All published articles of this journal are available on ScienceDirect.
Identifying the Associated Risk Factors of Time to First Antenatal Care Contacts among Pregnant Women in Somalia: A Survival Frailty Approach
Abstract
Background
Antenatal care (ANC) utilization offers a wide range of interventions, such as education, counseling, screening, treatment, monitoring, and supporting the health of pregnant women, making it a significant opportunity for expectant mothers. This study aims to investigate the time to the first ANC contact among pregnant women and to identify associated factors by employing the Accelerated Failure Time (AFT) model using different frailty distributions.
Methods
This study used Somalia's Health and demographic survey data. A sample of 3138 women of reproductive age (15-49 years) were included in the study and accelerated failure time (AFT) models with different frailty distributions were compared using information criteria to select the best model.
Results
Among the women included in this study, only 33.1% of them received their first ANC contacts within the recommended time during their pregnancy. A gamma frailty model with log-logistic as base-line distribution was found to be the best model for the time-to-first ANC utilization for our data. The final model, based on the log-logistic gamma frailty, identified marital status, mother's occupation, wanted pregnancy, region, parity, wealth index, education level of mother, persons deciding on mother health care, and media exposure are significant (p-value <0.05) predictors of time to the first ANC contact in Somalia. The final model evidenced a high degree of heterogeneity at an individual level regarding the time to the first ANC utilization in Somalia.
Conclusion
The median time for the first ANC contact among pregnant women was 6.2 months. To ensure accurate analysis and better policy recommendation, different candidate models were compared, and the univariate gamma frailty model with a log-logistic baseline was found to be the most appropriate approach for analyzing time to the first ANC contact among pregnant women. Maternal and child health policies and initiatives must better focus on women's development and implement interventions aimed at increasing the timely initiation of prenatal care services. More specific policy measures, such as targeted educational campaigns, improved pregnancy services, and efforts to minimize regional disparities, should be prioritized as urgent intervention mechanisms.
1. INTRODUCTION
Antenatal care (ANC) utilization offers a variety of interventions, such as counseling, screening, treatment, monitoring, and supporting the health of pregnant women, making it a critical opportunity for expectant mothers [1]. Globally, pregnancy and childbirth complications claim the lives of 830 women every day and over 303,000 women annually [2]. Out of these, only 1% occur in developed countries, while 99% occur in emerging economies [3]. In a 2019 study in Somalia, 84.1% of the participants received antenatal care during their last pregnancy. However, only 28% met the minimum requirements of ANC contacts set by WHO for pregnant mothers [4].
The WHO recommends that all expectant mothers should initiate their ANC follow-up within 12 weeks after conception [5]. The fetus develops at its highest rate during the first trimester of pregnancy, a crucial period when all major organs form and require specific attention [6].
Women in Somalia have one in 22 lifetime risk of maternal death, making its maternal mortality rate (MMR) amongst the highest in the world, estimated to be at 692 deaths per 100,000 live births according to the Somali Health and Demographic Survey done in 2020 [7]. There are several reasons for the high maternal mortality rate in Somalia, amongst them low uptake of antenatal and postnatal care and a low number of deliveries at health facilities or with skilled health care providers [8].
Prior research in Kenya and Uganda found that the duration until the first ANC interaction was five months and seven months, respectively [9, 10]. The Somali Health and Demographic Survey (SHDS) in 2020 reported that 31% of women aged 15–49 received ANC from skilled personnel during their last birth, and 24% of the women had at least 4 ANC contacts [7]. However, only 17% of women received more than two tetanus toxoid injections during their pregnancy [11]. A large proportion of women, 89% of mothers, did not receive any postnatal check-up within the first two days after childbirth [12].
