All published articles of this journal are available on ScienceDirect.
Optimizing Early Discharge Planning in Oncology: Improving Health Service using Lean Six Sigma Methodologies
Abstract
Background
Early discharge planning (EDP) in oncology is essential for ensuring continuity of care, reducing prolonged hospital stays, and optimizing resource utilization. Prolonged hospital stays can increase the risk of infections, delay access to new admissions, and strain healthcare resources. Implementing Lean Six Sigma methodologies significantly improved discharge planning by reducing workflow inefficiencies, enhancing compliance, and optimizing resource utilization. The structured use of DMAIC and process capability analysis led to reduced hospital stays, lower bed occupancy, and improved patient transitions, highlighting LSS as a practical framework for continuous quality improvement in oncology care.
Purpose
This study aimed to improve workflow efficiency, compliance, and patient outcomes in oncology discharge planning by implementing Lean Six Sigma methodologies.
Methods
The study was conducted at the Sultan Qaboos Comprehensive Cancer Care and Research Center; this pre-and post-intervention study applied the DMAIC (Define, Measure, Analyze, Improve, Control) cycle to identify inefficiencies and implement targeted interventions. Cp (Process Capability Index) and Cpk (Process Capability Index for Centering) are key indicators used to evaluate a process's ability to meet specified limits. Length of stay, compliance rates, and bed occupancy were also analyzed. Qualitative data supplemented the findings from staff interviews and process mapping.
Results
Post-intervention, the mean compliance rate was increased to 89.54% from 68.10% (p-value <0.05). By 68.82%, the observations below 80% compliance threshold were reduced. Process capability indices improved, with Pp rising to 0.41 from 0.22 and Ppk increasing to 0.39 from -0.27. As reflected by improvements in the Z.Bench score, Variability was significantly reduced from -0.80 to 1.18. The bed occupancy rate experienced a noticeable decline to 77% in September 2024 from 95% in June 2024 (p-value <0.05). An overall decrease in the average length of stay (LOS) was shown to be 6.5 days in September 2024, compared to 9.0 days in June 2024 (p-value <0.05).
Discussion
The study demonstrated that implementing Lean Six Sigma significantly improved discharge compliance, reduced bed occupancy, and shortened the length of hospital stay, highlighting its effectiveness in optimizing oncology workflows. These results support existing research that emphasizes LSS as a valuable tool for reducing process variability and enhancing patient-centered care through structured, data-driven interventions. However, the study’s single-institution design and lack of a control group limit the generalizability of findings, suggesting a need for further validation in diverse healthcare settings.
Conclusion
Implementing LSS in oncology discharge planning significantly improved process efficiency and compliance. The significant reduction in LOS reflects the success of Lean Six Sigma in enhancing efficiency, improving patient safety, and optimizing hospital resource utilization, leading to better patient outcomes in oncology care. The findings underscore the potential of Lean Six Sigma methodologies to optimize workflows and foster a culture of continuous improvement in healthcare.
1. INTRODUCTION
Discharge planning is a structured process developed to safely and effectively transit patients from inpatient to outpatient care or home settings [1, 2]. It includes collaboration among a multidisciplinary team, such as nurses, social workers, oncologists, and caregivers, to meet patients and their families' needs. This process covers identifying potential challenges and barriers to discharge, setting achievable goals, and individualize care plans covering medical, emotional, and logistical aspects [3, 4].
Early planning is crucial since it supports anticipated barriers, such as follow-up care, medication adherence, and managing side effects and complications [5, 6]. Initiatives like structured communication frameworks and multidisciplinary rounds ensure that the aspects of patient care are acknowledged and addressed for a smooth transition [1, 3].
Effective discharge planning benefits oncology patients and their families, healthcare workers, and the healthcare organization [7]. For patients, it ensures reduced risk of hospital readmissions and continuity of care and promotes efficient treatment that enhances the quality of life [1, 7]. Early identification and addressing discharge barriers can lead to timely and efficient interventions, improving patient outcomes and satisfaction [8, 9]. From a healthcare perspective, efficient discharge planning optimizes hospital stays and resource utilization and reduces healthcare costs [10].
Oncology patients require structured discharge planning to ensure timely follow-up care, prevent hospital readmissions, and optimize bed availability. However, many hospitals face significant challenges that hinder the efficiency of the discharge process. Inconsistent compliance with discharge protocols often delays patient transitions, while prolonged bed occupancy due to inadequate discharge coordination impacts hospital capacity and timely admissions. The lack of standardized discharge workflows also results in variability across departments, creating inefficiencies in patient care transitions. These issues are further compounded by operational inefficiencies that reduce resource utilization and escalate hospital costs, highlighting the need for a structured, data-driven approach to improving oncology discharge planning [9-11].
Many studies showed significant improvements in the oncology setting using different quality improvement models [12-23]. A survey aimed at standardizing the discharge process for inpatient hematology and oncology patients demonstrated that implementing a structured discharge protocol reduced the average time to follow-up appointments from 17 to 10 days [9]. This improvement facilitated timely post-discharge care, potentially reducing readmission rates and enhancing patient outcomes. Another study examined the effectiveness of a discharge plan model for South Korean cancer patients transitioning back to the community. The findings highlighted the importance of comprehensive discharge planning in addressing patients' social and medical needs and improving their post-discharge quality of life [10].
Integrating Lean Six Sigma with EDP is essential to address the challenges in oncology service to provide care by confirming a timely patient discharge. This reflects EDP effectiveness by enabling appropriate management and better care quality of ICU transfers and patient critically sick admissions [19-29]. Moreover, congestion in operational expenses is minimized by the LSS through a facilitated discharge process and decreasing delays [12]. Strategies related to contributing factors in oncology care included high-quality metrics such as enhancing patient satisfaction rate and decreasing patient readmission [11, 12].
LSS methodologies have been increasingly adopted in healthcare to improve service quality and operational efficiency [30-49]. A systematic literature review identified that combining Lean and Six Sigma principles effectively reduces waste and process variability, leading to enhanced patient care and reduced costs [20]. Further research into LSS applications in healthcare settings revealed that these methodologies are effective across various contexts, including hospitals and outpatient clinics. The studies reported improvements in internal processes and customer perspectives, underscoring the versatility and efficacy of LSS in healthcare [21].
Furthermore, the LSS methodology has successfully impacted the interventions without affecting patient safety and highlighted the improvements in coupling EDP and LSS, which is reflected by reducing the length of stay (LOS), enhancing the allocation of resources, and improving the efficiency of the discharge process [22-29]. Thus, utilizing LSS tools with the Enhanced Recovery After Surgery (ERAS) protocols has created a robust framework in complicated oncology cases through achieving early and safe discharges [13, 14].
