All published articles of this journal are available on ScienceDirect.
The Impact of the COVID-19 Pandemic on Lifestyle Behaviors among School Children in Morocco
Abstract
Introduction
Usually, active children were the first to be affected during the COVID-19 pandemic. This study aimed to describe and assess the impact of the COVID-19 pandemic on the lifestyle behaviors of schoolchildren in Marrakech, Morocco.
Methods
Parents of children from three private voluntary primary schools were asked to complete an online questionnaire. Diet, physical activity, and sleep information were collected from May 11 to June 04, 2020. Changes in lifestyle before and during the COVID-19 pandemic were assessed and analyzed.
Results
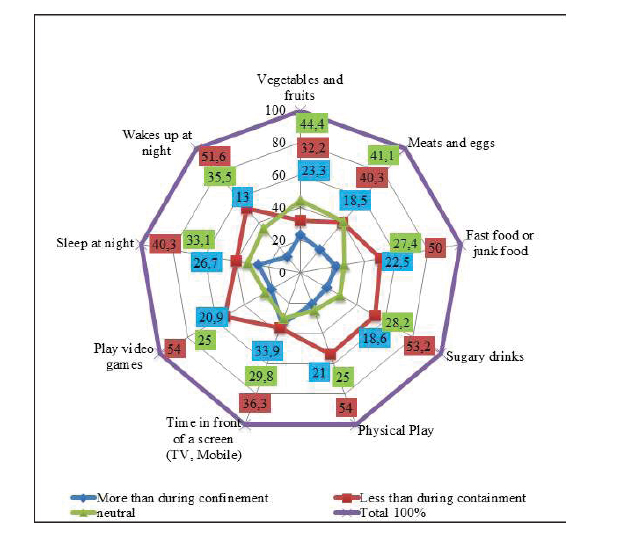
There were 124 participants. There were 54% males, the average age was 9.77 ± 1.96 years, and the average BMI was 20.46 ± 6.32 kg. During the COVID-19 pandemic, the following behavioral trends were reported: an increase in the consumption of sugary drinks (53.2%), an increase in the consumption of sweets and chips (50%) (Control no variation of 27.4% and a decrease of 22.5%), increased sedentary time (TV/mobile: 52.4%; video games: 54%), decreased quality of sleep (51.6%) and increased physical game activity (54%).
Conclusion
When encouraging pandemic measures to address COVID-19, it is crucial to consider the invisible effects of these restrictions on the health of childern and to plan for parallel actions to maintain healthy lifestyles and prevent possible impacts on the level of overweight in this vulnerable population.
1. INTRODUCTION
1.1. The Global Impact of COVID-19
The entire planet has been faced with a potentially severe pandemic of pneumonia caused by a new corona- virus named severe acute respiratory syndrome corona- virus 2 (SARS-CoV-2), which was initially detected and reported in Wuhan, Hubei Province, China [1]. The COVID-19 pandemic has since spread widely around the world, with more than 13,575,040 confirmed cases and 584,556 people deceased as of July 16, 2020 [2]. This global crisis profoundly impacted children, disrupting their education, social interactions, and daily routines. Many faced significant challenges to their physical and mental well-being due to extended school closures and increased isolation [3-5].
1.2. Government Responses to COVID-19
In Morocco, drastic measures were put in place to stop the spread of the virus and limit its damage. In addition to the travel ban, several options, such as working from home and closing schools, were operated under forced restrictions [2]. In the wake of this state of health emergency implemented in Morocco to address the COVID-19 health crisis, there is concern about the possible impact this pandemic will have on the health of this pediatric population. Several studies have shown that in such times of crisis, children, as a vulnerable population, are often seriously affected, not only in terms of health but also in terms of socioeconomic status and well-being [3-5].
1.3. Impact on Children as a Vulnerable Population
This vulnerability can be reflected in the receptivity of children to disease and access to active education, balanced nutrition, appropriate sports, and recreational programs, as well as physically and psychologically safe environments [6-8].
Approximately 9.3 million Moroccans were between the ages of 0 and 14 in 2020, demonstrating the significant impact of the pandemic on this demographic. Moroccan children, along with the 2.34 billion children and young people under 18, live in one of the countries that have implemented movement restrictions due to COVID-19 [9]. These restrictions include locking schools, closing playgrounds and public parks, and confining homes with conditioned and limited access to the outside [10].
