All published articles of this journal are available on ScienceDirect.
Investigating the Effectiveness of the Health-promoting Lifestyle Educational Program on Suicidal Thoughts in Healthcare Workers
Abstract
Background
Suicide is a crisis, and its occurrence in healthcare workers (HCWs) is a special challenge that requires urgent interventions.
Aim
This study was conducted to determine the effectiveness of the health promotion lifestyle training program on suicidal thoughts in HCWs.
Methods
This one-sample longitudinal study was conducted using a multi-stage sampling method on 248 healthcare providers in 2023. In the first stage, the Beck scale was used to measure suicidal thoughts, and the DASS-21 was used to measure depression, anxiety, and stress. In the second stage, individuals with suicidal thoughts were placed in a separate group, and educational intervention continued for them. The health promotion lifestyle training protocol was provided to this group as a training program, and researchers followed up on its implementation for 95 days. In the third stage, after the completion of the educational intervention, the Beck scale and DASS-21 were once again provided to the target group. Data were analyzed in SPSS-25 statistical software.
Results
27.8% of participants had suicidal thoughts, 7.66% represented high-risk suicidal ideation, and 20.1% had low-risk suicidal ideation. 69 HCWs who had suicidal thoughts used the health-promoting lifestyle education program for 95 days. The percentage of suicidal thoughts in people with high suicidal risk ideation decreased from 7.66% to 4.03% (p<0.05), and in people with low-risk suicidal ideation decreased from 20.1% to 13.30% (p<0.05).
Conclusion
Health promotion educational programs can be used as an effective intervention in improving mental health indicators and reducing suicidal thoughts in HCWs.
1. INTRODUCTION
Our healthcare systems are currently under previously unheard-of demands as a result of the coronavirus pandemic. The 2019 coronavirus pandemic created long-term stressful conditions for HCWs. Given the current state of affairs, they are still under psychological stress from the ensuing crises in healthcare budgets and the cost of living. Psychological issues can have a detrimental impact on job security and patient care quality, increasing employee attrition [1]. Since the COVID-19 pandemic began, a large number of people have been clinically diagnosed with worry and terror tendencies. A collection of symptoms brought on by an imperfect ability on the part of humans to cope with life's stressors and strains is known as anxiety. These include anxiety about having a serious accident, dying, losing control, having trouble relaxing, being unstable, having trouble breathing, sweating excessively, having palpitations, feeling numb or tingly in the limbs, having hot flashes, being restless in the legs, feeling lightheaded or dizzy, shivering, trembling in the hands, and having indigestion. The main cause of anxiety with COVID-19 appears to be its unknown nature, which leads to cognitive ambiguity regarding the virus and how to treat it. Even though COVID-19's catastrophic waves have passed, it's unclear what kind of spike and grave circumstances we'll encounter if another severe wave happens. The body's immune system may be weakened by this fear and anxiety, leaving it more susceptible to illnesses like COVID-19 [2]. In order to provide treatment for critically ill patients, HCWs must deal with a variety of psychological and physical stressors, such as anxiety, sadness, and symptoms of post-traumatic stress disorder. The mental discomfort linked to COVID-19 has disproportionately affected nurses and nursing staff because of their critical role in infection reduction and direct patient care. Because of the nature of their work, which includes caring for seriously ill and injured patients, handling patient fatalities, having larger workloads, and working long hours, HCWs are subject to high levels of stress [3]. When there is a greater need for healthcare, as in the case of a public health emergency or disaster, these professional pressures are frequently made worse. HCWs are more susceptible to post-traumatic stress reactions and are more sensitive to job stressors [4]. Increased rates of psychopathology, including depression, anxiety, and post-traumatic stress disorder, have been reported in national and worldwide investigations of the occupational and health consequences for HCWs during the COVID-19 pandemic. The COVID-19 pandemic has caused behavioral changes in healthcare personnel, such as sleep disturbances, relationship issues, and drug usage. It has also increased burnout rates, compassion fatigue, and job discontent. In reality, HCWs-especially registered nurses, healthcare support workers, and health technicians-are more likely to commit suicide than non-HCWs, according to a study of data from the 2008 American Community Survey and the National Death Index through 2019 [4, 5]. Because medical assistant training is rigorous and stressful and can have significant effects on patient care, medical assistants' psychological health is a serious concern. A crucial phase in a doctor's career, medical residency is marked by lengthy work hours, lack of sleep, elevated stress levels, social isolation, and emotional problems. These elements may raise the chance of acquiring psychiatric problems and significantly worsen psychological suffering [6, 7]. Studies carried out in low- and middle-income nations have demonstrated a noteworthy incidence of anxiety and depression among