All published articles of this journal are available on ScienceDirect.
Multifaceted Therapeutic Approaches for the Management of Dyspareunia: A Narrative Review
Abstract
Background
Dyspareunia is a complex health issue in women and causes an increased risk of sexual dysfunction, relationship conflict, mood disorders, and decreased quality of life. This narrative review aimed to explore the different therapeutic approaches for managing this complex health problem among the women population.
Materials and Methods
Articles published in English in Google Scholar, PubMed, Scopus, ScienceDirect, Embase, CINAHL, Cochrane Library, and SAGE databases from 2017 to 2023 were searched. Twelve studies with dyspareunia as the primary clinical problem were chosen. The clinical efficacy of pelvic floor muscle training, perineal massage, biofeedback, manual therapy, dilator therapy, extracorporeal shockwave therapy, and visceral manipulation in the management of dyspareunia was evaluated in these articles.
Results
The literature review revealed that diverse interventions offer valuable options for managing dyspareunia, which can be tailored care to the individual patient’s requirement based on clinical evaluation decisions. This study summarized the multi-modal adjuvant therapeutic options for dyspareunia management.
Conclusion
From this review, it could be concluded that there is no consolidated evidence regarding the relative efficacy or effectiveness of various therapeutic interventions for managing dyspareunia. In light of the findings of this review, it could be safely said that a patient-centric eclectic approach incorporating different therapeutic modes will be most appropriate for the management of dyspareunia.
1. INTRODUCTION
Dyspareunia is a complex health issue in women that often goes neglected, and women with sexual pain are at an increased risk of sexual dysfunction, relationship distress, mood disorders, anxiety, depression, and decreased quality of life [1-3]. It can be described as periodic and unremitting pain during or attempting coitus [4]. According to DSM-V, dyspareunia comes underneath the Genito-Pelvic Pain/Penetration Disorders (GPPPD) classification of sexual dysfunction, and few clinicians still label dyspareunia and vaginismus terms differently [5, 6]. According to DSM-V, genito-pelvic pain/penetration disorder has been defined as persistent or recurrent difficulties with one (or more) of the following: i) vaginal penetration during intercourse, ii) marked vulvovaginal or pelvic pain during vaginal intercourse or penetration attempts, iii) marked fear or anxiety about vulvovaginal or pelvic pain during coitus, and iv) marked tensing or tightening of the pelvic floor muscles during attempted vaginal penetration [5]. Globally, the prevalence of sexual pain dysfunction- dyspareunia is estimated to vary from 3% to 18%. This wide variation is due to heterogenicity in methodologies of prevalence studies [7-12].
Dyspareunia can be further categorized into superficial (pain at the level of introitus) and deep dyspareunia (pain in the pelvis) [7]. Moreover, the etiologic complexities of this female disorder encompass infectious, inflammatory, structural, neoplastic, traumatic, hormonal, dermato- logical conditions (lichen sclerosis, lichen planus, contact dermatitis), vaginitis, interstitial cystitis, inadequate lubrication of the vagina, atrophy of the vaginal muscles, vaginismus, vulvodynia, pelvic floor disorders, ovarian masses, uterine retroversion, adhesion and inflammation in the pelvis, endometriosis, and history of sexual abuse [1, 5].
Non-judgemental history taking by conversing with the patient regarding pain, sexual issues, and any history of abuse and gathering in-depth information about medical/ surgical and obstetric information, conducting a bimanual examination, reviewing medications, evaluating the use of personal hygiene products may direct for an early diagnosis [11]. However, women suffering from this disorder usually have psychological effects due to painful coitus leading to anxiety, fear, frustration, and perceiving themselves as being inadequate, while accessibility issues to healthcare, miscommunication, and hesitancy to share about sexuality act as catalysts that make this disorder a more complex one [13, 14]. Treatment approaches solely be based on the etiology of patient’s complaints, which includes medical and surgical management with lubricants, moisturizers, vaginal estrogen, ospemifene, dehydroepiandrosterone, local testosterone therapy, cannabidiol, fractional CO2 laser treatments [13], vaginal dilation surgery under anesthesia [14], vestibulectomy [15], hymenectomy [16], vaginal rejuvenation surgery [17], and labiaplasty [18]. In most cases, pelvic floor physical therapy serves as an adjuvant treatment option with pelvic floor muscle training, electrical stimulation, thermo- therapy, perineal massage, manual therapy, biofeedback, shockwave therapy, visceral therapy, dilator therapy, etc. [19, 20]. However, the recommended line of treatment faces difficulties in incorporating it due to the potentiality of many types of barriers. As dyspareunia is an under-researched condition and affects many women with physical, psychological, and behavioral manifestations, reviewing different physical therapeutic approaches could help fill the void in knowledge to improve the health maintenance and care of women. Adopting evidence-based self-reported outcome measures for identifying the complexity associated with this sexual pain dysfunction may direct to planning an effective therapeutic approach to address the problems associated with the condition. Therefore, to clarify the clinically relevant problems, we reviewed the literature to highlight the conservative multifaceted therapeutic approaches to mark this complex disorder, which often goes unnoticed and neglected.