Despite all benefits, identified gaps and barriers such as inconsistency with patients' needs, lack of process standardization, and resource constraints urged the adoption of the LSS within the EDP framework [50-79]. Contrariwise, implementing Lean Six Sigma tools such as root cause analysis and process mapping to address gaps helps continuously improve the culture and ensures efficient discharge planning processes [27, 28]. Optimizing a better workflow and delivering patient-centered care remain crucial for implementing LSS in the oncology center for early discharge planning. However, enhanced operational efficiency ensures that LSS assists in timely discharging patients, minimizing congestion, and progressing the quality of delivery care [19, 23, 24]. Additionally, the usage of the LSS predictive analysis approach has been identified proactively in patients suitable for early discharge by reallocating resource utilization [23-25].
Leveraging Lean Six Sigma methodologies in early discharge planning is a key principle in reestablishing the standards of care in an oncology setting to achieve better patient outcomes, improving cost-effectiveness and overall healthcare efficiency in the future of the evolving healthcare system [21, 22]. This approach supports patients in better recovery through the proper coordination and follow-up care and reduces system inefficiencies [23, 24].
At Sultan Qaboos Comprehensive Cancer Care and Research Centre (SQCCCRC), oncology discharge planning remains a critical challenge, with inefficiencies leading to prolonged hospital stays, high bed occupancy, and inconsistent compliance with early discharge protocols. Existing discharge workflows lack standardization, causing process variability and operational delays. While Lean Six Sigma methodologies have been widely applied in healthcare settings, their role in optimizing oncology discharge planning at SQCCCRC remains underexplored.
This study aims to bridge this gap by applying LSS methodologies to streamline workflows, improve compliance with early discharge protocols, and enhance hospital resource utilization. The research seeks to answer the question: Can LSS interventions significantly enhance discharge planning outcomes at SQCCCRC? It is hypothesized that implementing Lean Six Sigma will lead to measurable improvements in compliance, efficiency, and patient flow, ultimately optimizing oncology discharge planning in this setting.
2. METHODS
2.1. Setting
The project was conducted at the Sultan Qaboos Comprehensive Cancer Care and Research Center (SQCCCRC), located within the University Medical City in Muscat, Oman. It is a state-of-the-art oncology center that offers comprehensive cancer treatment and research.
2.2. Design
The sample was a pre- and post-quality improvement design. Key metrics of the early discharge process in oncology patients were compared before and after LSS interventions to improve the process [11-15].
2.3. Sample
For a pre-and post-quality improvement design (pre- and post-intervention, but with different groups), the required sample size to achieve 80% power at a 0.05 significance level with a moderate-to-large effect size (Cohen’s f = 0.8) is 14 observations per group. Since the study had 30 pre-intervention observations and 51 post-intervention observations, the sample size exceeded the required threshold, ensuring sufficient power to detect statistically significant differences.
3. LEAN SIX SIGMA STEPS (DMAIC CYCLE)
3.1. Define
The project team identified primary issues, such as inefficiencies in the early discharge process and underperformance of the key performance indicators (KPIs) like poor compliance with discharge protocols, discharge timing, length of stay, cost saving, and bed occupancy rates were identified by the project team and developed a problem statement, based on how delays in discharge workflows impact resource utilization.
3.2. Measure
Based on the Center’s policy, an auditing checklist was developed to collect data on the current discharge process by including the average compliance with the early discharge process, and outcome key performance indicators were also measured involving the time of discharge, length of stay, and bed occupancy rates. Measures highlighting the workflow bottleneck included quantitative and qualitative data, such as interviewing staff, making direct observations, and reviewing patients' medical records.
The Measure phase involved collecting baseline discharge compliance data using statistical tools, including Process Capability Analysis and IMR Control Charts, to assess process performance and variability. Descriptive and inferential statistics were applied to determine compliance rates, process capability indices (Cp, Cpk), and variation trends over time.
3.3. Analyze
Mapping the process discovered ineffective documentation, lack of coordination between departments, and the absence of patient discharge readiness. However, identifying contributing factors to delays involved several root cause analysis techniques such as fishbone diagram and Pareto analysis. The feedback from the staff provided insights into the operational challenges.
3.4. Improve
Piloting targeted before fully implementing interventions such as streamlining discharge documentation processes, assigning discharge coordinators, implementing electronic discharge systems, and conducting staff training ensure that these solutions are feasible and practical. The Improve phase incorporated data-driven interventions, such as workflow standardization, real-time tracking mechanisms, and enhanced documentation procedures to optimize discharge flow. To quantify improvements, post-intervention compliance was measured using Process Capability Indices (Pp, Ppk) and Defects Per Million Opportunities (DPMO).
3.5. Control
Standard operating procedures (SOPs) were revised, tools for monitoring were introduced, and periodic audits were scheduled to ensure sustainability. The Control phase utilized IMR Control Charts to monitor ongoing performance and ensure process stability. Additionally, a dashboard was developed to track key performance indicators, ensuring the continuation of compliance and areas identified for future improvement.
4. DATA ANALYSIS
Quantitative data analysis was conducted using SPSS and Minitab to evaluate the impact of the intervention on oncology discharge planning. Descriptive and inferential statistical methods were applied to compare pre- and post-intervention metrics, including compliance rates, bed occupancy, and length of stay. The Friedman Test assessed significant differences over time, with a p-value threshold of <0.05 considered statistically significant.
Additionally, Process Capability Analysis was performed using Process Potential Index (Pp) and Process Performance Index (Ppk) to assess the stability and capability of the discharge process. The Z.Bench score was used to determine process alignment with compliance requirements, reducing the risk of deviations affecting patient care. The percentage of observations out of specification measured compliance adherence, where a decrease indicated improved reliability and efficiency in the discharge process. Defects Per Million Opportunities (DPMO) were also calculated to quantify process defects, with a reduction reflecting fewer inefficiencies and errors in patient discharge [35-54].
5. RESULTS
The sections below align with the DMAIC cycle, and each phase represents the analyzed results.
5.1. Define
The project in the defined phase was defined as “Lean Six Sigma to Improve Oncology Discharge Flow,” which focused on optimizing the availability of hospital beds for oncology patients post-discharge and overall operational efficiency by eliminating waste. A multidisciplinary team was created involving expertise from various departments within Sultan Qaboos Comprehensive Cancer Care and Research Centre (SQCCCRC), University Medical City, Muscat, Oman. Departments collaborated in this project included the Nursing Department, Patient Flow Department, Medical Oncology Department, Pharmacy Department, Holistic Department, Surgical Oncology Department, Dieticians Department, and the Quality and Accreditation Department, in addition to the leadership of the Center. This ensures a comprehensive approach to project goals, integrating clinical, operational, and quality perspectives. The defined project scope was as follows:
Project Name: Lean Six Sigma for Oncology Discharge Optimization.
• Justification: To maximize available beds for incoming patients needing critical care, improvement is essential to enhance the discharge flow. Prolonged bed occupancy by patients without a clinical need generates unnecessary costs and reduces operational efficiency. Optimizing resource allocation and improving the institution's potential revenue directly improves the discharge flow.
