All published articles of this journal are available on ScienceDirect.
The Prevalence of Advanced HIV Disease Among Adults Initiated on ART in the Western Oromia Region of Ethiopia
Abstract
Background
According to the World Health Organization, the rising number of individuals with HIV experiencing Advanced HIV Disease (AHD) poses a significant challenge to preventing new infections, complications, and HIV-related mortality despite the implementation of the test-and-treat approach. Ethiopia lacks empirical data on AHD, highlighting the need for further investigation. Therefore, this study aimed to assess the prevalence of AHD among adults initiating Anti reteroviral therapy (ART) to inform policy decisions and clinical practice.
Methods
A retrospective cross-sectional study was conducted in three high-volume public health hospitals using a systematic sampling technique. The Raosoft sample calculator was used to select a total sample of 544 patient records that met the inclusion criteria. A document review was conducted to examine the medical records of patients spanning from January 2017 to December 2021 by trained data collectors using a structured checklist.
Results
Study findings indicated an increasing AHD prevalence of 41.7% with 95% CI (37.5 - 46.0) over five years, especially prominent in the 35-44 age group (38.7%) and among males (51.5%). Controversially, a higher mortality rate was observed in non-AHD patients compared to those with AHD, warranting further investigation.
Conclusion
The high prevalence of AHD, particularly among men and middle-aged adults on ART in public hospitals, requires policymakers to develop targeted aged and gender interventions, community awareness, and education at both facility and community levels about the importance of early HIV diagnosis and treatment and adherence to reduce complications and preventable deaths related to AHD, including building the capacity of HCPs to comply with guidelines in healthcare practice.
1. BACKGROUND/INTRODUCTION
According to the World Health Organization (WHO), advanced HIV disease (AHD) is the stage of HIV infection in which the immune system is severely compromised, indicated by a low CD4 cell count below 200 cells/mm3 or the presence of certain opportunistic infections (OIs) or cancers [1]. These conditions are often referred to as acquired immune deficiency syndrome (AIDS)-defining illnesses. Advanced HIV disease is still a global public health concern threatening the health outcomes and prognosis of people living with HIV (PLHIV) despite the recommendations of WHO to provide a package of interventions, including screening, treatment, prophylaxis for major OIs, rapid ART initiation regardless of clinical staging and CD4 cell count, intensified adherence support, and key medicines and diagnostics for managing common causes of illness [2, 3]. Moreover, in more than 135 countries, ART has already been scaled up in response to the ‘test and treat’ recommendation, and treatment monitoring has become more accessible. However, AHD remains the leading cause of mortality among adults living with HIV (ALHIV) worldwide [3, 4]. About 4 million adults are living with AHD, with approximately 650,000 fatalities worldwide [5]. Providing targeted interventions that increase access to early diagnosis and ART service to these groups is vital to preventing and treating AHD.
The proportion of people suffering from AHD did not change in the last five years in low and middle-income countries (LMICs), while 30.7 million PLHIV had access to ART in 2023 globally [6-8]. Individuals with AHD are more vulnerable to OIs and require specific interventions [9-11]. Various efforts have been implemented to prevent AHD and new HIV transmissions in both developing and developed countries to end HIV by 2030. However, this remains a challenge, particularly in sub-Saharan Africa.
A study conducted in Latin America demonstrated that 56% of patients presented with AHD, which accounted for most deaths among PLHIV and was primarily caused by late presentation, with a lesser contribution from delays in ART initiation [12]. Late presentation with AHD also increases the public health burden [13], as it heightens the risk of community transmission and raises healthcare costs [14]. Enhancing early presentation and timely ART initiation can reduce HIV/AIDS-related burdens, which are preventable and manageable. According to studies, it has been reported that an increase of 71% of HIV-positive people beginning ART in LMIC had CD4 cell counts below 200 cells/mm3 or WHO stage III or IV [3, 9-11]. The distribution of AHD in South Africa (9.7%), Kenya (11.8%), and Malawi (7.8%), based on three population-based cross-sectional surveys, indicated that 37.3% of participants presenting with AHD were unaware of their HIV status [15], highlighting the need for further investigations. Patients with AHD have significantly worse clinical outcomes with higher recorded mortality compared to those presenting at an earlier stage or non-AHD [16, 17]. Emphasising the implementation of the AHD care package is key to improving the health and treatment outcomes of patients presenting with AHD at health facilities.
