All published articles of this journal are available on ScienceDirect.
Epidemiological and Seasonal Patterns of Respiratory Diseases at a Community Health Facility in Southwest Nigeria: A Five-Year Retrospective Analysis
Abstract
Background
Respiratory diseases are a leading cause of hospitalization and death in Africa. Information on the presentation and outcomes of respiratory diseases can improve disease management, health planning, and policy.
Objective
This study aims to identify the epidemiological and seasonal patterns of respiratory diseases at a health facility in southwest Nigeria.
Methods
We conducted a retrospective analysis of medical records for respiratory cases presented at the health facility over five years and descriptively analyzed the data. We then examined the association between the cases and age, sex, and/or seasonality using logistic regression analysis.
Results
Respiratory diseases accounted for 5,701 cases (7.4%) of 77,553 cases. The most common respiratory diseases were Upper Respiratory Tract Infections (URTI), with 4,719 cases (82.8%), asthma (657 cases, 11.5%), and allergic rhinitis (258 cases, 4.5%). Sex was significantly associated with URTI and asthma. The risk of URTI (OR = 0.744, 95% CI: 0.648, 0.855; p = 0.001) was significantly lower in females than males, while the risk of asthma was higher in females (OR = 1.074, 95% CI: 1.447, 2.007; p < 0.001). Except for pneumonia, all other respiratory diseases occurred mainly among adolescents and young adults (16-30 years). A seasonal pattern (with increased cases in the rainy season) was observed for pneumonia (OR=1.769, 95% CI: 1.196, 2.618; p = 0.004).
Conclusion
Understanding the trends and high-incidence periods of respiratory diseases is essential in proactively planning and managing respiratory conditions, particularly with the current realities of climate change.
1. INTRODUCTION
Respiratory diseases are a leading cause of hospitalization, and death globally, presenting substantial healthcare costs [1, 2]. The high burden of diseases, poor sanitation conditions, and poor healthcare systems in developing countries result in higher mortality rates from infectious respiratory diseases, especially in children [3, 4]. Lower respiratory tract diseases and tuberculosis are vital contributors to these high mortality rates in Africa.
Seasonal patterns of respiratory diseases are well-identified in temperate regions [5, 6]. Three important factors cause the seasonality of respiratory infections: environmental factors (seasonal changes in the environment), patterns, and viral factors [7, 8]. Temperature, humidity, and sunlight changes can reduce host resistance and increase susceptibility to infections. Furthermore, a reduction in temperature particularly favors the survival and transmission of respiratory pathogens, especially viruses, resulting in a surge in viral respiratory infections [7]. This knowledge has been used effectively in planning vaccination schedules to control acute respiratory diseases. Additionally, understanding the seasonal and environmental triggers of allergic respiratory diseases informs clinical care and management. However, there are apparent differences in the patterns and seasonal occurrence of respiratory infections in temperate regions compared to the tropics [9].Furthermore, seasonal patterns of respiratory diseases in the tropics have yet to be well identified, as more diversity has been reported [5, 10, 11].
In Nigeria, information on the prevalence and seasonal patterns of respiratory infections is limited [12, 13]. This gap poses a problem, as routine surveillance and monitoring are crucial for health planning and policy [14]. This study investigated the bio-demographics, epidemiological, and seasonal patterns of respiratory disease based on hospital visits at the Covenant University Medical Centre in Ota Ogun State, Nigeria.
2. METHODS
2.1. Study Design
This was a retrospective cross-sectional study. We retrieved anonymized records of respiratory diseases presented at the Medical Centre between January 2018 and December 2022. Data was collected between September and December 2022. Information obtained included age, sex, diagnosis, and hospital visit date.
2.2. Study Setting
Covenant University Medical Centre is a prominent healthcare facility located at the Covenant University Campus, at a latitude of 6.6726° N and a longitude of 3.1612° E. The Covenant University Medical Centre provides outpatient and inpatient healthcare services to the members of the university community (faculty, staff, and over 7,000 fully resident students).
