All published articles of this journal are available on ScienceDirect.
Assessment of Educational Needs of Patients in Clinical Hematology Towards the Implementation of a Structured Therapeutic Education Program
Abstract
Introduction
This study was conducted to assess the knowledge of patients with clinical hematology conditions and determine their educational needs in order to develop an adapted therapeutic education program in the clinical hematology department at Mohammed V Military Instruction Hospital. The objective was to identify areas where patients lack understanding in order to improve their management of the disease.
Objective
The objective of this study is to identify the educational needs of patients in clinical hematology.
Methods
The majority of patients have a good understanding of the essential aspects of their disease and treatment. However, significant gaps remain in understanding aspects related to disease acceptance, pain management, and relational and intimate issues. Patients have expressed a heightened need for information on practical aspects such as biological tests, fatigue management, and diet.
Results
Relational and intimate aspects are often perceived as less prioritized despite their importance. Religious beliefs play a significant role in how patients perceive their illness, with the majority viewing the disease as a form of predetermined fate.
Conclusion
The study highlights the importance of designing a therapeutic education program that addresses the specific needs of patients while considering their priorities and personal beliefs. The results emphasize the need to fill the identified gaps in understanding less addressed aspects of the disease and treatment. Therapeutic education program must be tailored to individual patients' needs to improve their overall management and quality of life.
1. INTRODUCTION
Globally, cancer accounts for 13% of mortality; three-quarters of these deaths occur in low- or middle-income countries, primarily in the poorest regions of sub-Saharan Africa, South Asia, and Latin America. It is considered a major public health problem [1]. In Morocco, cancer accounts for 7.2% of deaths, with 30,500 new cases each year [2].
Clinical hematology is a discipline that manages malignant hematopathies (cancers of the blood, bone marrow, and lymphatic system) characterized by acute and chronic pathologies that evolve slowly. Due to their severity and the challenges posed by comprehensive multidisciplinary management, often in emergency situations, they become a public health problem.
As with all diseases, patients with malignant hematopathies face complex challenges due to the nature of their illness, requiring multidimensional management. Safe and effective treatment, combined with adequate therapeutic education (TEP), is essential to help them better manage their daily lives [3].
Therapeutic patient education (TEP) is an innovative care approach [4] that significantly improves patients' quality of life, relying on a set of similar activities [5]. The WHO estimates that 50% of patients with chronic diseases do not adhere properly to their treatments, leading to increased morbidity and mortality and generating unnecessary healthcare expenses [6, 7]. Thus, according to WHO, “improving patient adherence to chronic treatment can be more beneficial than any biomedical discovery” [8].
In Morocco, TEP remains an unstructured practice. This survey is part of a project aimed at establishing a TEP program in clinical hematology. The goal is to understand the specific educational needs of patients with malignant hematopathies in order to determine the content and educational tools required.
2. METHODS
2.1. Study Type
This is a cross-sectional descriptive study conducted among patients with malignant hematologic disorders being followed up in clinical hematology in Morocco. This type of study allows for an immediate assessment of needs within a clinical context and aims to identify specific educational needs to develop an adapted therapeutic education program.
In order to ensure methodological rigor and transparency in the presentation of results, we have chosen to adopt the STROBE design. This choice helps to reduce potential biases and provides a comprehensive and clear description of the methodology as well as the results while ensuring the reproducibility of the study.
2.2. Study Population
The study includes adult patients (18 years and older) diagnosed with a malignant hematologic disorder, followed in the clinical hematology department of Mohammed V Military Instruction Hospital, both in the conventional and protected wards and in the day hospital. Patients who are in aplasia or newly hospitalized were excluded. Patients must be able to understand and respond to questions asked during interviews or via the questionnaire (Supplementary material).
2.3. Sampling
A convenience sample was used, consisting of 215 patients selected based on their availability and consent. Recruitment took place over a period of 9 months (July 2023 - March 2024), allowing for the collection of a representative sample of patients followed in clinical hematology.
2.4. Data Collection
Data were collected using a structured questionnaire divided into three sections:
2.4.2. General Knowledge about Therapeutic Education
General understanding of therapeutic education, sources of information, perception of the importance of therapeutic education.