In Ethiopia, limited information is available about the occurrence of AHD as there are a limited number of studies and evidence-based solutions among PLHIV generated to give immediate responses to the effect of AHD [18, 19]. Although the country has adopted WHO recommendations and developed national guidelines for implementing the AHD care package [20], this issue persists and requires urgent attention. Strategies to reduce the burden of AHD among adults in Ethiopia should be patient-centered and address identified gaps in both men and women. Therefore, the researchers conducted this study to determine the prevalence of AHD among adults initiating ART in public hospitals in West Oromia, Ethiopia, to guide policymakers in developing targeted strategies for preventing and managing AHD.
2. MATERIAL AND METHODS
2.1. Study Design and Setting
A facility-based retrospective cross-sectional study design was conducted to determine the prevalence of AHD among adults initiated on ART in this study. This design allows researchers to efficiently analyse the existing data to investigate associations between variables at a specific point in time, providing valuable insights into potential relationships [21]. It also provided quantitative descriptive percentages key to generating sufficient evidence regarding the prevalence of AHD that would be used to develop initiatives to improve the identification and management of AHD.
The study was conducted in three purposively selected tertiary-level public hospitals in the western part of the Oromia Region in Ethiopia, including Ambo General Hospital, Nekemte Specialised Hospital, and Shambu General Hospital, which are in the Ambo Town, Nekemte Town, and Shambu Town respectively. These facilities were selected because they had a high HIV risk and burden of a caseload of PLHIV on ART requiring routine HIV care. For each patient who started ART, all demographic and clinical information was recorded in HIV care and treatment registers and stored in the electronic medical record (EMR) for ART software. Patients who initiated ART between January 2017 and December 2021 were included in the study.
2.2. Study Population and Sample Size
In this study, the research population included all adult males and females aged 18 years and above who were initiated on ART between January 2017 and December 2021 in the three selected public hospitals. Their clinical and psychosocial support related to HIV care was documented in their medical records, including baseline CD4 cell count and WHO stages I, II, III, and IV, for inclusion in this study review. Moreover, the date of HIV diagnosis and ART initiation was also recorded. Children under 18 years old and patients without a documented date of HIV diagnosis, ART initiation, baseline CD4 count, or WHO staging were excluded. Additionally, patients recorded in ART registers between January 2017 and December 2021 as pregnant women, those transferred out in less than 12 months, and those transferred in were excluded from this study. The sample size was determined using the Roasoft sample estimation formula. Adults who initiated ART were calculated using the following assumptions: a 95% confidence level (CI), a 5% margin of error, a p-value of <0.05, and an expected AHD proportion of 40.1%. In addition, this was calculated based on a study conducted in China that estimated the number of adults who initiated ART [22]. A total sample size of 544 participants was involved in the study, accounting for a 1.5% allowance for expected limitations regarding missing data from medical records at baseline in the three selected public hospitals of western Oromia within the period of the study. The Proportion allocations were assigned as follows: Ambo General Hospital (205), Nekemte Comprehensive and Specialized Hospital (254), and Shambu General Hospital (85) in western Oromia, based on caseloads during the study period.
2.3. Sampling Methods
A systematic sampling technique was used to select adults who were newly diagnosed and initiated on ART to determine the prevalence of AHD and assess health and treatment outcomes at 12 months. This method was chosen as it is more suitable for extracting data from medical records to represent the study population. All adults initiated on ART were allocated a unique ART number (UAN) after they were diagnosed. All eligible patients were listed and retrieved from the EMR ART and were part of the sampling frame. The UAN is a standardised number given to all clients in the facilities based on the guidelines of Ethiopia. Then, the sampling frame was formed, the Kth value was calculated, and the required sample sizes of 544 were pooled up using systematic sampling from medical records in the three selected public hospitals in western Oromia [23].
2.4. Data Collection Methods
A retrospective document review was followed to collect data from the medical records of participants using a structured checklist of information that was used to determine the prevalence of AHD among adults initiated on ART. Furthermore, a structured checklist was adapted from literature, Ethiopia Demographic and Health Survey (EDHS) 2016, and WHO AHD toolkits [24]. The proportion of AHD, sociodemographics, clinical characteristics, and patient outcome information at 12 months from adults initiating ART were extracted by two experienced data collection supervisors with a Master's in Public Health (MPH) and three trained data collectors with a Bachelor of Science (BSc) in Nursing, each having 2 years of experience in clinical document review. These data were collected during the study period from February to April 2024 and were prepared in English. Each data collector was paired with an experienced supervisor.
