immune system response, as well as the nature of the illness, whether it is caused by infectious disease or due to idiopathic etiology [5, 6].
Body temperature is tested by a thermometer, which can be applied through several routes. Axillary, tympanic, rectal, and oral routes are all used by parents to detect elevated body temperature [7]. Researchers have assessed in previous studies the parent’s best route to recognize body temperature. More than 60% of parents consider rectal measurement to be the “gold standard” since it is the most accurate route. However, it has some disadvantages, such as the risk of bowel perforation if the thermometer is administered improperly [6]. Fever, also called pyrexia, is defined as an increase in the thermoregulatory set point of the hypothalamus caused by inflammatory cytokine. This is achieved by decreasing heat loss with vasoconstriction and producing heat by shivering [8].
Antipyretics are medications that act to lower body temperature. The only approved antipyretics in children are paracetamol, ibuprofen, and diclofenac in their wide dosage forms [9]. They are administered at a body temperature of 38.3°C and are significantly efficacious on high-grade fever [7]. In addition, antipyretics can reduce the duration of fever episodes and alleviate the discomfort of patients [6]. All studies have agreed that these drugs are the cornerstone of the treatment of fever; the faster the recovery, the less risk of developing fever complications like seizures and dehydration [9, 10].
None of the previous studies or guidelines have set recommendations that can help relieve the feeling of threat to parents. All parents reported the presence of some gap in their knowledge with respect to dealing with fever [10], such as how many times they have to take body temperature or what should be the next step in case home remedies have proven insufficient in reducing the body temperature [11]. The parents also reported being unaware of the appropriate time for medical intervention and the safest drug of choice among the different options [10].
Parents who work in the medical field (nurse, physician, pharmacist, etc.) were significantly anxious about their child’s fever, same as parents who have low health literacy [9, 11]. However, parents observed that their concerns about fever lessened or became more focused as they had more children [10]. It has been observed that with repetitive fever episodes and as the family members grow up, the fear of parents lessens, and their behaviour improves, especially in self-care [10, 12].
Regardless of education level, health literacy, and multi-children parents, fever is one of the oldest indicators of diseases and one of the most common causes for seeking medical attention [13].
Studies have reported a lack of counseling tips and efficient time during a pharmacist/physician’s interview with parents, resulting in an exaggeration of parental fear and panic [11, 12].
Parental knowledge about fever and antipyretics and the impact of this knowledge on parental practice toward childhood fever have been assessed. This study also aimed to detect gaps in the current knowledge that can be filled by the healthcare team.
2. METHODS
2.1. Study Design
A cross-sectional study was conducted to investigate parental knowledge, attitudes, and practices towards fever. Participants were parents who have at least one child aged between 3 to 5 years old in schools located in Bekaa, Lebanon. The schools that participated in this study were selected randomly.
2.2. Study Setting
The study was conducted in schools across the Bekaa Valley in Lebanon, which were selected to ensure a large and diverse sample size. The study proposal, along with the questionnaire, was submitted to the administrations of the participating schools. Of the institutions approached, nine private schools and one public school agreed to participate. Questionnaires were then distributed by the schools to the parents of students aged five years or younger, with instructions for the parents to complete and return them. This process took approximately one to two weeks.
The written questionnaire included sociodemographic questions, questions related to knowledge about fever and antipyretics, and attitudes and behaviors during fever episodes. This took place between October, 2018, to January, 2019.
No direct contact or phone call was placed between researchers and parents, and they were notified that their data and the information collected would be presented in the thesis defense, and the results would be published in a scientific journal later on. The study carried no physical, psychological, or social risks, so no intervention was taken. Besides, this study ensured privacy and confi- dentiality, as the participants did not have to provide their names or their children’s names. Moreover, there were no incentives for them.
2.3. Sample Size
A review of existing literature suggested that the targeted sample size was 1000, so 1300 questionnaires were distributed among schools. Eight hundred and eight parents returned the completely filled questionnaire, representing a response rate of 62%.
