All published articles of this journal are available on ScienceDirect.
Prevalence of Hypertension, Prehypertension, and High-normal Blood Pressure in Peru: A Systematic Review and Meta-analysis
Abstract
Introduction
Hypertension (HTN) is a major cardiovascular risk factor, with increasing concern over preceding conditions, such as prehypertension and high-normal blood pressure (HNBP). In Peru, the data on these conditions is heterogeneous and requires updating.
Objectives
This study aimed to determine the prevalence of HTN, prehypertension, and HNBP in Peru through a systematic review and meta-analysis.
Methods
A comprehensive search was conducted in scientific databases and government sources from 2000 to 2024. Studies with probabilistic sampling in the Peruvian population were included. Methodological quality was assessed, and a random-effects meta-analysis with subgroup analyses was performed.
Results
A total of 16 studies were included. The pooled prevalence of HTN was 21.07% (95% CI: 18.04%-24.27%), prehypertension was 29.14% (95% CI: 24.98%-33.49%), and HNBP was 13.25% (95% CI: 4.78%-25.08%). Differences were observed by sex, publication period, and geographic scope. Heterogeneity among studies was significant (I2 > 97% for all outcomes).
Conclusion
The combined burden of these conditions affects over 60% of the adult Peruvian population, posing a significant public health challenge. The high prevalence of Prehypertension and HNBP highlights the importance of primary prevention strategies. The observed variations suggest the need for tailored interventions for specific subgroups. This study provides an updated foundation for health policy planning and future research in Peru.
1. INTRODUCTION
Hypertension (HTN) remains a global public health issue and is considered one of the leading modifiable risk factors for cardiovascular diseases. According to the World Health Organization, over one billion people worldwide suffer from hypertension, with an increasing trend, particularly in low- and middle-income countries [1]. In Latin America, the prevalence of HTN ranges between 20% and 40% of the adult population, posing a significant challenge to regional health systems [2].
Peru, as a developing country, faces this issue in the context of lifestyle changes, rapid urbanization, and population aging, factors that have contributed to an increase in cardiovascular risks, including HTN [3]. However, data on the exact prevalence of HTN and related conditions in the country is heterogeneous and, at times, contradictory, complicating the implementation of effective public health policies.
It is important to note that the concepts and classifications surrounding hypertension have evolved over time. While the term prehypertension has been widely used and entrenched in clinical practice and research for many years, the most recent guidelines tend to favor the concept of high-normal blood pressure (HNBP) [4]. Nonetheless, given the persistence of the term “prehypertension” in the literature and its historical relevance, it is valuable to examine the prevalence of both conditions. Both prehypertension and HNBP represent intermediate states between normotension and established hypertension and are associated with a higher risk of progression to the latter, along with subsequent cardiovascular complications [5].
In 2019, Ruiz-Alejos et al. [6] conducted a systematic review on the prevalence of HTN in Peru. However, the field of cardiovascular epidemiology is dynamic, with new studies and data emerging constantly. Additionally, including concepts, such as the intermediate stages can provide a more comprehensive view of the blood pressure spectrum in the Peruvian population. Therefore, there is a need to update and expand this review to include more recent studies and address these additional categories.
The aim of this systematic review and meta-analysis is, therefore, to synthesize and update the available evidence on the prevalence of HTN, including prehypertension and HNBP, in Peru.
2. METHOD
2.1. Study Approach
Our study is a systematic review with meta-analysis, focusing on assessing the prevalence of HTN, prehypertension, and HNBP in Peru. We adhered to the principles outlined in the PRISMA 2020 statement [7], with adaptations made to meet the specific needs of our research.
2.2. Literature Search Process
We comprehensively searched multiple scientific databases, including Scopus, Web of Science, Embase, and grey literature sources. The search period took place in May 2024, including the most recent studies. We used a strategic combination of key terms in both Spanish and English related to “hypertension,” “high blood pressure,” “prehypertension,” “high-normal blood pressure,” and “Peru” and their equivalents in English.
2.3. Inclusion and Exclusion Criteria
Our review included various information sources, not limited to original articles published in scientific journals. We also incorporated technical reports, epidemiological bulletins, and national health survey databases, thereby expanding the scope of our search to capture a more comprehensive picture of the situation in Peru.
The inclusion criteria were: 1) Studies, reports, or surveys that reported the prevalence of HTN, prehypertension, or HNBP in the Peruvian population; 2) research that utilized probabilistic sampling techniques to ensure the representativeness of the results; and 3) publications in Spanish, English, or Portuguese.
We excluded studies focused exclusively on children or adolescents and those centered on populations (e.g., only patients with diabetes or kidney disease) that were not representative of the general population. Additionally, studies that did not provide precise data on the prevalence of the conditions of interest or did not use standardized diagnostic criteria were excluded.
2.4. Selection Procedure
The selection process was conducted in three stages: 1) duplicate removal using specialized software; 2) screening of titles and abstracts by two independent researchers, with a third reviewer resolving any discrepancies; and 3) full-text analysis of the selected articles and data extraction into an Excel matrix.
Subsequently, we used Microsoft Excel for systematic data extraction. We collected detailed information from each study, including the primary author and year of publication, the city or region of the study, specific inclusion and exclusion criteria of the study, sample size and demographic characteristics (percentage of women, age range), diagnostic criteria used for HTN, prehypertension, and HNBP, and the reported prevalence rates for each condition.
