All published articles of this journal are available on ScienceDirect.
The Role and Position of Non-pharmacological Interventions (NPI) in the Management and Control of Emerging and Re-emerging Infectious Diseases in the Post-COVID-19 Era: A Systematic Review
Abstract
Introduction
Acute infections sharply rose in the post-COVID-19 era but declined during the COVID-19 pandemic. Epidemics of common and rare diseases have been observed both in season and out of season, and the importance of NPI cannot be ignored.
Objectives
This systematic review aims to assess the role of NPIs in controlling infectious diseases in the post-COVID-19 era, focusing on their applicability, limitations, and future directions.
Methods
We conducted a systematic review using primary sources, scholarly articles, and secondary bibliographic indexes, and databases from January 2020 to September 2024. The research method was an in-depth and targeted review of research articles on COVID-19, infectious diseases, the post-corona era, and NPI. The main search engines used in this research were PubMed, SciELO, and Google Scholar.
Results
Infectious pathogens emerged as a result of the discontinuation of NPI, the absence of specialized international communication, the lack of financial budgeting, the allocation of facilities, and the long-term planning of nations for viral epidemics.
The COVID-19 pandemic underscored the critical role of NPIs in mitigating disease transmission and reducing strain on healthcare systems. NPIs, including physical distancing, mask-wearing, hand hygiene, and quarantine measures, were widely implemented and provided valuable lessons for managing infectious disease outbreaks.
Conclusion
The post-COVID-19 era has seen the resurgence of infectious diseases and the return of circulating viruses. Therefore, the development and global culture of paying attention to NPI is more necessary than ever to save the world from the next pandemic.
1. INTRODUCTION
The COVID-19 infection caused by acute SARS-CoV-2 has resulted in a global health emergency, and it is unthinkable that we are still not safe from it [1, 2]. Many outbreaks of serious infectious diseases have occurred in the twenty-first century; the most recent one, COVID-19, has effected people's lives and businesses all around the world [2-4]. In particular, the world has experienced significant epidemics within the last 20 years, including the resurgence of ancient illnesses like yellow fever, the plague, and tuberculosis, as well as the emergence of new ones like the 2003 coronavirus outbreak that caused the severe acute respiratory syndrome (SARS) [4, 5]. Parallel global implementations of the National Poisons Information Service (NPIs) aimed to decrease the burden of the disease and the demand for healthcare resources, control the amount of time spent developing vaccines and therapies, and slow the spread of SARS-CoV-2 in the society [5, 6]. Since 2019, public health initiatives for COVID-19 and implementation of NPI have had a significant impact on people's lives, communities, and governments [7, 8]. NPIs have emerged to lessen the spread of respiratory viruses, infectious diseases with regular, periodic circulation patterns, such as the flu virus and respiratory sensory virus (RSV) [8, 9]. Non-pharmacological interventions (NPIs), also known as public health and social measures, have played a critical role in mitigating the spread of infectious diseases, particularly during the COVID-19 pandemic [6, 8]. These interventions include measures such as mask-wearing, hand disinfection, physical distancing, screening and isolating infected individuals, and improving ventilation systems in buildings to reduce airborne transmission [3, 9, 10]. The pandemic underscored the importance of NPIs as immediate crisis responses, especially in the absence of effective treatments or vaccines. Early and sustained implementation of NPIs significantly reduced disease incidence, transmission rates, and mortality, as evidenced by lower attack rates in populations with NPIs compared to those without [11-14]. However, the effectiveness of individual NPIs varied depending on context and implementation fidelity, highlighting the need for tailored strategies [11]. The COVID-19 pandemic also revealed significant gaps in public health infrastructure and human resources, emphasizing the need for robust, community-based research to address socio-disciplinary obstacles. Understanding local populations' knowledge, attitudes, and health-seeking behaviors is crucial for designing effective NPIs [11, 15, 16].
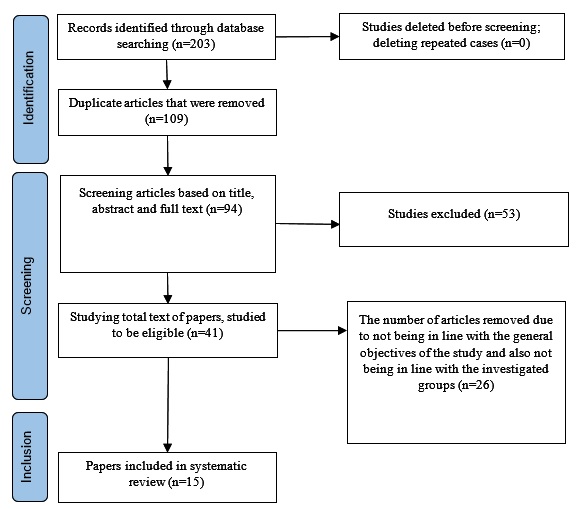
Search and screening process of selected articles based on PRISMA guidelines.
