All published articles of this journal are available on ScienceDirect.
Strengthening Health System Resilience through Digital Health: Challenges and Prospects in Indonesia's Rural and Remote Regions - A Scoping Review Protocol
Abstract
Introduction
Digital health has emerged as a critical tool for enhancing health system resilience, particularly in countries with substantial geographical disparities, such as Indonesia. Persistent barriers in rural and remote areas—limited internet access, inadequate infrastructure, and low digital literacy—continue to hinder the adoption of digital health initiatives. This scoping review aims to systematically map Digital Health Interventions (DHIs) implemented in rural Indonesia, identify key barriers and facilitators, and generate evidence-based recommendations for strengthening equitable healthcare delivery.
Methods
This study follows the Arksey and O’Malley framework and adheres to the PRISMA-ScR guidelines. A comprehensive search was conducted across PubMed, Scopus, Web of Science, Google Scholar, and Neliti.com for articles published between 2010 and 2024 in English or Bahasa Indonesia. Two independent reviewers conducted the screening, data extraction, and risk of bias assessment to enhance the quality and interpretation of findings.
Results
A total of 17,858 records were identified, and after screening and eligibility assessment, 20 studies were included. The studies reported various DHIs, including telemedicine services, mHealth applications, SMS-based platforms, and electronic health information systems deployed in rural and remote settings.
Discussion
Challenges to the implementation of DHI include infrastructural limitations, variations in digital literacy, and sociocultural barriers. Key enabling factors, such as supportive policies, sustainable funding, and community participation, have been identified as crucial for success.
Conclusion
The review offers a synthesis of digital health implementation experiences in underserved Indonesian regions, providing insights to inform future policies and initiatives aimed at building a resilient and inclusive health system.
1. INTRODUCTION
Health system resilience refers to the ability of health systems to anticipate, respond to, and recover from various shocks—such as pandemics, natural disasters, and economic crises—while continuing to provide essential healthcare services [1-3]. The World Health Organization (WHO) emphasizes that building resilient health systems is crucial for achieving Universal Health Coverage (UHC) and the health-related Sustainable Development Goals (SDGs) [4-7]. Strengthening resilience is particularly crucial in countries with geographically dispersed populations and unequal healthcare access, such as Indonesia [8, 9].
Digital health, which leverages Information and Communication Technologies (ICTs) to improve healthcare delivery, has been recognized as a key enabler of health system resilience [10-12]. Its applications include telemedicine, mobile health (mHealth) solutions, Electronic Health Records (EHRs), Health Information Systems (HIS), and even simple technologies, such as SMS-based communication platforms, all of which enhance efficiency, data accessibility, and patient care outcomes [13, 14]. The WHO's Global Strategy on Digital Health 2020–2025 underscores the transformative role of digital health in bridging healthcare gaps and ensuring service continuity during crises [2, 15].
In Indonesia, an archipelagic nation with more than 17,000 islands and significant healthcare disparities, the government has introduced various digital health initiatives to improve healthcare access and quality [16-18]. The SatuSehat platform (formerly PeduliLindungi) serves as a national integrated health data exchange system, streamlining patient records, vaccination data, and public health monitoring [17, 19]. The Blueprint for Digital Health Transformation Strategy 2024 provides a comprehensive roadmap for expanding digital infrastructure and services [20-22].
Despite these advancements, significant digital health disparities persist between urban and rural Indonesia. In 2019, approximately 94 million Indonesian adults lacked mobile internet access, with nearly 80% of them residing in rural regions of Sumatra, Java, and Bali [23, 24]. While rural internet penetration reached 74% in 2024, it still lags behind urban areas, where digital access is nearly universal. The East Ventures – Digital Competitiveness Index (EV-DCI) 2024 highlights an expanding gap between highly developed provinces like Jakarta and underdeveloped regions such as Papua. Beyond infrastructure limitations, low digital literacy also hinders digital health adoption [25, 26]. The 2023 Digital Health Maturity Assessment, covering 146 provinces and districts/cities, found that Indonesia scored an average of 2.73 out of 5.00, underscoring the need for stronger digital health infrastructure and capacity-building efforts [22]. The 2024 Digital Society Index further reflects Indonesia’s slow digital adoption, with rural communities experiencing the most difficulty integrating digital solutions into healthcare systems [27-30].
In addition to technological and infrastructure barriers, Indonesia’s vast linguistic and cultural diversity may affect the usability and accessibility of digital health services [31, 32]. Thus, local languages, sociocultural practices, and user-centered design must be considered in the implementation of DHIs to ensure equitable access [33]. Given the persistent digital divide and limited access to digital health services in rural Indonesia, it is crucial to systematically assess the landscape of Digital Health Interventions (DHIs) in these regions. While numerous digital health initiatives exist, there is a lack of consolidated evidence mapping their implementation, effectiveness, and the key barriers and facilitators to their success [34-36].
