All published articles of this journal are available on ScienceDirect.
Investigating the Perceptions and Attitudes of Tertiary Students Towards Female Condom Use in South Africa: A Quantitative Study
Abstract
Introduction
Female condom usage in South Africa remains significantly low despite ongoing public health initiatives. Tertiary students, a sexually active and at-risk group, face cultural, social, and informational barriers that hinder the adoption of female condoms. This study aimed to investigate the cultural, personal, and social perceptions of students at the University of Venda regarding female condom use.
Methods
The researcher used a cross-sectional descriptive design spanning February 2022 until April 2024 at a South African tertiary institution. The study was conducted at a tertiary institution in Limpopo province. Using a systematic sampling method, 386 students completed a self-administered questionnaire. Data were analysed using SPSS Version 29 to generate descriptive statistics and weighted averages, particularly for Likert-scale responses.
Results
Only 6.88% of students reported ever using female condoms, compared to 45.55% for male condoms. The majority (76.7%) lacked knowledge on how to use female condoms. Cultural discomfort with discussing sexual matters, particularly with parents, was prevalent (74.4%). Social stigma also emerged, with over 60% unwilling to collect female condoms publicly. Most students (88.9%) had never initiated female condom use during their first sexual encounter.
Discussion
Findings indicate that a combination of cultural taboos, misinformation, and social barriers contributes to the underuse of female condoms. Despite openness to safer sexual practices, students experience low confidence and limited institutional support in using female condoms. Theoretical alignment with the Health Belief Model and Theory of Planned Behaviour helps explain the psychosocial and behavioural dynamics observed.
Conclusion
This study emphasises how important it is for higher education institutions to have thorough, gender-sensitive sexual health programs. Reducing stigma, encouraging open communication, and incorporating hands-on training on female condom use are some of the practice implications. To enable students, particularly women, to make knowledgeable, independent decisions regarding their sexual and reproductive health, public health policymakers and university stakeholders should work together to normalise the use of female condoms.
1. INTRODUCTION
Lasse Hessel invented the female condom, which was authorised in 1993 to prevent sexually transmitted infections (STIs) and unintended pregnancies during sexual activity [1]. The primary purpose of female condoms is to provide women with the power and platform to shield themselves against Sexually Transmitted Infections (STIs), Sexually Transmitted Diseases (STDs), and unplanned pregnancies [2]. The use of female condoms in South Africa, as in many parts of the world, has been promoted as part of efforts to decrease the number of STIs and unwanted pregnancies [3]. The South African government, along with healthcare organisations and various NGOs, has launched campaigns to increase awareness about female condoms and promote their use. These initiatives aim to provide access to female condoms, educate people on their correct usage, and reduce the stigma associated with them [4]. According to the World Health Organisation (WHO), among 39.4 million HIV-positive individuals, 16.9 million were males, and 19.7 million were females, which makes them the largest population living with HIV [5]. South Africa first launched the female condom in 1998; currently, female condoms are used at a lower rate than male condoms by people under the age of twenty years. An estimated 8% of young women and 6% of young males are found to prefer using female condoms [6]. However, it is crucial to recognise that attitudes are dynamic and can change with proper education, awareness, and resource access. Subsequently, it is essential to explore some factors that may influence cultural attitudes toward female condoms, including gender dynamics, stigma, and religious and moral beliefs.
The cultural norms of male dominance in the home and in relationships expose women to less control or participate in making decisions on the use of condoms during sexual activity [3]. Another viewpoint that leaves women open to risk factors for STIs, STDs, and unintended pregnancies is the notion that using a condom while having sex with your spouse is when one is married [3]. Female students view condoms as reducing HIV transmission and are more inclined to negotiate their usage [2]. This denotes that successful implementation requires a multifaceted approach that considers the unique characteristics and needs of the student population. It's also essential to involve students themselves in the planning and execution of the program to ensure their voices are heard and their preferences are considered.
Most students in tertiary institutions are assumed to understand the significance of using a condom during sexual encounters, as well as the significance of female condoms, which is to empower women to defend themselves against STIs and STDs if their male partners refuse to use a male condom [4]. In 2020, Vhembe District had 64,327 persons who had HIV and AIDs, with Limpopo reporting 5954 teenage pregnancies birthed by teens between ten and seventeen years old [7]. According to a report done at Mopani, about 37 students were pregnant in 2017, and two teenagers between the ages of 14 and 16 were found pregnant at Mopani Primary School [7]. According to a study done at the University of Limpopo, students show interest in the usage of women's condoms; however, their inaccessibility in comparison to male condoms, lack of awareness about the usage of female condoms, cost and procurement in pharmacies have led to the underuse of female condoms at the tertiary institution [8]. South Africa initiated programmes addressing the social and structural factors exposing young girls and boys to vulnerability and increased risky behaviours. These programmes include She Conquers, YOLO, and Zazi, which are development programmes facilitated by the Department of Social Development [9]. However, more proper education and training on using female condoms are still needed to ensure their effective and consistent use.
