All published articles of this journal are available on ScienceDirect.
Knowledge, Behaviors, and Treatment Associated with Sexually Transmitted Diseases: A One-Group Pretest-Posttest Study among Vietnamese Patients
Abstract
Background
Sexually Transmitted Diseases (STDs), commonly referred to as venereal diseases, encompass several contagious ailments caused by a diverse array of microorganisms that vary in symptomatology, size, life cycle, and treatment resistance. The pathogens responsible for STDs include bacteria, viruses, fungi, and protozoa. Despite the diversity of STD pathogens, public understanding of transmission, prevention, and treatment remains limited. Additionally, changes in knowledge, behaviors, and treatment practices following non-pharmacological interventions remain controversial.
Objective
This research aimed to assess the STD status, knowledge, and behaviors of Vietnamese patients who visited the urology clinic at Le Van Thinh Hospital before and after both pharmacological and non-pharmacological interventions.
Materials and Methods
A one-group pretest-posttest design was used to assess the impact of interventions on knowledge, behaviors, and treatment related to STDs. Participants (n=108) were evaluated 1 week and 3 months post-intervention. The interventions included pharmacological treatment, administered according to the Vietnam Ministry of Health guidelines, and non-pharmacological interventions, including counseling, education, and awareness programs covering STD transmission, complications, prevention (e.g., condom use, health check-ups), and behavioral change. Data were collected through direct interviews, and SPSS was used for statistical analysis, with McNemar’s non-parametric test employed to assess changes over time.
Results
Of all participants, 86.1% had gonorrhea. Remarkably, a complete lack of condom use was noted (100%). Before the intervention, 64.8% of participants were found to have either below-average or average levels of understanding of STDs, and 100% participated in at least one risky behavior. Health education efforts led to a positive outcome, with 100% of participants showing good awareness. The majority of participants also showed reduced risky behaviors, with 52.8% using condoms. The therapeutic intervention achieved a 100% cure rate after 3 months, but limitations remained in the first week of treatment as three of the selected diseases demonstrated a treatment level of ≤ 25%.
Discussion
Our study reported a high figure for the incidence of sexually transmitted infections, alongside frequent high-risk behaviors. Moreover, limited knowledge about STDs reflects persistent gaps in awareness and preventive efforts. Non-pharmacological interventions helped patients improve awareness and reduce risky behaviors. Although treatment outcomes were favorable, the small sample size may reduce accuracy and generalizability.
Conclusions
The majority of the STD patients lacked knowledge and had a history of engaging in risky behaviors. The study demonstrated the effectiveness of current treatment protocols as well as the importance of education in increasing awareness and preventing risky behaviors.
1. INTRODUCTION
Sexually Transmitted Diseases (STDs) are widespread infections, primarily affecting young people. The World Health Organization (WHO) reports millions of new cases daily, but the true burden remains uncertain due to asymptomatic cases, limited diagnostics, and inadequate surveillance systems worldwide [1, 2]. STDs impact both physical and mental health, with a risk of vertical transmission during pregnancy. Syphilis can cause stillbirth and neonatal complications, while human papillomavirus may lead to cervical cancer. Gonorrhea and chlamydia increase the risk of pelvic inflammatory disease, infertility, and premature birth [1, 3]. Owing to their prevalence and associated problems, STDs substantially impact on the quality of life and mortality rates. Thus, the issue has transcended the strictly medical context, entering the domain of urgent societal responsibilities [2, 4]. In recent years, the prevalence of STDs has risen markedly due to the premature initiation of sexual activity, frequent partner changes, disregard for condom usage, insufficient sex education, and self-medication, among other factors [5, 6].
The decreasing age at which sexual intercourse begins has been identified as a contributing factor to the rise in STD incidence [5, 7]. Data from several European nations indicate that the average age of initial sexual intercourse has declined over the past 30 years, with a growing percentage of adolescents reporting sexual activity before the age of 16 years [8]. The premature initiation of sexual activity elevates the likelihood of engaging with several sexual partners and heightens the risk of acquiring a sexually transmitted infection [9, 10]. The risk is elevated for female teenagers due to their underdeveloped cervical anatomy, rendering them particularly susceptible to specific STDs [10]. Adolescents often avoid condoms due to inexperience or discomfort and focus solely on pregnancy prevention, reducing STD protection [9]. Moreover, numerous adolescents do not consider themselves at risk of acquiring STDs [11]. As the number of STD clinics has diminished, patients have increasingly sought care for STDs at general care clinics, emergency rooms, and family planning clinics [12]. General care physicians play a key role in STD detection, as many cases are asymptomatic. Primary care clinics diagnose up to 50% of reported STDs [7, 10]. In 2022, 71% to 80% of STD cases were recorded from non-STD clinics [13]. Expanded health insurance led to a 100% increase in primary care visits for STD care, while visits to STD clinics dropped by 20%. The rise was mainly driven by more women seeking STD treatment [14, 15]. Notwithstanding these changes in the venues for STD service delivery, publicly financed STD clinics remain a crucial safety net for uninsured individuals and other vulnerable groups seeking care [11].
