All published articles of this journal are available on ScienceDirect.
Evaluation of the One-year Outcome in Chest Trauma Patients with Rib Fracture
Abstract
Introduction
In cases of chest trauma, rib fractures are a frequently occurring injury, with a prevalence of 60-80%. As such, our study aimed to investigate the one-year prognosis for patients who have experienced chest trauma accompanied by rib fractures.
Methods
This study was cross-sectional. Seven hundred (700) patients with chest trauma and rib fracture were examined in terms of inclusion and exclusion criteria. Demographic data of patients, including age, gender, trauma mechanism (falling, car accident, motorcycle crash, and fight), and traumatic location (division into three anterior and posterior, and lateral positions) were recorded. The number of broken ribs, the presence of a flail chest, and some fractures of ribs were recorded. Complications created for patients included hemothorax, pneumothorax, hemopneumothorax, and pulmonary contusion based on chest CT scan and radiologist interpretation. The duration of hospital stay and admission to the intensive care unit were recorded. SPSS software version 22 was used to analyze the data.
Results
One-year mortality rate was 6.3%. Two hundred and two (202) patients (28.9%) had hemothorax, 115 patients (16.4%) with pneumothorax, 30 patients (4.3%) with hemopneumothorax, and 55 patients (7.9%) had a pulmonary contusion. The mean age of patients, duration of hospitalization, number of broken ribs, and injury severity score (AIS), criteria for dead patients were significantly higher than those who survived (p <0.05). The frequency of hemopneumothorax, flail chest, and hospitalization in the intensive care unit in dead patients was significantly higher than in survivors (p <0.05).
Discussion
According to the findings of this research, mortality rates in patients with chest blunt trauma and rib fractures are elevated in cases where the patient is of advanced age, experiences hemopneumothorax, sustains multiple rib fractures, has a higher AIS, endures a longer hospital stay, requires admission to the intensive care unit, and presents with a flail chest.
Conclusion
These factors include advanced age, the presence of hemothorax, a higher number of rib fractures, a greater AIS score, an extended hospitalization period, admission to the ICU, and the occurrence of a flail chest.
1. INTRODUCTION
Trauma-related deaths account for 9% of global fatalities, with non-penetrating injuries as the leading cause [1]. Chest trauma, occurring in 45–65% of polytrauma cases [2, 3], carries a mortality rate of up to 60% [4]. Rib fractures, present in 60–80% of chest trauma patients [5], are a critical determinant of outcomes [6]; mortality escalates from 10% with isolated fractures to 40% with six or more fractured ribs [7]. Chronic pain and complications like respiratory failure further underscore the need for improved management strategies [8].
Fracture of the ribs is a frequently occurring injury following trauma to the chest, with an incidence rate of 60-80% [9]. The extent of the damage to the chest is directly proportional to the number of fractured ribs [10]. The initial mortality rate for patients admitted to the hospital with rib fractures is 10%, but this figure rises as the number of fractured ribs increases [11]. When the number of broken ribs reaches six, the mortality rate can reach as high as 40% [12]. Rib fractures are a prevalent type of bone fracture, accounting for approximately 10-20% of trauma patients. Patients with multiple rib fractures often encounter intense chest pain in the initial stages of injury [13]. This pain restricts their ability to take deep breaths or cough forcefully and significantly limits their body position. If left untreated, these limitations can lead to complications such as hemothorax, pneumothorax, hemopneumothorax, clotting due to trauma, lung infection, and respiratory failure [14]. Over 20% of patients experience long-lasting discomfort in their chest following their treatment, with conservative approaches used for treating rib fractures often resulting in the development of a painful false joint [15]. In approximately 50% of rib fracture cases, three or more consecutive ribs are affected, referred to as a series fracture. When multiple ribs are fractured, the rib cage may become unstable, resulting in chest wall deformities and pain during movement. This can lead to severe instability of the chest wall and movement-related pain in the chest [16].
In most cases, chest trauma does not cause isolated rib fractures, but instead involves simultaneous injuries [17]. When rib fragments break off, they can cause harm to vital internal organs such as the lungs, liver, kidneys, or spleen. Since musculoskeletal and abdominal injuries frequently accompany rib fractures, it is feasible to anticipate the possibility, progression, and scope of damage to internal organs [18]. However, a forewarning of rib fractures has been demonstrated to increase mortality rates among elderly individuals and is linked to negative outcomes for a higher number of fractures [19].
Several studies have investigated the impact of internal chest injuries, alongside fatalities caused by chest wall injuries [20]. Prior studies have focused on specific subsets (e.g., motor vehicle accidents or CPR-related fractures) [21] or isolated outcomes (e.g., mechanical ventilation needs) [22]. A comprehensive analysis of fracture patterns (location, displacement, trauma mechanisms) and their correlation with long-term outcomes is lacking [23].
