All published articles of this journal are available on ScienceDirect.
Harnessing E-Health for Adolescent Sexual Health in Sub-Saharan Africa: A Systematic Review and Roadmap for Implementation
Abstract
Background
Sub-Saharan Africa (SSA) is grappling with alarming adolescent sexual health problems, including high HIV/AIDS rates and unintended pregnancies. E-health solutions offer a promising solution. This study systematically reviewed e-health interventions for adolescent sexual health in SSA, analysed studies published between 2013 and 2024, and proposed a roadmap for effective implementation to improve adolescent sexual health outcomes.
Methods
Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework, this study searched PubMed, Scopus, Web of Science, and AJOL for e-health interventions targeting adolescent sexual health in SSA. Studies were analysed for relevance, quality, and gaps. Findings were interpreted through the bi-theoretical lenses of the Technology Acceptance Model (TAM) and Diffusion of Innovations Theory (DIT).
Results
Out of 139 eligible studies, 17 met the inclusion criteria for this review. The findings highlight the effectiveness of e-health interventions and e-health tools and the barriers to their implementation, including gaps in policy support and digital access, alongside cultural and social factors that shape adolescents' receptiveness to these technologies. The review further showed that e-health integration is promising for improving adolescent sexual health.
Conclusion
E-health solutions hold great promise to improve the sexual health of adolescents in SSA. However, successful implementation must address infrastructure gaps, offer educators and health workers training, and ensure cultural sensitivity. Policymakers should update policies to bridge the digital divide and protect data privacy. This study provides a roadmap with key recommendations for stakeholders to effectively promote adolescent sexual health through e-health.
1. INTRODUCTION
The sexual health challenges of adolescents in SSA are complex and deeply rooted in socioeconomic, cultural, and systemic factors. These challenges, if not addressed or mitigated, could collectively pose significant barriers to the Sexual and Reproductive Health (SRH) of young people.
1.1. Overview of Sexual Health Challenges among Adolescents in Sub-Saharan Africa
Adolescents in SSA face many sexual health challenges, prominently characterised by high rates of sexually transmitted infections, HIV, unintended pregnancies, and gender-based violence. The region accounts for a disproportionate share of global HIV infections among young people, with less than 20% of adolescents aware of their HIV status, despite SSA hosting nearly 90% of the world's HIV cases among this demographic [1]. Factors contributing to this alarming statistic include inadequate access to youth-friendly health services and sexual health literacy, negative attitudes from health workers, and societal taboos surrounding discussions of sexual health [2-4]. Both authors further noted that the lack of youth-friendly services hampers the use of HIV prevention strategies, leading to increased vulnerability among adolescents [3, 4].
Furthermore, the prevalence of unintended pregnancies among adolescents is a critical concern, with studies indicating that approximately 46% of all pregnancies in this age group are unintended [5]. This is exacerbated by limited access to contraceptive methods and SRH education, which are essential for informed decision-making [6, 7]. The intersection of poverty, inadequate health facilities, and cultural norms further complicates the situation, often resulting in young women engaging in intergenerational relationships that increase their risk of both HIV and unintended pregnancies [8]. The consequences of such pregnancies are severe, often leading to health complications, social stigma, and economic challenges for young mothers [5, 9]. Child marriage, prevalent in some parts of the SSA region, significantly influences sexual health outcomes by leading to early childbirth and increased health risks [6, 9]. This practice is also associated with high fertility rates and poor sexual and reproductive health outcomes, primarily due to the limited access many young girls have to essential health services. Additionally, the COVID-19 pandemic has further strained SRH services, as diverted resources exacerbated the challenges faced by adolescents in accessing necessary care [10].
1.2. Importance of Digital Technologies in Revolutionising Adolescent Sexual Health in SSA
The importance of e-health in improving adolescent sexual health is increasingly recognised as a vital component in addressing the myriad challenges faced by young people in SSA. E-health encompasses a range of digital health solutions, including telemedicine, mobile health applications, social media, and online educational resources, which can significantly improve access to sexual health information and services. This is particularly crucial in regions where traditional sexual healthcare systems may be inadequate or stigmatised, such as in many parts of SSA.
One of the primary benefits of e-health is its ability to provide adolescents with confidential and accessible information regarding sexual health [11]. Many young people are reluctant to seek information from traditional sources due to fear of judgment or stigma. Online platforms can serve as safe spaces for adolescents to explore sexual health topics without the anxiety associated with face-to-face interactions. For instance, a study indicates that adolescents often prefer using digital media for health information, as it allows them to engage with sensitive topics at their own pace and in a private setting [12]. This aligns with findings from an earlier study, which emphasise that e-health can complement parental involvement by providing adolescents with additional resources [13]. Moreover, e-health initiatives can facilitate better communication between adolescents and healthcare providers. By utilising telehealth services, young people can consult with healthcare professionals remotely, benefiting those living in rural or underserved areas. This mode of communication not only increases access to sexual health services but also allows for more tailored and personalised care. For example, another study highlights that e-health platforms can empower sexual health education professionals to reach a broader audience and address specific adolescent needs [14].
In addition to improving access and communication, e-health can enhance the quality of sexual health education provided to adolescents. Digital platforms can offer comprehensive and age-appropriate sexual health education that is often lacking in traditional school curricula. For instance, a study conducted in low- and middle-income countries underscores the necessity of effective SRH interventions for adolescents, which can be delivered through e-health channels to ensure that young people receive accurate and relevant information [15]. This is important in contexts where misinformation is prevalent, as it can lead to risky behaviours and negative health outcomes.