2. METHOD
This narrative review was conducted to examine various therapeutic approaches for managing dyspareunia. Articles published in Google Scholar, PubMed, Scopus, ScienceDirect, Embase, CINAHL, Cochrane Library, and SAGE databases from 2017 to 2023 were searched. Articles published in the English language were searched using the following keywords and their matches: “Genito-pelvic pain/penetration disorder”; “female sexual dys- function”; “Genito pelvic pain penetration disorder”; “GPPPD”; “vaginismus”; “dyspareunia”; “sexual dysfunction”; “painful sex”; “sexual pain”; “genital pain”; “physical therapy”; “physiotherapy”; “vulvodynia”; “painful coitus”; “non-conservative management”; “electrotherapy”; “treatment”; “exercise therapy” used along with the Boolean operators “OR” and “AND”. Further 74 articles were found to be relevant on the chosen topic.
Solely based on the inclusion and exclusion criteria, 12 articles were deemed to be important. The research articles were typically considered for inclusion if they were descriptive, analytical, or review studies with content relevant to dyspareunia. Articles that provided information on secondary dyspareunia and if the literature content was outside the scope of this narrative review were considered for exclusion. The reference list used in the articles was examined to ensure the extensiveness of the search. The participants in the included studies were women with genito-pelvic pain/penetration disorder and dyspareunia, with unbounded age limitations. The outcomes of these studies were measures of pain, pelvic floor muscle function, sexual function, psychological symptoms of anxiety, depression, and quality of life.
2.1. Search Strategy
Seventy-four articles were identified, out of which 30 were removed for duplicity, and 44 articles were screened for eligibility. Twelve articles were included according to the criteria set by the authors. The results of the literature search strategy are described in a flow chart in Fig. (1).
3. RESULTS
3.1. Characteristics of the Articles
Twelve articles were included and summarized, which are presented in Table 1. According to the hierarchy of level of evidence from top to bottom, three systematic reviews examined the efficacy of manual treatment, antenatal perineal massage, and pelvic floor muscle training [23, 29, 31], and each demonstrated its effective outcome in managing the symptoms of dyspareunia. Two Randomized Controlled Trials (RCTs) and one non-randomized controlled trial showed the efficacy of pelvic floor muscle training [20-22], while a third RCT found that transvaginal massage improved dyspareunia symptoms [25], indicating that a multifaceted intervention may sound to be more effective in treating this sexual dysfunction rather than stand-alone treatment. The Valsalva maneuver also reduced chronic pelvic pain linked to dyspareunia by increasing the levator hiatus area [27] with anatomical consideration. In a pilot trial [24], pelvic floor physiotherapy improves the tonicity of the pelvic floor muscles and outperforms both superficial and deep dyspareunia. The pain associated with penetrative vaginal dysfunction was significantly reduced or resolved when low-dose high-frequency movement-based dilator therapy was used, according to a retrospective study conducted [26]. A qualitative review examined whether the acceptability of multimodal PFPT was satisfactory for gynecological cancer survivors with dyspareunia [30]. Moreover, a literature study found that visceral therapy is an excellent addition to traditional gynecological treatments [28]. In general, the interpretation of the result showed that each of the therapy modalities seems to be beneficial in managing the symptoms. However, none of the studies address the management based on the etiological complexity of the dyspareunia. Therefore, commenting on the efficacy of each treatment method seems to be promising. Table 2 summarizes the different physical therapeutic interventions- therapeutic benefits with the level of evidence.