2.3. Case Definition
Cases were defined as patients who came to the hospital with respiratory symptoms followed by a doctor’s diagnosis of respiratory disease. The diagnosis of respiratory diseases integrates clinical assessment with other relevant diagnostic procedures. This may involve, among others, chest radiographs and chest Computed Tomography (CT) scans, Mantoux tests, and blood and sputum cultures. Spirometry and echocardiography are also used as required to support a comprehensive diagnosis.
2.3.1. Respiratory Diseases
We collected data for patients the physician classified as having the following respiratory diseases: Upper Respiratory Tract Infections (URTI), pneumonia, tuberculosis, asthma, and allergic rhinitis. Cases of coryza, tonsilitis, nasopharyngitis, and bronchiolitis were classified as URTI.
2.4. Statistics and Data Analysis
Variables with missing data were discarded from the analysis. A descriptive analysis was run, and numbers and frequencies were reported. For quantitative variables such as age, we calculated the median and range. The Odds Ratio (OR) was calculated to assess the relationship between respiratory disease and independent variables such as gender and age group. The adjusted odds ratio was calculated using variables with statistically significant associations with respiratory illness. P<0.05 was considered statistically significant. All analyses were performed using the Statistical Package for the Social Sciences (SPSS), version 21 (SPSS Inc., Chicago, USA).
2.5. Ethical Consideration
This study received ethical approval from the Covenant Health Research Committee (CHREC) with approval number CHREC 154/2020. Informed consent was not required as patients were not interviewed, and data was obtained retrospectively from the medical records. All data accessed from clinical records were anonymized to maintain confidentiality.
The concluded study adhered to the ethical standards of the institutional committee responsible for human experimentation and aligned with the principles outlined in the Declaration of Helsinki.
3. RESULTS
3.1. Typical Characteristics of the Cases
A total of 77,553 outpatient visits were recorded during the study. Respiratory cases accounted for 5,701 (7.4%) outpatient hospital visits, with 3304 (58%) males accounting for the largest proportion. The average age of people with respiratory cases was 26.6 ± 15.6 years (range two months - 111 years). Patients aged 16-30 were the highest at 3745 (65.7%), and those aged 0-15 were 1314 (23%). The 31-45 age group was 386 (6.8%), with only 256 (4.5%) greater than 45 years.
The most reported respiratory cases were 4719 (82.8%) for URTI, while the least was 7 (0.1%) for tuberculosis, as presented in Table 1.
3.2. Relationship between Respiratory Diseases, Sex, and Age Groups
The prevalence of each respiratory disease stratified by sex is presented in Table 2. In particular, URTI was the most prevalent respiratory disease in females and males, with 79.23% and 83.95% of the cases, respectively. Females were less likely to have URTI (OR = 0.744, 95% CI: 0.648, 0.855; p = 0.001) than males. However, females had slightly higher odds of developing asthma than males (OR = 1.074, 95% CI: 1.447, 2.007; p < 0.001). Patterns remained the same even after adjustment for age group (Table 2).
| Respiratory disease | Count (%) |
|---|---|
| URTI | 4719 (82.8) |
| Asthma | 657 (11.5) |
| Allergic rhinitis | 258 (4.5) |
| Pneumonia | 119 (2.1) |
| Tuberculosis | 7 (0.1) |
| Disease | Sex |
COR (95% CI) |
AOR (95% CI) |
|
|---|---|---|---|---|
| Female | Male (ref) | |||
| URTI | 1930 (79.23%) | 366 (83.95%) | 0.783 (0.680, 0.903) * | 0.744 (0.648, 0.855) * |
| Asthma | 353 (14.49%) | 304 (9.12%) | 1.644 (1.391, 1.944) * | 1.074 (1.447, 2.007) * |
| Allergic rhinitis | 97 (3.98%) | 161 (4.83%) | 0.812 (0.622, 1.059) | 0.823 (0.636, 1.065) |
| Pneumonia | 53 (2.18%) | 66 (1.98%) | 0.896 (0.611, 1.313) | 1.109 (0.770, 1.599) |
| Tuberculosis | 3 (0.12%) | 4 (0.12%) | 0.850 (0.178, 4.049) | 1.034 (0.231, 4.623) |
The prevalence of respiratory diseases among age groups is shown in Table 3. Except for bronchiolitis and pneumonia, all other respiratory diseases occurred mainly among adolescents and young adults (16-30 years). Pneumonia was more prevalent among the pediatric group (0-15 years), while bronchiolitis was only reported in the pediatric age group.
