All published articles of this journal are available on ScienceDirect.
Knowledge, Attitudes and Practices of Men and Women Regarding Infertility in the City of Tshwane, Pretoria, South Africa
Abstract
Introduction
Infertility continues to be a major public health issue with deep social and psychological effects, particularly in low- and middle-income environments. The purpose of this study was to evaluate the knowledge, attitudes, and practices of men and women around infertility in the City of Tshwane, Pretoria, South Africa.
Methods
This descriptive quantitative study surveyed 390 participants in Tshwane District primary healthcare settings using a self-administered questionnaire and stratified sampling.
Results
The study found that most participants had a good understanding of infertility causes, with 67.4% identifying menstrual cycle irregularities as a potential factor for female infertility and 64.4% recognizing semen abnormalities as a cause for male infertility. However, there were some misconceptions identified, such as 30.5% of people believed that infertility was more common in women than in men, and 69.2% of individuals considered it a disability. With 79.5% of respondents identifying infertility as a medical problem, attitudes regarding it were largely positive. The majority—90.7% of the participants—were open to changes in lifestyle and assisted reproductive methods, such as IVF. Gender differences in coping mechanisms were found in that 79.2% of males favoured traditional medicine for the treatment of infertility, while 90% of the women preferred spiritual or religious practices.
Discussion
According to this study, both men and women in Tshwane had favourable views and good knowledge regarding infertility. Though there were some misunderstandings, most participants were aware of some causes of infertility. Openness to medical treatments was noted in the willingness to embrace assisted reproduction and lifestyle modifications.
Conclusion
The study found that while men and women had knowledge and positive attitudes toward infertility. However, misconceptions, such as viewing infertility as a disability and as a woman’s problem, persisted. Attitudes towards infertility from both genders were mainly positive, with significant support for lifestyle modifications and assisted reproduction technology. Gender differences in coping mechanisms were evident, with males choosing traditional medicine while women favoured religious methods. To increase awareness and lessen the stigma associated with infertility, the study stressed the need for gender-sensitive, culturally relevant health educational initiatives to improve awareness and address misconceptions.
1. INTRODUCTION
Infertility is a condition affecting the reproductive system of either males or females. It is regarded as a failure to fall pregnant after 12 months or more of regular unprotected sexual intercourse [1, 2]. Primary infertility is considered an occurrence in a couple who have never been able to conceive and have a live birth for more than five years of being in a sexual relationship without the use of any contraceptives [3-5]. At the same time, secondary infertility occurs when a couple has trouble conceiving after a previous pregnancy [1, 4]. The rising rates of infertility worldwide are acknowledged as a significant global issue affecting both women and men [5, 6]. Globally, infertility affects 8 to 12% of men and women of reproductive age [7, 8]. Over 40 million couples and 186 million individuals globally live with infertility [1, 9].
Multiple causes and consequences of infertility exist [10, 11]. Infertility in men and women may be caused by abnormalities related to the male and female reproductive systems [1, 12, 13]. Disorders of the ovaries, such as Polycystic Ovarian Syndrome (PCOS) or other follicular disorders of the uterus, fallopian tubes, and endocrine system, are the most common causes of infertility in females [14, 15]. In males, the diagnosis is mainly based on semen disorders detected during semen analysis [16, 17]. The causes include hormonal disorders, physical problems, lifestyle factors, psychological problems, sexual issues, chromosomal abnormalities, and single-gene defects [18-20].
Although infertility is not a life-threatening disease, it has serious psychosocial consequences [21]. This is often due to high levels of stress on couples or individuals [22, 23]. Infertility is a stressful process for partners in a relationship, but women report greater stress and a burden, making them more vulnerable [24, 25]. Infertility can consequently lead to a destabilisation in families, marriages, and relationships, which often results in divorce, polygamy, and or extramarital affairs [26, 27]. There is a high prevalence of depression and anxiety among infertile women; their self-esteem is negatively associated with depression and anxiety [28]. Community stigmatisation, as well as shame and exclusion, are some of the most painful consequences infertile individuals and couples face [29, 30].
Having children at one’s desired time is a fundamental human right [29, 31]. Over the years, the efforts of the health systems have shifted mainly to the prevention of unwanted or unintended pregnancies and pregnancies that happen too early or too late in life, consequently forsaking the magnitude and consequences of infertility [29, 31]. Traditional, cultural, and social practices influence every person’s life [32, 33]. How people live their lives and make decisions is not only guided by their religion, beliefs, and values but also by traditional, cultural, and social practices [32, 34]. Additionally, these practices play an important role in the knowledge, attitudes, and practices of everyone.