specialists, with rates ranging from 11% to 65%. Because medical assistant training is rigorous and tough, medical assistant psychological health is very important and can have a significant impact on patient care [8-11]. Serious repercussions, including suicidal thoughts and actions, can result from depression, particularly when it co-occurs with anxiety disorders. Suicidal thoughts have been reported in medical assistants in a number of studies, with an incidence of 4–35%. Suicide is the second most common cause of death for residents in the United States, according to the Accreditation Council for Graduate Medical Education (ACGME), with most suicides taking place during the first two years of training [9, 12]. The high risk of suicide among residents has been attributed to a number of causes, including lengthy and unpredictable work schedules, lack of sleep, burnout and cognitive decline, stressful events (such as life-or-death), and easy access to personal possessions [8, 13]. There may be regional, cultural, and contextual differences in the predictors of suicide thoughts and behaviors among medical assistants. Prior to the COVID-19 outbreak, there was no information available about the suicide rates of medical assistants in Iran. In 2016, a thorough review and meta-analysis revealed that the prevalence of suicidal ideation among medical students was 11.1% (95% CI, 9.0% to 13.7%) [14]. Nonetheless, there has been a rise in medical assistant suicides in recent years. According to a number of Iranian media reports, there were 15 recorded suicides involving physicians and medical assistants between June 2019 and 2021 [15]. This pattern is especially concerning because a large proportion of these occurrences happen quickly, suggesting a rise in these types of incidents over previous data. Anticipations of a decline in medical professional suicide rates following the COVID-19 pandemic have not materialized; instead, these tragic occurrences have remained common [16]. The ongoing issue at hand is attributed to various factors, such as a rise in workload, economic strains, substantial patient care obligations, societal stigma related to mental health disorders, and insufficient support networks within the healthcare system [15]. However, a thorough evaluation of this problem's scope has not yet been carried out. Thus, the purpose of this study was to elucidate the variables associated with suicidal ideation in Iranian medical assistants. To effectively address the mental health needs of medical assistants in Iran, support structures and treatments must be developed with an understanding of the particular difficulties they face. One of the best strategies for easing COVID-19-related anxiety is to support lifestyle modifications and health-promoting habits. The best approach to preventing numerous diseases and enhancing health is to modify one's lifestyle. Healthy habits, such as exercise and stress reduction, have been shown to be effective in lowering anxiety [2, 17]. A person's health and healthy lifestyle are strongly correlated, as was previously mentioned. A WHO study indicates that social support and lifestyle have a significant impact on health. A lifestyle that promotes health involves actions that provide individuals greater control over their health, which benefits both individual and societal health. Stress and anxiety can be predicted by six components of this lifestyle: spiritual growth, interpersonal interactions, health responsibility, stress management, and physical activity. Medical students lead unhealthy lifestyles, according to Iranian studies [2, 18-20]. Stress at work, which was brought to light during the COVID-19 epidemic, is still a major problem for medical personnel. In order to address the well-being of healthcare professionals, the authors of the current study set out to examine the use of peer support, self-care, and health-promoting lifestyle education as focused interventions. A health-promoting lifestyle can be achieved by profiling health-promoting lifestyle profile II (HPLPII). It should be noted that the health-promoting lifestyle profile II (HPLPII) is a tool for studying how sustainable huge populations [21, 22]. This profile has been translated into Spanish, Japanese, Arabic, and Turkish and is available [23, 24]. The basis of this profile is the model of perceived health promotion, which measures the probability of a person engaging in health-promoting behaviors [25]. The HPLPII is a modified version of the HPLP developed by Walker et al., and it measures the health-promoting lifestyle by focusing on the individual's innovative actions and perceptions that act in the direction of maintaining or increasing the levels of well-being, self-actualization, and individual satisfaction [25]. This questionnaire consists of 52 questions, which have 6 subsections under the headings of nutrition, physical activity, responsibility for health, stress management, interpersonal relationships, and spiritual growth. The HPLPII asks the respondent to indicate on a 4-point Likert response scale (never, sometimes, often, and usually) the extent to which he/she engages in specific health-promoting behaviors. In general, the health-enhancing lifestyle score and the behavior creation score are calculated using the average answers for all 52 questions and each sub-category (8 to 9 items). Walker and Hale Polerski reported a Cronbach induction of 0.94 for the HPLPII instrument [22]. The purpose of this study was to evaluate the impact of a lifestyle training program for health promotion on suicidal ideation in HCWs.