Primarily, ART registers, ART follow-up forms, and intake A and intake B forms of participants were used to review baseline sociodemographics, clinical services, and patient outcomes at 12 months initiating ART who participated in the study.
2.5. Data Management and Analysis
Intensive training was given to data collectors on how to extract data from medical records for three consecutive days. During data collection, personally identifiable information or names of ALHIV who were initiated on ART were not included. Numbers were used during data collection from medical records to keep the information obtained confidential and aimed at determining the prevalence of AHD among adults initiated on ART. Data collection supervisors ensured that data were complete and consistent daily during data collection time. During data collection, data collectors were supervised by the supervisor and received daily feedback from the researcher to ensure consistency in the study. After data collection, the completeness and consistency of the data were checked using Microsoft Excel checklists. The data were entered and cleaned using EpiData version 4.6.0.6 software, and descriptive data analysis was performed using the SPSS version 29 software. The prevalence of AHD and patient treatment outcomes were then presented in tables and figures indicating the mean, percentage, and median. The odds ratio was calculated, and a P-value of less than 0.05 was considered statistically significant [25].
2.6. Validity and Reliability to Ensure the Rigour of Quantitative Studies
Validity is concerned with the accuracy and truthfulness of scientific findings related to inferences about the effect of the independent variable on the dependent variable. Reliability refers to the consistency, stability, and repeatability of information obtained, with no changes occurring in similar results to measure variables [26].
For this research study, validity was achieved by selecting high-quality data from a reliable health system and ensuring data collection was performed by clinically experienced data collectors, who are nurses. This approach ensured that accurate data were consistently collected, facilitating the process of reaching sound, quality conclusions that effectively represent empirical reality.
A structured checklist was tested at a nearby public hospital, not included in the main study, to determine if the tool could yield similar results and ensure data consistency. The data were collected from existing reliable sources, and measures were taken to ensure stability [25].
2.7. Ethical Considerations
The approval to conduct the study was first obtained from the University of South Africa College of Human Sciences Research Ethics Committee (CREC): reference number: 19946546_CREC _CHS_2023 on 23 November 2023. Additionally, an ethical clearance was also obtained from Oromia Health Bureau with the reference number BFO/UBTFU/1-16/912 on 11 November 2023, and permission was obtained from hospital managers to review patient records from hospital managers. During data extraction, personally identifiable information about ALHIV, who were initiated on ART as well as the names of the hospitals, were not included to keep the information confidential and anonymous.
The study was carried out in compliance with ethical standards for research involving human participants, adhering to both institutional and national policies, as well as the ethical principles outlined in the Helsinki Declaration of 1975, as revised in 2013.
3. RESULTS
Study findings indicated an increasing AHD prevalence of 41.7% with 95% CI (37.5 - 46.0) over five years, especially prominent in the 35-44 age group (38.7%) and among males (51.5%). Controversially, a higher mortality rate was observed in non-AHD patients compared to those with AHD, warranting further investigation.
3.1. Characteristics of Study Participants
The socio-demographic characteristics of the patients were obtained from the medical records that met the inclusion criteria and were analysed, as they provided the context for interpreting the results and enabling analysis of specific subgroups, revealing potential differences in study results, including factors, such as age, sex, place of residence, religion, marital, education status, and occupation status as summarized in Table 1. The majority of participants who initiated ART between 2017 and 2021 were in the 35–44 age group, accounting for 199 (36.6%), while the lowest proportion was in the ≥55 age group, with 25 (4.6%) cases. The mean and median ages of the adults participating in the study were 35.5 and 35 years, respectively, with a standard deviation of 9.6 years.
The study found that females constituted the highest proportion of participants, with 307 (56.4%), compared to males, who accounted for 237 (43.6%). The majority of participants, 358 (65.8%), resided in urban areas, while 186 (34.2%) lived in rural areas. Regarding religion, the largest group was Protestants, comprising 257 (47.2%) of participants, compared to other religious affiliations. In terms of education, the highest proportion of participants had only primary education, accounting for 192 (35.3%), while 147 (27%) had no formal education, which may be linked to inadequate health literacy regarding treatment and adherence. This was followed by secondary education (138, 25.4%) and tertiary education (67, 12.3%). The marital status analysis showed that the majority of participants were married (345, 63.4%), followed by divorced (85, 15.6%), single (65, 11.9%), and widowed (49, 9%). Additionally, 177 (32.5%) of the participants were unemployed.