Managing STDs is complicated due to the prevalence of asymptomatic or moderate infections, which complicate detection. The variety of infectious comorbidities and social stigma also hinder patient-centered care; thus, multidisciplinary management is crucial [10, 12]. The WHO promotes STD education to reduce the disease burden. A study found that young students were mostly aware of Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome (HIV/AIDS), with limited knowledge of other STDs, mainly acquired from the Internet and media [9, 11, 16]. Many people, especially in developing countries, underestimate STD risk and lack awareness. Therefore, understanding symptoms and prevention is crucial to reducing transmission and infection rates [5, 7].
The incidence of STDs in metropolitan regions and megacities is rising. Previous studies have elucidated a correlation between the proliferation of STDs and extensive urbanization and migration. Moreover, in underdeveloped nations, STDs have been demonstrated to adversely affect public health, significantly impacting morbidity and mortality rates. Research on STDs in Vietnam is limited; therefore, this study aimed to assess the STD status, knowledge, and behaviors of participants and to evaluate changes in their knowledge and behaviors before and after intervention.
2. MATERIALS AND METHODS
2.1. Study Design and Setting
Our study involved a one-group, pretest-posttest design and was conducted on 108 patients who visited the urology clinic at Le Van Thinh Hospital, Thu Duc City, for STD testing and treatment. Participants were invited to complete 20-minute face-to-face interviews using structured questionnaires administered by well-trained researchers.
2.2. Sample Size
The following formula was used:
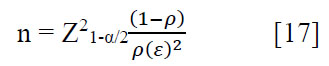 |
In this formula, n is the sample size; Z1-α/2 = 1.96 is the 95% confidence interval; ρ = 90.8% is the proportion of patients who understand STDs [5]; and ε = 0.062 is a relative precision, calculated as 6.2% of ρ. Substituting the relevant values into the above formula, the minimum sample size for the study was 102 patients; in total, 108 patients were included.
2.3. Pilot Study
A pilot study was conducted to assess the suitability of the questionnaire, evaluate the data collection process, and estimate initial parameters in preparation for the main study. The pilot study was conducted on a small sample of 20 individuals representing the target population, using direct interviews as the data collection method. This process included administering the survey, assessing participants’ feedback, and evaluating input on the clarity of the questions, completion time, and any issues encountered during implementation. The results helped identify errors or limitations in the questionnaire design and provided preliminary data for adjusting the sample size for the main study.
2.4. Interventions
Pharmacological interventions were administered based on the identified causative agents, strictly adhering to the treatment regimens outlined in the general guidelines of the Ministry of Health (Vietnam) to ensure standardized and effective care. Additionally, non-pharmacological interventions focused on educating the study subjects about their conditions and raising awareness of STDs were administered. These educational efforts included providing comprehensive information on the nature, transmission, and potential complications of STDs, as well as equipping individuals with knowledge of preventive measures, such as safe sexual practices, condom use, and regular health check-ups. To reinforce awareness, counseling sessions were conducted, and educational materials were disseminated to foster long-term behavioral changes that could contribute to reducing disease transmission within the community.
2.5. Data Collection
The questionnaire was developed in Vietnamese with additional revisions suitable for Vietnamese patients (Supplementary Material). It was divided into six parts (eight questions about socioeconomic characteristics, 10 questions about the participants’ STD status and risky behaviors, 18 questions about their awareness of STDs before and after intervention, four questions about treatment results after a week, four questions about treatment results after 3 months, and 10 questions about behaviors before and after intervention) and comprised multiple-choice questions (Fig. 1).
2.6. Questionnaire Validity
To validate the questionnaire on STD-related knowledge, behaviors, and treatment in a one-group pre-post study, key statistical methods were used to ensure reliability. Content validity was assessed by experts using the content validity index, requiring a score of ≥ 0.80. Criterion validity was determined by comparing questionnaire scores to a gold standard using Pearson’s correlation, with an acceptable r > 0.7.
2.7. Reliability Analysis
Reliability analysis ensured that the questionnaire on STD knowledge, behaviors, and treatment consistently measured what it intended. Internal consistency was assessed using Cronbach’s alpha (≥ 0.7), while test-retest reliability evaluated stability over time with the intraclass correlation coefficient (≥ 0.75). Together, these methods confirmed the questionnaire’s dependability for research and public health.
2.8. Data Analysis
Data from the collected forms were entered and processed using SPSS 20.0 software and medical statistics methods. Descriptive statistics (frequencies and percentages) were used for the following qualitative variables: gender, age group, marital status, occupation, education, income, place of residence, history of STDs, STD status, risky behaviors for STDs, and treatment outcomes. Comparative analysis of changes in knowledge and behaviors about STDs before and after intervention was performed using McNemar’s non-parametric test.
2.9. Ethical Considerations
All study participants provided informed consent before data collection, having fully understood the purpose, risks, and benefits of their participation. To protect participants’ personal information, strict confidentiality measures were implemented. All collected data were anonymized, securely stored in encrypted databases, and accessible only to authorized researchers. Identifiable information was removed or coded to prevent any link to individual participants. Additionally, no personal data were shared or disclosed beyond the research team. Participants had the right to withdraw at any stage without consequences, ensuring that their autonomy and privacy were fully respected.
3. RESULTS
3.1. Sociodemographic Characteristics of the Participants
Table 1 shows that most participants were men aged 20–49, unmarried, and residing in urban areas. They worked in various professions, primarily as workers and office staff, most of whom had an education level of high school or higher and a high income, in contrast to those with lower income and educational attainment. Furthermore, most participants reported no history of STDs, while a small proportion had previously contracted gonorrhoea.