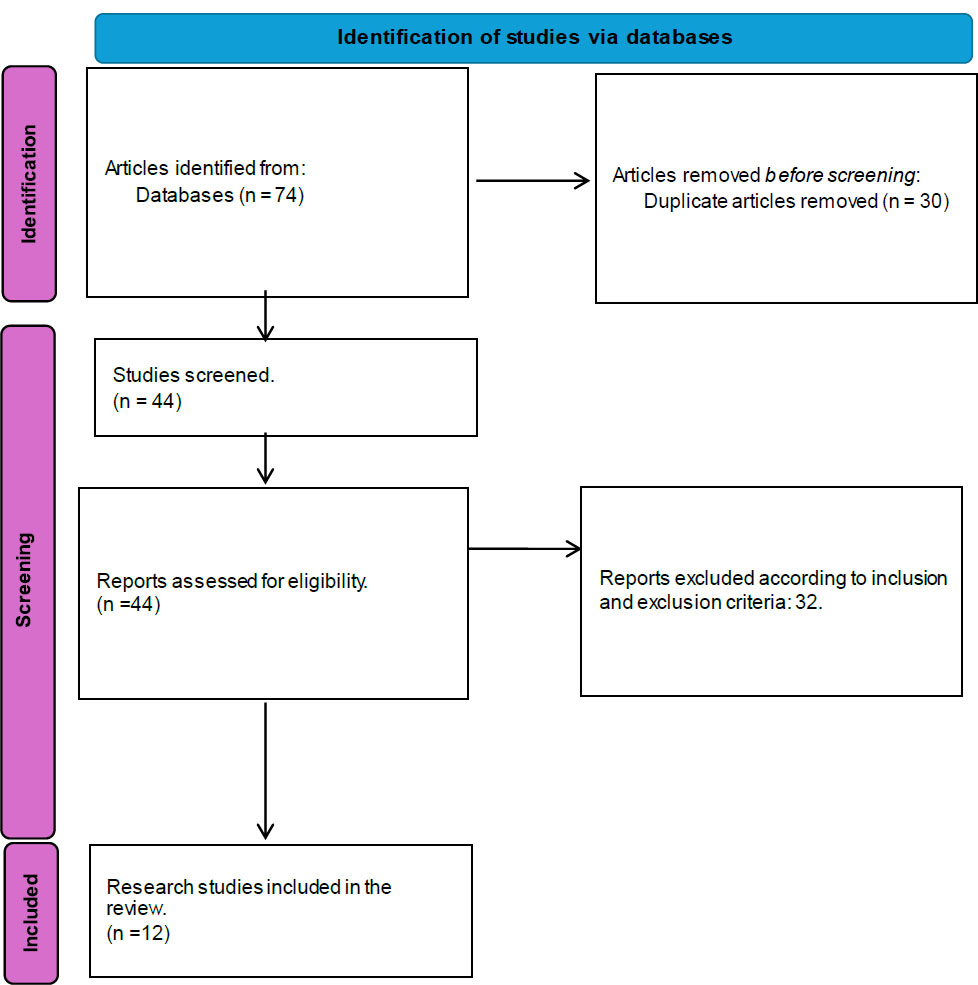
Search strategy.
| Author/Year/Refs. | Study Design | Participants | Outcome Measures | Findings/ Outcomes | Conclusion |
|---|---|---|---|---|---|
| Da Silva et al. 2017 [21] | Non-randomized control trial | Eighteen women with a diagnosis of dyspareunia grouped into the dyspareunia (n=8) received PFMT and the chronic pelvic pain group (n=10), which received placebo treatment. | Visual Analogue Scale, McGill Pain Index, Female Sexual Function Index, and Hospital Anxiety and Depression Scale (HADS) | A significant improvement in symptoms of dyspareunia was measured by VAS and McGill Pain Index (p < 0.001) in either group, while there were no significant differences in HADS scores. The dyspareunia group showed improvements across all outcomes, and the CPP group showed improvement only in the pain domain. | Transvaginal massage using the thiele technique effectively alleviates dyspareunia attributed to pelvic floor muscle tenderness, providing durable relief from pain. |
| Schvartzman et al. 2019 [20] | Randomized control trial | Women with dyspareunia (40-60 years) were randomized into the first group (n = 21), received five one-hour sessions of infrared therapy for relaxation of PFM, myofascial release, and pelvic training (PFMT group); and the second group (n = 21) received five one-hour sessions of thermotherapy to lower back with myofascial release of the abdominal diaphragm, piriformis and iliopsoas muscles. | Visual Analogue Scale (VAS), Female Sexual Function Index (FSFI), quality of life (QOL), and PFM function. | Pain scores in the PFMT group decreased from 7.77±0.38 to 2.25±0.30 on VAS and in the LB group from 7.62±0.29 to 5.58±0.49. | Pelvic floor muscle training protocol effectively improved pain, quality of life, sexual function, and pelvic floor muscle function. |
| Ghaderi et al. 2019 [22] |
Randomized control trial | Sixty-four women with dyspareunia were randomized into the experimental group (n = 32) and received electrotherapy, manual therapy, and PFM exercises and the control group (n = 32) received no treatment while on the waiting list. Evaluations of PFM strength and endurance, sexual function, and pain were assessed pre and post-3 months of treatment and at 3-month follow-up. | Female Sexual Function Index, (FSFI), visual analogue scale (VAS). |
A significant improvement was noted in the experimental group. The mean difference in PFM strength between groups was 2.01, and in endurance was 6.26 s. The mean difference in FSFI score and VAS was 51.05 and 7.32, respectively. | Pelvic floor rehabilitation is an important part of a treatment approach to dyspareunia, and genito-pelvic pain and dysfunction require a multifaceted intervention. |
| Trahan et al. 2019 [23] | Systematic review | Works of literature from 1997 - 2018 were systematically reviewed, in which 1 RCT and 3 observational studies where 18- 75 years females with dyspareunia were intervened with manual therapy (massage, trigger point therapy, myofascial release, pelvic manipulation, or graded exposure) as a treatment. | FSFI, VAS, McGill Pain Index, HADS, Mankoski Pain Scale, Numerical Rating Scale (NRS), and the Patient Global Impression of Improvement Scale | The primary outcome assessed the pain subscale of the female sexual function index. All studies demonstrated notable enhancements in the pain domain of the Female Sexual Function Index (P < 0.5), supporting manual therapy as an effective approach. | Endorse manual therapy effectiveness in reducing intercourse-related pain. |
| Del Forno et al. 2020 [24] | Pilot study | Superficial and deep dyspareunia were evaluated by numerical rating scale and the levator hiatus area (LHA) using 3-D/4-D trans perineal ultrasound, and each participant received five individual sessions of ultrasound visual feedback-assisted pelvic floor physiotherapy. Dyspareunia and LHA were reassessed at one month post-therapy session and compared with pre-therapy assessment. | NRS Score, Levator Hiatus Area, Valsalva Manoeuvre, PFM function | NRS scores significantly decreased for both superficial dyspareunia and deep dyspareunia, with p-values of 0.0027 and 0.0385. Post-therapy, LHA values were significantly larger at rest (11.5 ± 2.4 cm2 vs. 10.4 ± 2.1 cm2 at maximum pelvic floor muscle contraction (10.5 ± 2.1 cm2 vs. 9.5 ± 3.0 cm2) and at maximum Valsalva maneuver (14.0 ± 2.5 cm2 vs. 12.0 ± 2.2 cm2). | Pelvic floor physiotherapy improves superficial and deep dyspareunia symptoms and promotes pelvic floor muscle relaxation. |