2.5. Additional Data Extraction Strategy
In our data extraction process, we adopted a comprehensive approach to maximize the use of available information. When articles or reports did not directly provide all the necessary data for our analysis, but access to the original study databases was available, we proceeded to extract the required information directly from these primary sources.
This approach allowed us to significantly enrich our analysis by ensuring the inclusion of complete and accurate data, even when not directly presented in the original publications. Additionally, this methodology enabled us to perform more detailed and specific analyses tailored to the objectives of our systematic review.
In all cases, special care was taken to document the exact source of each piece of data, clearly distinguishing between information extracted directly from publications and data derived from our own calculations based on the original databases. This transparency in the data extraction methodology enhances the reliability and reproducibility of our findings.
2.6. Methodological Quality Assessment
We employed the tool developed by Munn et al. [8] to assess the risk of bias in prevalence studies. This tool considers aspects, such as the sample's representativeness and the measurement methods' adequacy. Studies were categorized as having a high, medium, or low risk of bias based on their compliance with the established criteria.
2.7. Statistical Analysis
A random-effects model meta-analysis was conducted to estimate the pooled prevalence of the three study outcomes. Additionally, we performed a sensitivity analysis stratified by sex, year (<2013 and ≥2013), and scope (national vs. subnational). Heterogeneity among studies was assessed using the I2 statistic and Cochran’s Q test.
Furthermore, we conducted a stratified sensitivity analysis by these same variables to evaluate the robustness of our findings. Funnel plots were used to assess potential publication bias.
2.8. Ethical Considerations
Since our research is based on the analysis of already published studies, the ethical risks are minimal. Therefore, a review by a research ethics committee was not deemed necessary. However, we adhered to ethical research principles, ensuring integrity and transparency in reporting our methods and results.
3. RESULTS
3.1. Study Selection
The research commenced with the identification of 2,821 publications from electronic databases and additional sources. After removing duplicates, titles and abstracts of the remaining 1,749 articles were screened. This process led to the selection of 87 studies for full-text review. Ultimately, only 16 investigations met all established inclusion criteria and were incorporated into the systematic review. The flow diagram illustrating this selection process is presented in Fig. (1).
3.2. Characteristics of the Studies
A total of 16 studies were included in this review [9-23]. It is important to note that among the selected studies, reports from the 2009 Epidemiological Bulletin of the Ministry of Health [14], the National Survey of Indicators for Non-Communicable Diseases (ENINBSC) [11], and the Nutritional Surveillance by Life Stages (VIANEV) [19] were used in place of published articles. For the study by J.J. Miranda [15], the original study was utilized, and additional data were extracted since the PERU MIGRANT study database is openly accessible [24].
Most studies were conducted in Lima, Peru's capital, but investigations also took place in other regions, such as Arequipa, Tumbes, Puno, and Ayacucho. Some studies, such as the ENINBSC [11], VIANEV [19], and the study by Loayza-Castro [25], had national coverage, encompassing multiple departments across Peru.
The sample sizes varied considerably among the studies. Romero (2014) [17] had the smallest study, with 76 participants in Asháninka communities in Junín, while Loayza-Castro (2024) [25] had the largest, with 33,103 participants. The ENINBSC [11] 2004-2005 had the largest, with 4,096 participants.
Most studies focused on adults, with age ranges varying from 18 to 99 years in some cases. Some studies, such as Bernabé-Ortiz (2018) [20], focused on more specific age ranges, such as 30-64 years, while the VIANEV [19] covered 18 to 59 years. The study by Geldsetzer Pascal (2019) [21] encompassed a broad range from 40 to 96 years, and Loayza-Castro (2024) [25] ranged from 18 to 99 years.
Overall, there was a tendency to have more women than men in the samples. For example, the Epidemiological Bulletin (2009) [14] had 62.2% women, and Revilla L. [2014] had 62% [16]. However, some studies, such as Bernabé-Ortiz (2020) [22], had a more balanced distribution with 49.6% women.
Regarding the assessment of outcomes, all 16 studies evaluated the prevalence of HTN. Additionally, only Revilla L. (2014) [16] and Bernabe-Ortiz (2015) [18] evaluated prehypertension. Meanwhile, Miranda JJ [15], Loayza-Castro [25], VIANEV [19] and ENINBSC [11] evaluated HNBP.
Concerning the diagnostic criteria used for blood pressure abnormalities, J.J. Miranda, Loayza-Castro, VIANEV, and ENINBSC employed the 2023 criteria from the International Society of Hypertension (ISH) and the European guidelines [4]. The remaining studies used the criteria from the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7) [26]. All studies used the classical cutoff points of 140/90 mmHg for HTN and prior diagnosis of hypertension. No study solely assessed HTN by self-report. For prehypertension, the range of 120-139/80-90 mmHg (JNC7) was used, while for HNBP, the range of 130-139/85-89 mmHg was applied.
Finally, a timeline has been created, presented in Fig. (2), offering a visual perspective of when the various studies included in this review were conducted and indicating the establishment of the databases used. Complementing this, Fig. (3) is a geographic map of Peru that uses a color-coding system to highlight the departments where the analyzed studies were conducted, thus providing a spatial distribution of the research.