• Purpose: Enhancing the early discharge process in an oncology setting is the primary purpose of utilizing Lean Six Sigma to optimize workflow efficiency, enhance patient safety, reduce delays, and ensure a seamless transition from hospital to home care while minimizing unnecessary hospital stays and maximizing resource utilization.
• Goal: Improving compliance with the early discharge process, decreasing bed occupancy and length of stay, decreasing cost, and enhancing early timing for discharging the patients.
• Client: Hospital management and oncology patients.
• Customer Impact: Faster discharge times will improve the patient experience by minimizing their hospital stay, reducing the risk of exposure to hospital-related complications, and ensuring continuity of care promptly.
• Impact on the Organization: Key organizational benefits include reducing unnecessary financial expenditures associated with prolonged hospital stays and enhancing the turnover rate of beds, indirectly contributing to increased revenue generation and improved operational efficiency.
5.2. Measure
The Process Capability Analysis figure provides a statistical baseline for assessing the compliance of the discharge planning process before implementing interventions (Fig. 1). Key metrics reveal significant deficiencies in the current system. The sample mean compliance rate is 68.10%, far below the minimum acceptable level of 80% (Lower Specification Limit, LSL) and well short of the ideal 100% target (Upper Specification Limit, USL). This indicates that, on average, the process is underperforming and failing to meet basic standards. A wide range from below 40% to 90% is represented in the histogram (Fig. 1), demonstrating a variation in the compliance rate. Lack of consistency and the prevalence of data below the acceptable threshold is shown by the fit of a Weibull distribution reaching a peak below 80% in a bell curve; this inconsistency suggests a process that struggles to adhere to discharge protocols reliably.
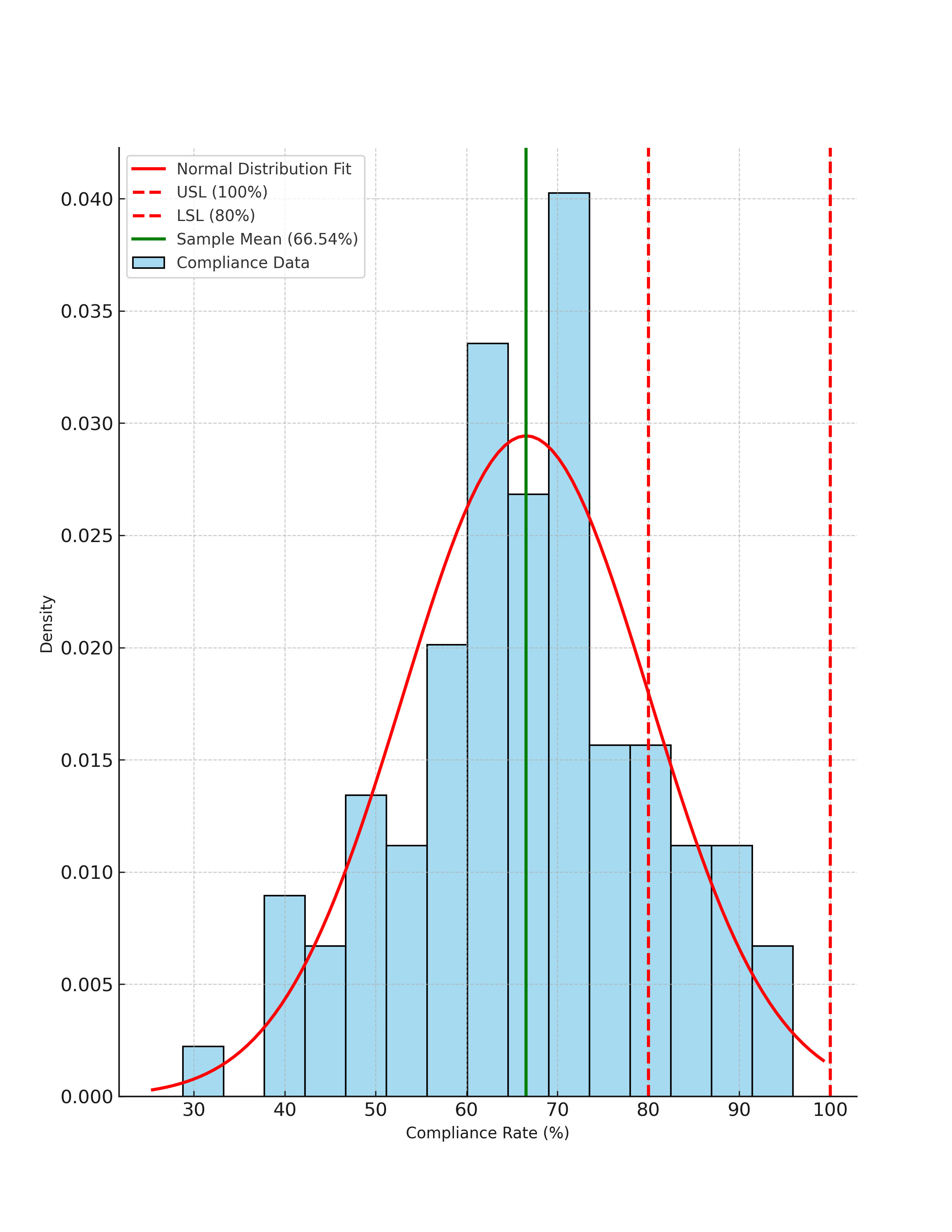
Histogram for compliance with early discharge planning (Pre Data) with normal distribution fit.
This figure illustrates the distribution of compliance rates before intervention. The standard distribution fit (red curve) indicates the overall trend, while the sample mean (green line) highlights the central tendency. The process specification limits (USL = 100%, LSL = 80%) set the acceptable range for compliance. The significant portion of data falling below LSL demonstrates the need for improvement in discharge process adherence.
The Process Capability Indices further quantify the inadequacies. A Cp value of 0.22 illustrates a variation in the process, as evidenced by the excellent significance result compared to the range accepted, indicating that the system lacks the potential to meet compliance requirements consistently. The Cpk value of -0.27 suggests that the process mean is a misaligned and out-of-specification range, reflecting high variability and inability to comply with lower limits. These statistics together demonstrate a process that is incapable and miscentered. Thus, urgent improvements in reducing variability and centering outcomes toward expected standards are required. These insights provide a data-driven basis for targeted Lean Six Sigma interventions in the discharge planning process.