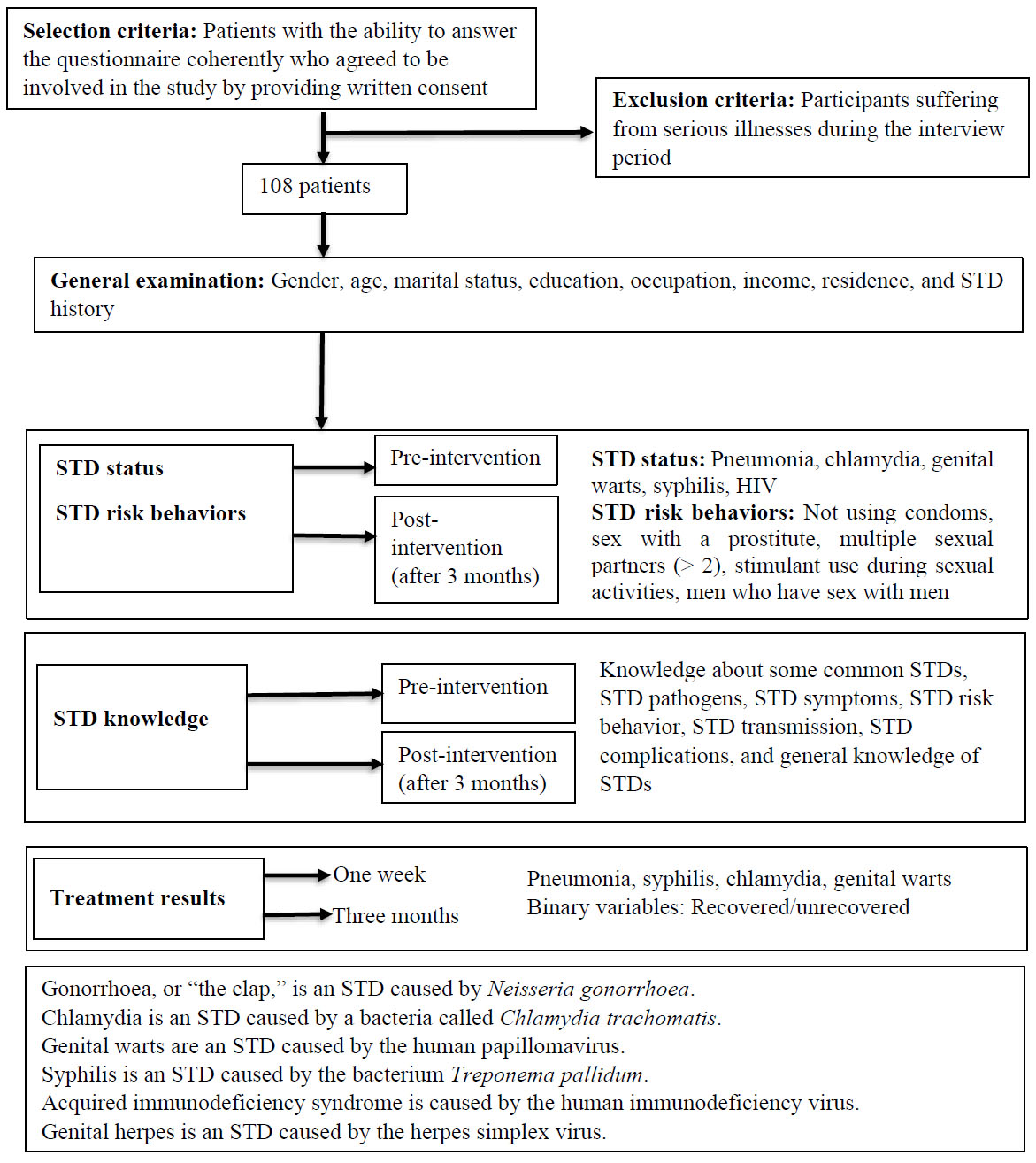
Study flowchart.
| Characteristics | Frequency | Percentage (%) | |
|---|---|---|---|
| Age | < 20 | 5 | 4.6 |
| 20–29 | 42 | 38.9 | |
| 30–39 | 34 | 31.5 | |
| 40–49 | 18 | 16.7 | |
| 50–59 | 6 | 5.6 | |
| ≥ 60 | 3 | 2.7 | |
| Gender | Male | 105 | 97.2 |
| Female | 3 | 2.8 | |
| Marital status | Unmarried | 53 | 49.1 |
| Married | 31 | 28.7 | |
| Divorced/widowed | 24 | 22.2 | |
| Education level | Elementary | 9 | 8.3 |
| Secondary | 14 | 13.0 | |
| High school | 43 | 39.8 | |
| College/university/postgraduate | 42 | 38.9 | |
| Occupation | Office staff | 28 | 25.9 |
| Worker | 27 | 25.0 | |
| Driver | 15 | 13.9 | |
| Trader | 16 | 14.8 | |
| Student | 12 | 11.1 | |
| Farmer | 5 | 4.6 | |
| Others | 5 | 4.6 | |
| Income | High-income | 78 | 72.2 |
| Upper-income | 16 | 14.8 | |
| Middle–income | 7 | 6.5 | |
| Low-income | 7 | 6.5 | |
| Residence | Urban | 76 | 70.4 |
| Rural | 32 | 29.6 | |
| History of STDs | No | 94 | 87.0 |
| Yes (gonorrhoea) | 14 | 13.0 | |
3.2. STD Status and Risky Behaviors of the Participants
As summarized in Table 2, most participants had already been diagnosed with STDs (primarily gonorrhea) at enrollment. The most common risky behavior was a lack of condom use, followed by having sex with sex workers. In contrast, only a few were positive for HIV or syphilis. Additionally, men who have sex with men (MSM) represented a small proportion of the study group.