2. AIMS AND OBJECTIVES
According to Ofosu-Budu, addressing the knowledge, attitudes, and practices of men and women can help reduce the stigma and misconceptions associated with infertility [16, 30, 35]. Knowledge is a highly valued state where one is in cognitive contact with reality. In this study, knowledge refers to the awareness and understanding of infertility as a subject matter determined by every individual’s previous experience or education regarding infertility [36]. Attitude is a person’s feeling or opinion about a certain subject, matter, or behaviour influenced by past experiences or the opinions of others around them [37]. In this study, attitude refers to the opinions or feelings of men and women regarding infertility based on their understanding and past experiences. Practices refer to an act that is often a habit or a custom guided by personal norms [38]. In this study, practices refer to the actions, habits, culture, customs, as well as spiritual and traditional beliefs guided by norms.
There is minimal evidence of studies conducted in urban and rural settings of South Africa (SA) regarding the knowledge, attitudes, and practices of women and men towards infertility [39]. To address this issue, we conducted a quantitative, descriptive study to investigate the knowledge, attitudes, and practices of men and women regarding infertility in three (3) selected Primary Health Care (PHC) clinics in District One, City of Tshwane, Pretoria, South Africa.
To achieve this aim, the following objectives were measured:
- To assess the knowledge of men and women regarding infertility
- To determine the attitudes of men and women regarding infertility
- To determine the practices of men and women regarding infertility
- To establish the relationship between gender and the knowledge of men and women regarding infertility
3. MATERIALS AND METHODS
3.1. Design
A quantitative survey design was used to assess the knowledge, attitudes, and practices of men and women regarding infertility in Tshwane, Pretoria, South Africa.
3.2. Setting and Respondents
The study was conducted at three (3) selected clinics in the City of Tshwane Municipality district. The clinics offer PHC services for children and adult patients. The clinics mainly cater to community members of various ethnic backgrounds, including Black, White, Coloured, and Indian. A set of criteria was used to choose the sample's subjects. To be included in the sample, respondents had to meet the following requirements: women aged 18 years and above; men aged 18 to 55 years; and currently residing in the City of Tshwane while seeking primary health care at one of the three (3) clinics.
Respondents who did not meet the inclusion criteria were excluded from the study. This included men and women younger than 18 years of age, men older than 55 years of age, and respondents who did not reside in the City of Tshwane or were not seeking PHC services from any of the three selected PHC clinics.
The sample size calculated for the study was 377, and the Cochran equation was used to estimate the sample size. Sample size: For unknown populations, the suggested population size to estimate the required sample is N = 20,000. The study employed stratified sampling techniques and aimed to recruit a sample size of 377; however, a total sample of 390 patients was approached and willing to participate in the research study, each of whom met the study entry criteria and voluntarily completed the consent and study questionnaire. A breakdown of the male and female population from each clinic is presented in Table 1.
| - | Male | Female |
|---|---|---|
| Clinic 1 | 7 | 93 |
| Clinic 2 | 20 | 152 |
| Clinic 3 | 16 | 102 |
The data was collected over a period of two (2) weeks in October 2023. To increase gender representation by recruiting both male and female participants, data were collected from different clinics, serving diverse demographics on different days. The researcher and clinic staff recruited both female and male participants, and the questionnaire was gender-neutral, covering content that both males and females could relate to. Regardless of all these efforts, most participants were still primarily female, which is indicative of the gender disparities in PHC clinics' health-seeking patterns and practices.
3.3. Survey Measures
The questionnaire was adapted from a study conducted in Saudi Arabia [40]. The questionnaire consisted of four (4) sections, sections A to D. Section A aimed to collect demographic data such as age, gender, residential area, marital status, highest level of education, and occupation. Section B focused on the knowledge and factors that may affect infertility. Section C determined the attitudes of respondents regarding infertility. Section D focused on the practices of the respondents regarding infertility.
3.4. Reliability of the Questionnaire
Reliability can also be enhanced by minimising measurement error sources like data collector bias. The researcher's bias as a data collector was minimised by distributing the questionnaires alone and enforcing uniform criteria, such as being kind and encouraging of every response. The physical environment where the respondent filled out the questionnaires was an orderly and quiet space in the clinic to offer the respondent psychological comfort, confidentiality, and privacy. The respondents had chairs to sit on and a pen to complete the questionnaire. The tool was piloted and found to be valid and reliable.
3.5. Statistical Analysis
For data analysis, the International Business Machines (IBM) Statistical Package for the Social Sciences (SPSS) version 28 was used to produce the analysis. Descriptive statistics were employed to present the findings of the study. The data interpretation included descriptive statistics in the form of frequency tables and percentages. To determine whether there is an association between Gender and Knowledge, Attitudes, and Practices, the Fisher-Freeman-Halton Exact test was performed. This test was chosen because the structure of the contingency table did not meet the assumption of a Pearson chi-square test, which requires that the expected count in a cell be greater than 5. The test was conducted at a 5% significance level. If the p-value obtained is less than 0.05, we reject the null hypothesis that there is no association between the variables.