2.4. Survey Instrument
The adopted questionnaire in the study was developed, validated, and used in previous research. However, it was translated to reflect customs and practices in Lebanon and piloted with a sample of 15 parents, followed by a cross-sectional study in Beirut by Pharm-D students in 2018.
A total of 90 questions related to the study were asked. It also included personal information, such as the age of each parent, nationality, educational level, and if any of them has a medical background or belongs to any healthcare specialty like being a nurse or a doctor or a pharmacist. Also, the parents were asked about the definition of fever, at which body temperature they recognize fever, and the best route of measurement considered by them to test body temperature. The attitude regarding the medical attention they seek in case of fever, the proper administration of antipyretics, and the indication of antibiotics were also asked in this questionnaire. In addition, questions regarding the attitude of parents with respect to other concomitant symptoms, such as if the child is experiencing loss of appetite, presenting with symptoms of dehydration, and feeling irritated and bothered, were also asked. Sections related to knowledge, attitude, and behaviour in the questionnaire were asked in the Arabic language (the Lebanese native language).
The parents in this study were free to express their feelings and worries about the consequences of fever. Response options included yes/no and agree/disagree, along with the Likert scales. In the questionnaire, scales were set to assess the level of satisfaction the parents had during a clinical interview for education and counseling methods. This survey aimed to evaluate the level of adherence to drug therapy, along with the beliefs about the use of antibiotics as adjunctive treatment for fever, even in non-infectious pathology.
2.5. Statistical Analysis
Data was analysed using SPSS V.21.0. Categorical variables were described by the count and proportion of each category. Continuous variables were described by their means and standard deviation (SD) or by their medians and interquartile range (IQR), depending on whether they were normally distributed or not. Crude associations between categorical variables were assessed using Pearson’s chi-square test. P values < 0.05 corresponded to strong evidence [14]. P-values alone do not permit any direct statement about the direction or size of a difference or a relative risk between participants of interest [15].
3. RESULTS
3.1. Participants’ Characteristics
A total of 808 parents completed the questionnaire by either mother or father. Six hundred thirty-two of them had a university degree, and only a few belonged to the medical field (20.2% and 13.5% for mother and father, respectively). The majority of parents were Lebanese (87% mothers and 90.3% fathers), and the others were mentioned as either Arab or non-Arab. Moreover, 10.6% of parents had only one child, 38.4% had 2 children, and the rest had more than 2.
Sociodemographic characteristics are listed in Table 1.
3.2. Parental Knowledge about Fever, Antipyretics, and Antibiotics
Seven hundred ninety-four parents considered a body temperature above 37 °C indicative of a fever, but only 18% of them correctly identified a body temperature of 38.3 °C as indicative of a fever, which aligned with its definition. The majority of participating parents (89.1%, n = 683) were afraid of fever, which may be a leading cause of brain damage, and approximately more than two-thirds (71.3%, n=543) considered fever as a disease by itself.
According to 59.5% of the respondents, fever indicates the presence of infection, and most of them (69.1%) believed that it is caused by bacterial infections compared to viral infections.