2.4.3. Specific Knowledge about the Disease and Treatment
understanding of the disease, the prescribed treatment, and physical and psychological aspects related to the disease.
A 5-point Likert scale was used, where 1 means “Not informed at all” and 5 means “Very well informed”. The questionnaire was administered face-to-face based on patient availability.
2.5. Data Analysis
Data were analyzed quantitatively using SPSS software. Descriptive statistics were used to summarize the sociodemographic characteristics of the participants and their level of knowledge regarding their disease and aspects related to therapeutic education.
2.6. Ethical Considerations
The research was approved by the ethics committee of Biomedical Research, Morocco [73/2024]. All participants were informed about the study's objectives and provided their informed consent before participating. The confidentiality of participants' information was strictly maintained.
The study will be conducted in accordance with the principles set out in the Declaration of Helsinki, all applicable regulations and according to established international scientific standards.
3. RESULTS
The sample of 215 patients shows a clear male predominance with a male/female sex ratio of 2.08. The average age of the patients is 51.67 years (standard deviation = 0.487). Regarding the level of education, 79.62% of the patients have a secondary or higher education level. The majority of participants reside in urban areas (80.55%) compared to rural areas (19.44%) (Table 1).
The distribution by dominant pathologies in the clinical hematology department is as follows: 32.40% of cases are multiple myelomas, 24.07% acute leukemias, 17.59% chronic lymphoid leukemias, 14.81% non-Hodgkin lymphomas, 6.48% chronic myeloid leukemias, 2.77% myelodysplastic syndromes, and 1.85% Hodgkin lymphoma (Fig. 1).
3.1. General Knowledge about Therapeutic Education
Table 2 shows that age is a significant factor for questions regarding knowledge of therapeutic education (p-values of 0.010 and 0.000, respectively). However, age did not show a significant difference in the perceived need for therapeutic education. This indicates a significant association between age and knowledge of the objectives of therapeutic education.
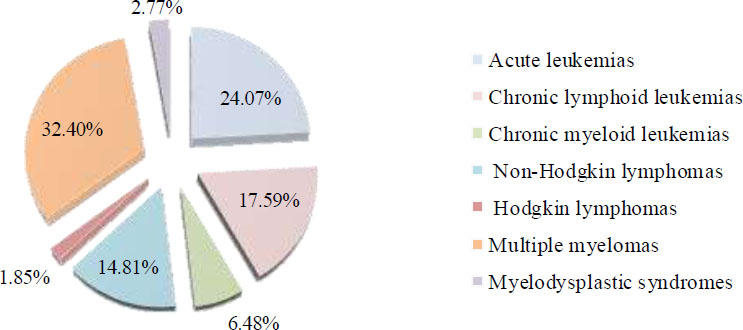
Distribution of pathologies in clinical hematology at HMIMV.
| Characteristics | n=215 |
|---|---|
| Sex | |
| Female | 70 (32.40%) |
| Male | 146 (67.59%) |
| Age | |
| Under 65 | 134 (62.03%) |
| Over 65 | 82 (37.97%) |
| Education Level | |
| Illiterate | 6 (2.77%) |
| Primary | 38 (17.59%) |
| Secondary or higher | 172 (79.62%) |
| Residence | |
| Urbain | 174 (80.55%) |
| Rural | 42 (19.44%) |
| Therapeutic Education-based Questions | Yes | No | p-value | Khi-2 | Exact Sig |
|---|---|---|---|---|---|
| Have you ever heard of therapeutic education? | (134) 62.3% | (81) 37.7% | 0.010 | 6.640 | 0.014 |
| Do you know the objective of therapeutic education? | (106) 49.3 | (109) 50.7% | 0.000 | 14.528 | 0.000 |
| Do you feel the need to receive therapeutic education? | (120) 55.8% | (95) 44.2% | 0.139 | 2.189 | 0.158 |
3.2. Specific Knowledge of Patients
The regression analysis shows that the model's constant is significantly different from zero, with a B value of 37.151 (p < 0.001), indicating that even in the absence of other variables (age, education level, pathology), the knowledge score is estimated at 37.151. The age coefficient is also significant, with B = 8.012 (p = 0.005), suggesting that an increase of one unit in age is associated with an average increase of 8.012 points in the knowledge score, with a 95% confidence interval ranging from 2.493 to 13.531, confirming the robustness of this effect. In contrast, the education level does not appear to have a significant effect on the knowledge score, with a coefficient B = 2.198 (p = 0.449) and a confidence interval that includes zero [-3.519, 7.914], indicating that the effect is not statistically significant. Finally, the “pathology” variable has a significant and positive effect on the knowledge score, with a coefficient B = 3.238 (p < 0.001) and a 95% confidence interval ranging from 1.80 to 4.67, showing that the pathology significantly contributes to the variation in the knowledge score. These results highlight the importance of age and pathology in explaining patient knowledge, while education level does not seem to play a significant role (Table 3).