3.6. Ethical Considerations
Written permission to conduct this study was obtained from the University of Pretoria’s Faculty of Health Sciences Research and Ethics Committee and the Gauteng Province Research Committee under the following ethics approval reference numbers: University of Pretoria 190/2023 and Gauteng Province 61/2023. Informed consent was obtained from all the respondents prior to their participation.
Each of the respondents was informed of their right to freely withdraw their participation in the study at any time without any consequence or penalty. Furthermore, the Declaration of Helsinki's ethical standards were followed in the conduct of this study. Confidentiality and anonymity were adhered to protect the respondent’s privacy and maintain anonymity by ensuring that no personal identifying information was required on the questionnaire. All questionnaires were coded for identification and securely stored behind a lock and key, where only the researcher had access to them.
Fundamental ethical principles, including beneficence, human dignity, justice, anonymity, confidentiality, self-determination, and scientific honesty, were adhered to ensure the protection of the respondents. Beneficence was maintained by ensuring that all respondents were protected from physical, mental, and emotional harm. The researcher upheld this principle by ensuring the respondents had a safe environment that provided them with psychological support during data collection. The principles of human dignity and justice were adhered to by ensuring that the respondents were fully informed about purpose and objectives of the study. Scientific honesty was respected by maintaining transparency in the data collection and analysis process. This was done under the supervision of a supervisor and an independent statistician to prevent data manipulation and to ensure the integrity of the findings. External validity, the degree of generalizability of study results to the intended audience, is known as external validity. The primary factor affecting the eventual external validity of the research is the method used to select the sample [41]. All the respondents who approached to partake in the study completed the questionnaire.
4. RESULTS
4.1. Demographics Analysis
The study aimed to recruit 377 respondents; however, 390 were recruited and completed the questionnaire. All respondents fulfilled the requirements to participate in the study. Most of the respondents (89%) were females, and 11% of the respondents were males. The most common age groups were between 35 and 55 years (48%), followed by 25-35 years (45%). Most respondents were single (57%), 27% were married, and 16% were divorced. Most respondents were from a township (75%), while 18.5% were from suburban areas. The highest level of education (47%) was college graduates, and most respondents (53%) were employed.
4.2. Knowledge Factor Variables That May Affect Fertility and Its Associated Relationship with Gender
Table 1 summarises the gender-specific responses from the respondents regarding their knowledge of factors and perceived misconceptions that may affect fertility in men and women. Additionally, Table 1 highlights the relationship between knowledge factors, perceived misconceptions, and gender regarding factors that may affect fertility in men and women.
Most respondents in this study showed good knowledge and understanding towards different causes of infertility as they agreed that abnormal menstruation (67.4%), abnormalities of semen and sperm in men (64.2%), history of infections of the reproductive system in women (64.3%) and men (61%), and psychological stress (71.5%) can cause infertility. Additionally, the respondents showed good knowledge and understanding regarding the effects of previous use of contraceptives (62.0%) and intrauterine devices (56%) by disagreeing with these factors’ ability to impact one’s fertility. However, when asked about lifestyle factors that can affect fertility, most respondents showed a lack of knowledge as they disagreed that drinking alcohol (58.8%), smoking (64.2%), and engaging in vigorous exercise (61.7%) can affect fertility. Furthermore, most respondents showed a lack of knowledge and understanding by agreeing that black magic (56.5%) and supernatural causes (71.2%) can affect fertility. The Fisher Hamilton Exact test produced a significant relationship between gender and knowledge about abnormal menstruation, that is, ovulation problems or blocked tubes affecting fertility among women and men (p-value = 0.04). Most females (69.3%) agreed, whereas some males (51.2%) agreed with the statement; some of the males (29.3%) respondents disagreed, compared to 9.3% of the females who disagreed.
Fisher Hamilton Exact test yielded a significant relationship between gender and knowledge about black magic as a cause of infertility in men and women (p-value 0.045). Most females (56.5%) agreed with the statement, similarly, so did most males (56.1%), whereas some male (43.9%) and female respondents (33.3%) disagreed with the statement. All other knowledge factors that may affect fertility variables were not statistically significant with gender, as shown in Table 2.