3.2. Prevalence of AHD
The study results revealed that 174 (32%) of adults who initiated ART were categorized as WHO stage III or IV. Additionally, 127 (23.3%) of participants had a CD4 cell count of <200 cells/mm3. A total of 74 (32.5%) participants met the criteria for AHD based on WHO stages III and IV and a CD4 cell count of <200 cells/mm3 at ART initiation.
Overall, the prevalence of AHD was 227 (41.7%) with a 95% CI (37.5–46.0) at the time of enrollment in care among adults who started ART during the five-year study period, as summarized in Fig. (1). As shown in Fig. (2), the prevalence of AHD by sex declined in 2019 but began increasing in 2020 and 2021, highlighting the need for action. Furthermore, as indicated in Fig. (3), AHD prevalence among the 18–24 age group decreased in 2019 and 2020 but started rising again in 2021 compared to other age groups.
Despite a decrease between 2017 and 2019, the occurrence of AHD has increased from 2020 to 2021 in both sexes, prompting notable concerns and underlining the necessity for immediate interventions, as outlined in Fig. (2).
| Characteristics | Frequency | Percent (%) |
|---|---|---|
| Age (n=544) | - | - |
| 18-24 | 53 | 9.7 |
| 25-34 | 184 | 33.8 |
| 35-44 | 199 | 36.6 |
| 45-54 | 83 | 15.3 |
| >=55 | 25 | 4.6 |
| Sex (n=544) | - | - |
| Female | 307 | 56.4 |
| Male | 237 | 43.6 |
| Residence (n=544) | - | - |
| Urban | 358 | 65.8 |
| Rural | 186 | 34.2 |
| Religion (n=544) | - | - |
| Protestant | 257 | 47.2 |
| Orthodox | 250 | 46 |
| Muslim | 29 | 5.3 |
| Catholic | 4 | 0.7 |
| Others | 4 | 0.7 |
| Education level (n=544) | - | - |
| No education | 147 | 27 |
| Primary education | 192 | 35.3 |
| Secondary education | 138 | 25.4 |
| Tertiary education | 67 | 12.3 |
| Marital status(n=544) | - | - |
| Single | 65 | 11.9 |
| Married | 345 | 63.4 |
| Divorced | 85 | 15.6 |
| Widowed | 49 | 9.1 |
| Occupation status (n=544) | - | - |
| Unemployed | 177 | 32.5 |
| Farmer | 107 | 19.7 |
| Daily laborer | 72 | 13.2 |
| Government employees | 66 | 12.1 |
| Merchant | 53 | 9.7 |
| Drivers | 14 | 2.6 |
| Non-government employees | 4 | 0.7 |
| Others | 51 | 9.4 |
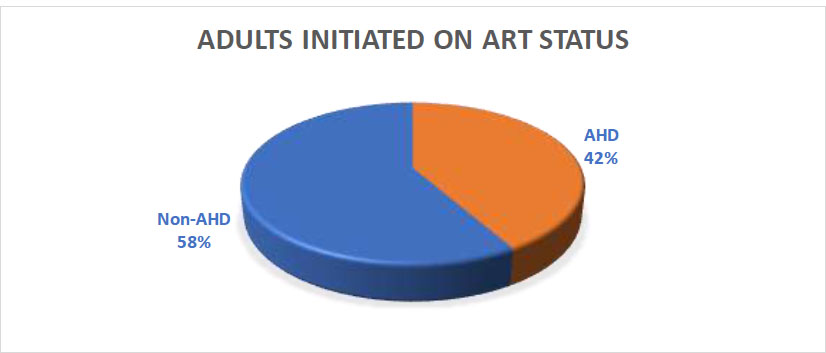
Percentage of AHD among adults who were initiated on ART from 2017-2021 (n=227).