According to Table 4, the majority of patients have a good understanding of the essential aspects of their disease and treatment. However, some areas remain insufficiently understood, highlighting the need to strengthen efforts in training and therapeutic education. Identifying educational priorities is crucial to guiding actions toward areas requiring special attention.
| Variable | Coefficient B | Standard Error | t valeur | p-value | 95% Confidence Interval |
|---|---|---|---|---|---|
| Constant* | 37,151 | 8,800 | 4,222 | 0,000 | [19,804, 54,498] |
| Age | 8,012 | 2,800 | 2,862 | 0,005 | [2,493, 13,531] |
| School level | 2,198 | 2,900 | 0,758 | 0,449 | [-3,519, 7,914] |
| Pathology | 3.238 | 0.731 | 4.428 | 0.000 | [1,80, 4,67] |
| Variable related to Patient’s Knowledge | Mean±SD | Low | Mean | High | Prioritization of Knowledge among Patients |
|---|---|---|---|---|---|
| Knowledge of the disease | 3,40 ±1,525 | 9 (4.2%) | 97 (45.1%) | 109 (50.7%) | Prorité3: >50% |
| Symptom of the disease | 3,40±1,525 | 9 (4.2%) | 97 (45.1%) | 109 (50.7%) | Prorité3: >50% |
| Method of administration of the treatment | 3,40±1,525 | 9 (4.2%) | 97 (45.1%) | 109 (50.7%) | Prorité3: >50% |
| Side effects of the treatment | 3,40±1,525 | 9 (4.2%) | 97 (45.1%) | 109 (50.7%) | Prorité3: >50% |
| Acceptance of the disease | 2,60±1,264 | 9 (4.2%) | 149 (69,3%) | 93 (26.5%) | Priorité 1: 21-30% |
| Adaptation to care | 2,38±1,25 | 8 (3.7%) | 136 (63,2%) | 52 (24.2%) | Priorité 1: 21-30% |
| Relational side: Family, friends | 42,60±1,264 | 9 (4.2%) | 149(69,3%) | 57 (26.5%) | Priorité 1: 21-30% |
| Pain management | 2,94±1,381 | 9 (4.2%) | 140 (65,2%) | 65 (30.3%) | Priorité 1: 21-30% |
| Biological tests | 3,41±1,463 | 21 (9.8%) | 94 (43.7%) | 100 (46.5%) | Priorité 2: 31-49% |
| Treatment | 3,33±1,465 | 9 (4.2%) | 114 (53,0%) | 92 (42.7%) | Priorité 2: 31-49% |
| Healthy lifestyle | 3,33±1,465 | 9 (4.2%) | 114 (53,0%) | 92 (42.7%) | Priorité 2: 31-49% |
| Treatment success rate | 2,93±1,403 | 21 (9.8%) | 118 (54,9%) | 76 (35.3%) | Priorité 2: 31-49% |
| Diet | 3,33±1,465 | 9 (4.2%) | 114 (53,0%) | 92 (42.7%) | Priorité 2: 31-49% |
| Acceptance of the treatment | 2,33±1,263 | 5 (2.3%) | 134 (62,3%) | 76 (35.4%) | Priorité 2: 31-49% |
| Belief and spirituality | 2,13±1,261 | 6 (2.8%) | 111 (51,7%) | 98 (45.6%) | Priorité 2: 31-49% |
| Fatigue management | 2,98±1,379 | 9 (4.2%) | 139 (64,7%) | 67 (31.2%) | Priorité 2: 31-49% |
| Physical activity | 3,28±1,465 | 9 (4.2%) | 116 (54,0) | 90 (41.9%) | Priorité 2: 31-49% |
| Sexual activity | 3,16±1,412 | 11 (5.1%) | 128 (59,5%) | 76 (35.3%) | Priorité 2: 31-49% |
3.2.1. Most Critical Elements
Patients place great importance on aspects directly related to managing their disease and side effects, with high average scores (3.40 ±1.525). This may be explained by the significant impact of these elements on their daily lives and overall treatment success.