2. METHODS AND MATERIALS
248 HCWs, including physicians, residents, and nurses, who worked at Damghan Velayat Hospital, Rezaee Damghan Hospital, Imam Hossein Shahroud Hospital, and Kausar Semnan Hospital in 2023 were included in this one-sample longitudinal study. Trained interviewers gave the participants an explanation of the study's objectives before distributing and collecting the questionnaires; no names or initials were required on the questionnaires in order to protect their anonymity. The second page of the questionnaire detailed the inclusion criteria, which required respondents to confirm their consent to participate in the study. To guarantee that the study was targeted at a particular and pertinent participant group, access to the complete questionnaire was restricted to those who provided a yes response to these preparatory questions. Those who failed to provide informed consent to participate in the trial and those who missed three months of work-related hospital stays were among the exclusion criteria. We particularly refer to suicidal thoughts in HCWs, and we chose a conservative prevalence rate of 50% to establish our sample size, taking into account both low and high levels of suicidal risk in light of the lack of accessible studies. A statistical power analysis was conducted using a 95% confidence level, a 5% margin of error, and 248 people as the ideal sample size. An available sampling method was used for this research. Participants were given a written questionnaire to examine the factors linked with suicidal thoughts. The factors of interest in this survey were measured using a combination of demographic questions and standardized measures. The questionnaire's introduction page lays out the study's objectives in simple terms. The written questionnaire consisted of 64 items covering a variety of topics, such as demographics, expertise, having children, suicidal thoughts, place of residence, living arrangements, alcohol/drug use, history of psychiatric disorders, history of self-harm, personal history of suicide attempt, family history of suicide attempts, number of work shifts per month, death of loved ones due to COVID-19, items from the Depression, Anxiety, and Stress Scale (DASS-21), and components from the Beck Scale for Suicidal Ideation (BSSI) as well as items from the Beck Scale Ideation (BSSI) were conducted.
2.1. Beck Scale for Suicidal Ideation (BSSI)
The Beck Scale for Suicidal Ideation (BSSI), developed by Aaron T. Beck in 1979, is a widely recognized instrument for assessing suicidal thoughts and behaviors. This 19-item self-report questionnaire evaluates three dimensions of suicidal ideation: intensity, frequency, and intent. Each item is scored on a scale from 0 to 2, reflecting the absence, mild presence, or severe presence of suicidal thoughts, resulting in a total score that ranges from 0 to 38 [26]. The initial five items are specifically designed to identify individuals experiencing suicidal ideation; if respondents score zero on both the active suicidality item (item 4) and the passive suicidal desire Item (item 5), they are instructed to skip the remaining 14 items. Conversely, if any active or passive suicidal thoughts are present, scoring the additional items is required. Those with such thoughts are classified as suicidal ideators [27]. Although there is no universally accepted cutoff score for the BSSI to determine levels of suicidal risk, various studies have suggested criteria based on empirical findings and clinical insights. Specifically, a total score of 0 across all 19 items indicates no risk, while scores ranging from 0 to 5 suggest low risk, and scores of 6 and above indicate high risk [28]. Extensive investigations have affirmed the robust psychometric properties of the BSSI, with reported high internal consistency (Cronbach's alpha between 0.89 and 0.96) and good test-retest reliability (correlation coefficients exceeding 0.80) [29]. In their research, Esfahani et al. demonstrated that the Persian adaptation of the BSSI exhibited considerable internal consistency, with Cronbach's alpha values between 0.829 and 0.837. Moreover, this version of the BSSI displayed a notable correlation with depressive symptoms and confirmed a unidimensional factor structure [30].
2.2. Depression, Anxiety, and Stress Scale-21 (DASS-21)
A screening instrument called the DASS-21 is used to evaluate symptoms of stress, anxiety, and depression that a person may have had in the week before the evaluation. It is divided into three subscales, each with seven items: stress, anxiety, and depression. The relevant item scores, which range from 0 (does not apply to me at all) to 3 (applies to me a lot or most of the time), are added up to determine the final score for each subscale [31]. Across a range of languages and demographics, the DASS-21 has demonstrated strong internal consistency and reliability [32]. The Persian DASS-21 study demonstrated good test-retest reliability (0.881-0.740), high internal consistency (Cronbach's alpha: anxiety 0.79, stress 0.91, depression 0.93), and a satisfactory model fit in confirmatory component analysis (RMSEA 0.079, CFI 0.078). Provided an ICC of 0.75 to 0.86, indicating dependability in a nursing sample [33]. 27.8% of the 248 HCWs who participated in the study's first phase-69 of them-had suicidal thoughts. These individuals proceeded to the study's second phase, which ran for 95 days, from September 1, 2023, to December 5, 2023. A follow-up was conducted on the group of individuals with suicidal ideation after the health promotion lifestyle training program was implemented. The 52 implementation items in six fields-nutrition (7 items), physical activity (8 questions), health responsibility (13 items), stress management (5 items), and interpersonal relationships (8 items)-that make up the health promotion lifestyle education program are taken from a questionnaire with the same title. The results are displayed in Table 1 [34]. The instrument used in this research includes the health-promoting lifestyle profile of Walker et al. (1987), whose English version contains 52 items that are answered using a 4-point response format (1 = never, 2 = sometimes, 3 = often, and 4 = always and usually), but the Persian version that was used was slightly changed, and the participants with suicidal thoughts were asked to use this program in the form of a daily program for 95 days. Performance reports of the health-promoting lifestyle program were collected daily from the participants, and the information was categorized.