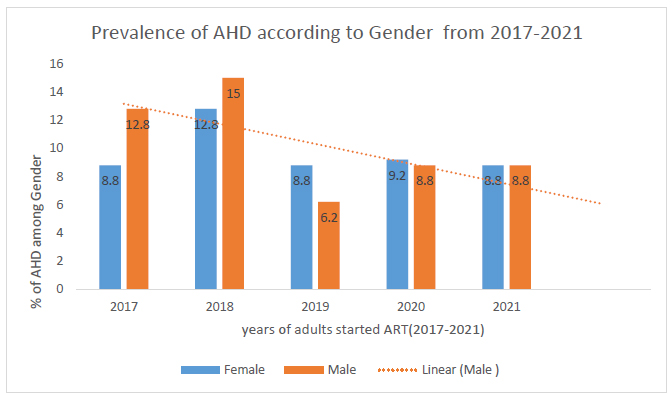
Percentage of AHD among sex category of adults initiated on ART from 2017-2021 (n=227).
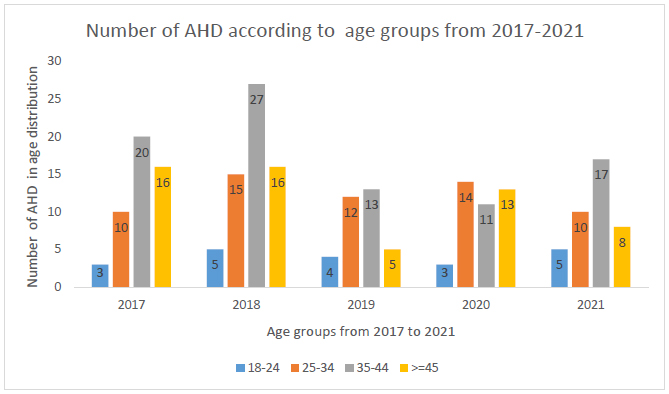
Number of AHD among age group distributions of adults initiated on ART from 2017-2021 (n=227).
Furthermore, there is a significantly higher incidence of AHD within the 35-44 age group, despite the implementation of the test and treat strategy in this region, highlighting the need for targeted interventions, as illustrated in Fig. (3).
3.3. Clinical Characteristics of the Study Participants with AHD
As depicted in Table 2, the majority of study participants, 348 (64%), underwent CD4 cell count testing at the initiation of ART. However, 196 (36%) did not, raising concerns about why healthcare providers (HCPs) missed these patients, as this indicates severe immunosuppression at enrollment in HIV care and treatment, requiring specialized care. A total of 271 (49.8%) participants were categorized as WHO Stage I, followed by 151 (27.8%) in WHO Stage III, 99 (18.2%) in WHO Stage II, and 23 (4.2%) in WHO Stage IV. Additionally, 401 (73.7%) of participants initiated ART within seven days of HIV diagnosis, while 143 (26.3%) experienced late ART initiation. This raises concerns about delays in seeking treatment or initiation by HCPs. The late initiation of ART among PLHIV with AHD remains a critical issue that requires urgent attention.
| Characteristics | AHD Status (%) | - | |
|---|---|---|---|
| - | Non-AHD (n=317) |
AHD (n=227) |
Total (%) (n=544) |
| CD4 cell count at enrollment(cells/mm3) (n=544) | - | - | - |
| Yes | 185(58.4) | 163(71.8) | 348(64.0) |
| No | 132(41.6) | 64(28.2) | 196(36.0) |
| CD4 cell count result (n=348) | - | - | - |
| <=200 cells/mm3 | 0 | 127(78) | 127(36.5) |
| 200.01-350 cells/mm3 | 69(37.3) | 14(8.6) | 83(23.8) |
| >350.01 cell/mm3 | 116(62.7) | 22(13.4) | 138(39.6) |
| WHO Clinical staging at enrolment(n=544) | - | - | - |
| I | 240(75.7) | 31(13.7) | 271(49.8) |
| II | 77(24.5) | 22(9.7) | 99(18.2) |
| III | 0 | 151(66.5) | 151(27.8) |
| IV | 0 | 23(10.1) | 23(4.2) |
| ART initiation(n=544) | - | - | - |
| Early ART initiation | 258(81.4) | 143(63) | 401(73.7) |
| Late ART initiation | 59(18.6) | 84(37) | 143(26.3) |
| - | Adults’ Status | Total (n=544) |
|
|---|---|---|---|
| - | Non-AHD (n=317) |
AHD (n=227) |
|
| Engaged in care at 12 months(n=544) | - | - | - |
| Yes | 274(86.4%) | 194(85.5%) | 468(86%) |
| No | 43(13.6%) | 33(14.5%) | 76(14%) |
| Death at 12 months(n=544) | - | - | - |
| Yes | 19(6%) | 12(5.3%) | 31(5.7%) |
| No | 298(94%) | 215(94.7%) | 513(94.3%) |
| Lost to follow-up at 12 months(n=544) | - | - | - |
| Yes | 24(7.6%) | 21(9.3%) | 45(8.3%) |
| No | 293(92.4%) | 206(90.7%) | 499(91.7%) |
3.4. Clinical Patient Outcomes of Study Participants
As presented in Table 3, most participants, 468 (86.03%), remained engaged in care for 12 months after starting ART, while 76 (13.97%) were disengaged within 12 months, highlighting a challenge that should be addressed to improve patient health outcomes. Among those disengaged from care, 31 (5.7%) deaths were recorded within 12 months of treatment, while 45 (8.3%) participants were lost to follow-up. Further research is needed to determine the causal relationship behind this. Although all patients who initiate ART are expected to continue lifelong treatment and care, the issue of disengagement remains a concern and must be addressed.