Restrictions aim to minimize the risk of transmission of the virus; however, several studies have shown that these measures of restriction and social distancing, if they are prolonged, could have severe consequences for the physical and mental health of children, emphasizing the need for early detection and preventive interventions to protect children from the severe consequences that such pandemic measures can have on their health [11-15].
Furthermore, the behavior of children at home during school holidays or on weekends can be partially transposed to the COVID-19 pandemic restrictions. These factors increase the risk of overweight and obesity, which can affect cardiovascular and metabolic prognoses in adulthood [16] because changes in these parameters can affect three main factors of overweight, namely, the hours, quantity, and quality of meals; the frequency and intensity of physical activity; and the quantity and quality of sleep. The context of pandemics favors sedentary behaviors and very fragile mental health in children [12, 17, 18] and can cause unfavorable changes in nutritional quality, energy balance, and psychosocial balance in the medium term. This can have long-term harmful effects on overweight individuals and subsequently on the metabolic and cardio- vascular prognoses of these children [19].
1.4. Study Objectives
This study focused on the consequences of adopting these generalized measures linked to the COVID-19 pandemic on the lifestyles of children, mainly eating behaviors, physical activity, sedentary lifestyles, and sleep. The purpose of this study was to measure changes that may affect the physical and psychological health of Moroccan children, thus providing parallel interventions capable of preventing a predictable impact on the level of adiposity of this fragile population and negatively affecting their physical well-being and mental and social health in adulthood.
2. MATERIALS AND METHODS
This cross-sectional descriptive study was carried out in three private primary schools in the city of Marrakech, Morocco. The parents of the school children were asked to voluntarily provide information about their children via a self-administered online questionnaire. Given the constraints of access to information and face-to-face recruitment of participants due to the restrictions applied by the state of emergency, the choice of schools was based on purposive sampling (reasoned selection). The selection of schools was thus established by considering the online accessibility of the contact details of all parents of registered students, the administrative willingness of schools to participate in the study, and the responsiveness of the parents of students.
The inclusion criteria for the participants were:
- Being enrolled in primary school during the collection period, regardless of age, gender, or educational level.
- Having access to the internet to answer the online questionnaire.
- Having agreed to voluntarily participate in the study by checking the corresponding box to access the form and entering their email address after reading and understanding the objectives of the study.
The questionnaire was based on a literature review (questions were derived from the French Questionnaire for assessing children's lifestyle habits recommended by the National Nutrition and Health Program (PNNS) [20], adapted to lockdown circumstances) and consisted of thirty closed questions, including thirteen multiple-choice questions, nine numerical responses, and six Likert scale questions. The questionnaire was administered according to the criteria of confidentiality, self-determination, and informed consent of the participants.
The questions were divided into three sections describing eating habits (frequency, quality), physical activity habits and sedentary lifestyle (duration of activity versus time spent in front of screens), and sleep and rest habits (quantity and quality) without considering socio- demographic and weight information, including age, sex, educational level, weight, height, and residence. A fourth section has been added to compare these habits temporally before and during the COVID-19 pandemic. The study spanned from May 11 to June 04, 2020. After collection and preparation, the statistical analysis was performed using SPSS version 21.0 for Windows. The self-reported data were thus summarized using frequencies and percentages for the qualitative variables and the means and standard deviations for the quantitative variables.
3. RESULTS
Out of 400 parents contacted by email, only 124 responded to the online form, with participants distributed among the three schools: 41 from the first school, 43 from the second, and 38 from the third. The average age, weight, height, and body mass index (BMI) of the boys were 54%, 9.7 ± 1.9 years, 33.9 ± 7.4 kg, 131.7 ± 16, 7 cm, and 20.5 ± 6.3 kg/m2, respectively. More than half of the respondents (54.9%) had completed primary school in the last two years, and a family history of overweight was reported in 21% of the respondents. In addition, 58.1% of the respondents lived in a separate house with no neighboring cohabitation. Tables 1 and 2 describe in detail the characteristics of the included school children. The data collection period coincided with Ramadan (the holy month of fasting for Muslims). However, only 15.3% of the school children fasted regularly.