The Control Chart Analysis in Fig. (2) below illustrates the IMR (Individual-Moving Range), showing the low compliance of the early discharge process with a mean below 100%, revealing the need for improvement to comply with the requested standards. Observations were within the Upper Control Limit (UCL) of 100% and the Lower Specification Limit (LSL) of 80%, indicating general compliance. Still, points below the 80% LSL showed unique cause variations that require further investigation. The Moving Range Chart indicated notable variability between consecutive compliance observations, with some ranges exceeding the UCL for moving range, reflecting inconsistencies in the process. These findings emphasize the need to address low compliance rates, reduce variability by standardizing procedures, and enhance consistency in early discharge to ensure better alignment with the target compliance goals.
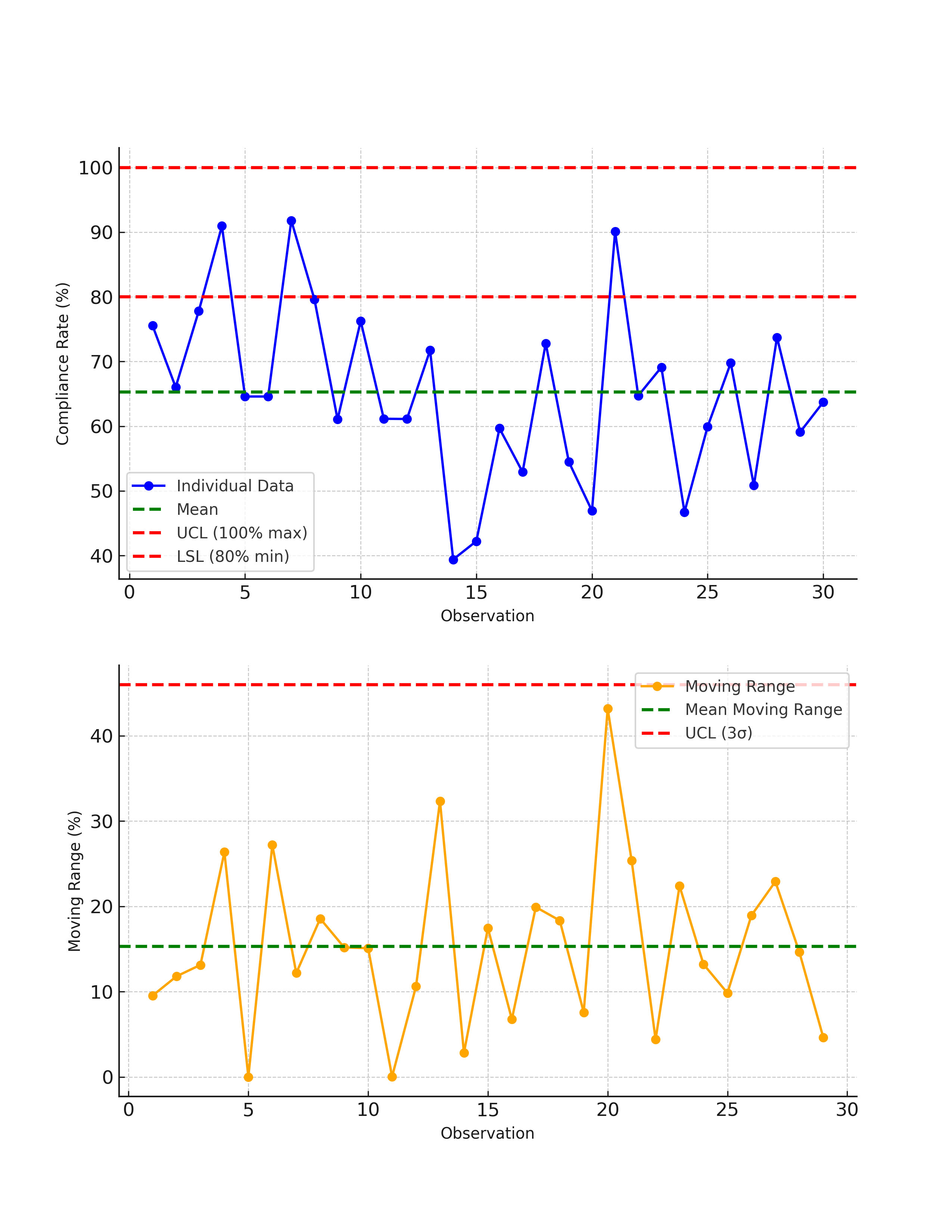
IMR (Individual-Moving Range) control chart for compliance with early discharge planning (pre-intervention).
This figure illustrates the variability in compliance rates before intervention using an Individual Chart (top) and a Moving Range Chart (bottom). The Individual Chart plots compliance rates over time, showing fluctuations around the mean (green dashed line) and highlighting points below the lower specification limit (LSL = 80%) that indicate process inconsistencies. The Moving Range Chart visualizes changes between consecutive compliance rates, with several values exceeding the upper control limit (UCL = 3σ), signifying high process variability. These trends emphasize the need for standardization and process improvements.
5.3. Analysis
The diagram represents a fishbone (Ishikawa) analysis to identify the root causes affecting the effectiveness of discharge planning (Fig. 3). The key categories influencing the process are system, method, staff, and patient factors. System-related issues include unclear policies, roles, and responsibilities, the non-mandatory nature of discharge planning in the hospital information system (HIS), and limited PC availability, which hinders seamless communication and workflow.
This mind map illustrates the key factors contributing to inefficiencies in the discharge planning process. The root causes are categorized into System, Process, Staff, Patient, and Psychosocial Factors.
Process-related challenges involve unclear discharge planning procedures, inadequate consultation programs, lack of standardization, delays in treatment and medication orders, and the absence of discharge integration in huddle meetings, resulting in inefficiencies and delays. Staff-related barriers include lack of coordination, insufficient knowledge about discharge planning, inadequate patient education, time management issues, and physicians' agreement to extend stays at patients' requests, which can lead to resource wastage. Patient-related factors include psychosocial challenges, such as transportation issues and family delays in picking up patients, contributing to discharge delays. These combined factors underline the need for enhancing discharge planning by addressing these systemic, procedural, and interpersonal issues to streamline workflows and improve efficiency.
5.4. Improve
The discharge planning process was improved by implementing several key actions to address inefficiencies and standardize procedures based on the analysis results and many published studies [65-98]. The documentation process for all professionals was standardized, including the location and frequency of updates, to ensure clarity and accountability. Discharge-ready patients were identified through an online platform shared by project members, allowing the team to track and manage cases efficiently. A dedicated discharge planner team was introduced, with clearly defined responsibilities to streamline workflows and enhance communication. Physicians were instructed to complete all consultations before the patient’s final day and finalize discharge orders and medication lists on the morning of discharge. Allied professionals, including dietitians, physical therapists, and social workers, were required to complete their discharge summaries at least one day before the discharge date, with the remaining documentation finalized by 9 a.m. on the day of discharge.