Regarding factors influencing the time to first ANC contact, various studies showed that maternal age, educational status, wealth index, residence (rural or urban), husband’s education, pregnancy intention, women’s autonomy, distance to a health facility, pregnancy complication, knowledge about timely booking, having decision-making power to use ANC were statistically associated with the timely commencement of antenatal care [4, 6, 11]. The studies showed that being a resident of a rural and nomadic community negatively affects ANC uptake compared to urban residents [13, 14]. In addition, clannism and political conflicts causing a lack of peace and political unrest result in less uptake of ANC in Somalia. For health services providers, security issues in the Sanaag and Sool regions become an obstacle to serving the community [15]. Moreover, previous studies examined factors associated with time to first ANC contact among pregnant women using semi-parametric and parametric survival models. However, these studies were conducted on a small scale in different parts of Somalia, which limits their ability to capture the full extent of ANC utilizations of the first ANC contact. These studies also failed to address the variation across different regions or places of residence within the country [16-18]. Therefore, the need to introduce a frailty term to quantify the difference across the location of residence of pregnant women in Somalia is what motivates the current study. The assumption of heterogeneity between individuals is important when survival data come from different groups or when individuals have repeated measurements. Introducing a frailty term allows us to account for associations and unobserved heterogeneity in the study. However, the omission of such frailty terms in the survival data may lead to estimation and prediction problems, introducing biased estimated coefficients and making the regression parameter estimates approach zero [19]. For clustered data, presenting a frailty term provides a more robust estimation compared to standard accelerated failure time (AFT) models [20].
To address all these limitations, this study aims to identify the factors that influence the time to the first ANC contact among Somali pregnant women by employing AFT univariate and shared frailty models and considering various baseline distributions.
2. METHODS AND STUDY DESIGN
2.1. Study Design
2.1.1. Study Design
This study used data from the Somalia Health and Demographic Survey (SHDS). The survey was primarily collected in 2020 to provide information on key demographic and health indicators, making the first health and demography survey in the country’s history. The dataset contains 47 sampling strata, with a final frame consisting of 9136 enumeration areas (7,308 in urban and 1,828 in rural) [21]. In this survey, Lower Shabelle and Middle Juba regions and some parts of the Bay region were excluded from the study due to security reasons. A total of 16,486 women were interviewed with a response rate of 95% [21]. For this study, 3138 women who met the inclusion and exclusion criteria from 11 regions were included in the survey (Fig. 1).
2.1.2. Response Variables
The outcome variable for this study is time to the first ANC contact, measured in months, among pregnant women. The survival time was defined as the duration of pregnancy (in months) measured from the time of conception to the first ANC contact (event). A woman who attended an ANC contact within 12 weeks was considered as an event, and others are considered as censored.
2.1.3. Risk Factors
Different risk factors were considered in this study to determine their effect on time to the first ANC contacts. These are the occupation of the mother, age, number of children, region, media exposure, educational level, place of residence, wealth index, who decided on health care services utilization, marital status, and wanted pregnancy. Furthermore, we looked at residence as a clustering effect in the frailty models in order to quantify the unobserved effect.
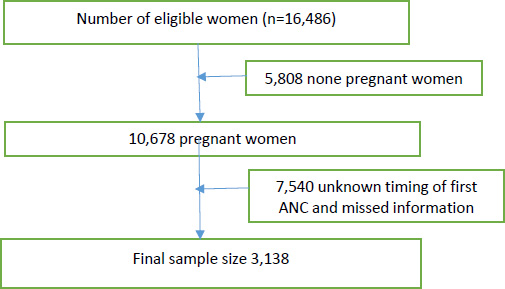
Sample size and sampling procedure to reach the final sample size in 2020 SDHS.
2.2. Statistical Analysis
The data used for this study were secondary data obtained from the Somalia Health and Demographic Survey (SHDS) surveyed in 2020. After data management and cleaning, the time to the first ANC contact was estimated using the Kaplan-Meier method, and the log-rank test was applied to compare survival time differences between groups of categorical variables with the outcome of interest. The most frequently applied models in any survival data are the Cox PH model, AFT model, and parametric shared frailty models. This study tried to see the performance of each model and compared using AIC and BIC to select the best model that fits the data well [22, 23]. The final model was chosen using AIC and BIC criteria, and the model validity was checked using a residual plot.
2.2.1. Accelerated Failure Time Model with Frailty Approach
In AFT models, it is assumed that the effect of the covariates is a multiplication of the expected survival time. A general formulation of the AFT hazard model with p covariates is:
 |
(1) |
where η = a'X = a1x1 + a2x2 + ... + apxp is the linear component of the model and e(a1x1+a2x2+...+apxp) is the acceleration factor, where a1, a2,..., ap are the unknown regression coefficients of the explanatory variables x1, x2, ... , xp [24]. In this study, both univariate and multivariate (shared frailty) models were employed to select the best model which describes the data well. Analyzing clustered survival times requires special treatment because most models assume that observations are independent, and grouped data clearly violate this assumption. In univariate frailty survival models, it can be used to assess the heterogeneity among individuals, and the influence of unobserved risk factors in a proportional hazards model. Whereas in multivariate frailty survival models, the shared frailty model is used to assess the dependence between the individuals within the group [25-28].