| Use of Mental and Physical Care Programs | Repeating Motivational Statements Daily, before Starting Work, while Resting, and before Sleeping |
|---|---|
|
I request information from experts on how to properly take care of myself
I participate in training programs in the field of personal health care I check my heart rate while doing sports I discuss health concerns with health professionals I report unusual symptoms of the disease to the doctor or other health personnel I discuss my problems and concerns with people around me I read and watch TV programs or articles about maintaining and improving health I choose a diet that is low in fat or saturated fat and low in cholesterol I read the labels of packaged foods containing oils and sodium, such as canned goods, etc I ask health personnel such as doctors and other nurses to understand their orders I check my body at least once a month for signs of danger and physical changes If necessary, I will ask for advice or guidance I am supported by a group of people who care about me and care for me When I ask health experts, doctors and nurses about health issues, I like them to give me a lot of information |
I feel that I am progressing and growing in a positive direction I am satisfied with myself and feel relaxed I hope for the future I believe that my life is purposeful I strive to achieve my long-term life goals I am aware of the issues that are important to me in life Everyday life is interesting and challenging for me I feel connected to forces greater than myself I am supported by a group of people who care about me and care for me I create a balance between work and leisure time I am ready to learn new experiences |
| Strengthening and expanding social relations | Taming the mind |
|
I spend my time with close friends
I have a meaningful and satisfying relationship with others It is easy for me to express concern, love, and intimacy to others I find ways to create intimate and close relationships I am touched and touched by the people I care about I solve my problems through dialogue and agreement with others I easily praise others for their successes |
I use special methods to control my stress I focus on good thoughts while sleeping I sleep enough Every day, I set aside a few minutes to relax and relax my muscles I walk to avoid fatigue I accept the issues of my life that I have no power to change I practice relaxation and methods like yoga for 15-20 minutes daily |
| Exercise and physical activity | Follow a healthy diet |
|
I exercise during the normal activities of the day, such as walking at lunchtime, using the stairs instead of the elevator, parking the car in a place further from my destination and, walking to work, etc.
I participate in light to moderate physical activities, such as endurance walking, 5 days a week, 30-40 minutes each day. I do vigorous exercise at least 3 times a week for 20 minutes or more, cycling, brisk walking, running, etc. I have a regular exercise schedule. I spend my free time doing physical activities, such as swimming, cycling, etc I do stretching exercises at least 3 times a week During sports activities, my heart rate reaches the desired level |
I eat breakfast I limit the use of sugar and sweets I eat 3-5 servings of vegetables daily I only eat 2-3 servings of red meat, chicken, dry beans, eggs, and nuts per day. I eat 2-3 servings of milk, yogurt or cheese daily I only eat 2-3 servings of red meat, chicken, dry beans, eggs and nuts per day I eat fruit 2-4 times a day I eat 6-11 meals of bread, rice, and pasta every day |
2.3. Statistical Analysis
Version 25 of the SPSS program was used to examine the data. The participants' characteristics and their BSSI and DASS-21 scores were summed up using descriptive statistics like frequency and percentage. The relationship between suicidal ideation and other clinical and demographic factors was investigated using a chi-square test. In order to account for potential confounders in our investigation of suicidal ideation among HCWs, multiple linear regression analysis was utilized to identify the predictors of suicidal ideation based on variables strongly associated with the Chi-square test. Additionally, data analysis was conducted using ANOVA statistical tests. For every test, the significance threshold was fixed at 0.05. Completely missing cases were not included in the analysis. The average percentage of suicidal thoughts in Iranian HCWs with dangerous thoughts in 2023 after COVID-19 before and after using the health-promoting lifestyle program has been shown and determined by a one-way ANOVA test.
3. RESULTS
Twelve respondents, out of the 260 people who got the survey in its initial phase, either did not respond at all or answered it in part. Consequently, 248 people were the final study participants. A 95.3% response rate was obtained. All of these individuals' data were included in the analysis. According to the findings, the majority of participants are female, between the ages of 30 and 36, married, clinical specialists in their first year of residency, childless, living with a spouse, renting or owning a home, and without a history of mental health issues, drug or alcohol abuse, psychiatric disorders, family history of suicide attempts, or self-mutilation. The range of shifts per month on average was 0 to 7, and the amount of COVID-19 exposure at work was moderate. The bulk of participants had a history of COVID-19 infection, but none of them had been hospitalized or had lost a close member as a result of the virus. Approximately 33% of the individuals employed mental health services during the COVID-19 pandemic and had monthly incomes of less than 6 million tomans (≈200 euros). The majority of participants in our study did not exhibit suicidal ideation, according to the BSSI scores, although a sizable percentage did exhibit low- and high-risk suicidal ideation. Furthermore, a considerable proportion of participants reported moderate to extremely severe levels of stress, anxiety, and depression, and these disorders were also highly prevalent among them. Table 2 contains further demographic and clinical details.