| Del Forno et al. 2021 [25] |
Randomized controlled trial | Thirty nulliparous women with a diagnosis of DIE and superficial dyspareunia randomized into 17 (study group) and 13 (control) underwent 3D/4D trans-perineal ultrasound to measure levator hiatal area (LHA) at rest during maximum pelvic floor muscle contraction and at maximum Valsalva maneuver. Follow-up assessment at four months. | NRS, LHA during maximum Valsalva maneuver, at rest, and on maximum PFMC | The percentage change in LHA on maximum Valsalva maneuver between the two examinations was higher in the study group than in the control. A significant difference between the PFP and control groups in chronic pelvic pain was noted. |
In women with DIE, PFP seems to increase LHA on the Valsalva maneuver, leading to improved superficial dyspareunia, chronic pelvic pain, and pelvic floor muscle relaxation. |
| Miles & Miles 2021 [26] | Retrospective study | Twenty-six premenopausal women who were referred to pelvic floor physical therapy for dyspareunia completed a course of movement-based dilator therapy and underwent 2 - 6 pelvic floor physical therapy visits in a span of 0 to 44 weeks. | NPRS with intercourse | The mean pain score decreased significantly from 8.3 ± 2.2 (pre-treatment) to 1.3± 2.0 (post-treatment), and 58% of patients reported complete resolution of dyspareunia. | Utilizing low-dose, high-frequency movement-based dilator therapy led to a significant reduction or resolution of pain associated with penetrative vaginal disorder. |
| Hurt et al. 2021 [27] | Prospective, randomized, double-blind, placebo-controlled study | Sixty-one women with dyspareunia were randomized into treatment and placebo groups and received perineal ESWT weekly for 4 weeks, while the placebo group received placebo stand-off treatment. The severity of dyspareunia was assessed at pre-, post-treatment, and follow-up (1, 4, and 12 weeks) after the final ESWT session. | Marinoff Dyspareunia Scale, visual analogue scale | The treatment group exhibited differences on the Marinoff Dyspareunia Scale and VAS score. The effect sizes were both large: Marinoff 0.825 and VAS 0.883. | Extracorporeal Shockwave Therapy significantly alleviated the subjective component of pain among women with dyspareunia. |
| Wojcik et al. 2022 [28] | Literature review | - | - | Visceral therapy aims at restoring intra-organ movement, reducing tension, focusing on the area of the two cylinders of the trunk, and supporting the functioning of the vascular system in the vicinity of the uterus. | Apart from standard treatment methods used in gynecology and sexology, physiotherapy with visceral therapy is of great value in dyspareunia management. |
| Fernández-Pérez et al. 2023 [29] | Systematic review | With retrieved literature from Scopus, Medline, PubMed, CINAHL, and Web of Science, a sample of 1401 women with dyspareunia from different research was studied. | - | Included articles- multimodal physiotherapy (6), electrotherapy (5), Thiele's massage (3), interdisciplinary interventions or pelvic floor muscle training (2), and extracorporeal shockwave therapy (1 article) were meta-analyzed, and the result showed improvement in pain intensity and quality of life in a patient with dyspareunia. | Physiotherapy techniques, such as perineal muscle strengthening, transcutaneous electrical nerve stimulation, Thiele massage, and manual trigger point release therapy, reliably improve pain and quality of life in dyspareunia patients. |
| Cyr et al. 2023 [30] | Qualitative review | Twenty-eight gynecological cancer survivors with dyspareunia participated in a 12-week multimodal PFPT treatment in which semi-structured telephone interviews were conducted to gather qualitative data on women's perspectives and experiences of the treatment. | Female Sexual Function Index, Female Sexual Distress Scale-Revised, Body Image Scale, Beck Depression Inventory, International Consultation on Incontinence Questionnaire |