Furthermore, e-health can play a significant role in addressing mental health issues related to sexual health. Adolescents often experience psychosocial distress that can impact their sexual behaviour and overall well-being. Another study emphasises the need for comprehensive SRH education to prevent adolescent mental health problems, suggesting that e-health platforms can integrate mental health resources alongside sexual health information [16]. By providing holistic support, e-health can help adolescents navigate the complexities of their sexual health while also addressing underlying mental health concerns.
The integration of e-health into adolescent sexual health services also has the potential to foster community engagement and support. Online forums and social media platforms can create spaces for adolescents to share experiences, seek advice, and build peer support networks. This communal aspect can be particularly beneficial in combating the isolation that many young people feel regarding their sexual health concerns. Also, involving adolescents in developing sexual health education programs can lead to more effective outcomes, highlighting the importance of community input in shaping e-health initiatives [17]. Moreover, e-health can facilitate the dissemination of information regarding available sexual health services, including contraception and STI testing [11]. Many adolescents are unaware of the resources available to them, which can hinder their ability to make informed decisions about their sexual health. By leveraging digital platforms, health organisations can effectively promote these services and ensure adolescents know how to access them. This could be critical in regions with limited healthcare access,as highlighted by another study that discusses the barriers to accessing SRH services in Nigeria [18].
1.3. Gaps in Research
Several studies have investigated sexual health interventions targeting adolescents in SSA, such as the review of school-based sexual health interventions to prevent STI/HIV, exploration of the determinants of high-risk sexual behaviour, and sexual learning [19-22]. In addition, various studies showed variations in contraceptive prevalence in different countries and provided insights into the interplay between social factors and sexual debut among vulnerable populations [23, 24]. Despite the extensive research on sexual health interventions in SSA, there is a limited focus on e-health interventions and an actionable roadmap for its development specifically tailored for adolescent sexual health in the region. While studies have explored various interventions, there is a need for more targeted research on the effectiveness of e-health solutions in improving adolescent sexual health outcomes.
1.4. Research Objectives
- To systematically review the literature on e-health interventions for adolescent sexual health in Sub-Saharan Africa from 2013 to 2024.
- To analyse relevant published studies regarding sexual health and e-health in Sub-Saharan Africa within the same period,
- To identify supportive provisions and existing gaps.
- To develop a comprehensive roadmap for effectively implementing e-health solutions in adolescent sexual health in Sub-Saharan Africa.
1.5. Research Questions
- How effective are e-health interventions in improving adolescent sexual health outcomes in SSA?
- What challenges hinder the successful implementation of e-health solutions for sexual health education in Sub-Saharan Africa?
- What are the key provisions and gaps in existing policies related to e-health and sexual health education in Sub-Saharan Africa between 2013 and 2024?
- What are the essential steps for developing and implementing an e-health intervention for adolescent sexual health in Sub-Saharan Africa?
1.6. Theoretical Framework
This study used the Technology Acceptance Model (TAM) combined with the Diffusion of Innovations Theory (DIT). Integrating the TAM with the Diffusion of Innovations Theory (DIT) provides a robust framework for understanding the adoption and acceptance of new technologies in various contexts [25]. By combining these two theoretical perspectives, researchers can gain insight into the factors that influence individuals' intentions to use and adopt innovative technologies, making them suitable for the study’s focus on e-health interventions for adolescent sexual health in SSA. Researchers have empirically investigated students' intention to use e-learning systems by integrating TAM with innovation diffusion theory [26]. The study highlighted the significance of this theoretical integration in the educational context, emphasising its potential to enhance our understanding of students' technology acceptance behaviours. By bridging TAM's focus on individual perceptions with Diffusion of Innovations Theory's emphasis on social influence, the study provided valuable insights into students' intentions to use e-learning systems. In the context of e-government services, the two frameworks provide a suitable platform to examine the factors motivating government employees to use e-government systems by highlighting the importance of adopter profiles and acceptance factors in shaping employees' intentions to use e-government systems [27, 28]. For instance, TAM and the diffusion of innovation theory were applied in Malaysia to explore technology adoption, highlighting the role of perceived innovation characteristics in influencing user intentions [29]. Similarly, another study used these theories and the Unified Theory of Acceptance and Use of Technology (UTAUT) to analyse the adoption of the Internet of Things (IoT) in Saudi Arabia, offering insights into acceptance modelling [30]. In Kenya, TAM and diffusion of nnovations were employed to study a digital sexual health education tool, demonstrating their unified effectiveness in explaining user behaviours in resource-poor settings [31]. These studies collectively underscore the relevance of these theoretical models in understanding individual and social influences on adopting e-health. By integrating these theoretical frameworks, the study provided an in-depth understanding of the factors influencing technology adoption in the public sector. This combined approach allows for an understanding of individual-level factors, such as perceived usefulness and ease of use, and broader systemic factors, such as communication channels, social systems, and innovation attributes that influence the adoption and implementation of e-health interventions for adolescent sexual health.