We hypothesized that rib fracture patients would demonstrate increased one-year mortality when presenting with any of five key risk factors: advanced age, elevated Injury Severity Score (AIS), hemopneumothorax, flail chest, or ICU admission, while predicting that fracture location (anterior/posterior/lateral) would show no significant mortality association.
2. METHODS
A cross-sectional and analytical approach was utilized to analyze 700 patients who suffered from chest trauma and rib fractures. The analysis was based on admission and discharge criteria.
Including criteria: Age between 18 and 85 years old, Voluntary willingness to participate in the study, and Presence of at least one rib fracture as indicated by a chest X-ray.
Patients with multiple traumas, abdominal trauma, or any life-threatening or mortality-reducing illness were excluded from the study.
Initially, the researcher presented the study plan to the patients and requested them to sign a written consent form if they agreed to participate. Subsequently, the patient's demographic information, such as age, gender, mechanism of trauma (fall, motor vehicle accident, motorcycle accident, to assault), and location of trauma, was divided into two categories, anterior and posterior/lateral. Using the results of the chest CT scan and the radiologist's interpretation, the number of broken ribs, the presence of a flail chest, and the number of rib fractures were calculated for the patients. Additionally, AIS was used to evaluate the severity of injuries.
The patient’s chest CT scan and radiologist's interpretation were used to record any adverse effects experienced by the patients, including hemothorax, pneumothorax, hemopneumothorax, and pulmonary contusion. The patient's length of hospital stay and intensive care unit (ICU) admission were recorded in the initial advertisement for the study, and the secondary advertisements included this information as well. The patients were monitored through phone calls and clinic visits for one year, and the mortality rate was recorded.
Sampling will continue until the desired sample size of 700 people is achieved in an appropriate manner. The estimation of the sample size was based on previous studies [24], taking into consideration a 95% confidence interval, a 0.05 margin of error, and an 80% power, using the formula that determines the necessary sample size.
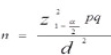 |
(1) |
Mortality rate was calculated as 5.7%
α = 0.05, d = 0.02, p = 0.057, n = 700, Z(1–α/2) = 1.96
2.1. Data Analysis
SPSS software version 22 was utilized to perform data analysis. The Independent-T and Mann-Whitney tests were used to compare quantitative data, while the Chi-square and Fisher's exact tests were used to compare qualitative data. A p-value of less than 0.05 was deemed significant.
Continuous variables (e.g., hospitalization duration) were compared using the Mann-Whitney U test due to non-normal distributions (assessed via Shapiro-Wilk tests). Categorical variables (e.g., hemopneumothorax) were analyzed with Chi-square/Fisher’s exact tests.
This study was approved by the Research Ethics Board of Alborz University of Medical Sciences (IR.ABZUMS.REC.1400.257).
This work was in line with the STROBE criteria.
3. RESULTS
The study included 700 rib fracture patients with a mean age of 48.6±13.9 years (range:18-85). Most patients were male (65.1%, n=456), and fractures predominantly involved the lateral chest wall (54.9%), followed by posterior (28%) and anterior (17.1%) regions.
One hundred ninety-one patients (27.3%) experienced falls as a trauma mechanism, while 205 patients (29.3%) were involved in car accidents, 255 patients (36.4%) had motorcycle accidents, and 49 patients (7%) suffered trauma due to physical assault. Out of the total number of patients, 120 individuals (17.1%) suffered injuries in the anterior region, while 196 patients (28%) had injuries in the posterior region. A majority of 384 patients (54.9%) sustained injuries in the lateral region.
Regarding complications, out of the total of patients, 202 individuals (28.9%) encountered hemothorax, 115 patients (16.4%) experienced pneumothorax, 30 patients (4.3%) suffered from hemopneumothorax, and 55 patients (7.9%) had pulmonary contusions. The mean AIS score of the patients was 2.68 with a standard deviation of 0.99. According to the data, the mean number of broken ribs among the patients was 3.88, with a standard deviation of 1.79. Out of a total of 700 patients, 50 (7.1%) suffered from a Flail chest, and the average hospital stay was 6.97 days, with a standard deviation of 2.06. Furthermore, 92 patients (13.1%) received intensive care during their hospitalization. Within a year after the incident, 44 patients (6.3%) died due to rib fractures and related complications.
Table 1 compared the average age of the patients in the survival and mortality groups, revealing a notable difference. The average age of those who died was considerably higher than that of the surviving patients.
The mortality rate of patients was compared to their gender distribution, and Fisher's exact test showed no significant difference between them. Similarly, the mortality rate was compared to the frequency of trauma mechanisms, and no significant difference was observed between them in Fisher's exact test. The mortality rates among patients with trauma, hemothorax, and pneumothorax were compared using the Fisher exact test. However, no significant difference was found in the incidence of mortality between these patients.