3.3. Treatment Results
The treatment efficacy observed after the first week was relatively low, with three of the selected diseases demonstrating a treatment level of ≤ 25%, no recovery among syphilis cases, and only chlamydia reaching 100% efficacy. However, after 3 months, all patients achieved full recovery. These results are presented in Table 3.
3.4. Participants’ Behaviors regarding STDs Before and After the Intervention
Table 4 shows positive changes regarding the participants’ involvement in reducing risk factors and enhancing preventive measures, including increased condom use and reduced sex with sex workers. However, only a minority completely avoided all risky behaviors post-intervention.
| Characteristics | Frequency | Percentage (%) | |
|---|---|---|---|
| STD status | Gonorrhoea | 93 | 86.1 |
| Chlamydia | 7 | 6.4 | |
| Genital warts | 4 | 3.7 | |
| Syphilis | 2 | 1.9 | |
| HIV/AIDS | 2 | 1.9 | |
| Risky behaviors | Not using condoms | 108 | 100 |
| Having sex with sex workers | 89 | 82.4 | |
| Multiple sexual partners (≥ 2) | 74 | 68.5 | |
| Stimulant usage during sexual activities | 54 | 50.0 | |
| Men who have sex with men | 11 | 10.2 | |
| STDs | Cases | Treatment Success After a Week | Treatment Success After 3 Months | *p-value | ||
|---|---|---|---|---|---|---|
| Frequency | Percentage (%) | Frequency | Percentage (%) | |||
| Gonorrhoea | 93 | 5 | 5.4 | 93 | 100 | < 0.001 |
| Syphilis | 2 | 0 | 0 | 2 | 100 | 0.157 |
| Chlamydia | 7 | 7 | 100 | 7 | 100 | 1 |
| Genital warts | 4 | 1 | 25 | 4 | 100 | 0.0832 |
| Characteristics | Pre-intervention | Post-intervention | *p-value | ||
|---|---|---|---|---|---|
| Frequency | Percentage (%) | Frequency | Percentage (%) | ||
| Sexual partners | |||||
| 1 person | 34 | 31.5 | 42 | 38.9 | < 0.001 |
| At least 2 people | 74 | 68.5 | 66 | 61.1 | |
| Having sex with sex workers | |||||
| Yes | 89 | 82.4 | 45 | 41.7 | < 0.001 |
| No | 19 | 17.6 | 63 | 58.3 | |
| Using condoms | |||||
| Yes | 0 | 0.0 | 57 | 52.8 | < 0.001 |
| No | 108 | 100 | 51 | 47.2 | |
| Men who have sex with men | |||||
| Yes | 11 | 10.2 | 8 | 7.4 | < 0.001 |
| No | 97 | 89.8 | 100 | 92.6 | |
| Risky behaviors in general | |||||
| Yes | 108 | 100 | 94 | 87.0 | < 0.001 |
| No | 0 | 0 | 14 | 13.0 | |
3.5. Participants’ Knowledge about STDs Before and After the Intervention
As presented in Table 5, most participants had a medium level of knowledge about STDs, especially STD symptoms, common risky behaviors, and transmission routes, such as having sexual intercourse without condoms. However, few were aware of parasitic causative agents, transmission through unsafe blood transfusions or needle sharing, and complications. After the intervention, the participants achieved excellent knowledge levels compared to before, particularly on STD complications and transmission routes.