| Categories | Frequency | Percentage | |
|---|---|---|---|
|
Gender (n=124) |
Female | 57 | 46,0 |
| Male | 67 | 54,0 | |
|
Primary school level (n=124) |
Level 1 | 13 | 10,5 |
| Level 2 | 9 | 7,3 | |
| Level 3 | 19 | 15,3 | |
| Level 4 | 15 | 12,1 | |
| Level 5 | 25 | 20,2 | |
| Level 6 | 43 | 34,7 | |
|
Habitat type (n=124) |
Apartment in a building | 49 | 39,5 |
| Detached accommodation | 59 | 47,6 | |
| Villa | 13 | 10,5 | |
| Other | 3 | 2,4 | |
| Family history of overweight (n=124) | None | 91 | 73,4 |
| Mother/Father/Brotherhood | 26 | 21,0 | |
| Other | 7 | 5,6 | |
| - | Females (N=57) | Males (N=67) | Total (n=124) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean±SD | Range | Mean±SD | Range | Mean±SD | Range | ||||
|
Age (years) |
9.74±1.89 | 5-13 | 9.80±2.02 | 5-13 | 9.77±1.95 | 5-13 | |||
|
Weight (Kg) |
33.67±7.60 | 18-47 | 34.88 ±7.33 | 20-50 | 33.91±7.39 | 18-50 | |||
|
Height (cm) |
130.56±15.77 | 100-163 | 132.56±17.58 | 100-170 | 131.75±16.68 | 100-170 | |||
|
BMI (kg/m2) |
20.27±5.93 | 9-39 | 20.62±6.66 | 10-41 | 20.46±6;32 | 9-41 | |||
| Frequency per day | Fruits | Vegetables | Meat and egg | Sweet desserts |
|---|---|---|---|---|
| - | N(%) | N(%) | N(%) | N(%) |
| None | 6(4.84) | 5(4.03) | 5(4.03) | 14(11.29) |
| Once | 63(50.81) | 54(43.55) | 79(63.71) | 72(58.06) |
| Twice | 34(27.42) | 46(37.10) | 24(13.35) | 29(23.39) |
| Three or more times | 21(16.94) | 19(15.32) | 16(12.9) | 9(7.26) |
Table 4.
| Mean±SD | Range | ||
|---|---|---|---|
| TV or mobile phone (in minutes) | 196.2±70.9 | 60-303 | |
| Computer or video games (in minutes) | 110.9±103.4 | 0-540 | |
| Active play (in minutes) | 66.5±78.0 | 0-480 | |
On the one hand, the respondents reported regular and assiduous daily consumption of the main meals (50.8%) of eggs and meats (96%), vegetables (96%), and fruits (95.24%). In addition, foods with high energy intake, such as crisps, savory cakes and peanuts (68.5%), chocolate bars (54.8%), pizzas (50.8%), fries (55.6%) and cakes (55.6%), were banned.
A significant proportion of respondents declared that they regularly consumed sweet creams and desserts per day (58.06%), quiches at least once a week (71%), burgers (83.9%), sodas (75, 8%), sandwiches (85.5%) and systematically added seasonings to their dishes (61.2%), including ketchup (55.6%), mayonnaise (65.3%) and salt (80.6%) (Table 3).
On the other hand, regarding sedentary habits and/or physical activity, only 22.6% of the parents surveyed noted the inactive nature of their children during the pandemic. The average daily time spent in active play was 66.5 ± 78.0 min.
On the other hand, the daily average time spent in front of a screen was 196.2 ± 70.9 min for television/telephone games and 110.9 ± 103.4 min for computer/video games. More than half of those surveyed said that their schools broadcast structured physical activity programs online (56.5%), the weekly broadcast frequency of which fluctuated between once (69.8%), twice (11.3%), and three or more times (3.8%). Most of the school children surveyed declared that they did not follow these programs broadcast during the pandemic (60.4%), while others regularly followed these physical education classes (15.1%) (Table 4).
Changes in school children’s behavior during versus before the pandemic.
In addition, sleep behaviors/habits and physical/ psychological recovery presented quantitative and qualitative fluctuations during the pandemic.