Discharge planning was further integrated into admission protocols, ongoing care, final-day activities, and huddle meetings, ensuring continuity and focus throughout the patient’s hospital stay. Priority status was assigned to discharge patients, expediting their documentation processes to avoid unnecessary delays. Floated beds were added as a temporary solution for delayed patient documentation. An automated alert system was introduced to notify Admission, Discharge, and Transfer (ADT) teams and staff of High Dependency Unit (HDU) transfers immediately after the order was placed. Additionally, hospital policies were revised to align with these improvements, ensuring long-term compliance and sustainability. These measures collectively reduced inefficiencies, enhanced process standardization, and ensured a more efficient and patient-centered discharge process.
Post-intervention, the compliance rates exhibited substantial and measurable improvements, significantly enhancing the early discharge planning process. The mean compliance rate increased to 89.54%, a notable improvement from the pre-intervention mean of 68.10% (p-value <0.05). This upward shift highlights that the process is now more aligned with target compliance standards, with most observations surpassing the Lower Specification Limit (LSL) of 80% (Fig. 4).
This figure compares compliance rates before and after intervention using process capability histograms. (Left: Pre-Intervention Data) shows a lower mean compliance rate with significant variability, with many values falling below the lower specification limit (LSL = 80%). (Right: Post-Intervention Data) illustrates a noticeable improvement, with most compliance rates surpassing the LSL and clustering closer to the target range. The normal distribution fits (red curves) indicate an overall shift towards higher compliance, demonstrating the effectiveness of the intervention in reducing non-compliance and improving discharge efficiency.
As Table 1 shows, the Process Potential Index, Pp, increased by 0.19, from 0.22 to 0.41, indicating the overall potential capability of the process under ideal conditions. This means variability is reduced, and it can also meet compliance requirements. The Process Performance Index, Ppk, more impressively describes how well the process mean is centered within the specification limits. The Ppk value showed a considerable increase of 0.66, starting from a negative value of -0.27, which is an indication of misalignment and, hence, poor performance, a positive value of 0.39. This shift indicates that the process mean has moved into the acceptable range, significantly reducing non-compliance.
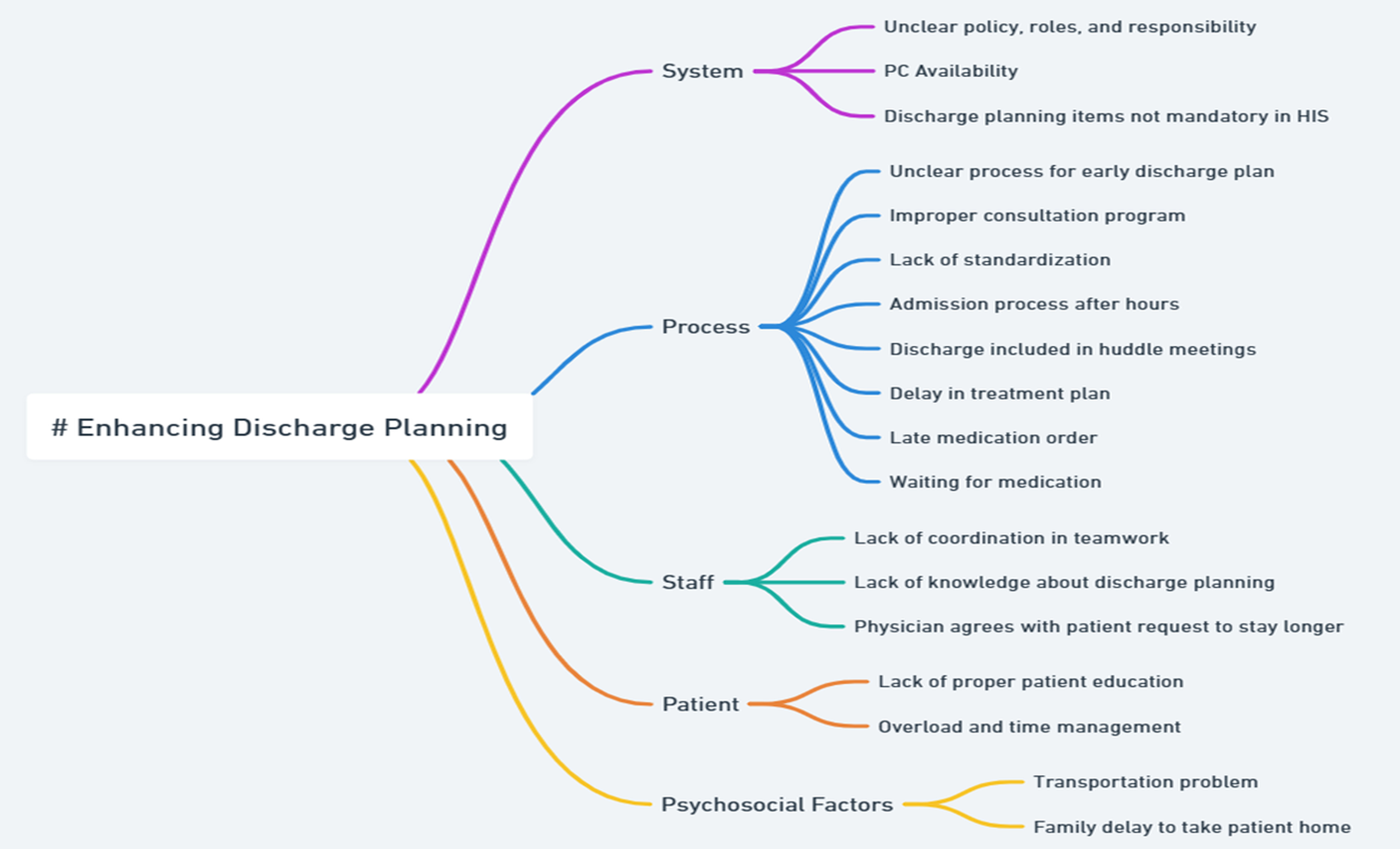
Root cause analysis for enhancing discharge planning using a mind map.