| Parameter | Number/ Frequency (%) | |
|---|---|---|
| Age (years) | Mother (n = 771) | Father (n = 750) |
| < 20 | 5 (0.6) | 1 (0.1) |
| 20-25 | 99 (12.8) | 4 (0.5) |
| 26-30 | 194 (25.2) | 51 (6.8) |
| 31-35 | 315 (40.9) | 268 (35.7) |
| 36-40 | 130 (16.9) | 236 (31.5) |
| >40 | 28 (3.6) | 190 (25.4) |
| Nationality | Mother (n = 728) | Father (n = 721) |
| Lebanese | 638 (87.6) | 655 (90.8) |
| Arab | 68 (9.4) | 49 (6.8) |
| Non-Arab | 22 (3) | 17 (2.4) |
| Education | Mother (n = 709) | Father (n = 633) |
| University | 383 (54) | 249 (39.3) |
| High school | 149 (21) | 144 (22.7) |
| Others | 177 (25) | 240 (38) |
| Specialty | Mother (n = 252) | Father (n = 192) |
| Medical | 51 (20.2) | 26 (13.5) |
| Non-Medical | 201 (79.8) | 166 (86.5) |
| How many children do the parents have? (n = 773) |
1 | 82 (10.6) |
| 2 | 298 (38.6) | |
| 3 | 258 (33.4) | |
| 4 | 93 (12) | |
| 5 | 42 (5.4) | |
| Past medical history (any chronic disease) (n = 757) | No | 716 (94.7) |
| Yes | 41(5.3) | |
| Statement | Answer and Number/Frequency (%) | ||
|---|---|---|---|
| - | Agree | Disagree | - |
| Fever might be beneficial for my child’s health (n = 762) | 213 (28) | 543 (71.3) | - |
| I’m afraid fever may lead to brain damage (n = 773) | 683 (89.1) | 82 (10.8) | - |
| - | Yes | No | I don’t know |
| Antibiotics are used to cure infections caused by bacteria (n = 748) | 517(69.1) | 72(9.6) | 165(20.9) |
| Antibiotics are used to cure infections caused by viruses (n = 774) | 324(45.8) | 238(31.9) | 166(22.2) |
| In cases of fever, there is an infection (n = 785) | 451(59.5) | 153(17.8) | 171(22.6) |
| - | Yes | No | - |
| Do you administer medication to your child, like acetaminophen (paracetamol), without consulting the doctor first? (n = 738) |
405(51.7) | 327(47.5) | - |
The levels of knowledge of parents regarding the drugs and their use varied. It was found that 24% of them gave antipyretics to their child at a body temperature of more than 38.3 °C, while 34.3% of them gave antipyretics regardless of their cause and reason. On the other hand, 11.9% of parents did not know whether giving an antibiotic to a feverish child was right or not, and 67.3% of them did not initiate antibiotics for a fever treatment regardless of the cause of the body temperature elevation.
The information on parental knowledge about fever and its medications is mentioned in detail in Table 2.
3.3. Parental Practices of Fever and Antipyretics
Even though paracetamol was found to be the most used antipyretic, only 47% of parents knew the exact interval duration of it (Fig. 1), and almost half of the respondents (51.7%) initiated the medication in feverish children without the consultation of the doctors. More than three-fourths of the participants (81.2%) believed that different dosage forms and alternating between oral and rectal drug administration are beneficial, and 234 (30.7%) of parents combined two different classes of antipyretics. Parental practices toward fever and antipyretics are presented in Fig. (2) and Table 3.
3.4. Parental Attitudes about Fever
It has been reported that 65.9% of parents could distinguish their child’s fever by touching the forehead, and 6.2% believed that touching the skin is enough without any further thermometer measurement. Nonetheless, more than a third of parents (38%) confirmed the illness by administering the thermometer rectally, and others preferred the otic method (20.2%). Most parents (95.1%) could notice the upset and discomfort during their child’s fever illness. Furthermore, 77.9% believed that fever may lead to dehydration, and 89% reported that fever may lead to convulsion (febrile seizure) at a very high temperature. For that, half of the parents (51.4%) measured their feverish child's body temperature 4 to 6 times a day, while those who overreacted towards their child’s fever, i.e., 12.8%, mea- sured it more than 10 times a day.
In this study, the parents were asked about their preferred time for seeking medical consultation and their most trustful source of information among the medical staff. In this regard, 59% indicated that doctors’ advice was the most reliable source of information regarding feverish children, and more than half of the parents (52.8%) considered that asking more than one physician might positively affect their child’s outcome. The details of the parents’ visit to the doctor are presented in Fig. (3).