The average sleep time of the school children surveyed was 8.3 ± 1.8 hours, and most participants said that their children slept continuously at night (65.3%) and were active and dynamic upon awakening (77.4%).
Analysis of changes in child lifestyle behaviors before and during the COVID-19 pandemic revealed an increase in the following factors: consumption of sugary drinks (53.2%), consumption of sweets, crisps, and junk food (50%), no variation (27.4%), a decrease (22.5%), sedentary time (TV/Mobile: 52.4%; Video games: 54%), time spentactive play at home, and amount of sleep (40.3%) (with no variation of 25% and a decrease of 20.9%), while quality decreased (51.6%) (Fig. 1).
4. DISCUSSION
This study aimed to investigate the impact of the COVID-19 pandemic on the lifestyle habits of school- children in the city of Marrakech. The study revealed changes in the eating, activity, and sleeping behavior of schoolchildren during the COVID-19 pandemic. These results corroborate those of several studies [6, 12, 15, 17, 21-24]. Thus, whatever represents a contextually delimited case, the data are revealed after analysis and inter- pretation of the relevant information on three levels:
The first plan is related to eating habits. The results of this study showed, at first glance, during the pandemic, normal behavior in the consumption of vegetables, fruits, and protein products (eggs and meat), which is consistent with several studies that have explained the benefits of home confinement as an opportunity for working mothers to ensure the quality of homemade meals [21]. However, harmful changes have been noted in consuming products with high-energy intake (fast food, junk food, and sugary drinks). Studies have warned against excessive sugar consumption for children aged 4 to 17, mainly emphasizing sugary drinks and pastries/cookies/cakes, which are high in sugar and have low nutritional benefits [25]. These latter behavioral trends promote an energy imbalance between consumed and expended calories. When combined with a sedentary or inactive state, they are fundamental factors of obesity and overweight in children worldwide [19].
Second, regarding sedentary habits, the school children surveyed reported an increase in the length of time spent in front of screens (TV, laptop, video games), which significantly increases the time spent sedentary and threatens the metabolic health of these children [19]. The impact of increasing screen time is unfortunately not limited to sedentary lifestyles and addiction problems but is also associated with poor oral hygiene and obesity [26], social and emotional problems [26], and myopia [27]. The results of the present study also showed a remarkable increase in the time spent on physical games, and the majority of assessments of overactivity in the subjects studied. This could indicate an improvement in the mode of physical activity of these children during the pandemic. On the one hand, the salient lack of attendance and adherence to structured courses of physical activity, which are disseminated for their benefit by their educational establishments, and on the other hand, the increase in time of sedentariness that was previously discussed, one can claim a systematic regression in their energy expenditure. This interpretation is supported by several studies that have shown that most parents seem to underestimate the overweight and physical activity problems of their children [28]. The increase in school children’s activity during the pandemic can thus be explained by the vagaries of a subjective comparison of parents. This comparison remains based on hyperactivity states generated in children by the psychological effects of a feeling of pressure due to prolonged contiguity and spatial restrictions linked to the pandemic.
The last plan is to focus on rest and sleep behaviors. The responses of the respondents showed that the sleep duration increased during the pandemic but at the expense of quality. The children surveyed, by experiencing changes favorable to a sedentary lifestyle and to a restricted environment loaded with stress and anxiety, are indirectly exposed to the risk of sleep disorders [29, 30]. These sleep irregularities occur primarily at night, which affects the child's ideal development and growth since growth hormones are produced at night [31]. The increase in the use of LED screens (laptops, TVs, video games, and computers) among respondents is also a risk factor that desynchronizes the circadian clock of children and damages their sleep quality. Poor-quality sleep results in impaired academic performance, anxiety disorders, depression, and violent and hyperactive driving [32-34]. Moreover, lack of sleep is correlated with a reduction in cognitive abilities, particularly verbal comprehension, leading to a cognitive deficit of about 11 points every three years [35].
5. STRENGTHS OF THE STUDY
The present study reserves the ingredients of an original and pioneering study. On the one hand, this is the first study to explore changes in behavior, both eating and sedentary and asleep, during the COVID-19 pandemic. It also aims to be a pioneer by studying the effects of the COVID-19 pandemic on the lifestyles of children in primary schools; finally, it can be claimed to be the only contemporary study to address the effects of the COVID-19 pandemic on the behavior of Moroccan children.