| BSSI | ||||||
|---|---|---|---|---|---|---|
| Characteristic | No Suicidal Ideation N=179 (72.1%) | Low Risk Suicidal Ideation N=50 (20.1%) | High Risk Suicidal Ideation N=19 (7.66%) | Pearson ChiSquare Value | df | P-value |
| Gender | 1.432 | 2 | 0.324 | |||
| Female | 123(74.5%) | 31(18.7%) | 11(6.66%) | |||
| Male | 56(67.4%) | 19(22.8%) | 8(9.63%) | |||
| Age | 6.853 | 4 | 0.511 | |||
| 2229 | 31(68.8%) | 9(20%) | 5(11.1%) | |||
| 30–36 | 132(73.7%) | 36(20.1%) | 11(6.14%) | |||
| 37–40 | 16(66.6%) | 5(20.8%) | 3(12.5%) | |||
| Marital status | 6.358 | 4 | 0.214 | |||
| Married | 113(86.2%) | 13(9.92%) | 5(3.81%) | |||
| Single | 58(60.4%) | 27(28.1%) | 11(11.4%) | |||
| Divorced | 8(38%) | 10(47.6%) | 3(14.2%) | |||
| Specialty | 7.152 | 4 | 0.158 | |||
| Doctor | 104(88.1%) | 10(8.47%) | 4(3.38%) | |||
| resident | 32(47.7%) | 26(38.8%) | 9(13.4%) | |||
| Nurse | 43(68.2%) | 14(22.2%) | 6(9.52%) | |||
| Accommodation | 2.785 | 4 | 0.489 | |||
| Dormitory | 5(50%) | 2(20%) | 3(30%) | |||
| Rental home | 65(59%) | 34(30.9%) | 11(10%) | |||
| Personal home | 109(85.1%) | 14(10.9%) | 5(3.90%) | |||
| Having children | 0.211 | 2 | 0.875 | |||
| No | 147(72.7%) | 39(19.3%) | 16(7.92%) | |||
| Yes | 32(69.5%) | 11(23.9%) | 3(6.52%) | |||
| Living arrangement | 3.149 | 4 | 0.715 | |||
| Spouse | - | - | - | |||
| Relatives | 104(86.6%) | 11(9.16%) | 5(4.16%) | |||
| Peers | 67.6(69.5%) | 17(23.9%) | 6(8.45%) | |||
| - | 27(47.3%) | 22(38.5%) | 8(14%) | |||
| Personal history of suicide attempts | 27.685 | 2 | 0.002 | |||
| No | - | - | - | |||
| Yes | - | - | - | |||
| - | 177(75%) | 46(19.4%) | 13(5.50%) | |||
| - | 2(16.6%) | 4(33.3%) | 6(50%) | |||
| History of psychiatric disorders | 13.058 | 2 | 0.003 | |||
| No | - | - | - | |||
| Yes | - | - | - | |||
| - | 163(84%) | 23(11.8%) | 8(4.12%) | |||
| - | 16(29.6%) | 27(50%) | 11(20.3%) | |||
| Family history of suicide attempts | 11.658 | 2 | 0.004 | |||
| No | - | - | - | |||
| Yes | 174(29.6%) | 38(29.6%) | 14(29.6%) | |||
| - | 5(29.6%) | 12(29.6%) | 5(29.6%) | |||
| History of self mutilation | 17.882 | 2 | 0.001 | |||
| No | - | - | - | |||
| Yes | 177(74.6%) | 46(19.4%) | 14(5.90%) | |||
| - | 2(18.1%) | 4(36.3%) | 5(45.4%) | |||
| History of COVID19 infection | 0.289 | 2 | 0.745 | |||
| No exposure | - | - | - | |||
| No | 9(52.9%) | 5(29.4%) | 3(17.6%) | |||
| Yes | 17(62.9%) | 6(22.2%) | 4(14.8%) | |||
| - | 153(75%) | 39(19.1%) | 12(5.88%) | |||
| Number of shifts in a month | 9.654 | 4 | 0.038 | |||
| 0–7 | - | - | - | |||
| 8–14 | 138(95.8%) | 3(2%) | 3(2%) | |||
| 15 and above | 34(38.2%) | 41(46%) | 14(15.7%) | |||
| - | 7(46.6%) | 6(40%) | 2(13.3%) | |||
| COVID19 Work Exposure | 14.125 | 4 | 0.016 | |||
| High exposure | ||||||
| (Working in COVID19 wards or respiratory emergency) | 140(80.4%) | 26(14.9%) | 8(4.59%) | |||
| Moderate exposure | ||||||
| (Occasional visits or consultations in the COVID19 ward) | ||||||
| - | 39(52.7%) | 24(32.4%) | 11(14.8%) | |||
| History of admission due to COVID19 infection | 2.358 | 2 | 0.365 | |||
| No | - | - | - | |||
| Yes | - | - | - | |||
| - | 167(74.2%) | 43(19.1%) | 15(6.66%) | |||
| - | 12(52.1%) | 7(30.4%) | 4(17.3%) | |||
| Death of close persons because of COVID19 | 22.65 | 2 | 0.002 | |||
| No | - | - | - | |||
| Yes | - | - | - | |||
| - | 146(83.9%) | 22(12.6%) | 6(3.44%) | |||
| - | 33(44.5%) | 28(37.8%) | 13(17.5%) | |||
| Depression | 131.286 | 8 | 0.001 | |||
| No Depression | - | - | - | |||
| Mild | 38(97.4%) | 1(2.56%) | 0 | |||
| Moderate | 80(97.5%) | 2(2.43%) | 0 | |||
| Severe | 42(60%) | 27(38.5%) | 1(1.42%) | |||
| Very severe | 11(40.7%) | 13(48.1%) | 3(11.1%) | |||
| - | 8(26.6%) | 7(23.3%) | 15(50%) | |||
| Use of mental health services during COVID19 pandemic | 9.645 | 2 | 0.007 | |||
| No | - | - | - | |||
| Yes | - | - | - | |||
| - | - | - | - | |||
| - | 126(75%) | 31(18.4%) | 11(6.54%) | |||
| - | 53(66.2%) | 19(23.7%) | 8(10%) | |||
| Income per month | 8.655 | 4 | 0.036 | |||
| - | - | - | - | |||