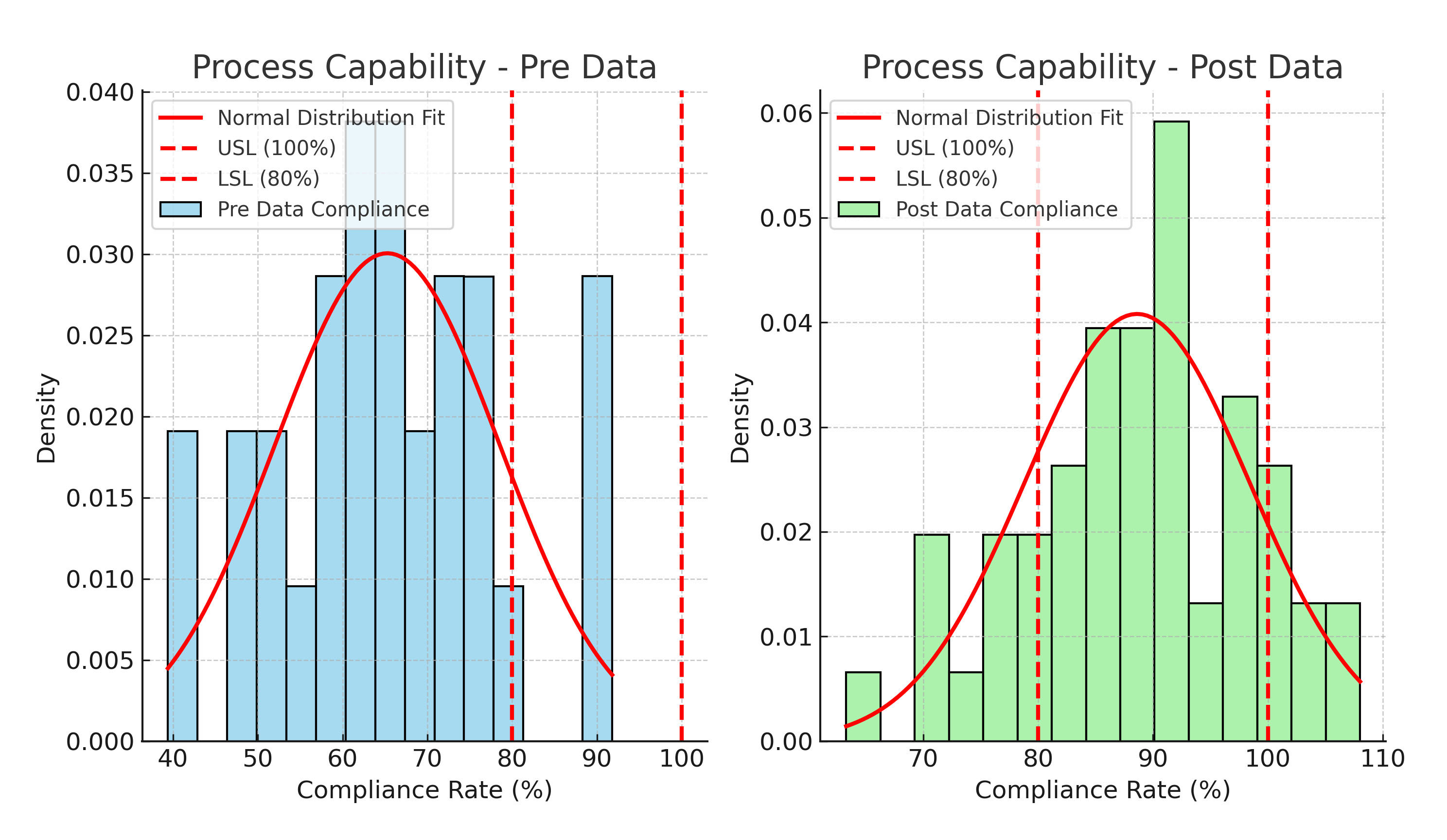
Process capability analysis for compliance with early discharge planning (pre- and post-intervention).
| Metric | Before Intervention | After Intervention | Change |
|---|---|---|---|
| Total N | 30.0 | 51.0 | - |
| Process Potential Index (Pp) | 0.22 | 0.41 | 0.19 |
| Process Performance Index (Ppk) | -0.27 | 0.39 | 0.66 |
| Z.Bench Score – Compliance Alignment (Z.Bench) | -0.8 | 1.18 | 1.98 |
| Percentage of Observations Out of Specification | 76.67 | 7.84 | -68.82 |
| Defects Per Million Opportunities (DPMO) – Process Non-Compliance | 766666.0 | 78431.0 | -688235.29 |
Process Potential Index (Pp) and Process Performance Index (Ppk) are critical for assessing process stability and capability, ensuring that discharge planning meets operational standards with minimal variability. The Z.Bench score provides insight into how well the process aligns with compliance requirements, reducing the risk of deviations that could impact patient care. The percentage of observations out of specification is crucial in measuring compliance adherence, as a decrease signifies a more reliable and efficient discharge process. Additionally, DPMO (Defects Per Million Opportunities) is a key metric for evaluating process defects, where a reduction reflects fewer inefficiencies and errors in patient discharge.
The improvements in compliance are further underscored by a sharp decline in the percentage of observations falling below the LSL. Pre-intervention, 76.67% of observations were below the LSL, reflecting significant non-compliance. Post-intervention, this figure dropped by 68.82% to only 7.84% of observations, indicating that the process now consistently meets the minimum standards. Correspondingly, the Defects Per Million Opportunities (DPMO) fell drastically, from 766,666 to 78,431, reducing 688,235 defects per million opportunities. This decline highlights a substantial improvement in process quality and reliability.
Additionally, the Z.Bench value, a measure of how far the process is from the target in standard deviation units, improved significantly by 1.98, rising from -0.80 to 1.18. This positive change demonstrates that the process is now much closer to meeting its compliance goals, with fewer deviations from the target.
The bed occupancy rate experienced a noticeable decline from 95% in June 2024 to 77% in September 2024, showing decreased center resource utilization (p value <0.05). Similarly, the average length of stay (LOS) improved overall, decreasing from 9.0 days in June 2024 to 6.5 days in September 2024 (p value <0.05).
5.5. Control
Fig. (5) illustrates the Combined IMR (Individual-Moving Range) Control Chart for pre- and post-intervention compliance with the early discharge planning process, highlighting significant improvements post-intervention. In the Individual Chart (top), the blue line represents compliance rates, with pre-intervention data points displaying lower values and more considerable variability. In contrast, post-intervention points are higher and closer to or above the 80% LSL, indicating enhanced compliance. The mean compliance rate, represented by the green dashed line, shows a shift closer to the target compliance level, reflecting overall improvement. Pre-intervention data reveal several points below the 80% LSL, underscoring inconsistent compliance that required intervention, whereas post-intervention points demonstrate more excellent stability and adherence to standards.
This control chart displays compliance rates before and after the intervention. (Top: Individual Chart) illustrates compliance rate fluctuations, with pre-intervention data showing high variability and post-intervention data demonstrating improved consistency and alignment with the lower specification limit (LSL = 80%). (Bottom: Moving Range Chart) visualizes changes in compliance rate between consecutive observations, where post-intervention data exhibit reduced fluctuations, indicating a more stable and controlled discharge planning process. The shift in mean compliance rate and reduced variability confirms the intervention's effectiveness in standardizing discharge planning and improving adherence to protocols.
The Moving Range Chart (bottom) further emphasizes these improvements, as the orange line shows reduced variability in compliance rates post-intervention. Pre-intervention variability was marked by high spikes in the moving range and several points exceeding the UCL, indicating significant fluctuations in compliance. In contrast, post-intervention moving range values are lower and more consistent, reflecting a stabilized and controlled process. These insights confirm that the implemented interventions successfully increased compliance rates, reduced variability, and improved overall control of the discharge planning process, moving the process closer to achieving consistent and reliable outcomes.