6. LIMITATIONS OF THE STUDY
The current report has several limitations, including the impossibility of generalizing the results because children from the public sector or rural schools were not included in the sample and the coverage error generated by the online survey adopted in the present study. The statistics were only descriptive, so in the absence of before-after measures, and although the changes observed align with expectations, it is difficult to be sure that similar effects would not have been observed before the pandemic. Some data on eating or sleeping habits may be biased because the data collection coincided with Ramadan. However, this last factor did not influence 84.7% of the school children surveyed. The COVID-19 pandemic may have heightened parents' concerns about their children's behavior, potentially influencing their responses. Similarly, caution should be exercised when comparing the results of this study to those of other studies conducted during the COVID-19 pandemic, mainly due to differences in the extent and practical forms of the pandemic measures and their duration between countries and regions.
Briefly, the majority of these limits remain understandable given the operational requirements of this study (restriction of accessibility related to pandemic measures and inevitable use of online surveys).
CONCLUSION
With pandemic measures, it, therefore, seems more difficult for primary school children to maintain a well-balanced diet, especially a dietetic nonobesogenic diet, to practice structured physical activity in the absence of social ties with their friends and congeners, despite the existence of dedicated programs and systematic online distribution.
By prohibiting active travel outside of homes (play areas, commuting between school and home, public gardens), opportunities to move become almost absent, inevitably increasing the chances of these children gaining weight and affecting their cardiovascular prognosis in adulthood.
It is therefore advisable, when encouraging the application of pandemic measures to address COVID-19, to consider the invisible effects of these restrictions on the health of children and to plan parallel actions to maintain healthy lifestyles and prevent possible impacts on the level of overweight in this vulnerable population.
To address these concerns during COVID-19 pandemic conditions, parents, schools, and policymakers need to collaborate in order to implement specific strategies:
For Parents
Encourage healthy eating by involving children in meal planning and preparation, emphasizing the importance of balanced nutrition. Establish daily routines incorporating indoor physical activities, such as online exercise classes or dance sessions, to promote movement while staying home.
For Schools
Utilize virtual platforms to offer structured physical activity sessions, such as online physical activity classes or fitness challenges that encourage participation from home. Additionally, it provides resources and guidance for parents on creating healthy meal plans and engaging in nutritional education.
For Policymakers
Implement policies that support access to online physical activity and nutrition resources, including virtual community programs and webinars for families. Promote public health campaigns that focus on maintaining healthy habits during lockdown, ensuring families have the necessary information and tools.
Furthermore, it is crucial to emphasize the importance of ongoing monitoring of children's health and lifestyle habits during and after such crises. Regular assessments can help identify trends and long-term effects related to diet, physical activity, and overall well-being. By gathering and analyzing this data, stakeholders can develop targeted interventions to support the health of children after crises, ensuring they receive the necessary resources and guidance to thrive.
AUTHORS’ CONTRIBUTIONS
L.Y.: Planned, executed, and collected the data. He also interpreted the results of the study and wrote the research article; E.H.: Contributed to the interpretation of the data and correction of the article; M.S.: Analyzed the data with SPSS; and M.A., and L.A.: Led the study and corrected the article.
LIST OF ABBREVIATIONS
| BMI | = Body mass index |
| COVID-19 | = Coronavirus disease 2019 |
| LED | = Light-emitting diode |
| PNNS | = The French National Nutrition and Health Program |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The University Hospital Ethics Committee of the Faculty of Medicine and Pharmacy, Cadi Ayyad University of Marrakech, Morocco, approved its ethical authorization in June 2021 (Reference#21/2021).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
The online questionnaire edited for data collection contained an informed consent form to be accepted by anyone before participation.
AVAILABILITY OF DATA AND MATERIALS
All data and materials are available at the link below: https://drive.google.com/drive/folders/1moWFNYsu1XLzthVW_GtPWU4SabK0YNAj?usp=sharing
ACKNOWLEDGEMENTS
This research would not have been possible without the dedication of our participants, who volunteered their time and effort during the COVID-19 pandemic. Their contribution, made under such challenging conditions, has been crucial to the success of this study. The authors would like to sincerely appreciate their resilience and commitment.