The odds of each respiratory disease stratified by age are presented in Table 4. Age was associated with URTI, allergic rhinitis, and pneumonia. The odds ratio of URTI was significantly higher in the 16-30 age group (OR=1.373, 95% CI:1.014, 1.860) compared to the >45 age group. Additionally, the age group of 0-15 had significantly lower odds of allergic rhinitis (OR=0.391, 95% CI: 0.194, 0.786). Furthermore, 16–30-year-olds had significantly lower odds of pneumonia (OR = 0.084, 95% CI: 0.038, 0.185) compared to people over 45.
3.3. Seasonal Trends in Respiratory Diseases at Covenant University Health Centre
Differences in respiratory disease patterns were observed between seasons, with 3233 (56%) cases from April to October (rainy season) and 2545 (44%) cases from November to March (dry season). Three peak periods of respiratory cases were observed in June, October, and February, with the highest number recorded in October (Fig. 1).
| Age Group | 0-15 | 16-30 | 31-45 | >45 |
|---|---|---|---|---|
| URTI | 1079 (23.10%) |
3110 (66.58%) |
293 (6.27%) |
189 (4.05%) |
| Asthma | 129 (20.20%) |
425 (66.60%) |
51 (8.00%) |
33 (5.20%) |
| Pneumonia | 82 (71.30%) |
15 (13.00%) |
7 (6.10%) |
11 (9.60%) |
| Allergic rhinitis | 26 (10.30%) |
195 (77.10%) |
20 (7.90%) |
12 (4.70%) |
| Tuberculosis | 0 (0.00%) |
5 (71.40%) |
2 (28.60%) |
0 (0.00%) |
| Disease | OR for each age groupa | ||
|---|---|---|---|
| 0-15 | 16-30 | 31-45 | |
| URTI | 1.407 (1.004-1.973) | 1.418 (1.033-1.946) * | 1.126 (0.756-1.676) |
| Asthma | 0.708 (0.469-1.068) | 0.412 (0.581-1.249) | 0.924 (0.575-1.485) |
| Allergic rhinitis | 0.391 (0.194-0.786) * | 1.040 (0.571-1.892) | 1.160 (0.555-2.424) |
| Pneumonia | 1.417 (0.744-2.701) | 0.084 (0.038-0.185) * | 0.419 (0.160-1.101) |
The patterns of hospital visits for respiratory diseases by type were compared across the rainy and dry seasons (Table 5). URTI was the most prevalent respiratory disease in the rainy and dry seasons, with 81.82% and 83.03% of cases in each season, respectively. The odds of URTI were significantly lower during the rainy season (OR = 0.836, 95% CI: 0.732, 0.953).
Hospital visits for respiratory diseases were higher during the rainy season, except for tuberculosis (Table 5). Pneumonia was significantly associated with the rainy season (OR 1.769, 95% CI: 1.196, 2.618).