Suppose logTij be the logarithm of the survival time of the jth pregnant woman in the ith residence, (j = 1,2,...,ni and i = 1,2,...,r) and Xij be the vector of covariates associated with this individual. Then, the shared AFT frailty model is given by:
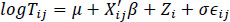 |
(2) |
where β is the vector of unknown coefficients, μ is the intercept parameter, σ is the scale parameter, ϵij are i.i.d random errors, and the Zi are the cluster-specific random effects, which are assumed to be i.i.d random variables with a density function f(Zi).
The selection of the frailty model distribution is one of the challenges in applying frailty models, and various studies have explored in selection of this frailty distribution. While some authors have used different distributions, such as gamma [27, 28], inverse Gaussian [29, 30], log-normal [31], and positive stable [32], the gamma and inverse Gaussian distributions are the most common and widely used in literature for modeling the frailty effect, which acts multiplicatively on the baseline hazard [29, 33]. In this study, we assumed that the shared frailty (random effect) Zi follows gamma or inverse Gaussian distribution. In a density function f(Zi), θ indicates the term frailty; where θ>0, indicates the presence of heterogeneity. So, the large values of θ reflect a greater degree of heterogeneity among place of residence of pregnant women and a stronger association within place of residence. In these models, frailty could be considered as an unobserved covariate that is additive on the log failure time scale and describes some reduced or increased event times for different clusters.
3. RESULTS
3.1. Descriptive Statistics
A total sample of 3138 women who became pregnant during the five years preceding the survey were included in this study from eleven regions of Somalia. The median time to first ANC contact was 6.2 months. Of the total pregnant women, about 1039 (33.1%) received their first ANC contact within the WHO recommended time, and 2099 (66.9%) did not receive their first ANC contact and were therefore considered as right censored. The highest number of participants in this study was from Woqooyi Galbeed, 634 (20.2%), whereas the lowest number was from Juba, with 146 (4.6%). The majority of respondents, consisting of 2385 women (76%) did not have any formal education, and only 305 (9.7%) pregnant women attended their secondary school or higher. With respect to women’s place of residence, 1915 (61.1%) were from rural areas. From those, only 572(18.2%) attended timely their ANC contacts, and the remaining 1223 (38.9%) were urban residents. The frequencies with corresponding percentages for all characteristics are depicted below (Table 1).
| Variables Categories | First ANC Contact | ||||
|---|---|---|---|---|---|
| Yes | No | ||||
| - | N (%) | - | N (%) | ||
| Age in 10-year groups | 15 – 24 | 462 | (14.7%) | 882 | (28.1%) |
| 25- 34 | 295 | (9.4%) | 665 | (21.2%) | |
| 35 – 49 | 282 | (9.0%) | 552 | (17.6%) | |
| Residence | Urban | 467 | (14.9%) | 756 | (24.1%) |
| Rural | 572 | (18.2%) | 1343 | (42.8%) | |
| Educational status | No education | 777 | (24.8%) | 1608 | (51.2%) |
| Primary | 157 | (5.0%) | 291 | (9.3%) | |
| Secondary and above | 105 | (3.3%) | 200 | (6.4%) | |
| Wealth index | Poor | 345 | (11.0%) | 781 | (24.9%) |
| Middle | 180 | (5.7%) | 389 | (12.4%) | |
| Rich | 514 | (16.4%) | 929 | (29.6%) | |
| Current marital status | Widowed | 302 | (9.6%) | 561 | (17.9%) |
| Married | 660 | (21.0%) | 1334 | (42.5%) | |
| Others | 77 | (2.5%) | 204 | (6.5%) | |
| Respondent currently working | No | 354 | (11.3%) | 685 | (21.8%) |
| Yes | 685 | (21.8%) | 1414 | (45.1%) | |