There is a dearth of data regarding students’ perceptions of the use of female condoms in South Africa. Most of the research undertaken in South Africa centred around challenges regarding using condoms for both men and women, factors contributing to STIs, teenage pregnancy, attitudes, sexual behaviour regarding adolescent pregnancy and reproductive problems, and students at Training College engaging in risky sexual conduct [10, 11]. However, there is a study that was done at the University of Limpopo focusing on the perspective of female condom usage among postgraduate students. This study revealed that the reported discarding and abuse of women's condoms among students relates to a lack of information and views about it. It was further discovered that effective initiatives and campaigns to promote student understanding are required to reduce unnecessary costs in the acquisition and delivery of female condoms [8]. As a result, this study was conducted to fill this gap by exploring the perceptions of students (undergraduate and postgraduate) on the usage of female condoms in institutions of higher education at the selected tertiary institution.
2. OBJECTIVES OF THE STUDY
The objectives of this study were to:
- Describe the cultural perceptions of students regarding the use of female condoms at the University of Venda.
- Identify the personal perceptions of students regarding the use of female condoms at the University of Venda.
- Determine the social perceptions of students regarding the use of female condoms at the University of Venda.
3. METHODS
3.1. Study Design
In this study, the researcher employed a quantitative analysis to ascertain the perceptions of students about the usage of female condoms. The researcher used a cross-sectional descriptive design to gather data quickly and reach a vast population. The researcher distributed the questionnaire to each respondent simultaneously while employing this technique. This enabled the researcher to get a large population quickly while obtaining relevant data to achieve the research objectives.
3.2. Study Setting
The study was conducted at an institution of higher learning in Limpopo province. Limpopo Province is one of South Africa's nine provinces, with two universities. Limpopo is located in the northern region of South Africa. Limpopo province covers 10.3% (125,755 square kilometres) of South Africa's total land area. There are five regions: Capricorn, Mopani, Sekhukhune, Vhembe, and Waterberg. The Limpopo provincial economy is the sixth biggest in the nation, with a GDP of R224 billion.
On the other hand, Limpopo has less human development than other provinces due to its rural nature. Teenage pregnancy proportions increased from 2% at 15 years to 27% at 19 years, with 71% being unwanted pregnancies and 29% wanting pregnancy [12]. Limpopo had a termination of youth pregnancy from 12.1% to 12.9% between the years 2017 and 2019 [13]. Limpopo province has 91.66% of individuals diagnosed with HIV, and 73.26% of those individuals are on Anti-retroviral treatment [14].
The selected tertiary institution has four faculties and 13 residences, accommodating about 3,826 male and female students on campus. There are accredited residents outside the campus who accommodate other students. The selected tertiary institution encompasses 21,000 km and has 14,949 students [15]. The chosen tertiary institution has one leading clinic that provides primary healthcare services, and private and public healthcare facilities are close to campus.
3.3. Population
The target population is 3826 male and female students residing on campus. The population-based frame used in this study was all female and male students currently enrolled with the selected tertiary institution and residing in the campus residences. These students stay on the campus and share the same characteristics.
3.4. Sampling
The researcher used a systematic or interval sampling method. Using Slovin's formula, the researcher calculated the sample size. The calculation formula used was n=N/ (1+Ne2). The researcher was using a confidence level of 95%. After Slovin's recommended sample size, the researcher added 10% to the given sample size. The addition of 10% was necessary so that it could cover the respondents who may not have finished the questionnaire and improve and strengthen the reliability and validity of the findings. The sample size found was 398. The study interval was calculated as 9, which was used to select participants' rooms and reduce selection bias. The sample size was 398, of which only 386 participants were considered, as other questionnaires were dismissed as they were incomplete. The target population was 3826 students residing on campus, both male and female students. The University of Venda had 14,949 students in 2023, and the students the researcher chose to sample were students residing on the campus, a total of 3,826 students. Hence, it limits the generalizability of the findings to the broader student body: N= 3826/ (1+(3826) (0,05)2 N=362,139. N=362. 10% of 362=36.2.
3.5.Inclusion Criteria
To be enrolled in this research, each responder had to be registered as a student at the selected University, staying on campus,18 years old and above, and provide a signed consent form.
3.6. Exclusion Criteria
In this study, all respondents who refused to sign a consent form decided not to answer the questionnaire, and those who resided off-campus were also excluded.