| Statement | Category | Gender | |||
|---|---|---|---|---|---|
| Can any of the following affect fertility? | Male | Female | Total | p - value | |
| Abnormal menstruation (Ovulation problems or blocked tubes) | Yes | 21 (51.2%) | 239 (69.3%) | 260 (67.4%) | 0.043 |
| No | 12 (29.3%) | 74 (21.4%) | 86 (22.3%) | ||
| Don't know | 8 (19.5%) | 32 (9.3%) | 40 (10.4%) | ||
| Abnormalities of semen and sperm in men | Yes | 22 (53.7%) | 226 (65.5%) | 248 (64.2%) | |
| No | 13 (31.7%) | 79 (22.9%) | 92 (23.8%) | 0.297 | |
| Don't know | 6 (14.6%) | 40 (11.6%) | 46 (11.9%) | ||
| History of infections of the reproductive system in women | Yes | 24 (58.5%) | 225 (65.2%) | 249 (64.3%) | |
| No | 11 (26.8%) | 88 (25.5%) | 99 (25.6%) | 0.476 | |
| Don't know | 6 (14.6%) | 32 (9.3%) | 38 (9.8%) | ||
| History of infections of the reproductive system in men | Yes | 26 (63.4%) | 206 (59.7%) | 232 (61.1%) | |
| No | 11 (26.8%) | 104 (30.1%) | 115 (29.8%) | 0 .938 | |
| Don't know | 4 (9.8%) | 35 (10.1%) | 39(10.1%) | ||
| Drinking alcohol | Yes | 16 (39.0%) | 129 (37.4%) | 145 (37.6%) | |
| No | 25 (61.0%) | 202 (58.6%) | 277 (58.8%) | 0 .590 | |
| Don't know | - | 14 (4.1%) | 14 (3.6%) | ||
| Smoking | Yes | 12 (29.3%) | 112 (32.5%) | 124 (32.1%) | |
| No | 27 (65.9%) | 221 (64.1%) | 248 (64.2%) | 0 .780 | |
| Don't know | 2 (4.9%) | 12 (3.5%) | 14 (3.6%) | ||
| Vigorous exercise | Yes | 8 (19.5%) | 110 (31.9%) | 118 (30.6%) | |
| No | 27 (65.9%) | 211 (61.2%) | 238 (61.7%) | 0 .098 | |
| Don't know | 6 (14.6%) | 24 (7.0%) | 30 (7.8%) | ||
| Previous use of contraceptives | Yes | 13 (31.7%) | 95 (27.6%) | 108 (28.1%) | |
| No | 22 (53.7%) | 217 (63.1%) | 239 (62.1%) | 0. 357 | |
| Don't know | 6 (14.6%) | 32 (9.3%) | 38 (9.9%) | ||
| Previous use of intrauterine devices | Yes | 11 (26.8%) | 107 (31.0%) | 118 (30.65) | |
| No | 24 (58.5%) | 192 (55.7%) | 216 (56.0%) | 0 .856 | |
| Don't know | 6 (14.6%) | 46 (13.3%) | 52 (13.5%) | ||
| Black magic | Yes | 23 (56.1%) | 195 (56.5%) | 218 (56.5%) | |
| No | 18 (43.9%) | 115 (33.8%) | 133 (34.5) | 0.045 | |
| Don't know | - | 35 (10.1%) | 35 (9.1%) | ||
| Supernatural causes | Yes | 33 (80.5%) | 242 (70.1%) | 275 (71.2%) | |
| No | 8 (19.5%) | 82 (23.8%) | 90 (23.3%) | 0.219 | |
| Don't know | - | 21 (6.1%) | 21 (5.4%) | ||
| Psychological stress | Yes | 31 (75.6%) | 245 (71.0%) | 276 (71.5%) | |
| No | 10 (24.4%) | 85 (24.6%) | 95 (24.6%) | 0.563 | |
| Don't know | - | 15 (4.3%) | 15 (3.9%) | ||
| Getting married at an older age | Yes | 27 (65.9%) | 236 (68.4%) | 263 (68.1%) | |
| No | 14 (34.1%) | 90 (26.1%) | 104 (26.9%) | 0.198 | |
| Don't know | - | 19 (4.9%) | 19 (4.9%) | ||
| Endocrine problems (Hormone imbalances) | Yes | 31 (75.6%) | 210 (61%) | 241 (62.6%) | |
| No | 8 (19.5%) | 119 (34.6%) | 127 (33%) | 0.115 | |
| Don't know | 2 (4.9%) | 15 (4.4%) | 17 (4.4%) | ||
| Diabetes mellitus | Yes | 29 (70.7%) | 176 (51%) | 205 (53.1%) | |
| No | 10 (24.4%) | 144 (41.7%) | 154 (39.9%) | 0.056 | |
| Don't know | 2 (4.9%) | 25 (7.2%) | 27(7%) | ||
| Obesity | Yes | 27 (65.9%) | 165 (47.8%) | 192 (49.7%) | |
| No | 14 (34.1%) | 159 (46.1%) | 173 (44.8%) | 0.052 | |
| Don't know | - | 21 (6.1%) | 21 (5.4%) | ||
| Are men to blame for infertility? | Yes | 9 (22%) | 110 (31.9%) | 119 (30.8%) | |
| No | 32 (78%) | 233 (67.5%) | 265 (68.7%) | 0.372 | |
| Don't know | - | 2 (0.6%) | 2 (0.5%) | ||
| Are men to blame for infertility? | Yes | 4 (9.8%) | 25 (7.2%) | 29 (7.5%) | |
| No | 37 (30.2%) | 313 (90.7%) | 350 (90.7%) | 0.697 | |
| Don't know | - | 7 (2%) | 7 (1.8%) | ||
4.3. Attitudes of Respondents Towards Infertility and Its Social Consequences
Table 2 presents the results of the respondents’ responses to questions that focus on their attitudes towards infertility and its social consequences. When asked whether they consider infertility a simple problem or not, most respondents (79.5%) agreed, while only a few (13.1%) disagreed. Most respondents indicated that they agree (88.5%) that infertility is an illness that should be treated medically. Most respondents also agreed (83.2%) that if a couple cannot have children, they should adopt a child or children, and that it is the responsibility of the community to help people without children (68.9%). The study also found that most respondents (64.6%) disagreed with men marrying a second wife if their wife was unable to have children, while some respondents (31.8%) agreed that men should marry a second wife. Furthermore, most respondents (88.1%) agreed that the use of fertility medications is acceptable, and that it is also acceptable (90.7%) to have a baby through In Vitro Fertilization (IVF).