| Number of children | less than or equal 4 | 553 | (17.6%) | 1312 | (41.8%) |
| greater than or equal 5 | 486 | (15.5%) | 787 | (25.1%) | |
| Wanted pregnancy | Then | 642 | (20.5%) | 962 | (30.7%) |
| Later | 163 | (5.2%) | 842 | (26.8%) | |
| No More | 234 | (7.5%) | 295 | (9.4%) | |
| Person who decides | Respondent | 315 | (10.0%) | 449 | (14.3%) |
| Husband | 86 | (2.7%) | 668 | (21.3%) | |
| Respondent and Husband Jointly | 476 | (15.2%) | 563 | (17.9%) | |
| Others | 162 | (5.2%) | 419 | (13.4%) | |
| Region | Awdal | 108 | (3.4%) | 192 | (6.1%) |
| Woqooyi Galbeed | 205 | (6.5%) | 429 | (13.7%) | |
| Togdheer | 85 | (2.7%) | 154 | (4.9%) | |
| Sool | 89 | (2.8%) | 211 | (6.7%) | |
| Sanaag | 128 | (4.1%) | 312 | (9.9%) | |
| Bari | 109 | (3.5%) | 228 | (7.3%) | |
| Nugaal | 60 | (1.9%) | 111 | (3.5%) | |
| Mudug | 83 | (2.6%) | 152 | (4.8%) | |
| Galgaduud | 69 | (2.2%) | 112 | (3.6%) | |
| Hiraan | 51 | (1.6%) | 104 | (3.3%) | |
| Juba | 52 | (1.7%) | 94 | (3.0%) | |
| Media exposure | Yes | 182 | (5.8%) | 354 | (11.3%) |
| No | 857 | (27.3%) | 1745 | (55.6%) | |
A test was conducted using the log rank to compare the survival distributions between groups for each categorical variable. The log-rank test showed that there is no statistically significant difference in the ‘survival' experience across different categories for the following factors: mother's education level, occupation, and media exposure. Similarly, the log-rank tests for other covariates revealed a statistically significant difference in survival experience among age groups, place of residence, wealth index, parity, marital status, region, decisions on the mother's health care, and whether the pregnancy was wanted.
The assumption of proportionality of the Cox PH model is also tested using rho (ρ) statistic with its associated p-value and scaled Schoenfeld residuals. A high rho (ρ) value indicates a strong correlation between the residuals and time, suggesting a systematic pattern in the graph, which reveals that the PH assumption is violated, and our test results confirmed the violation of the proportional assumption.
3.2. Accelerated Failure Time Model with Frailty Approach
Since the PH assumption was violated, the AFT model was used as an alternative model for analyzing the data with Exponential, Weibull, lognormal, and log-logistic as baseline distributions, with and without different frailty distributions by considering univariate and shared frailty approaches. The best model was selected based on the lowest AIC and BIC values. The model with a log-logistic baseline distribution and univariate gamma frailty showed the smallest AIC and BIC (5083.856 and 5259.345), as presented in Table 2. Therefore, the log-logistic AFT model with gamma shared frailty was found to be the best model for the given dataset.
3.3. Log-logistic AFT Model with Univariate Gamma Frailty
The results of the log-logistic AFT model with univariate Gamma frailty are presented in Table 3. The frailty term θ=1.63 indicates the existence of heterogeneity between individuals of pregnant women in Somalia. A likelihood ratio test for the hypothesis θ= 0 yielded a chi-square value of 153.95 with one degree of freedom, resulting in a highly significant p-value. The analysis based on the log-logistic AFT model with gamma frailty shows that marital status, mother's occupation, wanted pregnancy, region, parity, education level of the mother, wealth index, persons deciding on mother health care, and media exposure are significant predictors of time to the first ANC contacts. However, according to this model, the age group did not have a considerable effect on the time to the first ANC contact during gestational age (Table 3).