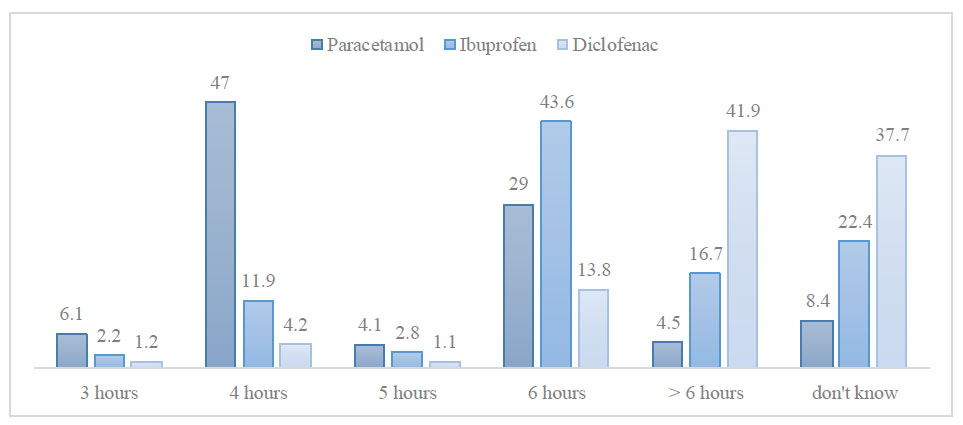
Parental practice towards the interval duration of antipyretics.
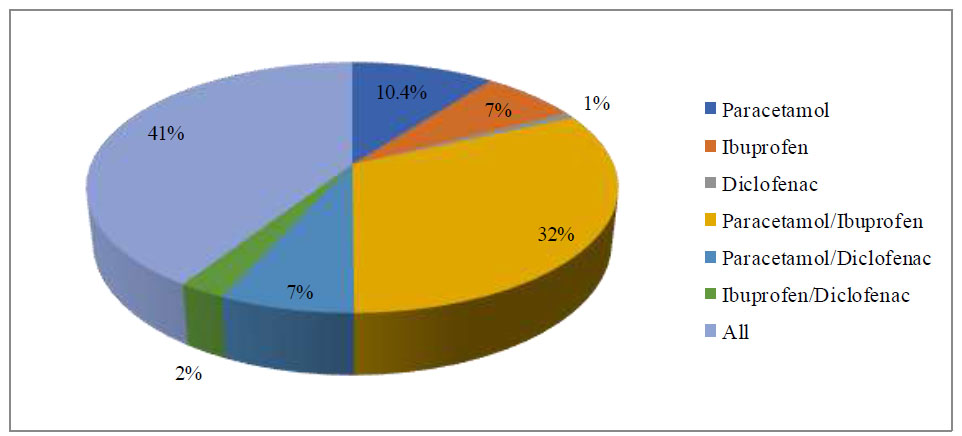
Usage of antipyretics according to the parents.
| - | No | Yes | I don’t know | ||||
|---|---|---|---|---|---|---|---|
| Do you think you can combine two different antipyretics? (n = 760) | 520 (68.4) | 234 (30.8) | 6 (0.8) | ||||
| Is there any difference between the dosage forms? (n = 773) | 145 (18.8) | 628 (81.2) | - | ||||
| Do you think that the dosage form you frequently use is the best choice? (n = 737) | 98 (13.3) | 639 (86.7) | - | ||||
| Please indicate in which cases you visit a general practitioner/family physician with your child. | |||||||
| - | Never | Rarely | Sometimes | Most of the time | Always | ||
| Fever in general (n = 766) | 97 (12.7) | 175 (22.8) | 276 (36) | 105 (13.7) | 113 (14.8) | ||
| When my child has a fever and takes in less fluids (n = 782) | 50 (6.9) | 144 (15.7) | 284 (34.1) | 144 (19.8) | 16 (21.9) | ||
| When my child has a fever and is drowsy (tired) n = 734) |
46 (6.3) | 103 (14) | 216 (29.4) | 148 (20.1) | 221 (30.1) | ||
| When my child has a fever and a skin rash (n = 706) |
45 (6.4) | 38 (5.4) | 65 (9.2) | 134 (19) | 424 (60) | ||
| When my child has a fever and is crying unstoppably (n = 733) | 47 (6.4) | 49 (6.7) | 109 (14.9) | 135 (18.4) | 393 (53.6) | ||
| When my child has a fever and is in pain (n = 759) |
24 (3.2) | 35 (4.6) | 103 (13.6) | 193 (25.4) | 404 (53.2) | ||
| When my child has a fever and is breathing differently (faster or moaning) (n = 749) | 26 (3.4) | 28 (3.7) | 57 (7.6) | 116 (15.5) | 522 (69.8) | ||