| S.No. | Criteria | Inclusion | Exclusion |
|---|---|---|---|
| 1 | Study Design/Approach | Mixed-methods, qualitative, and quantitative studies, systematic review | Case reports, opinion pieces without empirical, and studies not addressing SRH. |
| 2 | Population | Adolescents in SSA | Studies do not focus on adolescents in SSA. |
| 3 | Intervention/Focus | E-health interventions aimed at improving adolescents' SRH outcomes | Studies not focussing on e-health intervention |
| 4 | Language | Studies published in English | Studies not published in English |
| 5 | Publication Date | 2013 to 2024 | Before 2013 |
2. METHODOLOGY
We used a systematic review approach guided by the PRISMA framework to investigate e-health interventions for adolescent sexual health in SSA from 2013 to 2024. The choice of PRISMA for the review ensures the quality and transparency of the study and improves the credibility and reproducibility of research findings [32, 33]. The review synthesised the existing literature on e-health interventions for adolescent sexual health in SSA to answer research questions. The search used PubMed, Scopus, Web of Science, and African Journals Online databases. The following keywords and phrases were employed in the literature search to maximise the relevance of the results: “e-health,” “adolescent sexual health,” “Sub-Saharan Africa,” “e-health interventions,” “adolescent sexual health,” “Mobile health,” “sexual and reproductive health,” and “digital health solutions.” PROSPERO ID:640195
2.1. Inclusion and Exclusion Criteria
A rigorous quality evaluation process was applied to the included studies using a standardised appraisal checklist. This assessed the clarity of the objectives, the methodology, the data analysis and the relevance to the research questions. Mixed-methods studies were evaluated on integration, qualitative studies on depth and richness, and quantitative studies on statistical validity and reliability. Two independent reviewers conducted the evaluation to minimise bias, resolving discrepancies through discussion and consensus. This ensured the inclusion of high-quality studies that provided comprehensive perspectives on e-health interventions. The study's inclusion and exclusion criteria are outlined in detail in Table 1.
This systematic review adhered to the PRISMA framework, specifically the four stages: identification, screening, eligibility assessment, and inclusion [32]. A comprehensive literature search was conducted in PubMed, Scopus, Web of Science, African Journals Online, and Google Scholar databases, covering articles published in English between 2013 and 2024. The search strategy combined relevant terms to produce 1583 initial records. After eliminating duplicates, the relevance of the abstracts was rigorously screened using the inclusion and exclusion criteria (Table 1). This process narrowed down the eligible studies to 139. Further screening of full texts of 139 eligible studies excluded preprints, dissertations, and studies that do not align fittingly with the study objectives, resulting in 17 studies that strictly met the inclusion criteria. The full texts of these 17 studies were meticulously reviewed to verify alignment with the predetermined criteria. As illustrated in Fig. (1), this rigorous process ensured the inclusion of only the most relevant and methodologically sound studies for subsequent analysis.
The 17 selected studies (Table 2) underwent a critical assessment to assess their rigour and relevance to the research questions. A standardised data extraction method was used, capturing eight key variables: author and publication year, title, research setting, research design, data analysis method, research aims, key findings, and recommendations. To ensure the reliability and validity of the findings, two independent reviewers conducted a quality assessment of the included studies using predetermined selection criteria. Any discrepancies that occurred during study selection and data extraction were resolved through collaborative discussion and consensus between the author and reviewers, improving the robustness of the study's conclusions.
2.2. Data Analysis
The findings of the 17 selected studies were subjected to a thematic analysis [51] to identify common themes, trends, and insights regarding the impact of e-health on adolescent sexual health in SSA. This systematic analysis facilitated the drawing of meaningful conclusions and the development of a roadmap for implementation. The analysis began with developing a coding scheme or framework [52] to guide the analysis and ensure a structured approach to content interpretation. We established coding rules to maintain consistency and objectivity throughout the analysis [53]. These rules guided the classification and systematic text data coding according to predefined categories. The text data from the selected articles were then coded, adhering to these rules and categories [54]. The coding scheme was applied to identify themes, patterns and relevant information in all studies, providing meaningful information. After coding, the results were analysed to draw conclusions and identify overarching themes [55]. An iterative approach was employed throughout the coding process, continually refining and adjusting codes to capture emerging patterns and insights from the data [56]. This flexibility allowed for the continued enhancement of the coding process. Furthermore, the coding process involved two independent coders who systematically identified recurring patterns across studies using a predefined framework to ensure transparency and reliability. The initial codes were reviewed and refined based on emerging insights, ensuring consistency with the research objectives. The themes were validated through intercoder reliability by comparing the author's themes with the independent coders. Disagreements were resolved through collaborative discussions, fostering robust and credible results. The thematic coding framework organises the study into six main themes: the effectiveness of e-health interventions, barriers to implementation, policy support and gaps, cultural and social influences, e-health tools and platforms, and recommendations for implementation, as shown in Table 3. We systematically code and categorise data from the selected studies, identify patterns, and synthesise themes aligned with the research objectives and questions. Therefore, the coded data were thematically described, providing a comprehensive overview of the impact of e-health on adolescent sexual health in SSA.
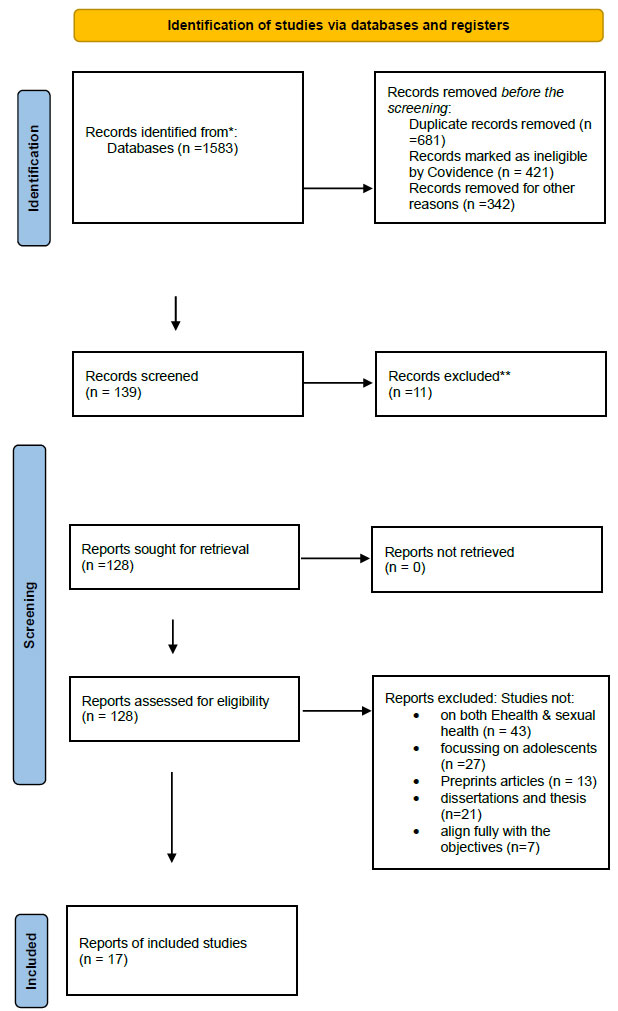
Article selection process guided by PRISMA. (A higher resolution / colour version of this figure is available in the electronic copy of the article).