| Models | No-frailty | Gamma Frailty | Inverse-Gaussian Frailty | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AIC | BIC | Individual | Shared | Individual | Shared | |||||
| AIC | BIC | AIC | BIC | AIC | BIC | AIC | BIC | |||
| Cox PH | 22330.37 | 22487.71 | - | - | - | - | - | - | - | - |
| Weibull | 5398.62 | 5568.06 | 5153.896 | 5329.39 | 5366.655 | 5542.14 | 5297.23 | 5472.72 | 5398.62 | 5568.06 |
| Log-normal | 5242.59 | 5412.02 | 5181.103 | 5356.60 | 5198.11 | 5373.59 | 5206.60 | 5382.09 | 5242.59 | 5412.02 |
| Exponential | 5875.77 | 6039.16 | 5877.769 | 6047.21 | 5853.36 | 6022.80 | 5875.77 | 6039.16 | 5875.77 | 6039.16 |
| Log-logistic | 5235.82 | 5405.26 | 5083.856 | 5259.35 | 5116.85 | 5292.33 | 5117.72 | 5293.20 | 5235.82 | 5405.26 |
| Covariate | Categories | Φ | SE | 95% CI for ϕ | p-value |
|---|---|---|---|---|---|
| Marital status | Widowed | Ref | - | - | - |
| Married | 0.48 | 0.06 | (0.38, 0.61) | 0.00* | |
| Others | 0.54 | 0.07 | (0.42, 0.70) | 0.00* | |
| Mother occupation | No Yes |
Ref 0.80 |
0.05 | (0.70, 0.90) | 0.01* |
| Mother education | No education | Ref | - | - | - |
| Primary | 0.91 | 0.04 | (0.84, 0.91) | 0.03* | |
| Secondary and above | 0.88 | 0.05 | (0.78, 0.99) | 0.04* | |
| Wealth index | Poor | Ref | - | - | - |
| Middle | 0.87 | 0.04 | (0.79, 0.95) | 0.00* | |
| Rich | 0.93 | 0.04 | (0.86, 0.99) | 0.04* | |
| Wanted pregnancy | Then | Ref | - | - | - |
| Later | 1.52 | 0.06 | (1.40, 1.66) | 0.00* | |
| No more | 0.89 | 0.04 | (0.82, 0.97) | 0.00* | |
| Region | Awdal | Ref | - | - | - |
| Woqooyi Galbeed | 1.11 | 0.06 | (0.99, 1.23) | 0.054 | |
| Togdheer | 1.09 | 0.07 | (0.96, 1.23) | 0.18 | |
| Sool | 1.13 | 0.07 | (1.00, 1.23) | 0.051 | |
| Sanaag | 1.13 | 0.06 | (1.08, 1.26) | 0.03* | |
| Bari | 1.01 | 0.06 | (0.89, 1.14) | 0.84 | |
| Nugaal | 0.99 | 0.07 | (0.86, 1.14) | 0.88 | |
| Mudug | 1.07 | 0.07 | (0.94, 1,21) | 0.31 | |
| Galgaduud | 1.02 | 0.07 | (0.89, 1.17) | 0.74 | |
| Hiraan | 1.13 | 0.08 | (0.98, 1.13) | 0.08 | |
| Juba | 1.03 | 0.09 | (0.89, 1.19) | 0.67 | |
| Parity | 3 and below | Ref | - | - | - |
| 4 and above | 0.84 | 0.03 | (0.78, 0.91) | 0.00* | |
| The person decided on the respondent’s healthcare | Respondent alone | Ref | - | - | - |
| Husband | 4.10 | 0.41 | (3.26, 5.01) | 0.00* | |
| Respondent and husband jointly | 1.97 | 0.21 | (1.61, 2.41) | 0.00* | |
| Others | 2.32 | 0.21 | (1.91, 2.80) | 0.00* | |
| Age | 15-24 | Ref | - | - | - |
| 25-34 | 1.01 | 0.04 | (0.93, 1.09) | 0.79 | |
| 35-49 | 0.97 | 0.04 | (0.89, 1.06) | 0.56 | |
| Media exposure | No | Ref | - | - | - |
| Yes | 0.91 | 0.04 | (0.82, 0.99) | 0.00* |
From Table 3, the acceleration factor and 95% (CI) of marital status for married women and others were 0.48 (0.38, 0.61) and 0.54 (0.42, 0.70), respectively, compared to widowed women (reference category). The acceleration factor and its 95% CI for pregnant women who are employed were (0.8; 95% CI: 0.70, 0.90). This shows that pregnant women who are employed have an earlier time of initiation to start their first ANC contact than mothers who do not have work. Pregnant women with secondary or higher education had a 12% shorter time to start their first ANC contact than those with no formal education (0.88; 95% CI: 0.78, 0.99). This indicates that women with secondary or higher education are more likely to initiate their first ANC contact within the first 12 weeks of pregnancy compared to uneducated women. Timely initiation of ANC contact for pregnant women who wanted no more pregnancy was 11% (Φ =0.89; 95% CI: 0.82, 0.97) shorter (early initiation) as compared to women who wanted their last pregnancy. However, the acceleration factor of women who tried to delay their pregnancy had a 52% (Φ =1.52; 95% CI: 1.40, 1.66) longer expected time to start their first ANC contact compared to the references category. Timely initiation of ANC contacts in Sanaag was 13% (Φ =1.13; 95% CI: 1.08) longer as compared to the Awdal region. This implies an increase in the log of survival time, indicating a longer expected duration before the first ANC contact in this region. Timely