| When my child has a fever for more than three days (n = 750) | 14 (1.9) | 41 (5.5) | 25 (3.3) | 56 (7.5) | 614 (81.8) | ||
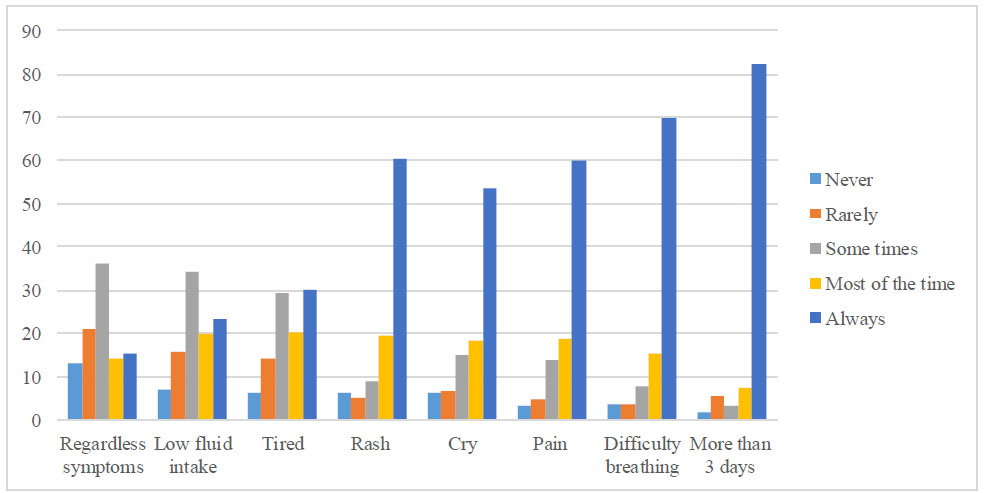
Parents’ visit to the doctor.
On the contrary, the role of the pharmacist seems to be minor among this population, where only 7.6% of the applicants consulted them alone, and 8.8% consulted them along with the doctor. Fig. (4) shows parents’ sources of information regarding fever.
4. DISCUSSION
According to our study, the age of parents positively affected their knowledge of fever. Older mothers correctly identified the cut-off temperature for confirming fever as a body temperature above 38.3 °C compared to younger mothers. Nevertheless, the association between age and knowledge improvement was not statistically significant (P value = 0.681 and P value = 0.444) for mothers and fathers, respectively. The fever cut-off is mentioned in Table 4.
The level of education of the participants and their specialty, whether in medical fields or not, showed no correlation with their knowledge about fever in their children. Moreover, the knowledge of parents regarding fever did not improve with an increase in the number of children (P value = 0.234); for example, 81.6% of those with three children answered incorrectly.
Therefore, parental knowledge or behaviors did not generally correlate with either parental experience or key sociodemographic characteristics.
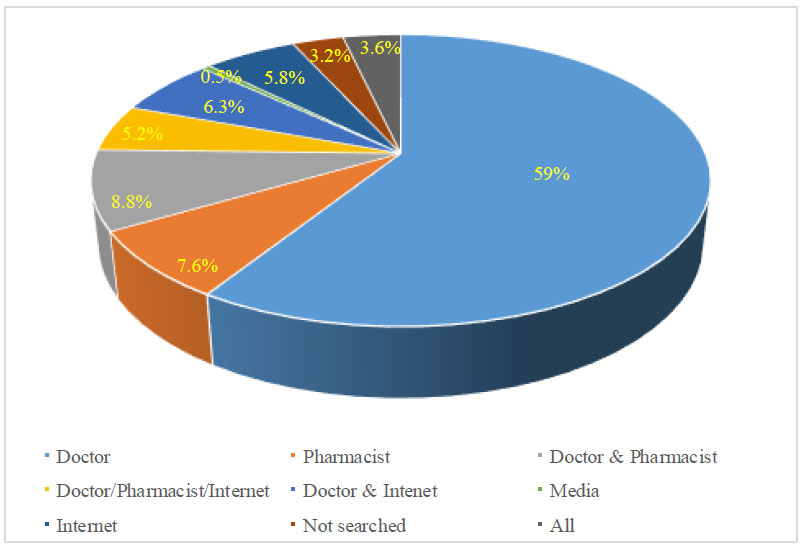
Parents’ sources of information regarding fever.