3.3. Meta-analysis of the Prevalence of HTN, Prehypertension, and HNBP
The meta-analysis of the prevalence of HTN in Peru, based on 16 studies conducted between 2005 and 2024, revealed a pooled prevalence of 21.07% (95% CI: 18.04 - 24.27%). There was considerable heterogeneity among the studies (I2 = 99.02%, p < 0.001), with estimates ranging from 10.53% (VIANEV 2017-2018) [19] to 45.49% (Goldstein 2005) [9]. The most recent and large-scale studies, such as Loayza-Castro 2024 [25] and Geldsetzer Pascal 2019 [21], reported prevalences of 20.43% and 26.42%, respectively, suggesting a downward trend in recent years.
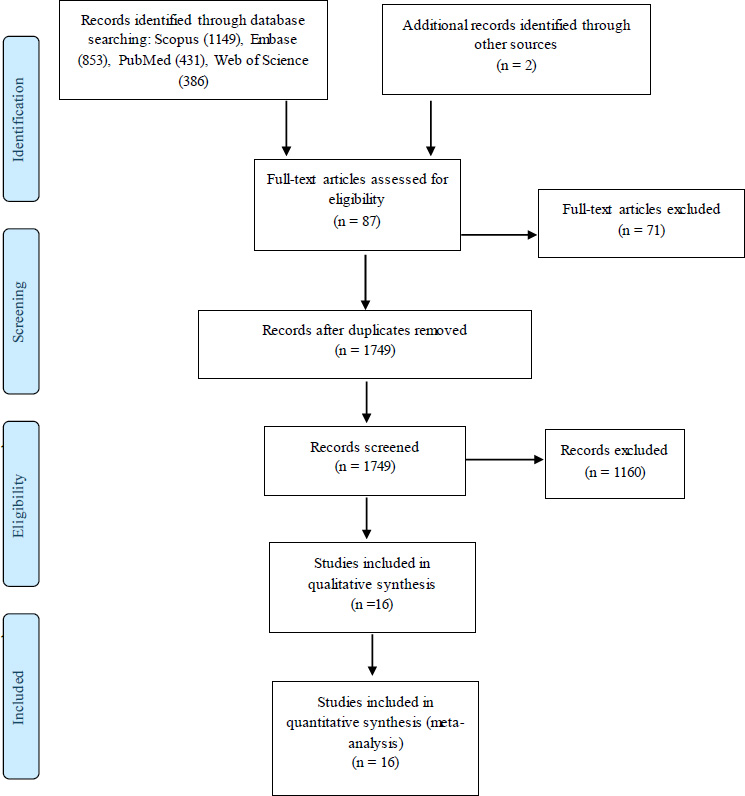
Flowchart of study selection.
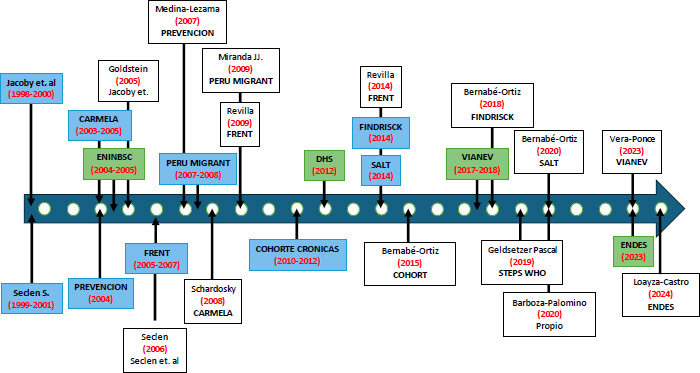
Timeline of research and database of the prevalence of HTA/PreHTA/HNBP in Peru.
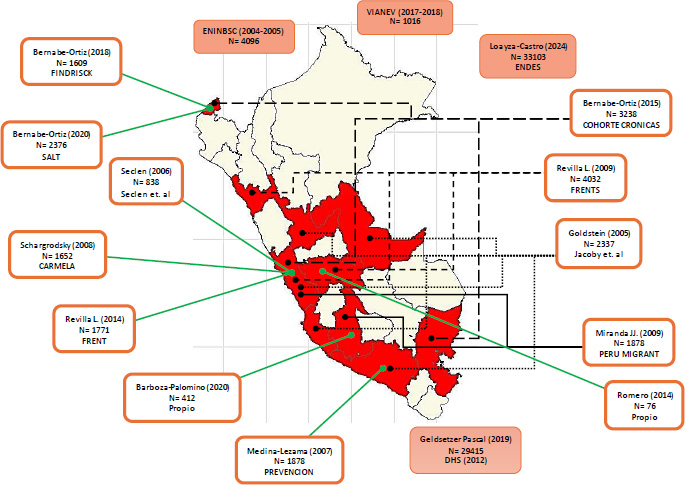
Geographic distribution of selected studies of the SR of HTA/PreHTA/HNBP in Peru.
The meta-analysis of the prevalence of prehypertension in Peru, based on 6 studies conducted between 2004 and 2024 [11, 15, 16, 19, 25, 26], showed a pooled prevalence of 29.14% (95% CI: 24.98% - 33.49%). There was significant heterogeneity among the studies (I2 = 97.86%, p < 0.001), with estimates ranging from 18.04% (VIANEV 2017-2018) [19] to 38.24% (Miranda JJ, 2009) [15]. Recent studies, such as Loayza-Castro 2024 [25], reported a prevalence of 33.16%.