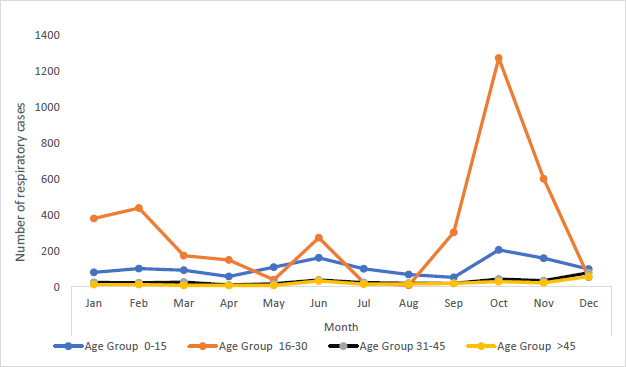
Seasonality of respiratory diseases at the Covenant University Medical Centre, Nigeria.
| Season | ||||
|---|---|---|---|---|
| Disease | Rainy Season (a) | Dry season (b) (ref) | Crude OR | p-value |
| Count (N) | Count (N) | (95% CI) | ||
| URTI | 2614 (81.12%) | 2113 (83.03%) | 0.836 (0.732-0.953) |
0.008* |
| Asthma | 376 (11.66%) | 281 (11.04%) | 1.064 (0.903-1.254) |
0.456 |
| Allergic rhinitis | 148 (4.59%) | 110 (4.32%) | 1.065 (0.821-1.371) |
0.519 |
| Pneumonia | 82 (2.54%) | 37 (1.45%) | 1.769 (1.196-2.618) |
0.009* |
| Tuberculosis | 3 (0.09%) | 4 (0.16%) | 0.592 (0.132-2.646) |
0.471 |
4. DISCUSSION
This study revealed Upper Respiratory Tract Infection (URTI) and asthma as the most prevalent infectious and non-infectious respiratory diseases, during the study period. Sex was associated with respiratory disease, with evidence of differences in prevalence between males and females. A significant association was observed between seasonality and respiratory disease, with more cases of respiratory disease during the rainy season and peak activity in October. During the dry harmattan period, a sharp increase in cases of respiratory diseases was recorded in January and February.
Overall, of all the hospital visits at the Covenant University Medical Centre, respiratory diseases had a prevalence rate of 7.4%. Previous studies in other hospitals in Nigeria had reported comparable prevalence rates of 9.3% and 10.2% [15, 16]. In contrast, a higher prevalence of 24.7% and 27.8% of respiratory diseases has been reported [13, 17]. The difference in prevalence rates of respiratory diseases could be due to the difference in the lifestyle and living conditions of the population studied. The Covenant University Medical Centre serves primarily members of the university community with families in the upper socioeconomic class and has adequate and well-ventilated living facilities on campus. Generally, malnutrition, overcrowding, and poor living conditions are risk factors for infectious respiratory diseases, especially in the tropics [18]. Notably, the prevalence rates may differ across the tertiary hospitals and other healthcare facilities in Ota.
In this study, URTI was the most prevalent respiratory disease, with 82.8% of all patients. This finding agrees with a previous case series report in which URTI was the most common infectious respiratory disease [13]. However, this contradicts reports from other studies in Nigeria, where tuberculosis and pneumonia were the most common [15]. Infectious diseases contribute significantly to the burden of respiratory diseases in developing countries. In Nigeria, lower respiratory tract infections and tuberculosis are the leading causes of death, accounting for 4% of all deaths [19].
The mean age of the study group was 26.6 ± 15.6 years, with a male predominance, as in other studies. [17, 20, 21] Asthma was more prevalent among adult females aged 31 and older. The findings of this study suggest that sex is an important factor in the development of respiratory diseases such as URTI and asthma. Specifically, females appear less susceptible to URTI than males but are more susceptible to asthma than males. Previous studies have also reported sex-related disparities in the prevalence of respiratory diseases [12, 13, 15, 16]. Several factors have been associated with sex-related differences in the prevalence of respiratory diseases, including asthma and COPD. Furthermore, sex and gender affect the presentation, diagnosis, treatment, and outcomes of various diseases [22]. These factors include genetics, environmental exposure to triggers/smoke, immunological responses, and sex hormones. For females, hormones modulate the immune pathways involved in asthma pathogenesis and influence the response to environmental triggers and medications.