| Characteristics | Pre-intervention | Post-intervention | *p-value | ||
|---|---|---|---|---|---|
| Frequency | Percentage (%) | Frequency | Percentage (%) | ||
| Knowledge about common STDs | |||||
| Gonorrhoea | 101 | 93.5 | 107 | 99.1 | 0.003 |
| Syphilis | 88 | 81.5 | 107 | 99.1 | < 0.001 |
| Genital warts | 83 | 76.6 | 105 | 97.2 | < 0.001 |
| HIV/AIDS | 76 | 70.4 | 108 | 100 | < 0.001 |
| Genital herpes | 23 | 21.3 | 83 | 76.9 | < 0.001 |
| Chlamydia | 13 | 12.0 | 55 | 50.9 | < 0.001 |
| Trichuris trichiura | 7 | 6.5 | 31 | 28.7 | < 0.001 |
| Knowledge of STD pathogens | |||||
| Virus | 84 | 77.8 | 105 | 97.2 | < 0.001 |
| Bacteria | 75 | 69.4 | 105 | 97.2 | < 0.001 |
| Trichomonas, Candida, Sarcoptes scabiei, Pthirus pubis | 20 | 18.5 | 85 | 78.7 | < 0.001 |
| Knowledge of STD symptoms | |||||
| List at least three correct symptoms | 93 | 86.1 | 108 | 100 | < 0.001 |
| List fewer than three symptoms | 15 | 13.9 | 0 | 0 | < 0.001 |
| Knowledge of STD risky behaviors | |||||
| Not using condoms | 99 | 91.7 | 108 | 100 | < 0.001 |
| Having sex with sex workers | 89 | 82.4 | 106 | 98.2 | < 0.001 |
| Multiple sexual partners | 59 | 54.6 | 104 | 96.3 | < 0.001 |
| Unsafe blood transfusion | 33 | 30.6 | 79 | 73.2 | < 0.001 |
| Knowledge of STD transmission | |||||
| Sexual activities | 102 | 94.4 | 105 | 97.2 | < 0.001 |
| Blood transfusion | 48 | 44.4 | 101 | 93.5 | < 0.01 |
| From mother to child | 46 | 42.6 | 92 | 85.2 | < 0.001 |
| Sharing a needle pump | 38 | 35.2 | 61 | 87.0 | < 0.001 |
| Knowledge of STD complications | |||||
| List at least three complications | 48 | 44.4 | 107 | 99.1 | < 0.001 |
| List fewer than three complications | 60 | 55.6 | 1 | 0.9 | < 0.001 |
| Quality of knowledge about STDs | |||||
| Bad | 31 | 28.7 | 0 | 0 | < 0.001 |
| Medium | 39 | 36.1 | 0 | 0 | < 0.001 |
| Good | 31 | 28.7 | 12 | 11.1 | < 0.001 |
| Excellent | 7 | 6.5 | 96 | 88.9 | < 0.001 |
4. DISCUSSION
4.1. Sociodemographic Characteristics of the Participants
The characteristics of our study cohort were consistent with those typically observed among patients visiting the urology department of Le Van Thinh Hospital. Existing research also indicates that men are significantly more likely than women to seek clinical care for STDs. Besides, changes in sexual behavior raise the risk of STDs in women, especially genital warts [18]. These gender differences may be attributed to the fact that sexual health remains a sensitive topic for many women. In numerous Asian cultures, persistent cultural stigma continues to discourage open discussion of STDs among women.
The large number of participants within the age range of 20–29 stems from the fact that this final stage of sexual development, coupled with curiosity, leads individuals to have a strong tendency to engage in sexual activities. Moreover, individuals want to prove their maturity and experience in the field of sexuality. Therefore, many of them seek out sexual activities. The above speculation is reinforced by a study conducted by Hanoi Medical University on 873 male patients who had STDs. The incidence of STDs in the age group of 20–30 years accounted for 44.33% of cases, and this age group was determined to be the one with the highest levels of physiological activity and sexual impulses that tended to seek out sexual partners to satisfy physiological needs [19]. In addition, the WHO estimated that, in addition to AIDS, if only four treatable diseases are taken into account (trichomonas, chlamydia, polio, and syphilis), more than 340 million new cases occur globally among 15–49-year-olds, underscoring this high-risk demographic [20]. Due to the complex nature of sexual life and the high rates of STDs reported previously, further research is required on this at-risk age group.
The fact that the majority of study participants were single and not bound by marriage and romantic relationships led them to engage in more vigorous sexual activity compared to those who were married or in a romantic relationship. Similarly, in a study conducted in 2022 on male subjects with STDs at the Hanoi Medical University Hospital, unmarried participants accounted for almost half of the participants, at 46.09% [19]. Conversely, a study on patients who visited the Suraksha Clinic under the Dermatology Department in Lady Hardinge Medical College, New Delhi state, India, from 2003 to 2019 found that the prevalence of STDs was higher in married people (81.7%) than in unmarried people (17.9%) [21], highlighting how cultural norms shape epidemiological patterns.
We observed a relationship between academic qualifications and the incidence of STDs because the majority of individuals with STDs had an education level of high school or higher. The high STD infection rate among individuals with a high school education or above contradicts initial assumptions, as these individuals are typically well-equipped with knowledge about STDs. However, these results show some similarities with a study revealing that academic qualification from the high school level onward accounted for 88.2% of 622 patients examined at the Vietnam National Hospital of Dermatology and Venereology from September to November 2018 [22]. In a 2021 study on drug use and health conducted by the United States Intramural Research Program at the National Institutes of Health, approximately 32.43% of participants held a college degree or higher [23]. Interestingly, the rising rates of STD infections among individuals with higher education levels may reflect a lack of emphasis on sexual health education and a general indifference toward preventive measures. This may be particularly true in educational systems where sex education is not prioritized alongside core subjects, such as English and mathematics. Further research is needed to better understand the underlying factors contributing to this concerning trend among well-educated populations.
Occupation and accommodation status also influenced the study results. The characteristics of an individual’s living environment and educational background can shape their cognitive processes and health-related behaviors. In our study, most participants were laborers or students—groups that often have limited exposure to public health education programs and possess less knowledge about sexual health and safety. Moreover, rapid urbanization and the pursuit of economic opportunities have led to population growth in major cities, particularly in Ho Chi Minh City. This demographic shift complicates epidemiological control and contributes to rising rates of STDs in urban areas, as also reported in Smith’s study on the Asia-Pacific region [24]. Additionally, higher income levels may enable engagement in riskier behaviors, such as substance use and relationships with sex workers, further increasing STD risk. However, it is equally important to consider rural and low-income populations, who often lack access to healthcare services and may, therefore, be underrepresented in official statistics. These findings highlight the need for further research into the relationships between place of residence, income level, and STD prevalence.