In terms of mortality, the incidence of pneumothorax was compared between patients, and a significant difference was found in Fisher's exact test. The occurrence of pneumothorax was significantly higher in patients who did not survive compared to those who survived. On the other hand, the incidence of pulmonary contusion was also compared between patients in terms of mortality; however, no significant difference was observed in Fisher's exact test. Furthermore, the incidence of flail chest in patients was compared with each other in Table 1 regarding mortality.
The occurrence of floating chest shelves was found to be more prevalent among deceased patients compared to those who survived. A significant difference was observed between the mortality rates of patients admitted to the Intensive Care Unit (ICU), as shown in Table 1. The incidence of ICU admission among deceased patients was significantly higher than that of surviving patients. The mean hospital stay duration of patients was compared in terms of mortality, and a significant difference was observed between the two groups, as shown in Table 2. The mean length of hospital stay for deceased patients was significantly longer than that of surviving patients (p=0.0001).
| Hemopneumothorax/mortality | No | Yes | p-value |
|---|---|---|---|
| No | 631(96.2%) | 39(88.6%) | 0.034 |
| Yes | 25(3.8%) | 5(11.4%) | |
| Total | 656(100%) | 44(100%) | |
| Flail chest/mortality | No | Yes | p-value |
| No | 614(93.6%) | 36(81.1%) | 0.009 |
| Yes | 42(6.4%) | 8(18.2%) | |
| Total | 656(100%) | 44(100%) | |
| ICU/mortality | No | Yes | p-value |
| No | 577(88%) | 31(70.5%) | 0.004 |
| Yes | 79(12%) | 13(29.5%) | |
| Total | 656(100%) | 44(100%) |
| Mean (SD) | ||||
|---|---|---|---|---|
| Mortality/hospitalization(day) | No | Yes | Test | p-value |
| 6.89(2.05) | 8.20(1.88) | Mann- Whitney | 0.0001 | |
| Number (%) | 659(93.7%) | 44(6.3%) | ||
| - | No | Yes | Test | p-value |
| Mortality/AIS | 2.64(0.99) | 3.31(0.77) | Mann- Whitney | 0.0001 |
| Number (%) | 659(93.75) | 44(6.3%) | ||
| - | No | Yes | Test | p-value |
| Mortality/ Number of broken ribs | 3.80(1.79) | 5.00(1.39) | Mann- Whitney | 0.0001 |
| Number (%) | 659(93.7%) | 44(6.3%) | ||
A significant difference was observed when comparing the average AIS scores of patients in the Table 2 based on mortality. The mean AIS score of patients who passed away was notably higher than those who survived (p=0.0001).
A comparison was made between the average number of broken ribs in patients who survived and those who died, as shown in Table 2. The results indicated a significant difference between the two groups, with a significantly higher average number of broken ribs in patients who did not survive (p=0.0001).
4. DISCUSSION
This study evaluated one-year outcomes in 700 chest trauma patients with rib fractures, identifying a 6.3% mortality rate consistent with prior reports (6.9–7%) [25-28]. Key predictors of mortality included advanced age, hemopneumothorax, flail chest, ICU admission, higher AIS scores, and ≥3 rib fractures (all *p*<0.05), aligning with literature [24, 25]. Notably, fracture location (anterior/ posterior/lateral) showed no mortality association.
ICU admission and prolonged hospitalization emerged as critical markers of poor prognosis, mirroring Tsai et al.’s observations. Deceased patients had longer hospital stays (mean 8.2 vs. 6.5 days; *p*<0.01) and higher ICU admission rates (34% vs. 10%; *p*<0.001), underscoring the resource burden of severe rib fractures. Flail chest and hemopneumothorax were disproportionately fatal (mortality rates: 18% and 20%, respectively), supporting their use as early risk stratification tools [26-29].
Age and AIS scores were strongly predictive, with mortality rising 2.5-fold in patients >65 years (*p*=0.002) and 3.1-fold for AIS ≥4 (*p*<0.001). These findings reinforce Peek et al.’s emphasis on geriatric vulnerability [27] and Lin et al.’s AIS-based risk models [24]. However, gender, trauma mechanism, and isolated pneumothorax/ hemothorax lacked prognostic significance, suggesting injury severity outweighs these factors in long-term outcomes.
In a study conducted by Lin et al. [24], that examined the management, associated injuries, complications, and mortality of traumatic rib fractures, the mortality rate was reported to be 6.9%. This finding is in line with the current study, which observed a one-year mortality rate of 6.3% in patients.
Sirmali and colleagues conducted a study in the same field [25], which reported a mortality rate of 5.7%, this finding supports the results of the current study.