6. DISCUSSION
Integrating Lean Six Sigma (LSS) methodologies with the early discharge planning process has tackled several gaps in process inefficiencies and has proven to be a successful method that improves patient flow and enhances the overall quality of care. Current research has demonstrated decreased workflow inconsistencies and wastage, which is aligned with LSS capabilities in streamlining healthcare processes. Studies revealed some factors that successfully solved the inefficient management of the discharge process by highlighting the importance of standardizing procedures and making
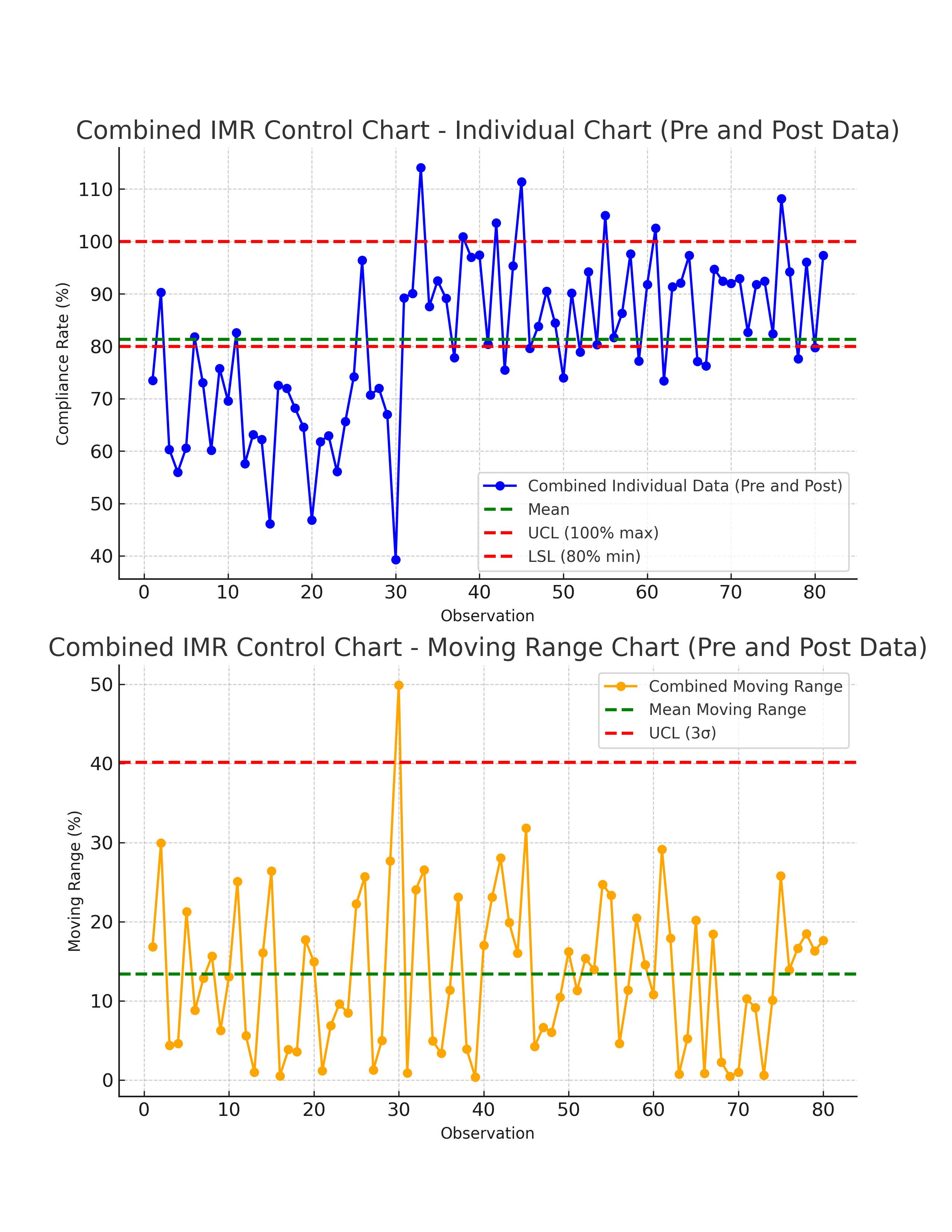
Combined IMR (Individual-Moving Range) control chart for compliance with early discharge planning (pre- and post-intervention).
interdisciplinary collaboration, which were essential components of this intervention [75-88]. Better coordination among staff, timely patient discharge support, and smoother post-hospital care transitions were keys to these improvements [20-32].
This project has another key finding targeted by the implemented interventions, such as minimizing delays and improving discharge protocol compliances, which are achieved by streamlining discharge processes and integrating discharge planner documentation in the electronic systems, reducing manual inefficiencies, resonating the results of many studies that elaborated in their Lean Six Sigma project that digital systems and clear discharge policies had a positive significance in improving the efficient workflow [33-46]. Furthermore, communication and accountability were enhanced by involving the multidisciplinary teams, which directly contributed to minimizing discharge delays and optimizing bed turnover [25, 26].
Proactive interventions such as early scheduling and engaging patients with the EDP process have improved the discharge timing and standardized the discharge process [11, 27, 28]. Rahul, Samanta, and Varaprasad (2020) demonstrated similar outcomes by presenting the outcomes of using LSS methodology that could minimize hospital congestion and enhance operational efficiency in high-demand healthcare settings. On the other hand, Lambaudie et al. (2020) revealed secondary benefits of these strategies encompassed a reduction in the likelihood of readmitting patients, resulting in incompletion of the discharge planning and streamlining with the Enhanced Recovery After Surgery (ERAS) principle.
Patient-centered interventions played a crucial role in enhancing compliance with the EDP by educating patients and their families about discharge protocols and engaging them in the early preparation for discharge has minimized delays resulting from logistical barriers that distinguished that interventions developed using LSS methodology have reduced some risks related to medication errors during hospital discharge. Focusing on patient readiness and reducing variability in discharge preparation, this project ensured a more reliable and efficient process [13, 29, 30].
Further project successful contributions are emphasized by continuously monitoring real-time feedback through tracking compliance metrics presented on dashboards, ensuring the prompt identification of deviations, and promoting continuous culture improvement [15, 29-31]. A study has demonstrated the criticality of emphasizing data-driven interventions in long-term sustainability to improve discharge planning processes.
The multidisciplinary stakeholder's engagement plays a pivotal role in achieving these outcomes by fostering shared responsibility and mutual accountability to improve communication among members and reduce silos [32-34]. Many studies show the importance of interdisciplinary teamwork in effectively implementing LSS projects in healthcare settings, especially those involving complex workflows like discharge planning [63-71].