The meta-analysis of the prevalence of HNBP in Peru, based on 4 studies conducted between 2004 and 2024 [11, 15, 19, 25], revealed a pooled prevalence of 13.25% (95% CI: 4.78% - 25.08%). There was extremely high heterogeneity among the studies (I2 = 99.69%, p < 0.001), with estimates ranging from 5.91% (ENINBSC 2004-2005) [19] to 22.81% (Loayza-Castro 2024) [25], as shown in Figs. (4-6).
3.4. Funnel Plot Analysis
The funnel plot illustrates the distribution of studies included in the meta-analysis of hypertension prevalence in Peru (Fig. 7). The shape of the plot is asymmetric, suggesting the potential presence of publication bias. The studies are unevenly distributed around the central line (pooled estimate θIV), with a concentration of studies at the top of the funnel. This indicates that studies with greater precision (lower standard error) tend to cluster near the combined prevalence estimate.
Some studies are observed outside the 95% confidence interval limits (represented by the gray lines), particularly at the left and right extremes of the plot. These outliers may represent studies with results significantly different from the overall estimate, possibly due to methodological or population differences.
3.5. Sensitivity Analysis of the Prevalence of HTN, Prehypertension, and HNBP
The sensitivity analysis of hypertension prevalence in Peru reveals interesting patterns (Table 1). By sex, a slightly higher prevalence is observed in males (20.84%) compared to females (19.47%), although the confidence intervals overlap. Temporally, studies conducted before 2013 show a higher prevalence (24.57%) compared to those after 2013 (18.54%), suggesting a potential decrease in recent years. Regarding scope, national studies report a higher prevalence (22.07%) than subnational studies (17.01%). In all cases, the significant heterogeneity (I2 < 0.001) indicates considerable variability among the studies, which could reflect real differences in the population or methodological variations.
The sensitivity analysis of prehypertension prevalence in Peru reveals notable differences (Table 2). By sex, the prevalence is significantly higher in males (42.67%) than in females (21.11%). Temporally, a slight decrease is observed in studies conducted after 2013 (27.36%) compared to those conducted earlier (29.36%). Regarding scope, subnational studies report a higher prevalence (32.14%) than national studies (26.30%). The significant heterogeneity (I2 < 0.001) across all subgroups suggests considerable variability among the studies, possibly due to methodological differences or real variations in the populations studied.
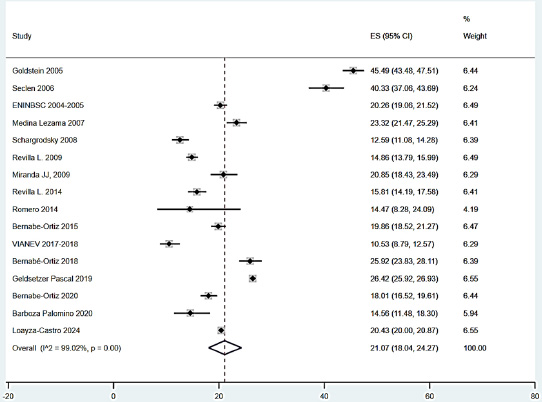
Meta-analysis of HTN prevalence in Peru.
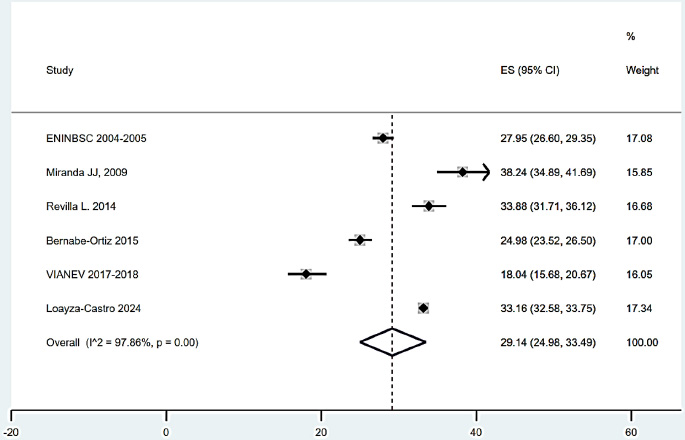
Meta-analysis of prehypertension prevalence in Peru.
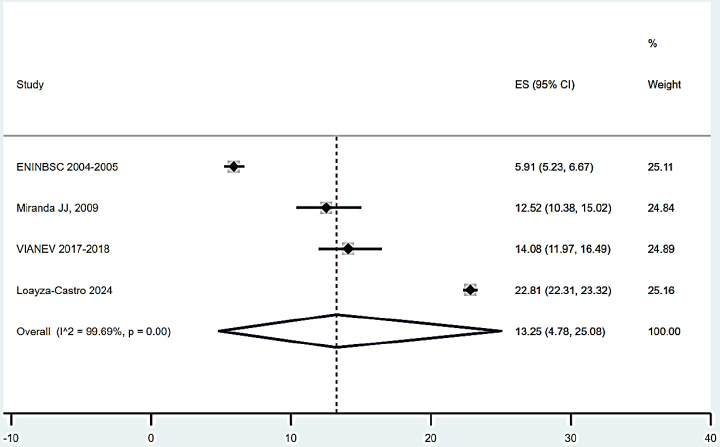
Meta-analysis of high-normal blood pressure prevalence in Peru.