4.2. Incidence of STDs and Risky Behaviors of Patients with STDs
4.2.1. Incidence of STDs
Since this study was conducted during the fourth phase of the coronavirus disease 2019 (COVID-19) pandemic, when Vietnam implemented social distancing measures, along with the general apprehension of the public and patients regarding the risk of COVID-19 transmission, the capacity for screening tests and the identification of individuals who have been or are at risk of contracting STDs was limited. On the other hand, prioritizing resources for preventing the COVID-19 pandemic may have led to reduced testing and diagnosis of at-risk individuals. Therefore, according to the researchers’ estimates, the number of people with STDs may be much higher.
Furthermore, a study in Vietnam reported a rapid increase in the incidence of sexually transmitted infections over the past decade, reaching 17.3% in 2017, with an estimated 200,000 new cases annually [25]. Similarly, a major survey conducted in the United States in 2018 identified up to 32 million men living with an STD [26]. This substantial pre-pandemic burden, combined with the current lack of widespread screening, raises concerns about a potential significant rise in sexual health issues following the COVID-19 pandemic.
The majority of patients in our study were diagnosed with gonorrhea, making it the most commonly identified STD in our sample. This distribution aligns with the prevalence patterns reported in previous studies. For example, in Spain, the incidence of gonorrhea has been increasing since the early 2000s [27]. Additionally, a WHO study reported over 82 million cases of gonorrhea globally in 2021 alone [28]. The higher prevalence of gonorrhea compared to other STDs may be attributed to its high transmissibility and the growing antimicrobial resistance of Neisseria gonorrhoeae to all therapeutic antibiotics [29], which reduces treatment efficacy [28]. Furthermore, many individuals with gonorrhea, especially women, often exhibit no obvious symptoms or only mild signs, such as unusual vaginal discharge, pain during urination, and lower abdominal pain, symptoms that are commonly mistaken for other urinary tract infections.
Although HIV/AIDS was recorded at a low rate in our study, it remains a significant public health concern due to challenges in controlling its spread, particularly driven by unsafe sexual practices and increased injection drug use. Notably, sexual transmission of HIV among MSM has risen rapidly in recent years. According to the Department of Prevention, Anti-HIV/AIDS (Vietnam Ministry of Health), the primary modes of HIV transmission in Vietnam are needle sharing among people who inject drugs and sexual contact with sex workers. However, sexual transmission, especially within the MSM population, has been on the rise [30]. The average HIV infection rate among MSM increased from 6.7% in 2014 to 12.2% in 2017, reaching 13.3% in 2020. In some regions, more than 50% of newly diagnosed HIV cases were among MSM. Despite this, in Ben Tre province in southern Vietnam, only 79% of MSM had undergone HIV testing in 2018 [31]. Sexual activity among MSM is recognized as a major risk factor driving the HIV epidemic both in Vietnam [32] and globally [20]. Therefore, further research focused on the sexual health needs of MSM populations is urgently needed.
4.2.2. Risky Behaviors
This study included several questions targeting behaviors known to be risk factors for disease transmission, particularly unsafe sexual practices extensively documented in public health reports, media, and legal texts. Alarmingly, all participants reported not using condoms, a finding that raises significant concerns. The absence of condom use eliminates the physical barrier that prevents direct contact between genitalia and bodily fluids, thereby facilitating pathogen transmission. Notably, many studies have consistently reported low rates of condom use among young people [31].
In addition to inconsistent condom use, the relatively high proportion of individuals engaging in sexual activity with multiple partners serves as a further warning sign. Having multiple sexual partners increases the likelihood of pathogen exposure and complicates efforts to monitor and manage individuals' health status. For men, each additional sexual partner increases the risk of contracting STDs by approximately 6% [33]. Moreover, sexual relations with multiple partners contribute to cross-transmission within the community, particularly among sex workers, who frequently have unprotected sex with multiple clients. This makes them highly vulnerable to STDs and accelerates disease spread. Reported STD rates among female sex workers range from approximately 33% to 50% [34].
Alcohol and drug use before and during sexual activity remain important contributing risk factors. In Brookmeyer’s study, the proportion of stimulant users was notably high at 86.4%, with a statistically significant p-value of less than 0.001 [35]. This finding strongly suggests a link between stimulant use and an increased risk of STDs. One possible explanation for this association is that stimulant use impairs self-control and decision-making abilities. Individuals under the influence of stimulants often experience heightened impulsivity, reduced inhibitions, and impaired judgment. As a result, they may engage in risky sexual behaviors, such as unprotected sex or multiple sexual encounters, without fully considering the potential consequences. The stimulating effects of these substances can lead to reckless and spontaneous decisions, further increasing the likelihood of STD transmission [36].
Besides these widely known factors, homosexual relationships are also notable, even though they have not yet emerged as a predominant source of STDs in the general community. This population is considered at elevated risk due to the biological vulnerability associated with unsafe sexual practices, such as anal sex and oral sex, leading to higher transmission rates of STDs [37]. Additionally, stigma and discrimination toward homosexuality prevent such individuals from accessing healthcare services, resulting in many MSM not receiving timely testing and treatment. A 2014 report from the United States Centers for Disease Control and Prevention showed that of the total of 91% of syphilis cases in men, 83% were among MSM. Moreover, MSM accounted for up to 51% of reported HIV cases across 26 states in the United States [38]. Further research is essential to develop solutions aimed at reducing the STD rate among this group.