Finally, many emphasized the value of systematic problem-solving frameworks in improving healthcare operations [25, 97-100]. This project utilized tools like the fishbone diagram to illustrate the root cause of delay in discharging patients, addressing issues such as unclear and non-standardized policies, lack of coordination, and delays in orders related to discharging patients. This project addressed root causes rather than symptoms [35-37]. Successful outcomes have included improved compliance rates with discharge protocols and reduced delays, aligning with broader goals of enhancing healthcare quality and efficiency of the process. These results underscore the transformative potential of LSS methodologies when implemented thoughtfully and strategically in high-demand environments such as oncology care. While challenges remain, the gains achieved provide a strong foundation for future improvement.
7. STUDY LIMITATION
While this study was conducted at single-institution focus, that limits the generalizability of the findings. The unique operational structure, patient demographics, and institutional policies may not fully reflect variations in discharge planning challenges across different healthcare settings, such as community hospitals, academic medical centers, or resource-limited facilities. Additionally, factors such as staffing models, electronic health record (EHR) integration, and hospital-wide quality improvement cultures may differ, affecting the scalability of the implemented interventions. However, the core principles of Lean Six Sigma—reducing process variability, enhancing compliance, and optimizing workflow efficiency—are widely applicable and can be adapted to other healthcare institutions with necessary contextual modifications. Future research should validate these findings in multi-institutional studies, incorporating diverse healthcare settings to assess the broader applicability of Lean Six Sigma in optimizing oncology discharge planning.
The absence of a control group in this pre-and post-intervention study presents a limitation in determining whether the observed improvements in compliance rates, length of stay (LOS), and bed occupancy were solely due to the Lean Six Sigma interventions. Without a control group, external factors such as policy changes, seasonal variations in patient admissions, staffing levels, or concurrent hospital-wide quality improvement initiatives could have influenced the results. This limitation affects the internal validity of the study, making it difficult to attribute causality definitively. However, the use of objective performance metrics (Cp, Cpk, Z.Bench, and DPMO) and statistical process control tools strengthens the credibility of the findings by quantifying improvements and reducing the likelihood of random variations.
Additionally, the reliance on electronic discharge systems may pose challenges in settings with limited digital infrastructure. The resource-intensive nature of Lean Six Sigma implementation, including training and staffing requirements, may also restrict its scalability in resource-constrained environments. Finally, the pre-and post-intervention design lacked a control group, which may limit the ability to attribute all observed improvements solely to the interventions.
8. IMPLICATION AND FUTURE RECOMMEN -DATIONS
Future studies should address the scalability of LSS methodologies through multi-center studies in various healthcare settings. In addition, embedding advanced predictive analytics and machine learning tools in discharge planning may further improve efficiency in the earlier identification of at-risk patients. Furthermore, developing simplified LSS frameworks for resource-poor environments will facilitate broader dissemination. The key drivers to maintaining this improvement will be regular audits, mechanisms for feedback, and training. Future research should incorporate a control group or a randomized design, comparing similar institutions or departments that did not undergo Lean Six Sigma interventions, to provide stronger causal evidence of the methodology’s effectiveness in optimizing oncology discharge planning.
Hospitals should implement standardized discharge protocols incorporating real-time tracking tools, automated alerts, and structured workflows to minimize delays. Strengthening multidisciplinary collaboration among nurses, physicians, patient flow coordinators, pharmacists, and allied health professionals through structured huddle meetings and improved communication frameworks is essential. Establishing real-time performance dashboards can facilitate continuous monitoring and feedback mechanisms, enabling proactive interventions when discharge metrics deviate from standards. Expanding Lean Six Sigma training within hospital quality improvement programs can promote data-driven decision-making and enhance process optimization. Additionally, hospital leadership should integrate Lean Six Sigma interventions into institutional policies, ensuring sustained improvements through dedicated resources, leadership involvement, and adherence incentives.
CONCLUSION
Integrating Lean Six Sigma methodologies into early discharge planning significantly improved workflow efficiency, patient outcomes, and resource utilization in an oncology setting. The implementation of data-driven interventions optimized the discharge process by identifying and addressing root causes, reducing process variability, and improving compliance with discharge protocols. Statistical analyses confirmed substantial improvements in discharge efficiency and compliance. These findings reinforce the importance of structured quality improvement initiatives in healthcare settings, providing a framework for sustained operational enhancements.
Beyond the immediate benefits, this study underscores the broader implications of Lean Six Sigma for discharge planning and oncology care. The results establish a precedent for applying data-driven quality improvement frameworks in hospital workflows, demonstrating how multidisciplinary collaboration and continuous process monitoring can drive long-term success.
The findings contribute to both theoretical and practical knowledge, reinforcing the significance of process standardization, stakeholder engagement, and strategic interventions in improving patient flow and healthcare efficiency. Future research should explore the scalability of these methods across different hospital departments and settings to validate their generalizability.
AUTHORS’ CONTRIBUTIONS
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| ADT | = Admission, Discharge, and Transfer |
| BMAT | = Bone Marrow Aspirate and Trephine |
| Cp | = Process Capability Index |
| DPMO | = Defects Per Million Opportunities |
| EDP | = Early Discharge Planning |
| ERAS | = Enhanced Recovery After Surgery |
| HDU | = High Dependency Unit |
| HIS | = Hospital Information System |
| IMR | = Individual-Moving Range |
| HIS | = Hospital Information System |
| ICU | = Intensive Care Unit |
| KPI | = Key Performance Indicator |
| LOS | = Length of Stay |
| LSL | = Lower Specification Limit |
| LSS | = Lean Six Sigma |
| PDSA | = Plan-Do-Study-Act |
| PCA | = Principal Component Analysis |
| QI | = Quality Improvement |
| SOP | = Standard Operating Procedure |
| UCL | = Upper Control Limit |
| USL | = Upper Specification Limit |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Institutional Review Board in Sultan Qaboos Comprehensive Cancer Care and Research Center, Muscat, Oman (CCCRC-01-2025 SV). Patient confidentiality was maintained throughout the project, and all interventions were designed to minimize disruption to clinical care processes. The study adhered to ethical principles, ensuring transparency and respect for all stakeholders.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the Zenodo Repository at [https://zenodo.org/records/15528716], reference number [DOI: 10.5281/zenodo.15528716].
FUNDING
This research was internally supported by the Sultan Qaboos Comprehensive Cancer Care and Research Centre (SQCCCRC)-University Medical City, Muscat, Oman.
CONFLICT OF INTEREST
Omar Ayaad is on the Editorial Advisory Board Member of the journal The Open Public Health Journal.
ACKNOWLEDGEMENTS
The authors thank the Sultan Qaboos Comprehensive Cancer Care and Research Center for their support and collaboration in this project—special thanks to the multidisciplinary team for their dedication and commitment to improving the discharge planning process. The authors also acknowledge the patient's and families' cooperation, contributing to the initiative's success.