| S.No. | First Author & Publication Year | Title | Research setting | Research Design | Data Analysis Method | Research Aims | Key Findings | Recommendations |
|---|---|---|---|---|---|---|---|---|
| 1 | Adepoju et al. (2017) [34] | Mhealth for clinical decision-making in sub-Saharan Africa: a scoping review | Sub-Saharan Africa | Scoping review | Thematic analysis | To assess mHealth interventions for clinical decision-making | Identified various mHealth tools to support clinical decisions in low-resource settings | Calls for improving infrastructure and digital literacy |
| 2 | Agblevor et al. (2023) [35] | “We have nice policies but…”: Implementation gaps in Ghana’s adolescent health policy | Ghana | Qualitative | Content analysis | To explore implementation gaps in adolescent health policy | Identified gaps between policy and practice | Suggests policy refinement to bridge practice gaps |
| 3 | Challa et al. (2017) [36] | Social influence on adolescent sexual health decision-making in Ghana | Ghana | Cross-sectional study | Descriptive statistics | To understand social factors in adolescent sexual health decisions | Multiple social influences affect adolescent sexual health choices | Recommends community-based interventions to improve adolescent health literacy |
| 4 | Chen & Mangone (2016) [37] | A systematic review of apps for adolescent pregnancy prevention | Various (global scope) | Systematic review | Comparative analysis | To evaluate mobile apps for preventing adolescent pregnancy | Mobile apps show potential but vary in quality | Calls for standardised evaluation criteria for app effectiveness |
| 5 | Chory et al. (2021) [38] | Mobile intervention for mental health and adherence in adolescents with HIV in Kenya | Kenya | Mixed method | Thematic analysis and descriptive analysis | To test mobile interventions supporting mental health and adherence for HIV patients | Improved mental health and adherence outcomes observed | Suggests scaling successful interventions and increasing accessibility |
| 6 | Cornelius & Appiah (2016) [39] | Using mobile technology to promote safe sex in adolescents | Africa and other regions | Literature review | Thematic synthesis | To explore mobile technology for promoting safe sex and sexual health | Identified effective mobile tech tools | Recommends development of culturally sensitive mobile health tools |
| 7 | Crowley et al. (2023) [40] | Technology-enabled health interventions for HIV adolescents | Low-/middle-income countries | Systematic review | Meta-analysis | To examine the acceptability and effectiveness of health tech for adolescents with HIV | Tech solutions increased acceptability, feasibility, and adherence | Highlights the need for tech adaptations specific to HIV-positive adolescents |
| 8 | Folaranmi (2014) [41] | Mhealth in Africa: challenges and opportunities | Africa | Scoping review | Descriptive analysis | To explore challenges and opportunities for mHealth in Africa | Infrastructure and digital literacy are major challenges | Recommends improving infrastructure and support for mHealth implementation |
| 9 | Karamagi et al. (2022) [42] | Digital health interventions for health systems in sub-Saharan Africa | SSA | Scoping review | Content analysis | To assess digital health interventions for system strengthening | Digital health interventions vary in effectiveness | Calls for standardised digital health policy and infrastructure investment |
| 10 | Lee et al. (2018) [43] | M-health policy readiness in sub-Saharan Africa vs OECD countries | SSA and OECD countries | Comparative analysis | Statistical analysis | To compare m-health policy readiness between regions | OECD countries are better prepared for m-health compared to SSA | Recommends enhancing m-health policy frameworks in SSA |
| 11 | Ruxwana et al. (2014) [44] | Quality assurance model for e-health in rural hospitals in South Africa | South Africa | Qualitative case study | Qualitative synthesis and document analysis | To propose a model for quality assurance in e-health implementation in rural hospitals | Developed a generic quality assurance model | Suggests adopting Quality Assurance models to support e-health success |
| 12 | Ibrahim et al. (2024) [45] | Social media for HIV/AIDS prevention | Africa and other regions | Scoping review | Descriptive analysis | To assess social media’s role in HIV/AIDS prevention | Social media helps increase awareness | Recommends leveraging social media to reach broader audiences |
| 13 | Wang et al. (2022) [46] | Access to digital media among adolescents in SSA | SSA | Survey | Multi-variate analysis | To assess digital access among adolescents | Socioeconomic factors limit digital access | Recommends policies for digital inclusion |
| 14 | AUDA_NEPAD (2023) [47] | Role of digital technologies in adolescent health services | SSA | Policy analysis | Policy evaluation | To evaluate policies enabling digital health for adolescents | Existing policies are supportive but require improvement | Suggests refining policies to close gaps in digital health access |
| 15 | Huang et al. (2022) [48] | Digital strategies for adolescent SRH and gender-based violence prevention | Low-/middle-income countries | Umbrella review | Systematic synthesis | To synthesise digital strategies for SRH and GBV prevention | Digital strategies enhance SRH outcomes | Calls for scaling digital solutions in low-resource settings |
| 16 | Sidamo et al. (2024) [49] | Adolescent utilisation of SRH services in Southern Ethiopia | Ethiopia | Cross-sectional study | Multilevel and latent class analysis | To explore factors influencing SRH service use among adolescents | Found social, economic, and policy factors affecting SRH service utilization | Recommends tailored interventions considering these factors |
| 17 | Chipako et al. (2024) [50] | Impact of SRH interventions for youth in SSA | SSA | Scoping review | Descriptive synthesis | To review SRH interventions and their impact on youth | SRH interventions improve knowledge and access but have challenges | Advocates for context-specific SRH strategies |
| S.No. | Theme | Description | Authors & Publication Year |
|---|---|---|---|