A statistically significant relationship was noted between gender and the perception of infertility as a simple problem (p = 0.001). Most male respondents (75.6%) agreed with this statement, while most female respondents (59.1%) disagreed. Similarly, gender was significantly associated with attitudes toward whether infertility should be treated medically (p = 0.038). While all male respondents (100%) supported medical treatment for infertility, only a slightly lower percentage of female respondents (87%) agreed.
Additionally, a significant relationship was identified between gender and the belief that society is responsible for assisting individuals without children (p = 0.004). Most male respondents (90.2%) agreed with this view, while only a few female respondents (26.7%) disagreed. The study also found a statistically significant association between gender and attitudes regarding the justification of males initiating polygamy in response to infertility (p = 0.001). While 65.9% of male respondents agreed that polygamy is a valid option if a first wife is unable to conceive, most female respondents (68.2%) were opposed to this view.
Furthermore, a significant relationship was observed between gender and attitudes toward adoption as a solution for individuals or couples without children (p = 0.001). Most female respondents (86.7%) supported adoption, while a significant proportion of male respondents (46.3%) opposed it. Lastly, gender was significantly associated with attitudes regarding the acceptability of IVF as a solution to infertility (p = 0.001). Most female respondents (91.7%) viewed IVF as an acceptable method for conception, whereas some (19.5%) of the male respondents disagreed. All data from this section is presented in Table 3.
4.4. Practices Regarding Infertility
Table 3 presents the respondents’ perspectives on infertility-related practices. In this section of the study, most respondents (71%) believed that both males and females should be investigated first when assessing infertility. A smaller proportion (15.9%) suggested prioritizing females, while some (10.3%) believed males should be investigated first. All data from this section is presented in Table 4.
Regarding preferences for medical consultation related to infertility, most respondents (67.9%) indicated that their first choice would be to consult a gynaecologist, while a significant percentage (55.4%) identified a urologist as their second preference. The detailed findings are presented in Table 5.
Regarding common lifestyle practices aimed at improving fertility, most female respondents (90%) reported seeking spiritual guidance, upliftment, or encouragement by reading the Bible. A significant percentage of the female respondents (85.2%) also indicated a willingness to quit smoking, while some (78.6%) agreed to stop alcohol consumption to enhance fertility. Additionally, both male (73.2%) and female (87.8%) respondents stated their willingness to incorporate exercise into their routines to improve fertility. The most common practice among both genders was following a specific diet, with 75.6% of males and 91% of females agreeing to this practice. Furthermore, 89.9% of the female respondents reported a preference for over-the-counter medications to enhance fertility, whereas 79.2% of male respondents favoured the use of traditional medicine. The details of these findings are presented in Fig. (1).