initiation of ANC contact for pregnant women with four or more children was 16% (Φ =0.84; 95% CI: 0.78, 0.91) shorter compared to those women with three or fewer children. The acceleration factor and 95% CI for decisions on mother's health care categories involving husband, respondent, and husband jointly and others were 4.10 (Φ =4.10; 95% CI: 3.26, 5.01), 1.97 (Φ =1.97; 95% CI: 1.61, 2.41) and 2.32 (Φ =2.32; 95% CI: 1.91, 2.80), respectively, using respondent alone as the reference category. This indicates that these categories had a longer time to the first ANC contact compared to the reference category (respondents alone). The acceleration factor and 95% CI for the wealth index for a group of middle and rich household families were 0.87 (0.79, 0.95) and 0.93 (0.86, 0.99), respectively, using the poor as a reference category, which indicates middle and rich groups started ANC earlier than the reference group at a 5% level of significance. The acceleration factor and 95% confidence interval for pregnant women with media access had a 9% (Φ =0.91; 95% CI: 0.82, 0.99) shorter time to start their first ANC contact compared to those without media access.
4. DISCUSSIONS
This study aimed to identify the factors associated with the time to the first ANC contact using the AFT model with frailty distributions. We considered different baseline distributions with different possible frailty distributions to investigate the model that best fits the data for predicting the time to the first ANC contact in Somalia. The models were compared using AIC and BIC criteria [34]. In our study, the log-logistic AFT model with univariate gamma frailty was identified as the best fit for the dataset. The result showed that the marital status of pregnant women, the mother's occupation, wanted pregnancy, wealth index, region, parity, education level of the mother, persons deciding on mother health care, and media exposure are significant predictors of the time to the first ANC contact. The findings are consistent with the studies done in [2-4]. The study also found that there was heterogeneity among individual levels of pregnant women regarding the timing of time of their first ANC contact. According to WHO guidelines, ANC should start in the first trimester of pregnancy [35]. This study revealed that the median time for pregnant women to initiate their first ANC contact was 6.2 months. This finding is in line with a study conducted in Ethiopia [1].
Based on our study, the marital status of pregnant women was a significant predictor for the time to the first ANC contact. In this study, the acceleration factor indicates that married women are more likely to initiate their first ANC contacts earlier than single women. Similar findings have been reported in other studies [36, 37]. A possible justification may be fear of public stigmatization. Primigravidas who are unmarried tend not to utilize ANC services. Additionally, those without partners might face certain financial challenges that limit their chances of attending regular ANC services. This study also found that women with media exposure were more likely to start ANC contact on time, which aligns with the studies conducted in [38-40]. One possible explanation for this could be that women who are exposed to media are more aware of the availability of maternal healthcare services and the advantages of using them when needed.
The results also showed that parity was associated with both the likelihood of receiving ANC and the timing of the first ANC contact. Women with four or more children had early initiation to start their first ANC contact than mothers with three or fewer children [41, 42]. Regarding mothers' occupation, pregnant women who have occupation had a shorter time to start their first ANC contact than their counterparts (who have no occupation). These findings are supported by similar studies [43, 44]. A possible reason may be occupation have a strong relationship with antenatal care services since transportation, consultations, and purchases of recommended drugs or medications cannot be disassociated from its usage.