| 1 | Effectiveness of e-health interventions | Examines the impact of e-health interventions on adolescent sexual health outcomes, including knowledge and behaviour change | [34, 38, 40, 48, 50] |
| 2 | Barriers to implementation | Discusses the challenges, including infrastructural limitations, digital literacy, cultural sensitivity, and teacher training | [41, 43, 44, 46, 47] |
| 3 | Policy support and gaps | Identifies supportive provisions for e-health and adolescent sexual health and examines policy gaps related to access, digital divides, and privacy | [35, 42, 43, 45, 47] |
| 4 | Cultural and social influences | Explores the role of social and cultural factors in shaping adolescent sexual health behaviours and receptiveness to e-health interventions | [36, 37, 39, 49] |
| 5 | Digital tools and platforms | Detail types of e-health tools used (e.g., mobile apps, SMS, social media) and their effectiveness in reaching adolescents | [34, 37-39, 45] |
| 6 | Recommendations for implementation | Provides a roadmap and critical steps for effective e-health intervention, including strategies for addressing digital divides, policy updates, and training | [35, 41, 42, 48, 50] |
3. RESULTS
The analysis of the selected literature reveals six key themes, essential to understanding the landscape of e-health interventions for adolescent sexual health in SSA (Fig. 2). Each theme contributes to a better understanding of how digital health technologies can support sexual health literacy and health outcomes for adolescents in SSA while highlighting critical challenges and areas for future improvement.
3.1. Effectiveness of E-Health Interventions
This review revealed that e-health interventions, such as mobile health (mHealth) applications and online platforms, have demonstrated positive outcomes in adolescent sexual health education and behaviour change in SSA. Studies highlight the potential of these tools to improve knowledge of SRH, promote safer practices, and support mental health among adolescents affected by HIV. Furthermore, this review found that technology-enabled interventions improved adherence to HIV treatment among adolescents and that improved SRH outcomes are linked to digital health strategies [40, 48]. These applications can provide a variety of functionalities, including health education, appointment scheduling, and reminders for medication adherence. For instance, mHealth can potentially improve clinical decision-making and patient monitoring, thereby enhancing the efficiency of healthcare delivery in low-resource settings [34]. The same authors noted that the widespread penetration of

The findings of the systematic analysis. (A higher resolution / colour version of this figure is available in the electronic copy of the article).
mobile phones in Sub-Saharan Africa, estimated at over 80%, makes mHealth a viable option to reach diverse populations, particularly adolescents who increasingly rely on mobile technology for information. These findings suggest that e-health solutions can play a significant role in reaching adolescents with critical sexual health information and support. However, further research is needed to quantify these impacts comprehensively.
3.2. Barriers to Implementation
The findings of this systematic review showed that the successful implementation of e-health interventions in SSA faces considerable challenges. Infrastructure limitations, including inconsistent internet access and limited mobile device availability, pose significant barriers, especially in rural areas [41, 46]. Additionally, insufficient digital literacy and cultural resistance to the adoption of technology further complicate the integration of e-health into adolescent sexual health. This review shows the need for comprehensive policy frameworks to address these challenges and support the broader use of mHealth [43]. These barriers highlight the need for multifaceted strategies to improve technology access, increase digital skills, and foster a supportive cultural environment.
3.3. Policy Support and Gaps
It emerged from the analysis that the current policies supporting e-health in adolescent sexual health demonstrate both progress and limitations. While some SSA governments and organisations have developed policies encouraging digital health initiatives, significant gaps persist, particularly in privacy protection, digital inclusion, and equitable access to resources. A study identifies disconnects between policy intentions and implementation in Ghana, while AUDA_NEPAD calls for refined policies to close digital divides [35, 47]. Addressing these gaps is critical to creating an enabling environment for e-health solutions, ensuring that interventions are accessible, secure, and effective for all adolescents.
3.4. Cultural and Social Influences
The findings indicate that cultural and social factors influence the receptiveness of adolescents to e-health interventions. Studies indicate that social norms, family expectations, and peer influences play a crucial role in shaping adolescents' attitudes toward sexual health and their use of digital health tools. For example, this review highlights the impact of social norms on adolescents' sexual health decisions in Ghana, suggesting that e-health interventions must be culturally sensitive and contextually relevant [36]. These findings underline the importance of incorporating cultural considerations into the design and implementation of e-health solutions to improve their acceptability and effectiveness among adolescents in SSA.
3.5. Digital Tools and Platforms
This review highlights various digital tools for delivering e-health interventions, including mobile applications, SMS programmes, and social media platforms. These tools offer an accessible and scalable means of reaching adolescents with information on SRH. Various studies demonstrate the efficacy of various mobile apps and social media in promoting safe sex practices and preventing adolescent pregnancy and highlight the advantages of using social media for HIV/AIDS prevention [34, 37, 39, 45]. However, despite their potential, the effectiveness of these tools often depends on adequate infrastructure, digital literacy, and a supportive policy environment.