| Less than 6 million Tomans (⁓200 €) | ||||||
| - | 18(78.2%) | 3(13%) | 2(8.69%) | |||
| 6–9 million Tomans (⁓200–300 €) | ||||||
| - | - | - | - | |||
| More than 9 million Tomans(⁓300€) | ||||||
| - | 143(72.5%) | 40(20.3%) | 14(7.10%) | |||
| - | - | - | - | |||
| - | 18(64.2%) | 7(25%) | 3(10.7%) | |||
| Anxiety | 73.652 | 8 | 0.001 | |||
| No anxiety | 101(97.1%) | 3(2.88%) | 0 | |||
| Mild | 33(84.6%) | 4(10.2%) | 2(5.12%) | |||
| Moderate | 27(40.2%) | 30(44.7%) | 10(14.9%) | |||
| Severe | 9(45%) | 7(35%) | 4(20%) | |||
| Very severe | 9(50%) | 6(33.3%) | 3(15%) | |||
| Stress | 85.364 | 8 | 0.001 | |||
| No Stress | 107(98.1%) | 2(1.83%) | 0 | |||
| Mild | 43(89.5%) | 3(6.25%) | 2(4.16%) | |||
| Moderate | 24(61.5%) | 12(30.7%) | 3(7.69%) | |||
| Severe | 3(8.82%) | 22(64.7%) | 9(26.4%) | |||
| Very severe | 2(11.1%) | 11(61.1%) | 5(27.7%) | |||
| Model | Unstandardized Coefficients |
Standardized Coefficients | t | P-value | |
|---|---|---|---|---|---|
| - | B | Std. Error | Beta | -0.415 | 0.863 |
| (Constant) | -0.212 | 0.352 | - | -0.408 | 0.721 |
| History of psychiatric disorders | -1.012 | 3.125 | 0.041 | 0.369 | 0.715 |
| History of Alcohol/substance use |
0.178 | 0.087 | 0.148 | 1.259 | 0.041 |
| Family history of suicide attempts | 2.998 | 1.265 | 0.157 | 3.278 | 0.007 |
| Personal history of suicide attempts | 5.256 | 0.0789 | 0.157 | 1.648 | 0.036 |
| History of self-mutilation | 8.458 | 1.325 | 0.186 | 2.663 | 0.001 |
| Number of shifts in a month | 0.325 | 0.75 | 0.146 | 2.364 | 0.034 |
| COVID-19 work exposure | 1.259 | 1.055 | 0.341 | 1.367 | 0.86 |
| Death of close persons because of COVID-19 | 1.489 | 0.936 | 0.118 | 3.156 | 0.03 |
| Use of mental health services during COVID-19 Pandemic | 1.658 | 0.874 | 0.64 | 1.367 | 0.169 |
| Income | -0.138 | 0.089 | -0.123 | -3.115 | 0.032 |
| Depression | 0.611 | 0.116 | 0.745 | 5.489 | 0.001 |
| Anxiety | 0.145 | 0.140 | 0.189 | 1.285 | 0.326 |
| Stress | 0.067 | 0.158 | 0.065 | -0.357 | 0.741 |
The Pearson chi-square test was used to examine the correlation between suicidal thoughts and other clinical and demographic factors. The analysis's findings are presented in Table 2. The results of the analysis demonstrated variables such as gender, marital status, specialized type, having children, living conditions, type of residence, history of COVID-19 infection, and history of hospitalization due to COVID-19 were not connected to thoughts of suicide. Suicidal ideation was substantially correlated with a person's history of mental illnesses, alcohol and drug abuse, family history of suicide attempts, personal history of suicide attempts, history of self-harm, and the number of shifts worked each month. Suicidal ideation was also substantially correlated with work exposure to COVID-19, with more exposure being associated with a higher risk of suicide ideation compared to a lower or no risk. Suicidal ideation was substantially correlated with the death of a loved one from COVID-19 and the use of mental health services during the pandemic, with higher use among high-risk individuals compared to low-risk individuals. Suicidal thoughts and income were substantially correlated, with lower income being more common in high-risk individuals than in no-risk or low-risk individuals. Suicidal ideation was substantially correlated with depression, anxiety, and stress; high-risk individuals were more likely to have higher levels of these three variables than low- or no-risk individuals. The study employed linear regression analysis to determine the characteristics that were evaluated as potential predictors of suicide. The regression model included only statistically relevant factors and the continuance score of suicidal thoughts based on the Chi-square test findings to determine the amount of explained variance (Table 3). Depression was the strongest predictor of suicidal thoughts, and all of these variables, with the exception of income, had a positive relationship with suicidal thoughts (p-value < 0.05).