4. DISCUSSION
This study aimed to determine the prevalence of AHD by analyzing the sociodemographic and clinical characteristics, as well as the clinical outcomes, of adults living with AHD among those initiated on ART in West Oromia, Ethiopia. The findings are intended to guide policymakers and program managers in developing targeted strategies to prevent AHD, improve the management of ALHIV and those with AHD, and review healthcare systems and social interventions associated with AHD. This, in turn, may help reduce AHD-related mortality and improve treatment and health outcomes.
4.1. Prevalence of AHD
The current study indicated that there is a high prevalence of AHD among adults initiated on ART between 2017 and 2021 and requires strengthening the management and monitoring of patients on ART in Ethiopia, particularly in the study area. This finding was similar when compared to a study performed in Uganda, where the prevalence of adults presented with AHD to care and treatment was 35.1% [7]. In addition, a systematic review and meta-analysis conducted in South Africa showed consistency with this study, where the prevalence of AHD among newly enrolled clients was 52.4% in 2010 and 43.4% in 2020, reflecting only a 2% decrease [27]. Similarly, a study in Sierra Leone reported an AHD prevalence of 41.6% [28]. In contrast, studies conducted in Senegal (71%) [29], Iran (53.9%) [30], and Epworth, Zimbabwe (47.4%) [31] reported a higher prevalence than this study.
On the other hand, the AHD prevalence in this study was higher than that reported in a cross-sectional study conducted in China (28.7%) at baseline review [32]. These differences among the previous studies are due to differences in the study population (the age of the participants <18 years included), sample sizes, the study design, and methodology. Additionally, factors, such as high turnover of skilled health personnel, limited healthcare workforce, and poor health-seeking behaviors have impacted the quality and accessibility of HIV care and treatment, contributing to high early mortality [19, 29, 33, 34]. The burden of AHD increases the risk of HIV-associated morbidity and mortality [35-38]. This requires optimisation of the targeted intervention package for early diagnosis of AHD and improving the quality of HIV care and treatment.
The highest proportion of participants with AHD was found in the 35-44 years age group (88, 38.8%), compared to the 18-24 years age group, which had 20 participants (8.8%) with AHD, as seen in the general distribution of participants. This is supported by a study done in Ethiopia that showed that older age had no significant association with AHD [39]. In Nasarawa State, Nigeria, the proportion of AHD was compared between adolescents 8(32%) and adults 159(51.3%). In addition, the highest percentage of AHD among age groups of 30-39 was discovered [40]. On the contrary, adolescents had a higher risk of AHD than adults [41]. There is a slight difference that might occur due to the study population difference. The prevalence of AHD among adolescents is warranted and needs further age-specific analysis. The male participants had higher 117(51.5%) AHD compared to females. This is supported by numerous studies indicating that the prevalence of AHD is higher among males than females among participants who initiated ART [35, 42, 43]. This disparity may be attributed to lifestyle factors, low health literacy, and a tendency for delayed healthcare-seeking behavior. In addition, men are thought to be less likely to seek medical attention for symptoms or health issues, which is exacerbated by traditional or conventional masculine norms that discourage men from discussing their health issues, which leads to delayed diagnosis, including early ART initiation or linkage or enrollment in care and treatment [13, 35].