This scoping review aims to address this gap by systematically analyzing DHIs in Indonesia’s rural and remote regions, guided by the PRISMA-ScR framework to ensure methodological rigor and transparency. The resulting synthesis is expected to offer valuable insights for policymakers, healthcare providers, and stakeholders in developing more targeted strategies to enhance health system resilience and promote equitable healthcare access, particularly in underserved areas. This review is guided by the following research questions:
1. What types of digital health interventions have been implemented in rural and remote areas of Indonesia?
2. What are the key barriers and facilitators to their implementation?
3. How do these interventions contribute to strengthening health system resilience in underserved settings?
2. METHODS
2.1. Study Design
This scoping review aimed to systematically explore and map the landscape of digital Health Interventions (DHIs) in Indonesia's rural and remote regions, following the framework proposed by Arksey and O'Malley [37]. To ensure transparency and rigor, this study adhered to the PRISMA-ScR guidelines for reporting scoping reviews [38]. The primary objectives were to identify existing interventions, assess challenges and facilitators in their implementation, and provide evidence-based recommendations to strengthen health system resilience. In addition, this review integrated the risk of bias assessment into the interpretation of findings, enabling more nuanced recommendations and highlighting the quality of available evidence. The protocol for this scoping review has been registered on the Open Science Framework (OSF) for transparency and can be accessed at https://osf.io/dj3b9/.
2.2. Eligibility Criteria
Studies eligible for inclusion were those focusing on the development, implementation, or evaluation of DHIs in rural and remote areas of Indonesia. DHIs are broadly defined as healthcare services or processes delivered using information and communication technologies (ICTs), such as telemedicine platforms, mobile health (mHealth) applications, Electronic Health Records (EHRs), Health Information Systems (HIS), and SMS-based technologies. Both quantitative and qualitative studies published between 2010 and 2024 in English or Bahasa Indonesia were considered. Exclusion criteria included studies focusing solely on urban settings, non-digital health interventions, editorials, commentaries, opinion pieces, and studies without full-text access. Additionally, grey literature, such as government reports and policy documents, were included only if they met methodological rigor (Table 1).
2.3. Information Sources and Search Strategy
A comprehensive literature search was conducted across multiple electronic databases, including PubMed, Scopus, Web of Science, Google Scholar, and the Cochrane Library. Additional databases, such as Embase and CINAHL were considered for broader coverage. Grey literature was explored through Neliti.com, a prominent Indonesian open-access repository, along with government reports and institutional repositories. The search strategy utilized Boolean operators and Medical Subject Headings (MeSH) terms related to digital health and healthcare delivery. Sample MeSH terms included “Telemedicine,” “Health Information Systems,” “Mobile Applications,” “Rural Health Services,” “Indonesia,” and “Health System Resilience.” The strategy was reviewed using the PRESS checklist to ensure validity and comprehensiveness [39].
2.4. Study Screening Process
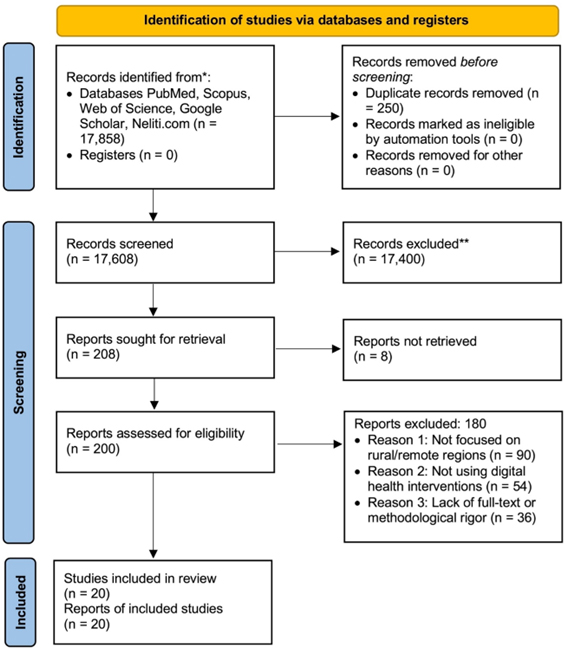
All search results were systematically imported into a reference management system for deduplication and screening. The screening process consisted of two stages: (1) title and abstract screening and (2) full-text review. Two independent reviewers assessed the relevance of studies based on predefined inclusion and exclusion criteria. Inter-rater reliability was measured using Cohen’s kappa coefficient to ensure consistency in study selection [40]. Any discrepancy was resolved through discussion or consultation with a third reviewer. The PRISMA flow diagram documented the study selection process.
2.5. Data Extraction and Management
Data were extracted using a standardized extraction form to ensure consistency. Key variables included study characteristics (authors, publication year, study design, and location), types of DHIs, target populations, reported outcomes, and identified barriers and facilitators (Table 2). All extracted data were managed using Microsoft Excel, and qualitative data analysis was conducted using MAXQDA software.
2.6. Risk of Bias Assessment
Although risk of bias assessment is not typically required in scoping reviews, this study incorporated it to inform the quality and strength of conclusions. The Cochrane Risk of Bias Tool was used for randomized controlled trials, the ROBINS-I tool for non-randomized studies, and the Critical Appraisal Skills Programme (CASP) checklist for qualitative studies [41, 42]. The results of these assessments were used to contextualize the findings and to identify areas where higher-quality evidence was needed. A summary table was included to present the outcomes of the bias assessment for all included studies.