3.2.2. Acceptance and Adaptation
Although these aspects are recognized as important, they are considered less critical than treatment and disease-related aspects (31-49%). This perception may reflect the idea that acceptance and adaptation, while essential, do not have as immediate or direct an impact on treatment or disease management.
3.2.3. Relational Aspects and Pain
Family support and pain management, although fundamental, are considered less of a priority compared to other elements, with lower average scores (2.60 to 2.94). This could indicate that patients prioritize the medical and practical aspects of managing their disease, relegating relational and comfort considerations to a secondary level.
4. DISCUSSION
This study aimed to assess patients' knowledge to determine their educational needs in the development of a therapeutic education program (TEP) at the clinical hematology department of the Mohammed V Military Instruction Hospital [9]. The importance of a well-structured therapeutic education program is increasingly recognized in the management of patients with chronic diseases, particularly in the field of hematology, where treatments are often complex and prolonged.
The research method used, primarily based on a questionnaire, allowed for the collection of valuable information regarding patients' perceptions and knowledge. However, this method has certain limitations, such as its inability to capture non-verbal data, including silences and emotions, which could provide additional insights into patients' needs [10]. Despite these limitations, the majority of patients expressed satisfaction with participating in the survey, highlighting the relevance of the approach used to collect data on their educational needs.
The socio-economic diversity of the patients was a key factor in the analysis of the results. This diversity allowed for a better understanding of each patient's skills, difficulties, and specific needs. These results are consistent with previous studies, including a national study in France, which demonstrated that the patient's psychosocial profile is crucial for adapting communication and educational interventions, especially during the announcement of an onco-hematological diagnosis [3].
The diversity of pathologies observed in our sample, although it could introduce bias, allowed for the exploration of a wide range of educational needs specific to each type of hematological disease. This diversity reinforces the idea that therapeutic education should be personalized and adapted not only to the pathology but also to the patient's overall profile.
The analysis results show that while the majority of patients understand the essential aspects of their illness and its treatment, there are still significant gaps in certain areas, indicating a need for additional targeted education. This observation highlights the importance of focusing educational efforts on areas where knowledge is insufficient to improve the overall care of patients. For example, aspects related to acceptance and adaptation, although important for effective disease management, are often perceived as less critical by patients. It is, therefore, crucial to raise awareness among patients about the importance of these aspects to promote better adherence to treatment.
Educating and informing patients about their disease and all aspects of their therapeutic protocol is extremely important, as it plays a crucial role in their care. It facilitates their acceptance and active participation in the treatment, leading to better treatment adherence [11-13]. To achieve this, patients must develop adaptive skills. According to the WHO, these skills are “personal, cognitive, and physical competencies that allow individuals to master and direct their existence, acquire the ability to live in their environment, and modify it.” According to Hagger et al. [14], patients' reactions and their physical and psychological functioning are linked to the announcement and representation of the disease and treatment. The quality of information provided during the announcement is important. A study conducted by Besson et al. on the announcement and choice of words in clinical hematology demonstrated that patients often struggle to understand their disease, but this does not prevent them from seeking information about their health and treatment. This information must be as clear, simple, and adapted to their needs as possible, without any taboos, enabling patients to make informed decisions regarding their health, whether medical, social, emotional, spiritual, or even in some cases, the decision to refuse treatment [15].