All participants were assessed in a theme-based format. Theme 1: treatment appropriateness, physical therapist care delivery; Theme 2: Treatment intensity demands; Theme 3: treatment affects motivation, participation, and beliefs. | Explored the acceptability of Multimodal PFPT and found it to be acceptable for gynecological cancer survivors with dyspareunia. |
| Milka et al. 2023 [31] | Systematic review | Literature encompassed from PubMed, Web of Science, Scopus, and Embase databases | VAS, Verbal Rating Scale, KHQ, ICIQ-SF, ICIQ-UI-SF | Various techniques and timings for conducting APM procedures were highlighted in 18 publications that were considered for review and investigated the risk of perineal injuries, such as tearing and episiotomy, postpartum pain, postpartum urinary-fecal incontinence, and dyspareunia. | APM serves as a protective measure against perineal injuries during labor and decreases the likelihood of experiencing fecal and gas incontinence in the postpartum period, but its effectiveness on dyspareunia seems to be doubtful. |
| Therapeutic Interventions/Refs. | Clinical Applicability | Therapeutic Effects | Level of Evidence |
|---|---|---|---|
| Pelvic floor training/rehabilitation [22,24,22,22,30,32,65] | Sexual dysfunction, dyspareunia, gynecological cancer state management | Improve pelvic floor muscle tone and coordination | I, II, IV |
| Biofeedback [33, 35] | Chronic pelvic pain, dyspareunia, hypertonic pelvic floor | Visual-assisted training to strengthen or relax pelvic floor muscles to improve bowel or bladder function and decrease some types of pelvic floor pain | II, III |
| Perineal massage [21,31,37,38,63] | Ease labor, levator ani injuries, dyspareunia | Increases perineal integrity and flexibility and improves pelvic floor muscle functions. | I |
| Manual therapy [29,41-43,64] | Pelvic pain condition, dyspareunia, orgasm dysfunction, infertility, menopausal symptoms | Reduce pain intensity, release tension throughout the pelvic musculature, | I, II, III |
| Vaginal dilator [26,46,48,49] | High-tone pelvic floor dysfunction, superficial dyspareunia, vaginal atrophy, agenesis, post-radiation adhesion | Reduce pelvic pain, stretch out vaginal tissues and opening, increase vaginal length, relaxation of pelvic floor muscles. | I, IV |
| Extracorporeal shock wave therapy [27,50,52-54] | Chronic perineal/pelvic pain, sexual pain, dyspareunia, vulvodynia, | Trigger the release of growth and anti-inflammatory factors, reduce subjective pain perception | II, III |
| Visceral therapy [28,56,58,62] | Pelvic floor disorders, painful sexual dysfunction | Encourage the normal mobility, tone, and inherent tissue motion of the pelvic viscera, their connective tissue, reduce pelvic pain | IV |
4. DISCUSSION
4.1. Pelvic Floor Muscle Training/ Rehabilitation
Pelvic Floor Muscle Training (PFMT) involves a combination of two or more interventions, such as manual therapy techniques and other modalities, to enhance the functioning and strength of the to-be-trained muscles. With the literature review, we identified three randomized controlled trials for PFMT. In an RCT by Ghaderi F et al., participants in the experimental group received a treatment program consisting of digital biofeedback, intravaginal manual techniques, supervised pelvic floor muscle exercises, and electrotherapy with high-frequency transcutaneous electrical nerve stimulation (TENS) at 110 Hz for 80 ms pulse duration and maximal tolerable intensity to relieve pain, and the study resulted that pelvic floor rehabilitation program improves genito-pelvic pain, sexual function, pelvic floor muscle (PFM) strength, and endurance in women with symptomatic dyspareunia [22]. Another RCT by Schvartzman R et al. concluded that pelvic floor muscle training improves pain, pelvic floor muscle functioning, sexual function, and quality of life in women with dyspareunia [20]. Del Forno S et al. suggested that pelvic floor muscle training requires an informative session, digital evaluation, and physio- therapeutic measures. It restored the normal pelvic floor tone and improved muscle coordination [25].