After the completion of the 95-day period of using the HCWs program by health workers with low-risk and high-risk thoughts, the BSSI test was performed again, and the results are shown in Fig. (1). The findings demonstrated that in the third phase of the research, the percentage of suicidal thoughts in individuals with high suicidal-risk ideation dropped from 7.66% to 4.03% (p<0.05), and in individuals with low-risk ideation dropped from 20.1% to 13.30% (p<0.05) following 69 HCWs who experienced suicidal thoughts using the health-promoting lifestyle education program for 95 days (Fig. 1). The comparison of suicidal thoughts in Iranian healthcare workers with low-risk and high-risk thoughts before and after using the health-promoting lifestyle program is shown in Fig. (1).
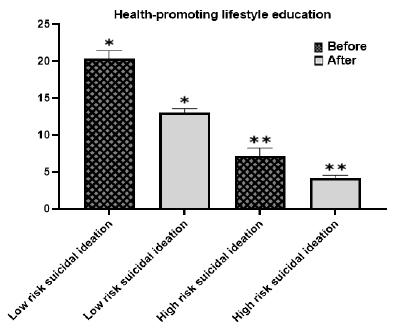
Col: One-way ANOVA. The average percentage of suicidal thoughts in Iranian healthcare workers with dangerous thoughts in 2023 after COVID-19 before and after using the health-promoting lifestyle program has been shown and determined (p<0.05).
4. DISCUSSION
The COVID-19 outbreak and spread have resulted in a rise in unemployment, social isolation, fatalities, and a decline in people's quality of life. The most recent WHO estimate states that as of November 16, 2023, there have been 6,980,000 deaths and 773 million confirmed cases globally. In Iran, there have been 14,6,000 reported deaths and 7,623,000 verified cases in total. A multicenter assessment of 1563 medical professionals conducted following the COVID-19 pandemic revealed that roughly 73.4% had traumatic stress, 50.7% had depression, 44.7% had general anxiety, and 36.1% had insomnia [2, 35]. These results should be taken into consideration while discussing mental health issues. A few years after the severe waves of the COVID-19 pandemic, the United States nursing staff survey revealed a rise in moral injury rates as a result of treatment decisions made with limited resources, higher levels of stress from work volume and intensity, and a newfound sense of vulnerability and fear for their own and their loved ones' safety [36, 37]. Similar findings were observed among nurses working in Egyptian hospitals during the epidemic; they reported higher levels of stress, lower job satisfaction, and a greater inclination to resign when faced with workplace stressors such as a heavy workload, exposure to mortality, personal worries, and stigma [38]. In particular, burnout rates rose during the pandemic despite the fact that rates of depressive symptoms and burnout stayed high in between time points. The results can point to long-lasting detrimental impacts on healthcare professionals' mental and physical well-being. There is ample evidence linking job stress to unfavorable psychological consequences. Very little research has been done to date on resilience processes and underlying factors that affect well-being, like perceptions and support in the workplace, that are related to the use of empirically supported individual-level treatments like (cognitive behavioral therapy or CBT) to improve mental health and well-being during and after a pandemic [4]. According to a study, the implementation of lifestyle training programs that promote health, as well as leaders' emotional support and sense of importance, are linked to the continuous distress of health care workers [1]. We are in favor of regular staff training in health care systems. Healthcare professionals could receive free or discounted access to fitness centers or swimming pools, fitness-focused digital apps, or weekly park runs, which are free 5km events held on Saturday mornings. Certain cardiac units in hospitals in London already use prescribed exercise, but only for patients [39]. It is anticipated that adding a weekly group fitness program for healthcare professionals will improve their mental health. According to one study, there was no discernible difference in the way nurses who took a daily probiotic pill and the placebo group felt about stress [40]. Nonetheless, we think that healthy food is an essential component of living a healthy lifestyle, and we advise that a balanced, nutritious diet be offered by paying for a nutritious meal or by offering information and training to promote the habit of eating healthily. The majority of lifestyle tactics are grounded in mindfulness. Programs for “mind management” and resilience frequently incorporate mindfulness. Programs for digital mindfulness, like headspace, may help mental health by lowering anxiety in difficult situations around the world, including the COVID-19 epidemic, and enhancing the quality of sleep for medical professionals under pressure [41]. We suggest that employers finance these digital programs, which frequently involve a paid subscription, for all healthcare professionals. That being said, we think there may be more effective ways to distribute mindfulness therapies. For instance, it has been demonstrated that a weekly meditation program led by a therapist via a digital messaging app lowers stress, anxiety, and depression particularly in the context of HCWs [1]. While online mindfulness programs can be beneficial, we believe that more conventional, non-digital methods of mindfulness, such as one-on-one and