Furthermore, the study found that participants with no formal education had a higher prevalence of AHD compared to those who were educated. This aligns with studies conducted in China [13] and Tanzania [35], which showed that formal education enhances health literacy, enabling PLHIV to understand HIV treatment and adherence better. However, the current study found no statistically significant association between HIV knowledge and AHD, warranting further research. In contrast, a study conducted in Selangor, Malaysia, indicated a significant association between HIV knowledge and late HIV presentation [44, 45].
This indicates that inadequate health literacy about HIV risks, treatment, and adherence has a negative impact on HIV management and should be addressed. Furthermore, this may explain why participants with no formal education have a limited understanding of HIV testing, which is essential for initiating HIV care and treatment. Education is a protective factor that enhances health-seeking behavior, facilitates better healthcare access, and improves overall health conditions and lifestyle [46].
4.2. Monitoring and Management of Patients Living with HIV
The study highlighted inadequate monitoring and management of PLHIV, with several patients lacking baseline test results and some delayed ART initiation, indicating a need for attention.
Although this study indicated that a high number of adults initiated on ART, 348 (64%), had CD4 cell test results at baseline, a considerable number of participants, 196 (36%), did not have baseline CD4 test results at their first clinic visit. This issue requires further investigation with HCPs to reduce it to zero and ensure testing before ART initiation. Among those who had CD4 test results, 127 (36.5%) were identified as having AHD, which requires attention. Additionally, 174 (23.3%) participants who did not undergo CD4 testing at enrollment were categorized as having AHD based solely on WHO staging. Some African countries, including Ethiopia, are not performing well in conducting CD4 cell tests at baseline. This is supported by a study in Zambia, where out of 174 participants who requested CD4 testing, only 77 (44%) had the test performed at baseline, highlighting the need for improvement [47]. However, the current study did not consider clients who had requested but not received CD4 testing at enrollment. Similarly, in Southwestern Asia, Iran reported low CD4 testing performance at enrollment, with only 612 (40.3%) undergoing the test [30]. A study in South Africa showed a decline in CD4 testing at ART initiation, from 78% in 2008 to 38% in 2017 [48].
In contrast, where CD4 testing was available, the percentage of results below 200 cells/mm3 improved from 10.5% in 2013 to 3.1% in 2021, indicating progress in ART services [49]. However, in the current study, 127 (36.5%) of participants had CD4 results below 200 cells/mm3. This can be explained by a lack of compliance due to CD machine unavailability and poor functionality, missing patient file reviews, and poor implementation of the package of care for AHD and HIV management guidelines across all healthcare providers (HCPs), which negatively affected monitoring. HCPs seem to focus mainly on ART initiation irrespective of WHO staging and CD4 results but do not conduct baseline tests and assessments and this should be ensured before initiation of ART. There is a gap that also leads to misclassification of HIV staging as per WHO definitions and guidelines, missing the opportunity to identify AHD early. Therefore, capacity building and training for healthcare providers (HCPs) and other stakeholders at the facility level are essential for the early diagnosis of AHD through CD4 test results and WHO staging for adults, including monitoring of implementation from the higher health bureau.
The study findings indicate that ART initiation among PLHIV has improved, as most ALHIV were initiated early on ART within seven days of diagnosis. Furthermore, the study indicated that the majority, i.e., 258(64.3%) of the participants who were initiated on ART early, had no AHD; however, a few, i.e., 143(35.7%), still had AHD. This finding is in line with a study conducted in Lesotho among participants with AHD, which found that 77(70.6%) of them initiated early ART and 32(29.4%) delayed ART initiation at the clinic [50]. This study further indicated that 84(58.7%) of participants who had AHD had initiated ART late due to the presence of OIs like TB, CM, and other diseases. There was no statistical association between HIV testing and service approaches related to AHD. However, community-based HIV counselling and testing approaches, lack of belief in the health benefits of early ART initiation, and failure to disclose ART status were the reasons for late ART initiation in meta-analysis and systematic review in sub–Saharan Africa [51]. The current study found that some patients missed the opportunity to be initiated early as per WHO guidelines, and this needs further investigation due to its policy and operational implications. This also delays screening, diagnosis, and treating major OIs among AHD individuals. Moreover, there is a need for community counseling to raise awareness of HIV status and encourage individuals to access ART. This should be addressed and closely monitored to improve ART initiation for HIV-positive individuals.