| - | - | Mother | Father | ||||
|---|---|---|---|---|---|---|---|
| - | - | Incorrect N (%) | Correct N (%) | P-value | Incorrect N (%) | Correct N (%) | P-value |
| Age (years) | < 20 | 4 (0.6) | 0 (0) | 0.681 | 1 (0.2) | 0 (0) | 0.444 |
| 20-25 | 83 (13.3) | 13 (9.7) | 4 (0.6) | 0 (0) | |||
| 26-30 | 157 (25.1) | 33 (24.6) | 40 (6.5) | 8 (6.1) | |||
| 31-35 | 255 (40.7) | 56 (41.8) | 224 (36.4) | 41 (31.3) | |||
| 36-40 | 102 (16.3) | 28 (20.9) | 184 (29.9) | 51 (38.9) | |||
| >40 | 24 (3.8) | 4 (3) | 158 (25.6) | 29 (22.1) | |||
| Education | University | 268 (49.7) | 70 (57.9) | 0.268 | 202 (39.1) | 47 (41.2) | 0.386 |
| High school | 121 (22.4) | 27 (22.3) | 116 (22.5) | 28 (24.6) | |||
| Others | 109 (20.2) | 15 (12.4) | 153 (29.7) | 29 (25.4) | |||
| College | 38 (7.1) | 9 (7.4) | 44 (8.5) | 9 (7.9) | |||
| Specialty | Medical | 40 (78.4) | 11 (21.6) | 1 | 21 (80.8) | 5 (19.2) | 0.807 |
| Non-Medical | 158(78.6) | 43 (21.4) | 130 (78.3) | 36 (21.7) | |||
| Nationality | Lebanese | 518 (81.8) | 115 (18.2) | 0.001 | 531 (81.9) | 117 (18.1) | 0.11 |
| Non-Arab | 60 (92.3) | 5 (7.7) | 45 (91.8) | 4 (8.2) | |||
| Arab | 12 (54.5) | 10 (45.5) | 12 (70.6) | 5 (29.4) | |||
| Number of children | |||||||
| - | Incorrect N (%) | Correct N (%) | P-value | ||||
| 1 | 69 (85.2) | 12 (14.8) | 0.234 | ||||
| 2 | 236 (80.3) | 58 (19.7) | |||||
| 3 | 208 (81.6) | 47 (18.4) | |||||
| 4 | 78 (83.9) | 15 (16.1) | |||||
| 5 | 36 (92.3) | 3 (7.7) | |||||
| Practice Score | Frequency (%) N = 666 (82.5) |
|---|---|
| 0 | 2 (0.3) |
| 1 | 1 (0.2) |
| 2 | 7 (1.1) |
| 3 | 8 (1.2) |
| 4 | 20 (3) |
| 5 | 21 (3.2) |
| 6 | 47 (7.1) |
| 7 | 86 (12.9) |
| 8 | 119 (17.9) |
| 9 | 152 (22.8) |
| 10 | 123 (18.5) |
| 11 | 63 (9.5) |
| 12 | 17 (2.6) |
| 13 | 0 (0) |
Fever, according to 51.9% of the parents, indicates the presence of infection regardless of the pathogens. While 64.1% were aware of the correct use of antibiotics to treat bacterial infections, 42.4% still believed that antibiotics could treat viral ones.
Concerning antipyretics, a third of the participants administered it to their children in case of fever, regardless of the clinical presentation. However, it is important to know the correct dosage of these antipyretics to reduce the risk of overdose or sub therapeutic doses. Understanding the proper time for antipyretic adminis- tration and the duration of action is also essential to properly control the symptoms while minimizing the risk of toxicity and side effects [12]. In this study, 64.4% of parents avoided combining two different classes of drugs to relieve fever, and 77.8% believed that the combination of different dosage forms results in a good outcome. Most of the parents used both syrup and suppositories, and they believed that alternating between oral and rectal administration is a beneficial practice [14]. The use of antipyretics and antibiotics was found to be well understood by parents.