In a 12-week therapy program for gynecological cancer survivors women with dyspareunia, which was part of the qualitative analysis by Cyr et al. in 2023, participants learned about the pathophysiology of dyspareunia and several pain-reduction tactics, such as the use of moisturizing agents, lubricants, breathing exercises, relaxation and therapeutic electromyography biofeedback, and manual therapy approaches, and the same study result suggested that multimodal pelvic floor physical therapy found to be acceptable for gynecological cancer survivors with dyspareunia in terms of symptomatic measures [30].
In a recent systematic review by Fernández-Pérez P et al., literature reflected that multimodal care with TENS, infrared therapy, myofascial release, intravaginal massage, perineal stretching, abdominal training, pelvic floor muscle training, extracorporeal shockwave therapy, transvaginal massage, and Thiele's massage as combination therapy and in conjunction with other treatment means, such as diazepam, or hormonal therapy, are quite efficacious in reducing pain intensity, the severity of dyspareunia, sexual distress, catastrophism, anxiety and improve perineal function, lubrication, and levator ani muscle contractility as well as dramatically change the quality of life among women with dyspareunia [29].
Awareness and general education related to the anatomy of the pelvic floor to make them aware of how to command their pelvic floor tone to increase muscle recognition and proprioception may assist in improving muscle tissue elasticity, its relaxation, and restoration of normal activity, which then helps to reduce pain in this sexual disorder [22, 32]. Therefore, focusing from the etiological perspective on the quality of adherence to exercise of pelvic floor muscle will direct to achieving the desired results of relieving dyspareunia symptoms of pain and associated problems.
4.2. Biofeedback
The learning and developing of self-control over physiological processes with visual, acoustic, and verbal feedback is achieved with biofeedback therapy in which autonomic and neuromuscular activity is measured basically to intervene in function that is otherwise outside awareness or under less voluntary control [33]. Biofeedback-assisted training is also one of several effective physical therapy techniques, with evidence that it positively affects pain reduction, overall symptom relief, and quality of life [33]. Moreover, biofeedback is also one of the several physiotherapy techniques that manage myofascial pain syndrome, pain in pelvic floor musculature and connecting fascia that may occur alone with no concomitant medical pathology, or it may exist as sequela to urological, gynecological, and colorectal medical conditions or other muscular-skeletal-neural problems [34]. Aalaie et al. concluded that biofeedback and electrical stimulation favor the Female Sexual Function Index score in patients with sexual dysfunction and stress incontinence, and the researcher suggested that to improve sexual function, biofeedback seems to benefit more than those receiving electrical stimulation [35].
Del Forno et al. intervened in deep endometriosis and dyspareunia problems with five individual sessions of PFM physiotherapy of 30 minutes each at alternative weeks 1, 3, 5, 8, and 11; during the first session itself, patients were given education regarding the pelvic floor muscles and five individual ultrasound-visual feedback-assisted pelvic floor physiotherapy sessions and the results showed favorable outcome, indicating PFM physiotherapy seems to increase levator hiatal area (LHA) leading to improved superficial dyspareunia, chronic pelvic pain, and pelvic floor muscle relaxation in women [25]. With this context, the prescription of biofeedback therapy is mainly directed to address the hypertonic state of the pelvic floor muscle, basically when considering the symptoms of dyspareunia, and its application may require combination therapy with other means or modalities for achieving a desired result.
4.3. Perineal Massage
Therapeutically, perineal massage has different applications, such as antenatal perineal massage and Thiele massage. In the past, perineal massage has been conventionally used in the antenatal period; therefore, it is also known as antenatal perineal massage (APM). It involves stretching the pelvic floor lining in preparation for labor to ease pain and discomfort, and it is known to reduce the incidence of episiotomy, third- and fourth-degree perineal tears, postpartum perineal pain, and anal incontinence [36]. APM is useful in reducing perineal trauma pain [37] and anal sphincter injury [38], and only a handful of studies have established a positive correlation of therapeutic perineal massage with the treatment of dyspareunia. Another massage technique, Thiele massage, is a scar reduction technique that appears to be very helpful for women with chronic pelvic pain caused by tenderness of the levator ani muscle and dyspareunia [21, 39]. Gommesen et al. found the association of perineal length with the risk of dyspareunia and suggested minimizing the extent of perineal trauma to manage the dyspareunia symptoms [40]. A systematic review by Milka et al. identified two RCTs where experimental groups received APM 5–10 minutes per day, but there were no specifications about how the technique was administered [31]. Perineal massage is theorized to work because it might increase the flexibility of the soft tissues and decrease the hypertonicity of the musculature around the perineum. In addition to it, because of the assertive preconceived notions of the procedure, it might motivate the patient to adhere to the massage, which might result in vaginal birth [37]. With this limited evidence, it can be stated that Thiele massage may improve dyspareunia symptoms, albeit with variations in outcomes across different aspects of sexual function.