4.3. Clinical Outcomes of Individuals with AHD
In this present study, the status of clinical outcomes after initiating ART at 12 months of participants was assessed. The findings indicated a higher proportion of deaths among non-AHD, 19(61.3%) cases, than those with AHD, 12 cases (38.7%), at 12 months of engagement in care. This highlights critical concern for the healthcare system, necessitating the development of targeted initiatives. This is contrary to the findings of most other studies, which reported a higher death rate among those with AHD, warranting further investigation to identify other contributory factors. This is supported by previous studies, which found a higher risk of death within 12 months and a lower likelihood of survival among participants with AHD compared to those without AHD, who were later more likely to stabilize [16, 31, 52, 53]. Moreover, this is also supported by a systematic review conducted on AHD and mortality in global health programming, which revealed that death may be related to disengagement from care at 12 months and late ART initiation [54].
This can be due to different study populations and different care and management for ALHIV who were initiated on ART. This should be addressed by providing tailored adherence counselling interventions and early ART initiation to PLHIV.
5. LIMITATIONS
The study used medical records of only three high-volume public hospitals of Oromia, with a smaller sample. The study findings are only applicable to the study settings and cannot be generalised in the whole country. However, they provide a basis for developing strategies that can be implemented on a smaller scale and potentially expanded to other regions. The medical records of some patients were not used because of incomplete data at baseline and follow-up visits regarding care, treatment, and support. This issue requires attention, as it is crucial for continuity of care and research. Further research could be conducted in decentralized and rural health facilities to identify gaps and develop strategies to address them in the future.
CONCLUSION
The purpose of the study was to determine the prevalence of AHD among adults initiated on ART following a cross-sectional retrospective design over the period of five years, and the study revealed a high prevalence of AHD among this study population at 41.7% with 95% CI (37.5 - 46.0) during the period of ‘test and treat’.
Therefore, this study underscores the need for policymakers to develop targeted interventions that include community and facility awareness on the importance of knowing HIV status, early treatment and adherence, early detection, and the effective management and monitoring of PLHIV. This should include compliance with WHO and national guidelines by healthcare providers (HCPs). In addition, capacity building, psychosocial support, and monitoring the implementation of the care package for AHD in healthcare practices are crucial. These measures may help reduce complications, hospitalization costs, and the need for specialised treatments, while addressing the efforts of various stakeholders to manage AHD-related mortality, which could have been prevented. Developing such strategies can improve the health and well-being of patients.
Further studies to understand late health service-seeking behaviour among HIV-positive individuals, especially men, are required to understand the circumstances and reduce late ART initiation and prevent AHD.
AUTHORS’ CONTRIBUTIONS
G.A.: Conceptualized, studied, collected, and analysed data; S.H.: Contributed to the verification of data analysis, and GA and SH wrote the manuscript.
LIST OF ABBREVIATIONS
| AIDS | = Acquired immunodeficiency syndrome |
| AHD | = Advanced HIV disease |
| ALHIV | = Adults living with HIV |
| ART | = Antiretroviral therapy |
| EAC | = Enhanced adherence counselling |
| EMR | = Electronic medical records |
| HIV | = Human immunodeficiency virus |
| HCPs | = Healthcare providers |
| LMICs | = Low- and middle-income countries |
| MOHSS | = Ministry of health and social services |
| OIs | = Opportunistic infections |
| TB | = Tuberculosis |
| UAN | = Unique ART number |
| PLHIV | = People living with HIV |
| UNAIDS | = Joint United Nations Programme on HIV/AIDS |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The approval to conduct the study was first obtained from the University of South Africa College of Human Sciences Research Ethics Committee (CREC): reference number: 19946546_CREC _CHS_2023 on 23 November 2023. Additionally, an ethical clearance was also obtained from Oromia Health Bureau, Ethopia, with the reference number BFO/UBTFU/1-16/912 on 11 November 2023.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data sets used and/or analysed during this study are available from the corresponding author [S.M] upon request.
ACKNOWLEDGEMENTS
The authors would like to extend their gratitude to the Ministry of Health and Social Service's research ethics committee for granting permission for data collection and publication. They also appreciate the clinical data collectors for their efforts in reviewing patient medical files. Additionally, they acknowledge the participants for their valuable contributions to this study by sharing their views and experiences.