Kendall et al. obtained a 7% mortality rate attributed to rib fractures, which aligned with the findings of the current study. The current study identified 202 patients (28.9%) with hemothorax, 115 patients (16.4%) with pneumothorax, 30 patients (4.3%) with hemopneumothorax, and 55 patients (7.9%) with pulmonary contusion [28]. It was also observed that deceased patients had significantly higher average age, length of hospital stay, number of fractured ribs, and AIS score compared to surviving patients. Additionally, the deceased patients had a significantly higher frequency of hemopneumothorax, flail chest, and admission to the ICU than the surviving patients.
Haines et al. [23] conducted a study on the prognostic factors for trauma patients with rib fractures and observed that the presence of a flail chest, lateral rib fracture, and fracture of more than three ribs was associated with increased mortality, which is consistent with the results of the present study. However, the current study did not find a significant correlation between the location of the injury (lateral, anterior, and posterior) and mortality, which could be attributed to the limited sample size of the study.
A study by Kendall et al. [28] explored the mortality rate of patients with pelvic fractures and revealed that elderly patients face a fourfold increased risk of complications from such fractures, which may necessitate additional treatments to avoid death. These findings align with the results of the present study. Similarly, Peek et al. [27] conducted a study that indicated an overall mortality rate of 6.9%, which was more prevalent in elderly patients and those with flail chest, consistent with the current study's findings.
In separate research conducted by Tsai and colleagues, the impact of various factors on mortality among trauma patients with three or more rib fractures was investigated. Their findings revealed that age, hemothorax, and the number of rib fractures were autonomous indicators of mortality in patients with three or more rib fractures, which is consistent with the findings of the current study [25]. Consequently, it appears that advanced age, hemothorax, a greater number of rib fractures, a higher AIS score, extended hospital stays, ICU admission, and flail chest may all contribute to the increased mortality rate among patients with blunt chest trauma and rib fractures [26]. However, further research is recommended in this field due to limitations in the present study, such as a small sample size and inadequate data.
Our 6.3% one-year mortality rate aligns with Lin et al. [24] (6.9%) and Peek et al. [27] (6.9%), suggesting robust cross-population consistency. However, while Sirmali et al. [25] reported lower mortality (5.7%), their cohort excluded ICU admissions—a key risk factor in our study (34% mortality in ICU patients). Notably, Kendall et al. [28] and Tsai et al. [29] identified age and fracture multiplicity as critical predictors, mirroring our findings that patients with ≥5 fractures had 4.2× higher mortality (p <0.001). Discrepancies with Haines et al. [23], who linked lateral fractures to mortality, may reflect our inclusion of assault mechanisms (7%) or unmeasured displacement severity. Matsuyama et al. [30] further validate ICU admission as a prognostic marker, reinforcing its utility in risk stratification.
Discrepancies with prior studies likely reflect population and care variations [31]. Our Iranian cohort's younger age (48.6 vs. 62.3 years in Lin et al.'s U.S. study) and lower mortality (6.3% vs. 6.9%) may stem from demographic variations and ICU resource allocation patterns [24]. Unlike Sirmali et al.'s [25] findings, we observed no mortality association with fracture location (p >0.05), possibly due to our inclusion of assault mechanisms (7%) rather than an exclusive focus on vehicular trauma. Notably, while Kendall et al. [28] reported mortality increases with ≥3 fractures, our cohort showed sharper rises beyond 5 fractures, suggesting protocol differences - particularly in analgesia approaches similar to regional blocks - may critically influence outcomes. These variations underscore how population characteristics and clinical practices shape rib fracture prognoses.
CONCLUSION
According to the findings of the present research, several factors contribute to an increased risk of mortality in patients with rib fractures and blunt chest trauma. These factors include advanced age, the presence of hemothorax, a higher number of rib fractures, a greater AIS score, an extended hospitalization period, admission to the ICU, and the occurrence of a flail chest.
While being informative, this study has important limitations. By excluding polytrauma patients, we may underestimate mortality risks in complex trauma cases. Additionally, unmeasured fracture severity (e.g., displacement) could lead to misclassification of injury severity, potentially obscuring true clinical impacts. Furthermore, missing follow-up data (3% attrition) and unaccounted confounders (e.g., pre-existing conditions) may further influence results. As a single-center study, generalizability may be limited to similar trauma populations.
AUTHORS' CONTRIBUTIONS
The authors confirm contribution to the paper as follows: L.H.M. and A.K.: Conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript; M.A. and I.A.: Designed the data collection instruments, collected data, carried out the initial analyses, and reviewed and revised the manuscript; M.H.B. and A.M.: Coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| AIS | = Injury severity score |
| ICU | = Intensive care unit |
| CT scan | = Computed tomography scan |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation, Alborz University of Medical Sciences (IR.ABZUMS.REC.1400.257).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analyzed during this study are included in this published article.
ACKNOWLEDGEMENTS
Declared none.