| - | Agree | Not sure | Disagree | p-value |
|---|---|---|---|---|
| I think infertility is an illness. | n=310 (79.5%) |
n=29 (7.4%) |
n=51 (13.1%) |
0.040 |
| I think infertility should be treated medically. | n=345 (88.5%) |
n=6 (1.5%) |
n=39 (10%) |
0.038 |
| I think it’s society’s responsibility to help people without children. | n=266 (68.9%) |
n=24 (6.2%) |
n=96 (24.9%) |
0.004 |
| I think that if women can’t have children, it is a valid reason for a man to marry a 2nd wife. | n=122 (31.8%) |
n=14 (3.6%) |
n=248 (64.6%) |
p<.001 |
| I think that if a couple can’t have children, they should adopt. | n=321 (83.2%) |
n=10 (2.6%) |
n=55 (14.2%) |
p<.001 |
| I think it’s acceptable to have a test tube/IVF baby. | n=350 (90.7%) |
n=20 (5.2%) |
n=16 (4.1%) |
p<.001 |
| I think that fertility medication is acceptable. | n=340 (88.1%) |
n=20 (5.2%) |
n=26 (6.7%) |
0.219 |
| Question | ||||
|---|---|---|---|---|
| Men | Women | Both | Other | |
| Who do you think should be investigated first? | 40 (10.3%) |
62 (15.9%) |
277 (71%) |
11 (8.4%) |
| Question | ||||
|---|---|---|---|---|
| Urologist | Gynecologist | Healer | Other | |
| First preference for consultation or seeking medical help. | 87 (21.8%) |
271 (67.9%) |
30 (7.5%) |
2 (0.5%) |
| Secondary preference for consultation or seeking medical help. | 216 (55.4%) |
100 (25.6%) |
67 (17.2%) |
7 (1.8%) |
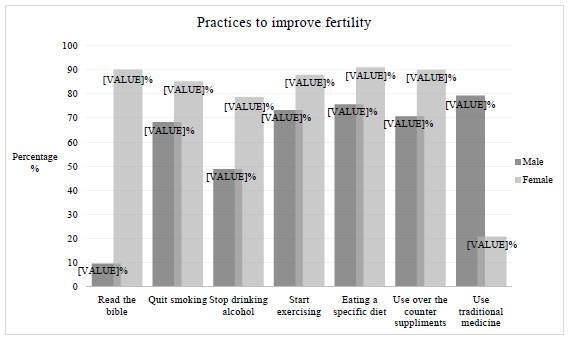
Practices to improve or support fertility.
5. DISCUSSION
This study aimed to investigate the knowledge, attitudes, and practices of men and women regarding infertility in three (3) selected PHC clinics in District One, City of Tshwane, Pretoria, South Africa. The results revealed that most male and female respondents had adequate knowledge and understanding of how irregular menstruation could impact fertility. Furthermore, abnormalities of semen and sperm in men, a history of infections of the reproductive system in women and men, as well as psychological stress, could contribute to infertility. Irregularities in the menstrual cycle can significantly impact fertility, as this is usually a sign of ovarian dysfunction; however, the knowledge and association between irregular menstruation and fertility issues is still poor [42, 43]. Additionally, low fertility awareness may contribute to infertility states. McLindon, who found that fertility awareness education improves knowledge of the menstrual and fertility cycle and may potentially assist in addressing infertility issues [44, 45].
The study also revealed that most of the respondents were also of the view that black magic and supernatural forces are causes of infertility, as most of the respondents indicated that black magic or supernatural forces can cause infertility. Similar findings were noted in Ghana [35]. The belief that supernatural causes, such as black magic, can cause infertility is prevalent in many cultures [46, 47]. In a study conducted in Indonesia, over half of the study population believed that supernatural forces, such as black magic, contribute to infertility [48]. Similar findings were noted in India, where a comparative study between fertile and infertile women showed that most of the infertile women believed that black magic or jinn caused their infertility [49]. Increasing fertility education to raise fertility awareness would play an important role in addressing misinformation and improving reproductive health knowledge among both males and females. It is important to note that most beliefs in supernatural powers and witchcraft are rooted in cultural and religious values. Taking this into consideration, infertility health education should seek to educate couples and individuals regarding the causes of infertility without shaming or disregarding ones cultural and religious values is important.
In this section, the results of this study revealed that most male and female respondents had a positive attitude about infertility being regarded as an illness. Furthermore, male and female respondents consider infertility a disease, while some referred to it as a disability. Most women live with a discredited social status due to their childless state in their communities [50]. The psycho-social and psychological challenges faced by men and women dealing with infertility indicate a need for support, health education, and access to affordable fertility health care. This can be done by integrating medical, psychological, social, and policy-driven interventions to support individuals and couples affected by infertility. This will help reduce the stigma, improve mental well-being, and improve access to the necessary healthcare services and resources.
The study highlighted that most men and women consider it the community’s responsibility to support or help couples without children. Furthermore, most men and women found it acceptable for couples without children to adopt. According to research, the society one lives in holds the responsibility to support childless individuals through the challenges they may face [51]. Childless individuals later in life often face limited social support, which may lead to an increased risk of isolation and mental health issues. Therefore, societal support systems may assist in decreasing the risks of isolation and mental health issues [52].
The study findings also revealed that most men and women did not think that a woman struggling to conceive was a valid reason for a man to marry a second wife. According to research, in some cultures, if a wife is unable to bear children, the husband may take another wife to fulfil his desire to have children [53]. However, most women in polygamous marriages experience emotional and social challenges [54, 55]. Similar findings were noted in Pakistan, where the women who permitted their husbands to marry another wife reported feelings of jealousy, unhappiness, and loneliness due to injustices by their spouses [53].