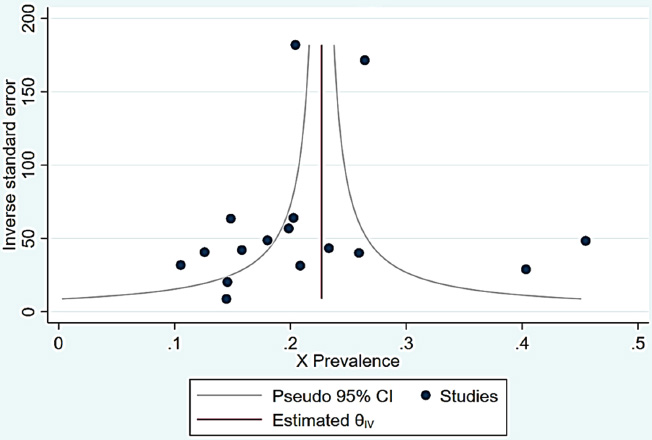
Funnel plot de la prevalence the HTA in Perú.
| - | Number of Studies | Prevalence % | IC 95% | I2 |
|---|---|---|---|---|
| Sex | - | - | - | - |
| Male | 11 | 20.84 | 14.47 - 25.58 | < 0.001 |
| Female | 11 | 19.47 | 14.54 - 24.92 | < 0.001 |
| Time | - | - | - | - |
| < 2013 | 7 | 24.57 | 18.43 - 23.49 | < 0.001 |
| ≥ 2013 | 9 | 18.54 | 20.00 - 20.87 | < 0.001 |
| Scope | - | - | - | - |
| Subnational | 3 | 17.01 | 13.29 - 21.10 | < 0.001 |
| National | 13 | 22.07 | 17.76 - 26.69 | < 0.001 |
The sensitivity analysis of the prevalence of HNBP in Peru reveals distinctive patterns (Table 3). By sex, the prevalence is notably higher in males (18.71%) than in females (9.33%). Temporally, a considerable increase is observed in studies conducted after 2013 (15.20%) compared to those conducted earlier (5.42%). Regarding scope, national studies show a slightly higher prevalence (9.94%) than subnational studies (7.52%), although only one subnational study is available. The significant heterogeneity (I2 < 0.001) across all subgroups indicates substantial variability among the studies, possibly reflecting methodological differences or fundamental changes in the population over time.
3.6. Risk of Bias Assessment
The bias analysis of HTN prevalence studies in Peru shows a generally positive picture regarding methodological quality (Table 4). Most studies meet the evaluated criteria, indicating a low risk of bias in key aspects, such as sampling frame, participant selection methods, sample size, and measurement procedures.
All studies used an appropriate sampling frame and adequate participant selection methods. Most also employed sufficient sample sizes and standardized measurement procedures. However, some variations in specific criteria were observed, as many studies did not clearly report whether data analysis was conducted with adequate coverage or if the response rate was appropriate.
4. DISCUSSION
4.1. Summary of Key Findings
This study reveals significant patterns in the prevalence of blood pressure disorders in Peru. Hypertension affects 21.07% of the population, while prehypertension and HNBP show prevalences of 29.14% and 13.25%, respectively. Notable differences by sex were observed, with higher prevalence in men across all categories. Temporally, there is a downward trend in HTN and Prehypertension in recent studies, contrasting with an increase in HNBP. National studies generally report higher prevalences than subnational ones. Although most studies show a low risk of bias, the funnel plot analysis suggests potential publication bias. These findings underscore the importance of these disorders as public health concerns in Peru and the need for prevention and control strategies tailored to observed trends.
| - | Number of Studies | Prevalence% | IC 95% | I2 |
|---|---|---|---|---|
| Sex | - | - | - | - |
| Male | 4 | 42.67 | 34.13 - 51.43 | < 0.001 |
| Female | 4 | 21.11 | 16.16 - 26.53 | < 0.001 |
| Time | - | - | - | - |
| < 2013 | 2 | 29.36 | 28.26 - 30.82 | < 0.001 |
| ≥ 2013 | 4 | 27.36 | 21.56 - 33.56 | < 0.001 |
| Scope | - | - | - | - |
| Subnational | 3 | 32.14 | 24.45 - 40.36 | < 0.001 |
| National | 3 | 26.30 | 20.11 - 33.00 | < 0.001 |
4.2. Comparison with Existing Literature
The combined prevalence of HTN in Peru, at 21.07% (95% CI: 18.04 - 24.27%), is consistent with previous estimates for the Latin American region. A recent meta-analysis by Díaz and Espeche (2021) reported a prevalence of 19.1% in Latin America and the Caribbean [27]. Our findings update and expand on the prior work of Carrillo-Larco et al. (2019), which estimated a prevalence of 20.1% in Peru [6].