4.4. Manual Therapy
Manual therapy (MT) procedures are the recommended course of treatment for many musculoskeletal pain syndromes [41], and their applicability is entirely based on clinical reasoning. Biomechanical, neuro-physiological, psychological, and non-specific characteristics function as mediators or moderators for treatment to be more insightful [42]. MT has also been widely incorporated to treat gynecological and obstetrics conditions, such as infertility, dys- menorrhea, pelvic pain, and menopause [43]. Wurn et al. suggested that cases of orgasm dysfunction and dyspareunia can be treatable by a distinctive site-specific protocol of manual soft-tissue therapy, and the therapy also seems to improve other aspects of sexual dysfunction [44]. In a systematic review, Trahan et al. examined the efficacy of manual therapy in reducing pelvic pain among females with dyspareunia and concluded that manual therapy is a non-invasive, non-surgical intervention that could be an addition to current gynecological and medical treatments of sexual pain [23]. However, further literature is required to develop evidence-based guidelines for the management of dyspareunia using manual therapy techniques.
4.5. Vaginal Dilator Therapy
A vaginal dilator is a smooth and cylindrical tool that comes in variable sizes and is used to minimize vaginal stenosis and scarring, prevent adhesions, promote improved vaginal healing, relax pelvic floor muscles, and prevent pain [45-47] and is generally indicated for gynecological cancers, Mullerian agenesis, dyspareunia, and pelvic floor disorders [48]. It has been shown more effective than the finger technique, which involves the use of one or two fingers to dilate the vaginal opening according to the level of spasm and state of the dysfunction [49]. Movement-Based Dilator Therapy (MBDT) is another intra-vaginal dilator method using non-threatening or painless exposures for those patients who classically experience pain with vaginal penetration, and this neurophysiological proprioceptive neuromuscular facilitation (PNF)-contract-relax technique uses a 1:2 ratio of contraction to relaxation and can be applied systematically to produce a desirable effect on the puborectalis, pubococcygeus, iliococcygeus, and obturator internus muscles bilaterally [26]. Miles et al. found that 58% of patients experienced complete resolution of dyspareunia with MBDT, and based on the evidence, it was concluded that MBDT could be classified as a time-limited adjunct for chronic pelvic pain with a dyspareunia symptom, especially in premenopausal patients [26]. Though vaginal dilator therapy seems to be a promising therapeutic option, psychosocial barriers, such as unfavorable accompanying symptoms, negative perceptions, uncertainty, and other unhelpful circumstances, may reduce adherence to the therapy, hence thereby reducing its effect. Further, positive communication and rapport with healthcare providers, patient support programs [45], psychological counseling, and relaxation therapy may thereby assist the patient in overcoming those emotional obstacles.
4.6. Extracorporeal Shockwave Therapy
Extracorporeal Shock Wave Therapy (ESWT) is known for its fewer adverse effects in treating musculoskeletal disorders, such as tendinopathies, spasticity, wounds, and delayed fracture healing [50]. The therapeutic appli- cability of ESWT is well-established in the literature related to specific gynecological dysfunction [27]. The physical forces generated by low-intensity shockwaves affect tissue mechanics and can trigger the release of growth and anti-inflammatory factors [51, 52]. Although it is known that the effect of ESWT is intensity-dependent, it seems to reduce pain perception even in the treatment of vulvodynia [53, 54].
Hurt et al., in an intervention study, administered weekly perineal ESWT for four consecutive weeks to a total of 4000 pulses with treatment parameters with the inclusion of an energy flux density of 0.35 mJ/mm2, frequency of 4 Hz, focus zone spanning from 0 to 30 mm, and therapeutic efficiency from 0 to 90 mm, and the results suggested that ESWT significantly reduced subjective pain associated with dyspareunia. Moreover, this study also described its therapeutic effectiveness [27]. However, an interventional study design with a randomized controlled trial is required to establish the definite therapeutic effect of ESWT on managing sexual pain symptoms.