4.3. Participants’ Knowledge about STDs
Despite ongoing efforts to raise public awareness about STDs, our findings identified a relatively low level of understanding. Such limited knowledge may contribute to increased transmission of STDs. Other studies have also noted that a lack of understanding regarding STDs can hinder disease prevention efforts [34, 39]. Although our results indicated that most participants demonstrated knowledge of common STDs, a significant proportion lacked understanding of less common STDs, such as chlamydia, which are becoming potential threats due to a recent rise in incidence [22].
Viruses and bacteria were widely recognized as causative agents. In contrast, parasites were less commonly identified, likely because they are rarely mentioned in the media and may be easily confused with viruses and bacteria due to a lack of knowledge. Interviews with rural Vietnamese women on their knowledge of STDs revealed that 17% of participants classified Pthirus pubis as an STD pathogen, while 52% and 34%, respectively, classified it as bacterial candida and vaginitis [40]. Such misconceptions pose significant challenges to disease prevention and treatment, particularly in underserved areas with limited access to diagnostic equipment.
STD symptoms were widely recognized in this study. In contrast, Nguyen Huu Sau reported that patients could only list some symptoms of STDs, including urethral ulcers (53.5%), genital redness (49.6%), and genital ulcers (48.8%) [22]. Moreover, in Mansor’s research, about 90% of participants stated that STD patients may not show any symptoms or signs [41]. These previous studies differ from our research in the level of understanding regarding STD symptoms. This difference may stem from variations in sample size and the level of knowledge about STDs between residential areas.
Regarding STD complications, a relatively low percentage of participants were aware of the potential consequences. This finding aligns with a study conducted among college students in India, where fewer than 50% of respondents had knowledge about STD complications [ 42 ]. The lack of awareness, particularly among individuals with higher education levels, may be attributed to limitations in sexual health education and psychological reluctance to openly address sexual health issues. Furthermore, public health efforts have often focused on disseminating information about a limited number of common STDs, resulting in insufficient knowledge about other infections. For example, previous studies in Vietnam have demonstrated low levels of accurate knowledge concerning complications associated with chlamydia, such as male infertility, pelvic inflammatory disease, and ectopic pregnancy [ 43 ], largely because chlamydia remains relatively unknown in the general population.
Not using condoms remains a significant and well-recognized risk factor for STD transmission, as widely highlighted in both research and media outlets. A study in Brazil on military recruits also reached a similar conclusion, with 97.2% of participants believing that not using condoms during sexual intercourse increases the risk of contracting STDs [44]. Although participants were aware of the potential dangers of risky behaviors in Mansor’s study, they could not name the two most effective preventive measures for STDs, that is, having sexual relations with one partner and using condoms during sexual intercourse [41]. The aforementioned study reflects the reality that important methods for preventing STDs are not well known, even though there is considerable knowledge about risky behaviors.
Apart from sexual intercourse being widely recognized as a common transmission route, only a few participants were unaware of the remaining transmission pathways, such as blood transfusion, mother-to-child, and needle sharing, which originally received little attention. This raises concerns about the lack of preventive measures for unpopular transmission pathways, particularly regarding needle sharing, due to its relevance to drug use, which is among the main drivers of STD transmission, especially HIV/AIDS [35].
4.4. Treatment Success, Risky Behaviors, and Participants’ Knowledge about STDs After the Intervention
4.4.1. Treatment Success
The clinical success rate for gonorrhea after one week of treatment in our study was comparable to rates reported in other research. For instance, Vanessa and colleagues reviewed medical records of 291 patients infected with Neisseria gonorrhoeae who were treated with cefixime between May 1, 2010, and April 30, 2011, at a sexual health hospital in Toronto, Canada, reporting a success rate of 6.77% [ 45 ]. Similar success rates for cefixime and azithromycin in treating gonorrhea have been observed in studies from the United States and Europe [ 46, 47]. Although all patients in our study achieved full recovery within three months, the initial failure rate after one week raises concerns about increasing antimicrobial resistance, a problem highlighted by other researchers [48]. Continued investigation is needed to develop more effective treatment strategies.
Among five patients treated for genital warts, four underwent minor surgical removal procedures, while one received trichloroacetic acid therapy. However, after one week, two patients who had surgery and the patient treated with trichloroacetic acid continued to exhibit symptoms. This finding is noteworthy, a report indicates treatment effectiveness rates of up to 86% [ 49 ]. It is important to consider, however, that the small sample size in our study may limit the reliability of these results and could contribute to discrepancies in conclusions regarding treatment efficacy.
Regarding chlamydia, complete success was achieved when the general guidelines of the Ministry of Health (Vietnam) were applied. Similar results were noted in MSM subjects with rectal chlamydia, where 100% of the cases in the doxycycline treatment group recovered, while only 74% of the subjects in the azithromycin treatment group showed positive results [50]. However, azithromycin is highly regarded for treating patients with erratic healthcare-seeking behaviors, poor treatment compliance, or unpredictable follow-up due to its single-dose regimen [51]. Therefore, the appropriate treatment plan should be decided based on the patient’s lifestyle and work characteristics.