The sensitivity analysis revealed exciting patterns. The higher prevalence in men (20.84%) compared to women (19.47%) aligns with global trends, as reported by Zhou et al. (2021) in their global analysis of HTN [28]. The decrease observed in studies after 2013 (18.54% vs. 24.57% before 2013) could reflect improvements in early detection and management of HTN, although this requires further investigation.
The difference between national (22.07%) and subnational studies (17.01%) highlights the importance of considering geographic and sociodemographic variations in public health intervention planning. This pattern is similar to that observed in other countries, such as Brazil, where Picon et al. (2018) found significant regional variations [29].
| - | Number of studies | Prevalence % | IC 95% | I2 |
|---|---|---|---|---|
| Sex | - | - | - | - |
| Male | 4 | 18.71 | 7.74 - 33.05 | < 0.001 |
| Female | 4 | 9.33 | 4.11 - 16.34 | < 0.001 |
| Time | - | - | - | - |
| < 2013 | 2 | 5.42 | 4.46 - 6.45 | < 0.001 |
| ≥ 2013 | 2 | 15.20 | 14.62 - 15.79 | < 0.001 |
| Score | - | - | - | - |
| Subnational | 1 | 7.52 | 5.32 - 10.53 | < 0.001 |
| National | 3 | 9.94 | 3.71 - 18.73 | < 0.001 |
These findings place Peru in an intermediate position compared to other Latin American countries. For example, Chile reports a higher prevalence (27.6%) [30], while Mexico shows a similar prevalence (20.9%) [31]. The heterogeneity observed in our study underscores the need for more detailed research on the factors influencing these variations within the Peruvian context.
4.3. Analysis of Pre-HTN States – Prehypertension versus HNBP
The analysis of pre-HTN states in Peru reveals interesting and potentially concerning patterns. The prevalence of prehypertension at 29.14% (95% CI: 24.98 - 33.49%) is notably higher than that of HNBP at 13.25% (95% CI: 4.78 - 25.08%). This difference is explained by the different diagnostic criteria used.
Prehypertension covers a broader range than HNBP, according to the most recent guidelines [4, 26]. This difference in definitions may contribute to the higher observed prevalence of the former. It is important to clarify that while the concept of prehypertension has not been widely used in recent years, it is associated with an increased cardiovascular risk and progression to established HTN, as noted in previous studies [32, 33]. A similar meta-analysis by Lewington et al. (2002) [32], which included data from over a million adults, demonstrated that the risk of cardiovascular disease increases linearly from blood pressure levels as low as 115/75 mmHg. This finding challenged the notion of a “safe” threshold for blood pressure and laid the groundwork for reconsidering normal ranges. More recently, the SPRINT (Systolic Blood Pressure Intervention Trial) in 2015 provided robust evidence that maintaining systolic pressure below 120 mmHg in high cardiovascular-risk adults could significantly reduce cardiovascular events and all-cause mortality [33]. This justifies the inclusion of Prehypertension in the present work.
On the other hand, the observed temporal trend is particularly relevant. While the prevalence of prehypertension shows a slight decrease in studies conducted after
| Study (Year of Publication) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| Was the sampling frame appropriate to address the target population? | Were the study participants recruited in a proper way? | Was the sample size adequate? | Were the subjects and setting of the study described in detail? | Was the data analysis conducted with sufficient coverage of the identified sample? | Were valid methods used for the identification of the condition? | Was the condition measured in a standard and reliable way for all participants? | Was there an appropriate statistical analysis? | Was the response rate adequate, and if not, was the low response rate handled appropriately? | - | - |
| Goldstein 2005 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| Seclen 2006 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| ENINBSC 2004-2005 | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Medina Lezama 2007 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| Schargrodsky 2008 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| Revilla L. 2009 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| Miranda JJ, 2009 | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Revilla L. 2014 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| Romero 2014 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| Bernabe-Ortiz 2015 | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| VIANEV 2017-2018 | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Bernabé-Ortiz 2018 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| Geldsetzer Pascal 2019 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| Bernabe-Ortiz 2020 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| Barboza Palomino 2020 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
| Loayza-Castro 2024 | Y | Y | Y | Y | Y | Y | Y | Y | U | 8 |
2013 (27.36% vs. 29.36%), HNBP presents a considerable increase (15.20% vs. 5.42%). This pattern may reflect changes in the lifestyle habits of the Peruvian population, as well as improvements in the detection and classification of these intermediate states.
Differences by sex are consistent across both categories, with a higher prevalence in men for both Prehypertension (42.67% vs. 21.11% in women) and HNBP (18.71% vs. 9.33%). This trend aligns with global findings suggesting greater male susceptibility to blood pressure alterations [34].
Comparatively, these results are similar to those reported in other Latin American countries. For example, a study in Brazil found a prevalence of prehypertension of 29.8% [35], while in Colombia, it was reported at 26.5% [36]. The variability in HNBP estimates is greater among countries, possibly due to the more recent adoption of this concept.
These findings highlight the importance of primary prevention strategies focused on these intermediate states, considering they represent a crucial opportunity for intervention before the development of established HTN [37].
4.4. Importance of Targeted Hypothesis Studies
It is essential to clarify that many studies included in this review were not explicitly designed to assess the prevalence of HTN, let alone prehypertension or high-normal blood pressure. However, they contained the necessary data to conduct the study.