in-person group meditation sessions, can be more successful but may come at a higher expense. It will cost money if a therapist is required to conduct sessions or instruct medical staff. Programs that teach transcendental meditation, for instance, may be useful in lowering anxiety and burnout. HCWs are particularly vulnerable to variables like exposure to potentially dangerous ethical situations, lack of confidence in voicing safety concerns and taking appropriate action, feeling unsupported by supervisors, and decreasing the standard of care. Suicidal ideas are becoming more prevalent among them [42]. Although not specifically addressing suicidal ideation as a symptom, psychological treatments like interpersonal therapy are helpful in lowering suicidal ideation by reducing overall depressive symptoms and should be prioritized [43]. The degree to which rates of poor mental health have risen since the pandemic is up for debate, although it is well acknowledged that, even before the pandemic, HCWs were especially susceptible to poor mental health. Moreover, this pandemic aggravated these existing vulnerabilities [44]. The review pointed out that adaptable treatments that are suitable for the local context and culture are essential for the successful implementation of programs. Effective communication, network coherence, a supportive learning environment where team members feel appreciated and involved in the process of change, and enough time and space for introspection and assessment are all crucial. Health-promoting lifestyle education makes it possible to implement a long-term strategy that includes sharing and learning from peers, talking with coaches, and setting aside time to take action, among other tactics for self-care that are based on current stress levels and concerns. The support is not very big. Our viewpoint, supporting data from our observations, a summary of the approaches we have suggested, and successful interventions in a controlled clinical trial are all included in this article.
CONCLUSION AND RECOMMENDATIONS
The COVID-19 pandemic has had an adverse effect on HCWs' risk factors for suicide. In the wake of COVID-19, this study aimed to increase the usage of the peer support intervention stress first aid among HCWs. The results show some promise for improving employee understanding and use of health resources, as well as influencing the culture around the conversation about emotional health through health-promoting lifestyle education. No matter their current state of mental health, all healthcare professionals should participate in mind management, resilience, and coping skills programs as they are useful in preventing burnout, stress, and negative mental impacts. Numerous delivery modalities are available for these programs, such as online modules, digital programs, or in-person group meetings. These therapies' efficacy is variable but still reasonable and appears to be most associated with improved mental health. The results of this study have consequences for clinical practice and those who create health policies. Understanding educational programs and psychology is important for developing effective treatment strategies for treatment staff. In addition, the findings of this study highlight the need for more careful monitoring of the treatment staff's performance, especially those who are facing problems. Early identification and management of mental disorders can help improve the functional outcomes of the study subjects and reduce long-term complications. The results showed that healthcare workers who were less able to adhere to the health promotion program were more exposed to risky thoughts.
RECOMMENDATIONS
1. More research: Check out more mind management, resilience and coping skills programs. This will help develop targeted therapies and improve low-risk and high-risk conditions for health care workers.
2. Promotion of mental health measures: stress first aid, peer support intervention among health care professionals, in health centers should be prioritized.
LIMITATIONS AND STRENGTHS OF THE STUDY
This survey exclusively included medical staff from hospitals in the province of Semnan. As such, care should be taken when extrapolating the results. Long-term, thorough research is advised in order to increase the precision with which low-risk and high-risk situations are described. Because this study was one-sample longitudinal in nature, inferences regarding causality are challenging to make. It is recommended that future research be done at different hospitals with a larger sample size in light of the aforementioned constraints in order to increase the reliability of the results.
AUTHORS’ CONTRIBUTIONS
E.A.: Study conception and design; M.H.G.: Data collection; R.R.: Draft manuscript.
LIST OF ABBREVIATIONS
| HCWs | = Healthcare Workers |
| HPLPII | = Health-promoting Lifestyle Profile II |
| DASS-21 | = Depression, Anxiety, and Stress Scale |
| BSSI | = Beck Scale for Suicidal Ideation |
| CBT | = Cognitive Behavioral Therapy |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has been approved by the Ethics Council of Damghan Azad University, Iran with the code of ethics (IR.IAU. DAMGHAN.REC.1400.005).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.