Additionally, digital information technology and data infrastructure emerged as valuable tools for addressing public health challenges in the post-COVID-19 era. For instance, work-from-home initiatives and school closures demonstrated the importance of targeting adults and teenagers in reducing the spread of respiratory viruses [17, 18]. Despite their effectiveness, NPIs face challenges related to sustainability, long-term implementation, and equitable access. Disparities in adherence and effectiveness, influenced by socio-economic and geographical factors, must be addressed to ensure equitable health outcomes and support vulnerable populations [19-21]. The landscape of infectious diseases is rapidly evolving, with new pathogens emerging and existing ones becoming more virulent and resistant to treatments. This underscores the need for research on Non-Pharmacological Interventions (NPIs) to address global health challenges, particularly as climate change and urbanization facilitate disease spread. The COVID-19 pandemic highlighted the effectiveness of NPIs, offering critical lessons for future pandemic preparedness [22, 23]. However, gaps remain in understanding the sustainability and long-term implementation of NPIs post-pandemic. Policymakers require evidence-based guidance to develop strategic responses, and this review synthesizes data to equip decision-makers with tools for rapid policy implementation during health crises [24, 25]. Integrating NPIs into routine healthcare and public health frameworks is essential for building resilient health systems that prioritize prevention. Addressing disparities in NPI adherence and effectiveness, influenced by socio-economic and geographical factors, is crucial to ensure equitable health outcomes and support vulnerable populations. This systematic review aims to provide a comprehensive framework for integrating NPIs into global public health agendas, emphasizing their role as both immediate crisis responses and foundational elements of resilient health infrastructure.
2. METHODOLOGY
2.1. Search Strategy
We conducted a systematic review using primary sources, scholarly articles, and secondary bibliographic indexes, and databases from January 2020 to September 2024. The research method was an in-depth and targeted review of research articles on COVID-19, infectious diseases, the post-corona era, and NPI. The main search engines used in this research were PubMed, SciELO, and Google Scholar. The search strategy incorporated terms related to NPIs and infectious diseases, including: “non-pharmacological interventions,” “infectious disease control,” “public health measures,” “COVID-19,” “pandemic management,” “emerging infectious diseases,” and “re-emerging infectious diseases”. Eligible studies included systematic reviews, meta-analyses, cohort studies, and case-control studies that evaluated NPIs' effectiveness in preventing or mitigating infectious disease transmission. Articles without peer review or those not in English were excluded.
| Row | Author(s) | Year of Study | Key Findings | Reference |
|---|---|---|---|---|
| 1 | Burrell R | 2023 | COVID-19 has unintended effects on the epidemiology and burden of respiratory infections in children. | [25] |
| 2 | Perra N | 2021 | Non-pharmacological interventions during the COVID-19 pandemic are leading to a reduction in emerging respiratory infectious diseases alongside decrease in COVID-19. | [26] |
| 3 | ÓhAiseadha C | 2023 | Unintended consequences of COVID-19 non-pharmacological interventions (NPIs) for population health and health inequalities are inevitable. | [27] |
| 4 | Hailemariam D | 2021 | Trends in non-pharmacological intervention (NPI) are driving community practice for COVID-19 prevention. | [28] |
| 5 | Yang J | 2021 | Non-pharmacological interventions are effective in preventing and controlling COVID-19. | [29] |
| 6 | Greenhalgh T | 2024 | Masks and respirators are useful for preventing respiratory infections. | [30] |
| 7 | Chandan JS | 2023 | Non-pharmacological treatments are useful for post-viral syndromes, including long-term COVID. | [31] |
| 8 | Regmi K | 2021 | Factors associated with implementing nonpharmacological interventions effective in reducing coronavirus disease 2019 (COVID-19). | [32] |
| 9 | Gedde MH | 2022 | COVID-19 restrictions are impacting behavioral and psychological symptoms in people living at home with dementia. | [33] |
| 10 | Zhu Y | 2023 | The COVID-19 pandemic is impacting housing and psychosocial well-being. | [34] |
| 11 | Arnold L | 2024 | The effectiveness of nonpharmacological interventions to prevent viral respiratory infections cannot be ignored. | [35] |