Most studies focused on other variables, providing the necessary data for this study. For instance, studies like ENDES or VIANEV were not conducted exclusively for HTN, unlike other investigations targeted at a specific disease, such as PERUDIAB [38]. While the TORNASOL study [39] conducted many years ago aimed to determine the prevalence of HTN and its related factors, it had significant limitations in terms of design.
This lack of specific focus can lead to underestimation or overestimation of prevalence. Moreover, the lack of standardization in blood pressure measurement and the definition of these intermediate states may contribute to the heterogeneity observed in our results. Studies not explicitly designed to detect them may lack the rigorous measurement protocols required for the accurate classification of these subtle states.
This limitation underscores the need for more research focusing on HTN and its pre-states in the Peruvian population. Studies designed for this purpose could provide more accurate estimates and allow for more detailed analysis.
4.5. Public Health Implications
The findings of our study have significant public health implications in Peru and internationally. The high combined prevalence of hypertension, prehypertension, and high-normal blood pressure, affecting over 60% of the adult Peruvian population, underscores the urgent need to implement more aggressive primary prevention strategies. These strategies should focus on lifestyle modifications, including a healthy diet, regular physical activity, and salt reduction, in line with WHO recommendations for preventing and controlling non-communicable diseases.
Our results also highlight the importance of improving early detection programs and monitoring blood pressure alterations. Considering recent evidence on the increased cardiovascular risk with blood pressures above 120/80 mmHg, it is crucial to expand and make screening programs more frequent. This, in turn, suggests the need to review and possibly update national clinical guidelines for blood pressure management, considering earlier interventions in individuals with prehypertension and high-normal blood pressure.
The differences observed among population subgroups, such as higher prevalence in men, indicate the need to develop public health strategies targeted at specific populations. This approach aligns with the principle of health equity promoted by international organizations. Moreover, the high prevalence of these disorders underscores the need to strengthen the capacity of the Peruvian health system to manage a potentially large volume of patients requiring intervention and follow-up.
Our study also identifies key areas for future research, including the need to explore the specific risk factors of the Peruvian population that contribute to these high prevalences and to develop and evaluate interventions adapted to the local context. The findings provide a solid foundation for international collaboration in the Latin American region, enabling comparisons and the exchange of effective prevention and control strategies.
Finally, these results have significant economic implications, suggesting the need for cost-effectiveness analyses of different prevention and treatment strategies. They also highlight the importance of implementing more effective public education campaigns on the risks associated with elevated blood pressure, even in ranges previously considered normal. Our study establishes an updated baseline for future monitoring and evaluation of public health interventions targeting blood pressure in Peru, with potential relevance for other countries in the region and globally.
4.6. Strengths and Limitations of the Study
This study provides a comprehensive and updated review of hypertension and related states in Peru, covering a wide period and various regions. The rigorous study selection and sensitivity analyses provide a thorough and nuanced view of the situation.
However, the study's limitations must be considered. The significant heterogeneity among the studies and the potential for publication bias require caution in interpreting the results. The variability in diagnostic criteria and the fact that many studies were not specifically designed to assess prehypertension or high-normal blood pressure could affect the accuracy of the estimates. Additionally, the representativeness of some geographic areas should be a concern, as shown in Table 5.
| First Author, Year | City | Inclusion Criteria | Exclusion Criteria | Sample Size | Sex (% Women) | Age | Database (Year of Collection) |
|---|---|---|---|---|---|---|---|
| Goldstein, 2005 | Lima (Magdalena and Comas), Ica, Arequipa, Huánuco, and Ucayali | Aged 20 years or older | Subjects who did not wish to participate | 2,337 | 1,165 (49.9%) | 38.0 (± 7.3); 42.1 (± 8.0) | Own Data |
| Seclen, 2006 | Rímac, SMP, Los Olivos | Aged over 30 years and residents of the mentioned areas | Type 1 diabetes, pregnant women, acute illness, any medical condition that could affect anthropometric or lab data, illiterate | 838 | 612 (68.3%) | Over 60 years, 36.1% | Own Data |
| ENINBSC 2004-2005 MINSA | National | Aged over 20 years, oriented in time, space, and place, without knowledge of having a severe illness | Pregnant or lactating women, individuals who had altered their regular diet due to illness, celebrations, physical disabilities, or athletes | 4,096 | 2,107 (50.1%) | 42.14 (15.33) | ENINBSC (2004-2005) |
| Medina Lezama, 2007 | Arequipa | Aged 20 to 80 years | Pregnant women | 1,878 | 1,011 (53.8%) | 49.6 ± 17.4; 48.5 ± 17.0 | Prevention (2005) |
| Schargrodsky, 2008 | Lima | Aged 25 to 64 years | Terminally ill, pregnant women, residents with different addresses, or those living in areas considered dangerous | 1,652 | 883 (53.4%) | 43.6 years | CARMELA (2008) |