The pregnant women who desired fever children had a longer time before starting their first ANC contact compared to those who desired more children, which aligned with the study [36]. This could be because women who desire more children are more driven to make sure they are safe during pregnancy, delivery, and after delivery. The motivation to have a healthy child may explain why the women who desire another child are more likely to attend their first ANC contact early. Another important variable in our study was the level of education; educated women were associated with early ANC contacts with trained health professionals. This result was consistent with the research' findings and conclusions [2-46]. Educated mothers know to start their ANC at the early age of the pregnancy.
Decision-making authority on mothers’ health care was another variable found to be associated with the time to the first ANC contact. When women were the sole decision-makers, pregnant women had a shorter time to start the first ANC utilization compared with joint decision-making with the husband or the husband alone as well as other people. Previous studies highlighted our findings [47, 48]. This may be because the mothers have the power to decide only themselves, and there is no influence of other bodies. The study also showed pregnant women who lived in Woqooyi Galbeed, Sool, and Sanaag had a longer time to start their first ANC contact compared to those in the Awdal region.
The study also revealed that women from households in the middle and high-income categories initiated their first ANC contact earlier than women from poor households and this is similar to reports by [46, 49]. A possible reason might be financial barriers, such as high out-of-pocket costs for consultations, which may significantly impact the low utilization of maternal health services such as ANC, especially in areas where resources are scarce and services are more expensive [50, 51].
CONCLUSION
In this study, the median time for the first ANC contact was 6.2 months, which is a significantly delayed time compared to the WHO's recommendation for ANC contacts.
To identify the risk factors for the time to the first ANC contact, various parametric shared frailty and AFT models were applied using different baseline distributions. Based on the AIC and BIC, the log-logistic gamma frailty model provided a better fit to the time-to-first ANC contact compared to other parametric shared frailty and AFT models. There is a frailty (clustering) effect on the time to the first ANC contact, which arose from differences in the timing of the first ANC receipt among various places of residence in Somalia. The major factors identified in this study were marital status, mother's occupation, wanted pregnancy, region, parity, mother's education level, decision-maker for the mother's healthcare utilization, and media exposure, all of which were statistically significant.
Policies and programs aiming at addressing residence differences in time to first ANC must be developed and implemented vigorously. Special focus must be paid to political unrest regions like Sanaag and Sool regions. More specific policy initiatives, such as targeted educational campaigns, enhanced pregnancy care, and attempts to decrease regional inequities, should be prioritized as immediate intervention strategies.
AUTHORS’ CONTRIBUTION
D.B.B., K.D. and M.I.A.: Involved in framing the problem, performing the data extraction, analyzing, editing, revising, and reviewing the entire manuscript; D.C. and N.N.R.: Involved in critically reviewing the manuscript. All authors have read and approved the final manuscript.
LIST OF ABBREVIATIONS
| ANC | = Antenatal Care |
| AFT | = Accelerated Failure Time |
| AIC | = Akanke’s Information Criterion |
| BIC | = Bayesian Information Criterion |
| SDHS | = Somalia Demographic and Health Survey |
| PH | = Proportional Hazard |
| WHO | = World Health Organization |
AVAILABILITY OF DATA AND MATERIALS
The data used in this study were Somalia Health and Demographic Survey 2020 data (SHDS 2020) and can be obtained or accessed from the Somalia National Bureau of Statistics (SNBS) at https://microdata.nbs.gov.so/index.php/catalog/50. This dataset is publicly available and can be accessed for research purposes. The data were accessed on May 1, 2024.
FUNDING
This work is partially based upon research supported by the South Africa National Research Foundation (NRF) and South Africa Medical Research Council (SAMRC) (South Africa DSTNRF-SAMRC SARCHI Research Chair in Biostatistics, Grant number 114613). The authors also would like to thank the South Africa National Research Foundation (NRF) and South Africa Medical Research Council (SAMRC) (South Africa DSTNRF-SAMRC SARCHI Research Chair in Biostatistics, Grant number 114613) for partially supporting this work. Opinions expressed and conclusions arrived at are those of the author and are not necessarily to be attributed to the NRF and SAMRC.
ACKNOWLEDGEMENTS
The authors would like to thank the Somalia National Bureau of Statistics for providing all the relevant secondary data used in this study.