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Study Focus | Digital health interventions in rural/remote Indonesia | Non-digital health interventions, urban-only studies |
| Study Design | RCTs, quasi-experimental, observational, mixed-methods, policy analyses, implementation reports | Editorials, commentaries, opinion pieces |
| Language | English or Bahasa Indonesia | Other languages |
| Publication Year | 2010-2024 | Pre-2010 studies |
| Availability | Full-text accessible | No full-text access |
| Variable | Description |
|---|---|
| Study Characteristics | Authors, year, study design, location |
| DHI Type | Telemedicine, mHealth, EHR, HIS, SMS-based, other ICT-based interventions |
| Target Population | Rural and remote communities in Indonesia |
| Reported Outcomes | Effectiveness, challenges, facilitators |
| Barriers and Facilitators | Key factors affecting implementation |
| Recommendations | Future implementation strategies |
2.7. Data Analysis
Both quantitative and qualitative data were synthesized to provide a comprehensive understanding of DHIs in Indonesia’s rural and remote regions. Descriptive statistics summarized study characteristics and outcomes, while qualitative data underwent thematic analysis using Braun and Clarke’s framework to identify key themes related to barriers, facilitators, and implementation strategies [43]. If feasible, a meta-analysis was conducted for homogeneous quantitative data.
3. RESULTS
A total of 17,858 records were identified through database searches (PubMed, Scopus, Web of Science, Google Scholar, and Neliti.com). After removing 250 duplicate records, 17,608 records remained for screening. Based on the title and abstract review, 17,400 records were excluded. Full texts were retrieved for 208 reports, and 200 were assessed for eligibility. Of these, 180 reports were excluded due to not focusing on rural/remote regions (n = 90), not utilizing digital health interventions (n = 54), or lacking full-text access or methodological rigor (n = 36). Consequently, 20 studies were included in the scoping review. The study selection process is illustrated in Fig. (1), following the PRISMA 2020 flow diagram framework [44].
4. DISCUSSION
This scoping review was designed to explore the landscape of Digital Health Interventions (DHIs) in rural and remote areas of Indonesia, with the intention of identifying common challenges, implementation enablers, and areas requiring further inquiry. By synthesizing evidence from diverse sources, the review may help inform discussions among policymakers, healthcare providers, and researchers on how digital health can be better tailored to underserved populations [13, 14, 45].
It is anticipated that the review will outline structural gaps in digital health adoption, particularly those related to infrastructure limitations, digital literacy, and fragmented policy implementation [22, 25, 26]. These findings may offer preliminary insights into potential strategies for narrowing urban-rural gaps in digital health access and promoting more inclusive access to digital health innovations [20, 27, 30].
In addition, the review will examine contextual factors—such as regulatory support, funding environments, and community participation—that have shaped the deployment of DHIs in various regions [38]. Consideration will also be given to more accessible technologies like SMS-based platforms, especially in low-connectivity settings [10, 11], and to the role of linguistic and cultural diversity in influencing intervention reach and uptake [28, 29].
Although empirical stakeholder engagement is not included at this stage, future research could integrate perspectives from health workers, community members, and local governments to enrich and validate the findings [38, 43, 44]. Such perspectives may contribute to a more grounded understanding of the practical and sociocultural dimensions of digital health implementation in diverse settings.
This study acknowledges several limitations. As a scoping review, it did not generate effect estimates or measure intervention efficacy. Moreover, the exclusion of non-English and non-Indonesian sources might limit the scope of the findings. Finally, the absence of real-time stakeholder input may constrain the practical contextualization of results. These limitations will be addressed in the interpretation of findings and recommendations.
CONCLUSION
This study outlines a planned scoping review that aims to map Digital Health Interventions (DHIs) in the rural and remote settings of Indonesia. The study will promote implementation experiences, contextual challenges, and enabling factors across diverse regions. While the review is not intended to generate definitive conclusions, its findings may provide early insights to guide future research, inform inclusive policy considerations, and contribute to broader efforts to strengthen health system resilience in resource-constrained settings.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: Study conception and design: RW; validation: SBS; and draft manuscript: FAR, JA, SS, AR, FJ, and RWB. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| DHIs | = Digital Health Interventions |
| WHO | = World Health Organization |
| UHC | = Universal Health Coverage |
| SDGs | = Sustainable Development Goals |
| ICTs | = Information and Communication Technologies |
| EHRs | = Electronic Health Records |
| HIS | = Health Information Systems |
| EV-DCI | = East Ventures – Digital Competitiveness Index |
| CASP | = Critical Appraisal Skills Programme |
AVAILABILITY OF DATA AND MATERIAL
The data supporting the findings of the article is available in the Open Science Framework (OSF) at https://osf.io/dj3b9/, reference number: dj3b9.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the Varians Statistik Kesehatan for providing the boot camp and mentoring to improve manuscript writing.