Nigeria has two major seasons: the rainy season, which occurs between April and October, and the dry season between November and March [23]. During the dry season, the harmattan period, characterized by dry and dusty air, begins in December, peaks in January, and declines in February. In this study, the seasonal patterns of respiratory diseases show a multi-peak period, with two peaks in the rainy season and the highest number of cases in October. During the dry season, a surge in cases was observed between January and February during harmattan. Correlations between seasonality, pneumonia, and URTI were also observed (p<0.05). Respiratory infections are more common during the rainy season in temperate regions. Cold temperatures and reduced sunlight lower immunity and keep viral respiratory pathogens viable for extended periods, thus increasing transmission rates [7, 8]. In the tropics, viral respiratory diseases have shown seasonality during rainy seasons and are positively correlated with increased rainfall and humidity [24, 25].
The surge observed in respiratory cases, especially URTI during January-February in the dry season, is notable. Dry and dusty winds in the Sahara characterize these months. The dust of the Harmattan wind has been identified as a risk factor for respiratory tract infections and asthma [26-29]. A study in the Sahel region of Niger revealed that airborne dust particles increased the carriage of pathogens through the nasal passage, impaired immune function, and contributed to lung inflammation, promoting respiratory infections [28]. In light of climate change, which is expected to exacerbate the frequency and intensity of extreme weather events [29, 30], insights into the seasonality of respiratory diseases can inform preparedness strategies. For example, anticipating the impact of longer and more intense harmattan periods on respiratory health can guide the development of early warning systems and adaptive measures to protect public health.
The data indicating a higher incidence of Upper Respiratory Tract Infections (URTI) and asthma during specific seasons, such as the rainy season and the harmattan period, can be instrumental in developing targeted public health interventions. For instance, the peak activity in October and the surge in cases during January and February suggest that health services could allocate more resources and prepare for increased patient loads during these times. This could include building up reserves of necessary medications, increasing the availability of healthcare personnel, and setting up specialized clinics to handle the influx of respiratory cases.
Overall, leveraging the study’s findings can enhance disease surveillance, resource allocation, and public health messaging, ultimately contributing to more resilient health systems capable of managing the current and future challenges posed by respiratory diseases and climate change.
There are certain limitations to the present study. This was a retrospective study, and data on socioeconomic status, disease severity, and mortality rates were unavailable. The University break periods may have impacted the number of cases during certain months. COVID-19 cases were excluded from the study as this facility is not accredited to handle such cases. As this study was based on a single health facility, future studies will need to include multiple facilities to improve the generalizability of the findings.
CONCLUSION
This study has provided more information on the burden of respiratory diseases with respect to seasonal variation. These findings support the need for public awareness of the prevention and control of respiratory diseases based on seasonal and location-specific realities. Furthermore, the knowledge of the peak period of respiratory diseases is valuable for health planning and policies.
AUTHORS’ CONTRIBUTION
OA, AE, and OO contributed to the study’s concept and design. AA collected the data and OO analyzed the data and performed the interpretation. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| CT | = Computed Tomography |
| URTI | = Upper Respiratory Tract Infections |
| OR | = Odds Ratio |
| CHREC | = Covenant Health Research Committee |
| DQN | = Deep Q-Networks |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study received ethical approval from the Covenant Health Research Committee (CHREC), Nigeria with approval number CHREC 154/2020.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was not required as patients were not interviewed, and data was obtained retrospectively from the medical records. All data accessed from clinical records were anonymized to maintain confidentiality.
AVAILABILITY OF DATA AND MATERIAL
All data generated or analyzed during this study are included in this published article.
FUNDING
The Covenant University Center for Research, Innovation, and Discovery (CUCRID) is acknowledged for sponsorship of the publication of this article.
CONFLICT OF INTEREST
Ademola O. Adebanjo is the Chief Medical Officer at the Covenant University Medical Centre Nigeria. The other authors have no relevant financial or non-financial interests to disclose.
ACKNOWLEDGEMENTS
The authors acknowledge the staff of the Records Unit at Covenant University Medical Centre for their assistance with data collection.