| Revilla L., 2009 | Lima, Trujillo, Villa el Salvador, Huancayo | Aged over 15 years | Under 15 years, less than one-year residency in the study area, pregnant women | 4,032 | 2,508 (62.2%) | 15 to 94 years (Mean: 39.2 - 41.7) | FRENT Lima (2007), VES (2006), Huancayo (2005), Trujillo (2006) |
| Miranda JJ, 2009 | Ayacucho, San Juan de Miraflores | Aged 20 to 80 years | Pregnant women | 1,878 | 53.83% | 49.05 | PERU MIGRANT |
| Revilla L., 2014 | Lima | Aged over 15 years | Under 15 years, less than one-year residency in the study area, pregnant women, disabling conditions preventing proper anthropometric evaluation | 1,771 | 1,105 (62%) | 39.5 years | FRENT Lima-Callao (2007) |
| Romero, 2014 | Junín, Satipo | Aged over 35 years, volunteers, both sexes, permanent residents in Asháninka communities present at evaluation | Logistical difficulties of working in remote areas | 76 | 40 (52.6%) | 47.4 (9.9) | Own Data |
| Bernabe-Ortiz, 2015 | Lima, Urban Puno, Rural Puno, Tumbes | Aged 35 years or older, full-time residents, provided informed consent | Pregnant women, mental disorders that prevented survey completion | 3,238 | 1,674 (51.7%) | 45.3 (IQR: 45.3–65.2) | COHORT CRONICAS |
| VIANEV, 2017-2018 | Lima, Callao, other urban areas, rural | Aged 18 to 59 years, fasting adults (9-12 hours) | Adults not listed for identification, pregnant/postpartum women, adults on medication affecting glucose or lipid profiles, non-fasting individuals, gastrointestinal problems, genetic conditions or malformations affecting anthropometric techniques | 1,016 | 561 (55.22%) | 38.57 (11.78) | VIANEV (2017-2018) |
| Bernabé-Ortiz, 2018 | Tumbes | Aged 30 to 69 years, full-time resident, capable of understanding procedures and giving informed consent, with a history of antihypertensive, elevated glucose, or family history of DM2 | Pregnant women, physical disabilities preventing anthropometric measurements, bedridden participants | 1,609 | 810 (50.3%) | 48.2 (± 10.6) | FINDRISCK (2014) |
| Geldsetzer Pascal, 2019 | Lima | Aged 40 to 96 years | Data unavailable for analysis | 29,415 | 15,472 (52.6%) | 54 | WHO STEPS |
| Bernabe-Ortiz, 2020 | Tumbes | All men and women aged 18 years or older from the six selected villages, capable of understanding procedures, giving informed consent, full-time residents | Self-reported history of chronic kidney disease and heart disease treated with digoxin | 2,376 | 1,179 (49.6%) | 43.3 ± 17.2 years | SALT (2014) |
| Barboza Palomino, 2020 | Huamanga (Ayacucho) | Aged 18 to 64 years living in Ayacucho | Pregnant or breastfeeding, neurological or mental health issues that interfere with logical interview responses | 412* | - | - | Own Data (2018) |
| Loayza-Castro, 2024 | 24 departments of Peru | Aged 18 to 99 years | Participants with incomplete data for main study variables, pregnant women, implausible values | 33,103 | 52.02% | 40.54 (15.97) | ENDES 2023 |
CONCLUSION
This study provides a comprehensive and updated overview of the prevalence of HTN, prehypertension, and HNBP in Peru. The findings reveal a significant burden of these conditions in the Peruvian population, with important variations by sex, study period, and scope. The high combined prevalence of these conditions, affecting over 60% of the adult population, underscores the magnitude of the public health challenge in the country. These results highlight the urgent need for more effective prevention, early detection, and management strategies to reduce the impact of cardiovascular diseases in Peru.
Based on these findings, we recommend implementing more aggressive public health policies focused on the primary and secondary prevention of HTN and related conditions. This includes strengthening public education programs on healthy lifestyles, expanding screening programs for early detection, and updating national clinical guidelines to address prehypertension and HNBP. Additionally, we recommend conducting longitudinal studies to better understand the progression of these disorders and their risk factors in the Peruvian context. Finally, developing culturally adapted interventions targeted at specific high-risk groups identified in this study is crucial.
AUTHORS' CONTRIBUTION
V.J.V.-P.: Contributed to the conceptualization, investigation, methodology, resources, writing of the original draft, review, and editing; F.E.Z.-M.: Contributed to the software, data curation, formal analysis, writing, review, and editing; N.M.S.-T.: Contributed to the investigation, methodology, writing of the original draft, review, and editing; L.A.M.V.-S. and L.E.M.V.-R.: Contributed to the investigation, methodology, project administration, writing of the original draft, review, and editing; J.A.L.-C.: Contributed to the investigation, resources, original draft writing, review, and editing; E.V.-V.: Contributed to the validation, visualization, original draft writing, review, and editing; C.I.G.De.C.: Contributed to the methodology, supervision, funding acquisition, writing, review, and editing.
LIST OF ABBREVIATIONS
| HTN | = Hypertension |
| HNBP | = High-normal blood pressure |
| ISH | = International Society of Hypertension |
| UNTRM | = Universidad Nacional Toribio Rodríguez de Mendoza de Amazonas |
AVAIALABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this research are available within the article.
FUNDING
This study was funded by Vicerectorado de Investigación de la Universidad Nacional Toribio Rodríguez de Mendoza de Amazonas, Peru.
ACKNOWLEDGEMENTS
A special thanks to the members of Universidad Nacional Toribio Rodríguez de Mendoza de Amazonas (UNTRM), Amazonas, Peru, for their support and contributions throughout the completion of this research.