Additionally, the study also found that most women supported adoption, while a significant proportion of male respondents opposed it. According to research, most adoptive parents have faced fertility problems and mentioned infertility as the primary reason for adoption [56, 57]. Although the transition from failed fertility treatments to considering adoption is difficult, most couples view adoption as an alternative after the financial and emotional stress that comes with failed fertility treatments [56, 58].
The study findings also revealed that most men and women had a positive attitude towards infertility being treated medically with fertility drugs and the use of IVF to try to conceive. The success rates of IVF have significantly improved over the years, as have birth rates. However, not all embryo transfers are successful. Most men and women, however, will eventually achieve success if they continue with treatment [59, 60]. This positive respondent’s positive attitude toward medical treatment, the use of fertility drugs, and IVF is an indication that most men and women would consider making use of these treatment options should they struggle to conceive.
Most men and women indicated that both partners should be investigated together at the same time, should they experience infertility. Most men and women stated that they would rather consult a gynaecologist first and a urologist secondly if they struggled to conceive. Couples who are having trouble getting pregnant often visit a gynaecologist before thinking about seeing a urologist. Numerous factors, such as cultural norms, the perceived duties of these specialists, and the early emphasis on female reproductive health associated with infertility, all have an impact on this decision [26]. Gynaecologists are usually the primary point of contact for couples seeking infertility assistance; they oversee treatments and perform early evaluations of the reproductive health of women [61]. Many couples prioritize gynaecological appointments because of this approach, which is in line with the widespread belief that infertility is predominantly a female concern [61, 62]. However, almost 50% of infertility cases around the world are due to male causes [63]. Despite this, cultural attitudes and a lack of knowledge regarding male infertility promote men putting off getting professional care [64]. The collaboration between gynaecologists and urologists is important for comprehensive infertility care as working together, the specialties can provide a more thorough evaluation and treatment plan for couples struggling to conceive [65, 66]. Therefore, it is essential for couples to consider early involvement of a reproductive urologist, alongside a gynaecologist for a more comprehensive assessment and treatment plan.
The study found that most men and women were willing to make necessary adjustments to enhance their fertility health. Most females in this study reported seeking spiritual guidance, upliftment, or encouragement by reading the Bible. Similar findings were noted in Turkey where women who underwent fertility treatments valued spiritual wellbeing. This study found a significant correlation between hope and spirituality, with most women who presented with high spiritual wellbeing also exhibiting high levels of hope [67]. This demonstrates how important spiritual beliefs and practices are in helping people deal with difficult life situations.
Additionally, the majority of the male and female respondents indicated a willingness to quit smoking and stop alcohol consumption to enhance fertility. Following an extensive study conducted by the Office of the Surgeon General, smoking increases the incidence of primary and secondary infertility in women [4, 68, 69]. This indicates that men and women are aware of the effects smoking and alcohol consumption have on fertility and how cessation thereof can assist in improving their fertility.
Similarly, both male and females stated their willingness to incorporate exercise and a specific diet into their routines to improve fertility. According to research, good fertility outcomes for both men and women are linked to a healthy, balanced diet high in fruits, vegetables, whole grains, and protein [70, 71]. These results indicate that both men and women are willing to make lifestyle changes to improve their fertility and that they understand the impact and advantages of a balanced diet on their fertility.
Lastly, the study found that most females reported a preference for over-the-counter medications to enhance fertility, whereas most males favoured the use of traditional medicine. These findings were contrary to those noted in Saudi Arabia and Ghana, where most respondents were unwilling to use over-the-counter medication and preferred alternative or traditional medication [72]. The use of complementary and alternative medicine, especially herbal and alternative supplementation for fertility support and preconception care, is growing in popularity [73]. Research shows that the use of herbal or traditional medicines in Africa and Asia is prevalent [74]. In a Zimbabwe study where experiences of women with infertility using traditional healthcare services were explored, the authors found that most women make use of herbal or traditional medicines before consulting with a healthcare professional [73]. This is alarming as it means that most men and women consume traditional medicine without evaluating the safety and efficacy of these medications [75, 76]. Although it is important to acknowledge that some men and women might prefer alternative supplements and/or traditional medicines, it is important for men and women to approach the use of traditional medicine with caution. This can be achieved by taking these medicines under the guidance of a professional.
6. LIMITATIONS
The potential limitation of the study includes limited generalizability due to the sample being restricted to specific regions or groups within Tshwane. Respondents may not represent the diversity of South Africa's broader population. The fact that this study was focused on PHC clinics in a particular geographic area may have limited its relevance to other settings or regions. Additionally, males were underrepresented in the sample, as most respondents were females.