Furthermore, a significant lack of knowledge was reported by the patients interviewed regarding the effectiveness and uncertainty of the treatment provided to them. The possibility or likelihood of prolonged treatment for these pathologies may be a factor [16]. In France, a survey organized by the Federation of Cancer Centers (FNCLCC) in twenty cancer centers in 2003 demonstrated that patients understood only the information received during the initial diagnosis and subsequent consultations, which were very brief and focused solely on clinical monitoring of treatment progress. After that, there was no longer room for structured information [16]. Thus, the majority of patients were not aware of the various biological tests awaiting them throughout their therapeutic journey, which can sometimes manifest as fear or even refusal to undergo them. In clinical hematology, certain biological tests, such as bone marrow biopsies, can be particularly challenging. To avoid this situation, it is best to inform and educate the patient about the essential biological tests related to their disease since any information the patient receives allows them to make an informed choice and decide whether to accept or refuse the care provided [17].
Lack of knowledge and information regarding lifestyle management, including diet, fatigue management, pain management, and physical activity, was expressed by the majority of patients interviewed. In hematology, the aggressiveness of treatments, particularly chemotherapy, radiotherapy, and hematopoietic stem cell transplantation, imposes physical, psychological, emotional, and cognitive constraints [18]. The consequences are severe and cause a considerable change in the quality of life, which is crucial for survival chances and chronic fatigue [19, 20]. Additionally, chronic fatigue (asthenia) often prevents patients from performing daily activities and maintaining a normal work schedule. Physical activity remains an option to combat this fatigue, as does pain management, which is a complex issue. Pain is common, and it can be present during diagnosis and treatment [21]. In an analysis of 32 publications, pain was the primary symptom in 70% of cancer patients and was experienced by 50% of those undergoing cancer treatment [22]. Pain and fatigue management is crucial, requiring knowledge, skills, and competencies on the part of the patient, which can only be achieved through structured therapeutic education, a relevant option for addressing these issues. Regarding diet, it is essential to monitor the patient's nutrition and educate them throughout the therapeutic process [23].
The intimate and relational aspect (family, friends, colleagues, etc.) also plays a role in the therapeutic education of the patient. A significant percentage of respondents reported a lack of knowledge, and most of them had difficulty addressing intimate topics with the medical team. The sexual aspect has always been relegated to the background in care and is often overlooked in favor of therapeutic effectiveness. In hematology, the systemic side effects of chemotherapy drugs can temporarily decrease sexual desire or physical capacity. Additionally, during the reactive depressive phase following the disease announcement and sometimes due to changes in body image caused by the disease or treatment, these changes can lead to sexual disorders in both men and women [24, 25]. Regarding the relational aspect, hematological diseases can affect relationships between the patient and their loved ones, leading to significant, sometimes sudden, disruptions in their social and professional lives, which can cause some individuals to experience isolation that is difficult to overcome [3].
The majority of patients expressed a high level of acceptance regarding the spiritual aspect due to their religion and beliefs. For them, being ill is “Makatib,” or predestination. They expressed their gratitude to God for this illness. It is worth noting that some patients have a pessimistic religious view of cancer, considering it a divine punishment for past sins [26]. Research has shown that patients need spirituality, which increases healing chances and is important for their physical health [27, 28]. Integrating the spiritual dimension into care through patient education and information is essential, leading to compassionate care and better support [26].
Therapeutic education relies on the patient's prior knowledge and impressions, as well as their ideas and perceptions [29] of the disease and treatment, to help them move forward [30, 31]. It should be noted that informing the patient is both a legal and ethical obligation and is an integral part of the care process [32, 33], which should be taken into consideration for better care.
In summary, most patients believe that being educated about their illness and treatment is important. However, some find this information stressful, and some reject the concept of therapeutic education out of fear of learning more. This observation reinforces the idea that therapeutic education should be structured according to the patient's needs, taking into account their preferences, beliefs, and personal values.
CONCLUSION
In conclusion, this study underscores the need for a structured TPE program in clinical hematology to address the specific educational needs of patients. By providing comprehensive education, healthcare providers can help patients better manage their disease, improve adherence to treatment, and enhance their overall quality of life.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| FNCLCC | = Federation of Cancer Control Centers |
| HMIMV | = Mohammed V Military Teaching Hospital |
| TPE | = Therapeutic Patient Education |
| WHO | = World Health Organization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Ethics Committee for Biomedical Research, Morocco reference number: 73/2024.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.