3.6. Recommendations for Implementation
This study provides actionable recommendations for developing and implementing e-health interventions in SSA. Key suggestions include addressing infrastructure barriers, such as limited digital access, through investments in mobile technology and internet coverage. Additionally, researchers emphasise the importance of providing educators with adequate training to use digital tools effectively and ensuring that content is culturally sensitive and age-appropriate [42, 50]. Policymakers are urged to update existing frameworks to promote digital inclusivity, protect user privacy, and ensure the sustainability of e-health initiatives. These recommendations offer a roadmap for stakeholders that aims to maximise the impact of e-health on adolescent sexual health in SSA.
4. DISCUSSION
This study shows the potential effectiveness of e-health interventions in improving health outcomes in Sub-Saharan Africa. E-health applications have revolutionised healthcare delivery in SSA, providing a convenient platform for disseminating SRH information directly to users' smartphones [34]. The same study highlights the ability of these apps to improve access to personalised health resources. Similarly, another study advocates for the use of websites and online portals as comprehensive hubs for safe sex education, contraception guidance, and information on STIs [57]. The study further emphasises the interactive potential of these platforms, such as forums and anonymous chat services, which foster user engagement and facilitate confidential consultations with healthcare professionals. In addition, an earlier study argues that SMS-based interventions are critical in promoting positive health behaviours, demonstrating success in encouraging adolescent contraceptive use [58]. These findings underscore the potential of SMS services as scalable and cost-effective tools for public health messaging. Another study highlights the role of social media platforms in addressing the stigma surrounding sexual health issues. The study argues that peer-to-peer communication facilitated by these platforms can normalise discussions around sensitive health topics, thereby improving health-seeking behaviours [59]. Likewise, a recent study supports this assertion, positing that social media is an underutilised but powerful medium for advancing adolescent SRH in contexts like South Africa, where stigma and cultural taboos often hinder open dialogue about sex [11]. This review indicates the transformative potential of telemedicine in SRH, particularly for underserved populations in remote regions. This aligns with another research that argues that telemedicine bridges critical gaps in healthcare access by enabling remote consultations for services such as STI testing and family planning advice, effectively mitigating geographical barriers [60]. However, the challenges of implementing these interventions include infrastructural limitations and socio-cultural barriers [61]. Despite these challenges, the evidence suggests that e-health interventions can effectively improve health outcomes, particularly when integrated into existing healthcare systems.
In support of the findings, a meta-analysis study demonstrates that digital tools increase awareness of safe sexual practices [62]. In the same vein, another study reports improved condom use and intentions among social media intervention participants [63]. Furthermore, another research links improved sexual health knowledge to improved mental and social well-being, highlighting the broader benefits of e-health interventions [64]. Comparative analyses reveal the strengths of various technologies: mobile health applications excel in personalising health information and sustaining engagement [65]. At the same time, social media platforms effectively reach broader audiences and promote community participation [63]. SMS-based tools offer immediacy and accessibility, demonstrating their role in improving knowledge and reducing risky behaviours [66].
This systematic review showed that implementing e-health solutions in SSA presents various challenges, including infrastructure limitations, privacy concerns, cultural sensitivity, and policy barriers, which shape its effectiveness and acceptance. This agrees with the other studies which show that disparities in internet access and limited smartphone availability in rural areas exacerbate inequities in healthcare delivery [67] and that low technological literacy is a significant barrier [68], necessitating the need for investment in digital literacy programmes. Furthermore, privacy concerns pose a barrier to engagement, as many adolescents are deterred from using digital health platforms due to inadequate data protection measures, fearing that their personal information will be compromised and confidentiality breached [69]. Cultural norms also play a critical role in accepting e-health due to the stigma surrounding SRH services [70]. Thus, there is a need for culturally sensitive interventions tailored to local contexts. An earlier study conducted in Nigeria advocates for the participation of community stakeholders in developing content to promote relevance and acceptance [68]. Likewise, some qualitative findings highlight two crucial factors in the success of e-health interventions: user-centered design and community engagement. Specifically, the study underscores the importance of creating user-friendly and culturally relevant designs that cater to the diverse needs of the target population [71]. Furthermore, community engagement plays a vital role in ensuring the effectiveness and sustainability of these interventions [72]. In addition, legal and policy barriers further complicate these challenges, impeding the effective implementation of e-health interventions. For instance, the restrictive regulations governing SRH education, as observed in certain cities in the United States, can constrain the scope and impact of these interventions, thus hindering their potential to improve health outcomes [73].
Furthermore, this review correlates that integrating e-health interventions into existing healthcare systems is crucial for maximising their impact. This aligns with the findings of another study that advocates for strengthening integrated sexual reproductive health and rights programs to achieve sustainable development goals in Africa [74]. This integration can facilitate referrals to clinics for services such as STI testing and contraceptive provision, ensuring that users receive holistic care. However, there is a need for ongoing training for healthcare providers to utilise e-health tools and engage with patients meaningfully and effectively [75]. Addressing these challenges is essential for ensuring the successful implementation of e-health interventions. The role of community health workers in implementing e-health interventions is also a critical consideration. A SSA study highlights the effectiveness of community-based interventions in preventing diseases among people living with HIV [76]. By equipping community health workers with mobile devices and training them in digital health literacy, they can better support their communities, facilitating access to health information and services. Nevertheless, weak health systems and inadequate funding can impede the long-term success of digital health programs [77]. Addressing these challenges is essential for ensuring the sustainability of e-health interventions.