CONCLUSION
This study investigated the knowledge, attitudes, and practices of men and women regarding infertility in three selected Primary Health Care (PHC) clinics in District One, City of Tshwane, Pretoria, South Africa. The findings indicate that while most respondents understood key infertility factors, such as ovulatory dysfunction, semen abnormalities, and reproductive tract infections, their awareness of the link between menstrual irregularities and fertility is limited. This indicates the importance of addressing infertility through targeted public health interventions in the City of Tshwane. Additionally, there are still misconceptions and cultural beliefs that infertility is caused by supernatural forces. These results highlight the importance of culturally appropriate reproductive education, which includes scientific information while respecting specific cultural and religious beliefs, customs, and practices.
Most respondents viewed infertility as an illness, with some considering it even a disability. While adoption is mainly accepted among women, male respondents were less supportive of it. Most male respondents were in support of polygamy as a solution to infertility. Most couples prioritize gynaecological consultations over urological assessments. These results highlight the need to incorporate male reproductive health into traditional fertility treatment protocols as well as offer gender neutral infertility education.
Lastly, despite all the differences, the study also highlighted similar gender perception differences regarding infertility. Both men and women expressed a willingness to adopt healthier behaviours to improve fertility, including dietary changes, cessation of smoking and alcohol consumption, as well as increased physical activity. Furthermore, an overall positive attitudes towards fertility treatments, such as IVF, fertility supplements, and medications, were mainly favoured by women, while most men prefer making use of traditional medicine. Differences in how communities view options such as adoption, use of traditional medicine, and the focus on women’s health over men’s when seeking help for infertility show that education around this issue needs to be more inclusive and sensitive to both genders. These different points of view highlight the importance of gender-sensitive health promotion strategies and inclusive educational programs in facilitating collaborative decision-making in couples as well as equal access to care.
Misinformation—such as thinking infertility is a disability or caused by supernatural forces—highlights the need for reproductive health services that are considerate of cultural beliefs while still providing accurate information. By raising awareness and encouraging both men and women to equally seek informed care, the stigma surrounding infertility can be reduced while empowering communities with information that will assist them in making more informed choices when dealing with infertility. Health education programs can eliminate myths with clear, understandable information while still acknowledging and respecting cultural norms and traditional beliefs. Public health campaigns have the potential to reduce stigma, promote accountability, and empower communities to make well-informed choices on reproductive health by increasing knowledge and awareness of infertility and encouraging men and women to seek timely and informed care.
In conclusion, tackling infertility in this setting requires a multifaceted public health approach that includes thorough, culturally aware health education in PHC while increasing community involvement. In South Africa and other settings, these strategies can assist in lowering stigma, debunking myths, encouraging shared responsibility in reproductive health, and eventually increasing access to fair infertility services.
RECOMMENDATIONS
The study underscores the need for fertility awareness programs, comprehensive medical evaluations, and culturally inclusive health education to dispel misconceptions, reduce stigma, and improve access to reproductive healthcare. Enhancing infertility awareness requires targeted education, culturally sensitive campaigns, and integrated medical care for both partners. Addressing stigma through psychosocial support, promoting healthy lifestyles, and regulating traditional medicine can improve outcomes. Policy reforms and research are essential to recognize infertility as a public health priority and expand access to care. The findings of this study stress the necessity of fertility promotion efforts through medical examinations and culturally sensitive health education interventions to alleviate misunderstandings and lessen stigma while enhancing access to reproductive healthcare. Enhancing infertility awareness requires targeted education, culturally sensitive campaigns, and integrated medical care for both partners. Results can be improved by encouraging healthy lifestyles, controlling traditional medicine, and addressing stigma with psychosocial support. To increase access to fertility care and acknowledge infertility as a public health concern, research, policy development, and changes are crucial.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: V.M.: Study conception and design; A.M.: Analysis and interpretation of results; M.R.M, N.V.S.: Draft manuscript; All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| IBM | = International Business Machines |
| PCOS | = Polycystic Ovarian Syndrome |
| PHC | = Primary Health Care |
| SA | = South Africa |
| IVF | = In Vitro Fertilization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the University of Pretoria’s Faculty of Health Sciences Research and Ethics Committee and the Gauteng Province Research Committee under the following ethics approval reference numbers: University of Pretoria 190/2023 and Gauteng Province 61/2023.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Both written and verbal consent were obtained from all the study participants.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the University of Pretoria Data repository site on the following link: URL and reference: https://doi.org/10.25403/UPresearchdata.26926699.v1.
ACKNOWLEDGEMENTS
The researcher would like to thank the Gauteng Department of Health and the City of Tshwane’s primary healthcare clinics for granting permission to use their premises for the purpose of conducting this study.
DISCLOSURE
Part of this article has previously been published in the thesis “Knowledge, Attitudes and Practices of Men and Women Regarding Infertility in the City of Tshwane, Pretoria, South Africa.” https://repository.up.ac.za/items /1cc6f9db-5297-4d5b-b5b6-c8b0beae58c0