4.7. Visceral Therapy
Visceral therapy involves the three-dimensional dynamics of the body’s biomechanics: the muscular-skeletal structure, muscular and fascial structure, connective tissue and the organs, reflex activity in the central and peripheral nervous system, and the circulation and draining of fluid systems in the human body [55, 56]. This technique has been used to treat chronic abdominal pain [57], diastasis recti [58], pelvic floor disorders [59], and painful sexual dysfunction [60]. A literature review by Wojcik M et al. discussed dyspareunia as a genital pain, which may result from an imbalance between the female genital organs and their surrounding tissues with other structures of the skeletal or visceral system, with impaired mobility and motility of organs, intra-organ movement, vascular drainage, a pressure gradient between the urogenital and diaphragmatic cylinders, dysfunctions in the area of the broad ligament of the uterus in which visceral therapy aims at restoring intra-organ movement, reducing tension, focusing on the area of the two cylinders of the trunk, and supporting the functioning of the vascular system in the vicinity of the uterus [28]. In general, visceral treatment for reproductive system dysfunction involves restoring postural balance, breathing, pelvic activity, and balancing the pressures between the diaphragms in the body [61, 62]. However, the clinical applicability and effectiveness of this treatment require further randomized controlled trials to contrast the varied treatment strategies, dosages, and duration of treatment sessions.
To manage dyspareunia effectively, multifaceted treatment options are available. Most of the cases remain undiagnosed due to multiple reasons, starting from hesitancy of the patient in discussing with the clinicians to the complexity of the diagnostic process. Each physical therapeutic intervention is under-researched to date; therefore, a conclusion regarding the dose and response ratio cannot be generalized. Secondly, limited literature on the effect of a single therapy vs. combination therapy on the management of dyspareunia has generated further issues. This narrative review poses certain limitations in terms of subjectivity, selection bias, and lack of systematic and quantitative analysis, which is restricted to critically analyzing the most efficacious treatment method for managing this sexual pain dysfunction, which usually affects all the domains from physical to psychological aspects of the woman. Due to the predominantly qualitative approach, the findings of this review are not conclusive and cannot be used to generalize about the definite management strategies for the categories of superficial and deep dyspareunia. However, the findings of these studies imply that public health, policymakers, and research are needed regarding the categories of dyspareunia management. Therefore, for a thorough and enhanced understanding of the utility of each of the different therapeutic means for managing this sexual pain dysfunction, systematic reviews of randomized controlled trials comparing different treatment strategies, dosages, and durations of sessions are required to figure out this complex women’s health issue to generate highest quality evidence-based therapeutic means. However, clinicians and health care providers must place great emphasis on the multidisciplinary approach to determine how this challenging sexual health dysfunction can be best supported or treated with a single or combination of physical therapeutic means.
CONCLUSION
The underlying causes for the development of dyspareunia are multi-factorial. It tends to cause harm to a woman’s physical and mental health, which could pose the greatest threat to the quality of life. Therefore, it is also important to establish which aspects of the patient’s life have been impacted. Remedial measures for dyspareunia are entirely based on the key diagnosis and require a multidisciplinary treatment approach to intervene in the specific body structure and function (vagina and supporting structures/ other pelvic structures). With the categorization into superficial or deep dyspareunia, the therapeutic approaches vary. The interventions discussed above encompass a range of approaches aimed at addressing dyspareunia, or painful intercourse, through various modalities, including pelvic floor muscle training/ rehabilitation, biofeedback, perineal massage, manual therapy, dilator therapy, shockwave therapy, and visceral therapy, which may be applicable as a single or combination therapy. For treating this complex gyneco- logical disorder, the multimodal adjuvant therapeutic approach seems to be advantageous for addressing the physical and secondary emotional problems associated with this issue. From this review, it could be concluded that there is no consolidated evidence regarding the relative efficacy or effectiveness of various therapeutic interventions for managing dyspareunia. Considering the findings of this review, it could be safely said that a patient-centric eclectic approach incorporating different therapeutic modes will be most appropriate for the management of dyspareunia. Therefore, the recommendation lies in the future and further research with a systematic review of randomized controlled trials to generate the highest quality evidence-based therapeutic means to figure out this challenging sexual pain dysfunction disorder of women.
AUTHORS’ CONTRIBUTION
M.R., K.D., and S.K.: Study conception and design; M.R., V.K., and M.N.: Methodology, data analysis, and interpretation; A.N., K.D., and S.K.: Writing, reviewing, and editing; K.D., V.K., M.R., and S.K.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| APM | = Antenatal Perineal Massage |
| CINAHL | = Cumulative Index to Nursing and Allied Health Literature |
| DIE | = Deep Infiltrating Endometriosis |
| DSM-V | = Diagnostic and Statistical Manual of Mental Disorders, Fifth edition |
| ESWT | = Extracorporeal Shockwave Therapy |
| FSFI | = Female Sexual Function Index |
| GPPPD | = Genito-Pelvic Pain/ Penetration Disorders |
| HADS | = Hospital Anxiety and Depression Scale |
| LHA | = Levator Hiatus Area |
| MBDT | = Movement-Based Dilator Therapy |
| NRS | = Numerical Rating Scale |
| PFMT | = Pelvic Floor Muscle Training |
| RCTs | = Randomized Controlled Trails |
| QOL | = Quality of life |
| VAS | = Visual analogue Scale |