The study findings reveal both progress and persistent gaps that shape the effectiveness of interventions in SSA. As highlighted by a study conducted in rural Zambia, there is a growing emphasis on mHealth integration in health systems, with national policies increasingly leveraging digital strategies to improve access to SRH services [78]. Similarly, another study indicates the shift toward holistic and comprehensive sexuality education, addressing not only biological but also social and emotional aspects of sexual health, as seen in Zambia’s policies that aim to delay sexual debut and promote safer practices [79]. However, critical gaps undermining these advancements, particularly in infrastructure, are inadequate internet access and low technological literacy, limiting the reach of e-health solutions, especially for marginalised groups [80]. Privacy and confidentiality also remain concerns, as adolescents’ engagement is hindered by insufficient protections, fostering distrust on digital platforms [81]. Furthermore, this review noted that policies often fail to accommodate diverse cultural norms, with restrictive beliefs about adolescent sexuality exacerbating adverse outcomes like unintended pregnancies and STIs [36]. Trends in policy development over the decade reveal increased technology adoption, with the call for national health indicators to track progress and greater multi-sectoral collaboration to address complex adolescent health needs [82]. Despite these advances, persistent implementation gaps, with conflicting attitudes among policymakers, still exist, leading to inconsistent enforcement and inadequate resources [35]. Addressing these challenges is crucial to translating policy into impactful practice for the sexual health of adolescents in the SSA.
4.1. Theoretical Implications
The theoretical implications of this study’s findings highlight the value of the Technology Acceptance Model and the Diffusion of Innovation theory in understanding the adoption of e-health interventions for adolescent sexual health in SSA. The Technology Acceptance Model emphasises that perceived ease of use and perceived usefulness are central to technology adoption. Adolescents are more likely to engage with e-health platforms when these tools are intuitive and demonstrably beneficial to their health. This study illustrates that access to user-friendly and effective digital health resources significantly shapes adolescents’ decision-making in SRH [36]. Furthermore, culturally tailored content improves the perceived usefulness of these tools. For example, addressing stigma and fear through targeted e-health solutions increases their appeal [83]. By ensuring that e-health interventions are accessible and relevant to adolescents’ needs, stakeholders can enhance the likelihood of widespread adoption.
The diffusion of innovation theory complements the technology acceptance model by exploring the social dynamics and characteristics of innovations that influence their uptake. The role of social norms and peer influences is significant, although its specific impact on adolescents’ sexual health behaviours warrants further research [84]. Trialability and observability also emerge as critical factors in encouraging adoption, as adolescents are more likely to embrace innovations that they can experiment with or observe their peers use effectively. Furthermore, a pilot study of a mobile intervention for mental health among HIV-positive adolescents in Kenya demonstrates that peer support promoted engagement and trust in the platform [38]. These findings align with the Diffusion of Innovation theoretical principles, emphasising that accessible, demonstrably effective, and socially supported innovations are more likely to succeed.
4.2. Roadmap to Implementation
Implementing e-health interventions for adolescent sexual health in SSA requires a comprehensive strategy addressing key challenges in infrastructure, cultural sensitivity, and data privacy. Central to this roadmap is stakeholder engagement, as engaging policymakers, healthcare providers, educators, community leaders, and adolescents ensures that interventions are tailored to diverse cultural contexts and specific adolescent needs. Capacity building is another priority, with targeted training for healthcare and community workers in using e-health platforms to effectively deliver culturally relevant and accurate information [85]. Infrastructure development is crucial, and it requires investments in reliable internet connectivity and mobile technology to bridge the digital divide, particularly in underserved areas of SSA. Partnerships with telecommunications providers can be crucial to expanding access to e-health tools [86].
To enhance acceptability, e-health solutions must be culturally sensitive. Collaborating with cultural experts and community leaders can ensure that content aligns with local norms and values, fostering trust and engagement. In addition, robust data privacy and security measures must be implemented to protect user confidentiality and build trust in digital platforms. Adhering to international data protection standards and training health providers on ethical practices can mitigate privacy concerns [87]. Finally, integrating e-health interventions into national health strategies ensures sustainability, scalability, and alignment with broader public health goals. Regular monitoring and evaluation mechanisms should assess their impact, track progress, and inform iterative improvements [82].
4.3. Stakeholder-Specific Recommendations
- Policymakers in SSA countries are urged to prioritise e-health in their national health agendas by addressing infrastructure gaps, strengthening privacy regulations, and promoting cultural adaptation in digital health interventions. Setting clear guidelines for implementation and fostering multi-sectoral collaboration can ensure cohesive strategies across the health, education, and technology sectors [85]. They should also allocate funding to expand connectivity and advocate for supportive legal frameworks to reduce barriers to e-health adoption in their countries [88].
- Healthcare professionals in various SSA health facilities need training in e-health tools and maintaining patient confidentiality to foster a supportive and non-judgmental adolescent environment. Capacity-building initiatives should equip providers with the skills to engage adolescents effectively and deliver culturally relevant care [87].
- Educators and educational authorities must be vital to improving technological literacy by incorporating digital health education into school curricula. Schools in SSA should serve as critical access points for adolescents to learn how to navigate e-health platforms confidently, empowering them to take control of their sexual health [80].
- Technology developers interested in introducing e-health products in SSA must collaborate with health professionals and community stakeholders to design intuitive, user-friendly digital health platforms suited to the needs of adolescents. Continuous user feedback should guide iterative improvements to these tools, ensuring they remain relevant and effective [86].
- Community leaders should be involved in developing and disseminating e-health interventions to ensure cultural alignment. Their participation can help address stigma and promote acceptance of sexual health education and interventions in traditionally sensitive contexts in SSA [36].