Syphilis treatment is based on benzathine penicillin 2.4 million units, with the appropriate injection dosage depending on the disease stage. Alternative therapies are considered in cases of low treatment effectiveness. According to the European guideline on the management of syphilis, intramuscular procaine penicillin for 10–14 days is the second-line option, along with other alternatives, such as doxycycline or azithromycin in cases of coagulopathy, penicillin allergy, or refusal of injectable treatment [52]. However, in clinical practice, the therapeutic efficacy of these alternative therapies is often limited, with reports of drug resistance to azithromycin and a higher failure rate for doxycycline compared to benzathine penicillin [53, 54]. Therefore, benzathine penicillin remains the most trusted choice. Given the decreasing effectiveness of treatment, further research is needed to identify appropriate therapies for syphilis.
4.4.2. Risky Behaviors and Participants’ Knowledge After the Intervention
The results of this quasi-experimental study indicated that the STD risk prevention intervention administered to patients at Le Van Thinh Hospital increased and sustained knowledge about STDs as well as promoted safer sexual behaviors, with monitoring indicating a reduction in STD prevalence. Our research provides evidence that effective educational interventions lead to gains in knowledge about STDs and shows that behavioral intentions can be modified toward “safer” sexual activities.
Through knowledge-sharing consultations, brochure distribution, and instructions on condom use, successive surveys demonstrated a significant increase in STD-related knowledge throughout the study. The proportion of participants with “excellent” knowledge rose from 6.5% at baseline to 88.9%, while the remaining 11.1% achieved a “good” level of understanding. A statistically significant improvement was also observed in participants' intention to always use condoms. This improvement in condom use is a crucial foundation for preventing and reducing the incidence of STDs. Additionally, the positive changes in STD knowledge contribute to strengthening prevention and control efforts, particularly among adolescents, and may help reduce premarital sexual activity [55]. However, our findings also revealed minimal changes in awareness of other risk factors, such as unsafe blood transfusions and needle sharing. Further research targeting these specific areas is necessary to enhance public understanding.
Overall, this study demonstrates the benefits of STD prevention through comprehensive sex education and educational reform, including the integration of information on STDs, risky behaviors, transmission routes, and less common pathological features. These efforts contribute to improved knowledge, the promotion of safer sexual practices, and a reduction in risky behaviors, particularly among highly educated individuals. The findings may also support the broader use of technology in STD-related education. Experts from the European Society for Sexual Medicine have emphasized that digital sex education, particularly through smartphone applications, is emerging as a new trend in sexual health education [56], offering rapid and accurate access to information and enabling better epidemiological monitoring of target populations.
5. LIMITATIONS
This study is subject to several limitations that should be considered when interpreting the findings. Since the research was conducted during the fourth phase of the COVID-19 pandemic, when Vietnam had implemented a lockdown policy, fewer patients could participate in the study, which limited the sample size. This limits generalizability, reduces accuracy, and decreases the statistical power of the study, as well as increases the margin of error. Additionally, the overreliance on binary (yes/no) questions may have introduced response bias, thereby affecting the objectivity and validity of the data collected. Therefore, further research is necessary to address these weaknesses.
CONCLUSION
Through this research, STD-related epidemiology, knowledge, and behaviors were recorded and summarized. By assessing STD status alongside social and lifestyle characteristics, the study provided insight into the behavioral patterns and knowledge levels of the cohort. Approximately 70% of participants demonstrated either average or below-average knowledge. While most participants were aware of symptoms, risky behaviors, and common transmission routes (such as sexual intercourse and lack of condom use), their understanding of complications, additional risky behaviors, and less common transmission routes (such as parasitic infections and unsafe blood transfusions) was limited. Furthermore, participation in risky behaviors, particularly the universal lack of condom use, contributed to the 100% STD infection rate observed among participants prior to the intervention.
After the intervention, participants demonstrated positive changes, including improved knowledge of causative agents, complications, and transmission pathways, as well as a reduction in risky behaviors. More than half of the participants reported condom use, and there was a noticeable decline in high-risk sexual behaviors among MSM individuals.
We also evaluated the effectiveness of current treatment protocols, which showed positive results after 3 months of treatment but had limited efficacy in the first week. Taken together, this one-group pretest-posttest study provides an objective perspective and a basis for designing measures to prevent, mitigate, and treat STDs.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contributions to the paper: Tam T.T.T. and Truc T.P. were responsible for the study conception and design, as well as data collection. Tin H.N., Tin T.L., and Tran T.N.N. conducted the analysis and interpretation of the results. The initial draft of the manuscript was written by Nghia N.N., Tin T.L., Tran T.N.N., and Tin H.N. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| AIDS | = Acquired Immunodeficiency Syndrome |
| COVID-19 | = Coronavirus Disease 2019 |
| HIV | = Human Immunodeficiency Virus |
| MSM | = Men who have sex with men |
| STDs | = Sexually Transmitted Diseases |
| WHO | = World Health Organization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Ethics Committee in Biomedical Research at Can Tho University of Medicine and Pharmacy in Vietnam (No. 576/PCT-HDDD on July 15th, 2022).
HUMAN AND ANIMAL RIGHTS
The procedure performed in this study involving human participants was by the ethical standards of research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article are available in the Collected data of STD study among Vietnamese Patients at https://doi.org/10.5281/zenodo. 15614618, [57].
ACKNOWLEDGEMENTS
The authors are grateful to Can Tho University of Medicine and Pharmacy in Vietnam for the time and effort they devoted to the study. They also thank Le Van Thinh Hospital for their support during the sample collection period.