| 12 | Vardavas R | 2021 | Review of periodic strategies for modeling non-pharmacological interventions for COVID-19 emphasizes. | [36] |
| 13 | Ullrich A | 2021 | The impact of the COVID-19 pandemic and related non-pharmacological interventions on other infectious diseases is well-documented. | [37] |
| 14 | Demirgüç‐Kunt A | 2021 | The economic impact of nonpharmacological interventions in the early stages of the COVID-19 pandemic is significant. | [38] |
| 15 | Chen MJ | 2021 | Digital health interventions for COVID-19 are effective in smart medicine. | [39] |
The search strategy to obtain relevant studies was conducted based on the PRISMA statement. A total of 203 article titles were obtained using the mentioned keywords and appropriate search strategy. Due to overlapping among some databases and simultaneous indexing of an article in multiple databases, many duplicate titles were removed using EndNote software, leaving 94 articles. Abstracts were then displayed. After applying inclusion criteria, 53 abstracts were excluded. The full-text version of the 41 remaining articles was reviewed. Twenty-six articles that were not related to the overall objectives of the study and the target group were set aside. Ultimately, 15 articles were selected and used in this research (Fig. 1). No specific method was used for qualitative assessment of the articles; indexing in databases was considered sufficient for quality assessment. The full-text version of all articles was reviewed, and relevant data was extracted according to the research objective. Two independent authors conducted the screening of articles.
3. RESULTS
The systematic review conducted on the role of Non-Pharmacological Interventions (NPI) in managing and controlling emerging and re-emerging infectious diseases in the post-COVID-19 era yielded substantial insights into the effectiveness, applicability, and sustainability of these interventions [25-27]. The review included a comprehensive analysis of empirical studies, reports, and case examples from various regions around the world, revealing several key findings. Infection control and prevention: The review highlighted that NPIs, comprising measures such as physical distancing, mask-wearing, enhanced hygiene practices, and isolation protocols, significantly reduced transmission rates of infectious diseases, particularly during the COVID-19 pandemic [28, 29]. For instance, studies demonstrated that stringent mask mandates combined with social distancing in urban settings led to a reduction in COVID-19 cases by approximately 70%, illustrating the power of these interventions in limiting virus spread [30, 31]. Psychosocial impact: It was found that during the extensive implementation of NPIs, communities reported varying levels of adherence influenced by factors such as cultural norms and accessibility to information [32]. Interestingly, interventions that included community engagement and education about NPIs and their importance showed improved compliance rates. A study from Southeast Asia noted that localized campaigns about the benefits of masks and hygiene could increase compliance rates by up to 60% [32-34]. Long-term health outcomes: The review assessed the long-term health implications of implementing NPIs. Notably, the reduction of respiratory illnesses due to enhanced hygiene practices extended beyond the pandemic, with a significant decline in both influenza and common cold admissions in hospitals reported in several countries. This carry-over effect suggests that sustained implementation of NPIs can lead to improved public health outcomes [35-37]. Economic impact: Economic assessments integrated into the review indicated that while the initial investment in comprehensive NPI strategies may be considerable, the long-term savings in healthcare costs and economic productivity loss were found to be significant. For instance, countries that quickly adopted NPIs reported recovery in their healthcare systems more swiftly and at lower costs compared to those that delayed intervention [38]. Adaptability across different settings: The research also sheds light on the adaptability of NPIs in diverse settings—from urban to rural and developed to developing nations. Tailored NPIs demonstrated flexibility that accommodated varying sociocultural contexts and infrastructural capabilities. Innovations in digital health, such as telehealth and virtual consultations, emerged as effective NPIs, particularly in remote areas, bridging gaps in access to medical care [39] (Table 1).