- For researchers, prioritising longitudinal studies would provide valuable information on the long-term effects of e-health interventions on adolescent sexual health outcomes in Sub-Saharan Africa. Furthermore, conducting a meta-analysis study would offer a more comprehensive understanding of the effectiveness of eHealth interventions, synthesising existing research to inform evidence-based practices.
These multi-stakeholder recommendations for the implementation of e-health interventions can address the multiple challenges of SSA adolescent sexual health, fostering improved outcomes and long-term sustainability.
4.4. Conceptual Framework for Implementing E-Health for Adolescent Sexual Health in Sub-Saharan Africa
The conceptual framework for implementing e-health interventions to improve adolescent sexual health in SSA, as illustrated in Fig. (3), integrates theoretical foundations, five key pillars, stakeholder roles, and a roadmap for implementation to achieve targeted outcomes. Based on the Technology Acceptance Model and Diffusion of Innovations theory, the framework underscores the importance of perceived ease of use, perceived usefulness, and social influences in adopting e-health tools. These theories provide a lens for understanding how adolescents and communities in SSA engage with digital platforms and highlight factors such as trialability, observability, and cultural acceptance as critical to success.
The five key pillars of the framework are foundational infrastructure, cultural adaptation, technological accessibility, policy and governance, and monitoring and evaluation. Foundational infrastructure focuses on improving telecommunications, Internet access, and mobile connectivity, particularly in underserved areas. Cultural adaptation ensures that e-health interventions are aligned with local norms through community engagement. Technological accessibility emphasises user-friendly tools, affordability, and digital literacy programmes for adolescents and educators. Policy and governance address data privacy, multi-sectoral collaboration, and supportive legal frameworks while monitoring and evaluation ensure continuous assessment and refinement of interventions to optimise outcomes.
The implementation roadmap consists of four phases: Planning and Engagement, Capacity Building, Deployment, and Monitoring and Iterative Improvement. These phases guide the systematic roll-out of interventions, from stakeholder consultations and capacity-building initiatives to deploying e-health platforms and evaluating their impact. Key stakeholders include policymakers, health professionals, educators, technology developers, community leaders, and adolescents, each playing a vital role in ensuring culturally sensitive, sustainable, and effective interventions. By fostering collaboration among stakeholders, addressing infrastructural gaps, and prioritising user needs, the framework could improve access to SRH services, enhance knowledge, reduce stigma, and establish sustainable health systems for adolescents in SSA.
4.5. Limitations of the Study
This study focuses on e-health interventions from 2013 to 2024 and may exclude relevant older studies, potentially limiting the scope of the knowledge gained.
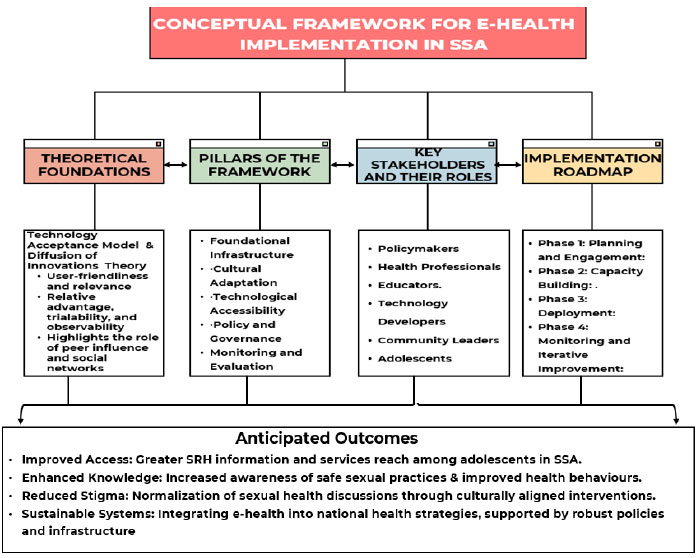
E-health conceptual framework. (A higher resolution / colour version of this figure is available in the electronic copy of the article).
Furthermore, the study's findings may not be generalisable beyond Sub-Saharan Africa, as different regions have unique healthcare systems and cultural contexts that may affect the applicability of the results. Interpretation of the study findings should consider these limitations.
CONCLUSION
This study highlights the transformative potential of e-health interventions in addressing adolescent sexual health challenges in sub-Saharan Africa. By integrating theoretical foundations such as the technology acceptance model and Diffusion of Innovations theory (DIT), the framework underscores the critical factors influencing the adoption and sustainability of e-health solutions. The proposed pillars, foundational infrastructure, cultural adaptation, technological accessibility, policy and governance, and monitoring and evaluation provide a comprehensive roadmap for implementing effective and context-specific interventions. Successful implementation depends on multi-sectoral collaboration, stakeholder engagement, and culturally tailored approaches that address infrastructural gaps, digital literacy, and privacy concerns. If implemented effectively, these strategies will enhance access to sexual and reproductive health services, empower adolescents with knowledge, reduce stigma, and establish resilient health systems, ultimately improving health outcomes and well-being for adolescents in the SSA region.
AUTHORS’ CONTRIBUTION
The authors confirm their contribution to the paper as follows: study conception and design: AA; data collection: II. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| SSA | = Sub-Saharan Africa |
| TAM | = Technology Acceptance Model |
| DIT | = Diffusion of Innovations Theory |
| PRISMA | = Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| HIV | = Human Immunodeficiency Virus |
| UTAUT | = Unified Theory of Acceptance and Use of Technology |
AVAILABILITY OF DATA AND MATERIAL
The data supporting the findings of the article are available on figshare: https://figshare.com/account/ articles/28444061 DOI: 10.6084/m9.figshare.28444061.
ACKNOWLEDGEMENTS
Declared none.