When queried about their medical consultations, a significant majority of parents (two-thirds) opted for doctors, while only a minority favored pharmacists, underscoring the limited involvement of pharmacists within this demographic. It is noteworthy that most parents preferred doctors for advice on their child’s condition even before symptoms manifest, possibly reflecting their concerns and anxieties.
It is crucial to understand that having a good knowledge of fever and recognizing its causes and consequences will directly affect the practice of its prevention and treatment [15]. Practice scores were calculated using 13 variables, including doctors’ consultations, antibiotics and antipyretics duration, combinations, and dosage forms. A high practice score indicated a strong understanding of fever-related information, where the highest score was 12 out of 13, while the majority of participants reported scoring 9 out of 13. Conversely, parents with low practice scores demonstrated a lack of knowledge and provided negative feedback regarding the causes and consequences of fever. Therefore, the approach to managing a feverish child, whether it involves antipyretics, antibiotics, or seeking medical attention, is influenced by a comprehensive understanding of fever as a whole. Practice scores are reported in Table 5.
Parents should be provided with evidence-based information to enhance their awareness and ensure the safety of their children in a format that is understandable and accessible [16, 17]. Obtaining the correct information for parents before their child falls ill, particularly regarding fever and medication use, is one of the most important points that should be prioritized.
Exploring the potential for an intervention to support parents in efficiently managing fever and febrile illnesses in their children should be a focus of future research. Making parents more empowered in the responsible care of their children is crucial for the public health sector.
4.1. Practical Implications
Physician consultations, comments, and education must be well considered during any fever episodes to establish the reason behind the illness and to maximize medical control. On the other hand, the pharmacist's role is complementary to the physician's importance concerning drug use. They allow the parents to be aware of the different types of antipyretics, their proper administration, calibration, the expected side effects, and to be away from the overdose or the sub-therapeutic dose.
The study was conducted prior to the global COVID-19 pandemic.
4.2. Strengths and Limitations of this Study
The large sample size of the participants, who were selected randomly from different sub-regions in Bekaa Valley, with a wide variety of socioeconomic levels, is one of the major strengths of this study. Another strength is the high response rate achieved from the school-based study. The evaluation of parents' attitudes, beliefs, and practices in a non-clinical setting added value and provided more realistic responses.
The limitations of this study were related to the responders themselves. Some participants left many sections unanswered, while others filled it based on their neighbors' or relatives' answers or answered it without having any information, and these factors may reduce the generalizability of the results to the entire population in this region. Additionally, the absence of the oral route as an option in temperature measurement methods excluded one way of assessing feverish children in this study. There was no assessment of actual parental behaviors or practices. Moreover, the exploration of the reasons behind parental knowledge gaps or misconceptions was limited. Furthermore, the importance of pharmacists in the parents’ education was not mentioned.
CONCLUSION
Parental knowledge regarding fever is widely acknowledged; however, it has not adequately assessed how this knowledge influences attitudes and practices. Collaborative efforts between parents and medical professionals, including doctors, pharmacists, and nurses, should be undertaken to achieve the best outcomes in controlling fever, understanding its causes, signs, and symptoms, and dispelling misinformation.
One of the challenges parents face with their children aged five years and younger is a lack of knowledge and practices about fever and misunderstandings of the critical information related to it. Therefore, education provided by primary caregivers and community pharmacists remains the cornerstone for improving parents' knowledge of fever, their awareness regarding fever assessment and management, and correcting their practices related to it.
AUTHORS’ CONTRIBUTION
S.K.: Study conception and design; F.T. and M.A.: Data collection; F.S.: Analysis and interpretation of results; J.W. and M.D.: Article revision; S.N. and F.H.: Draft manuscript.
LIST OF ABBREVIATIONS
| SD | = Standard Deviation |
| IQR | = Interquartile Range |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Ethical and Research Committee at the Lebanese International University, Lebanon under the number 2020ERC-121-LIUSOP.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.