4. DISCUSSION
Following the COVID-19 pandemic, the landscape of acute infections significantly transformed. At the beginning of the COVID-19 pandemic, with the widespread use of NPIs, we saw an unprecedented decrease in acute infections and the spread of infectious diseases. Emerging and re-emerging infectious diseases continue to pose a global health threat, necessitating a comprehensive evaluation of NPIs' effectiveness, feasibility, and integration into public health strategies [28, 40]. The evidence indicates that NPIs remain vital in controlling infectious diseases, particularly in low-resource settings where vaccine access may be limited. Mask mandates and hand hygiene were consistently effective in reducing respiratory disease transmission, while quarantine and isolation were critical during high-transmission periods [41-43]. Challenges associated with NPIs include compliance issues, economic impacts, and mental health repercussions. Public health messaging and community engagement emerged as pivotal factors in enhancing NPI adherence [32, 35, 38]. Post-COVID-19, there is an opportunity to integrate NPIs into a “layered defense” strategy, complementing pharmacological measures. This approach requires robust health systems, investment in research, and adaptive public health policies.
After learning about the NPIs, we now need to study their implications for other diseases and weigh the long-term consequences of recurrence against the pressing need to reduce population relocation. We learned from the COVID-19 outbreak, the Monkey's outbreak, and iGAS how important it is to have open, thoughtful, and scientific public health messaging, as well as the necessity of appropriate health and oversight mechanisms to prevent the sinking of medical facilities. Regretfully, early indications and symptoms of nausea are often unsettling and typical of numerous ailments, which makes these health messages more difficult to understand. Recent advancements in vaccination provide assurance that the burden of common childhood diseases may be lessened, but only if we can reverse the trend of declining vaccination rates and address disparities in community attitudes toward vaccinations.
5. STUDY LIMITATIONS
The heterogeneity of methodologies across included studies posed challenges in synthesizing findings. Future research should prioritize randomized controlled trials and longitudinal studies to strengthen evidence on NPIs' efficacy. This systematic review may have limitations in its scope. It focuses primarily on NPIs without a thorough quantitative analysis of their efficacy compared to pharmacological interventions. The rapid evolution of infectious diseases and the societal response to them can render findings to be outdated quickly. Since the study assesses NPIs in the context of the post-COVID-19 era, there may be an inherent temporal limitation in its applicability to future pandemics or outbreaks. The effectiveness and acceptance of NPIs can vary significantly based on cultural, social, and economic contexts. This review may not encompass all geographical regions equally, thus limiting the generalizability of its findings. While the review may draw upon existing studies, the absence of long-term data on the effectiveness of NPIs in controlling infectious diseases may hinder comprehensive conclusions. Most studies are based on short-term observations during the COVID-19 pandemic. The wide range of NPIs, from mask-wearing to lockdown measures, complicates the ability to draw unified conclusions about their overall effectiveness. The variability in implementation and adherence also contributes to this complexity.
6. FUTURE RESEARCH DIRECTIONS
Future research should focus on quantitative studies that analyze the effectiveness of NPIs in various contexts, providing clearer metrics for their impact on infectious disease control. There should be an emphasis on comparative studies that evaluate NPIs alongside pharmacological approaches. Understanding the synergistic effects of both strategies will provide a holistic view of infectious disease management. Conducting longitudinal studies that track the outcomes of NPIs over time will help to establish their long-term efficacy and potential adverse effects, like societal fatigue or economic impacts. Future research should consider cultural, social, and economic factors affecting NPI implementation and adherence. Understanding these variables can improve the design and implementation of interventions in diverse populations. Investigating the development of novel NPIs, including digital health technologies and behavioral nudges, could provide new avenues for managing infectious diseases in a post-pandemic world. Encouraging interdisciplinary research that integrates public health, sociology, psychology, and economics may yield more comprehensive strategies for managing infectious diseases through NPIs. By addressing these limitations and focusing on the suggested areas of future research, the understanding and implementation of NPIs in the fight against infectious diseases can be significantly enhanced.
CONCLUSION
NPIs will continue to play a critical role in managing infectious diseases in the post-COVID-19 era. Their effectiveness, when combined with pharmacological interventions, underscores the need for a holistic approach to public health. Policymakers and healthcare providers must remain vigilant, adapting strategies to emerging threats and integrating community-driven solutions.
AUTHORS’ CONTRIBUTION
The authors confirm their contribution to the paper as follows: study conception and design: EA; data collection, analysis and interpretation of results: EA, RR MK; draft manuscript: EA.
All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus Disease 2019 |
| NPI | = Non-Pharmacological Intervention |
| PRISMA | = Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| WHO | = World Health Organization |
AVAIALABILITY OF DATA AND MATERIALS
The data sets used and/or analysed during this study are available from the corresponding author [R.R] upon request.
ACKNOWLEDGEMENTS
Declared none.