3.7. Data Collection
The instrument the researcher used to gather data was a structured questionnaire with closed-ended questions. Before data collection, the researcher obtained ethical clearance and a permission letter from the director of residents. The permission letter was used to enter the students' residence. The researcher went door to door to the respondents' rooms, gave them informed consent, and read the information letter. The questionnaire was composed of 40 items. The reason for this questionnaire was to gather pertinent data for the study concerning tertiary students' opinions about the usage of female condoms at the University of Venda. The study's objectives informed the development of the self-administered questionnaire, formulated after a review of related literature. The researcher developed the questionnaire using English, the medium of instruction at the selected tertiary institution. It was made up of four sections: Section A: Demographic characteristics of respondents; Section B: Cultural perceptions of students regarding the usage of female condoms; Section C: Social perceptions of students regarding the usage of female condoms; Section D: Personal perceptions of students regarding the usage of female condoms. The variables used in this study were: outcome variable: female condom use (measured by self-reported yes/no), predictors: age, gender, educational level, relationship status, potential confounders: access to condoms, sexual health education exposure. Effect modifiers of gender differences in attitudes towards use were analysed. In this study, the diagnostic criteria do not apply.
3.8. Data Analysis
In this study, descriptive statistics were employed by the researcher through Statistical Package for the Social Sciences (SPSS) version 29.0.2.0 to describe and summarise data in meaningful and valuable ways. The researcher used frequency distribution, relationship measures, and central tendency measures to analyse data. Frequency distribution was used to analyse data and summarise the occurrence of results. Sensitivity analyses were not considered necessary because of the exploratory nature of the study and its small sample size. Weighted averages in this study were applied to responses from the Likert scale items to determine participants' overall positive or negative perceptions. The researcher calculated the mean of each table and then decided by comparing the average mean and the cut-off points, which made it easier to decide if the perception was negative or positive. Scores closer to 1 indicated negative perceptions, while scores closer to 5 indicated positive perceptions. A cut-off point was determined by the mean of each table, as shown in the table, to distinguish between overall negative and positive perceptions.
4. VALIDITY AND RELIABILITY
4.1. Validity
The researcher used face and content validity. To ensure content validity was established, the supervisors examined whether the questions covered areas under the study. Healthcare workers and health youth representatives assessed the questionnaires to make sure the questionnaire covered the area under study. The researcher used the comments from the questionnaire's validity assessment to modify it to measure the intended parameters.
4.2. Reliability
The researcher used the test-retest method to measure the instrument's reliability and ensure that the instrument yielded reliable answers. The researcher distributed the questionnaire to 10% (36 students) who did not form part of the study. The questionnaire was distributed to the same respondents on two occasions, five days apart, to avoid memorising the answers. The researcher checked whether the respondents' responses were missing or wrong by measuring the degree of relationship through the correlation coefficient. The researcher used the Cronbach's alpha test to assess the reliability of the device by measuring the correlation coefficient. The correlation coefficient was tested with Cronbach's alpha; the results were 0.725, indicating the questionnaire's reliability.
4.3. Ethical Considerations
The researcher presented the proposal to the supervisor and the public health department. The research was then assessed at the Faculty of Health Science for quality standards. The ethical clearance (FHS\23\PH\ 45\3011) was obtained from the selected University. With the approval of the student affairs, informed consent was given by the researcher to the respondents to sign and read the information letter.
5. RESULTS
5.1. Demographic Characteristics of Respondents
In total, 398 questionnaires were handed out to the respondents in different residences at the selected tertiary institution campus. A total of 386 questionnaires were captured using SPSS version 29.0.2.0; some of the questionnaires were not included as some were not fully answered. The mean age of respondents was 20.88, while 53.4% (206) of respondents were females and 46.6% (180) were males. The youngest respondents were 17, and the oldest was 26. Three hundred forty-six students were found to be single. Most respondents were first-year students, with 40.9%, followed by second-year students. Approximately 287 students were found to be sexually active, and 99 students were found to be not sexually active. Religiously, most participants were Christians (72,5%). Undergraduates (78%) were the most dominant respondents who answered questionnaires. Most respondents were from the faculty of science, agriculture, and engineering, with 37.6% (145), followed by the faculty of humanities, with 31.1% (124). Table 1 provides the demographic distribution of the respondents involved in the study. Most of the students who participated were age 19 (18.9%), followed by age 20 (15.5%), age 21 (13.7%), then others 18, 22, 25, 26, 22, 23, 17, then last 17 in order. (Table 2). The minimum age that took part in this study was 17, and the oldest was 26 years, with the mode being 19 years (Table 3). The histogram of the age of respondents in Fig. (1) shows that most participants are in a specific age group, with the majority between 20 and 24 years old.
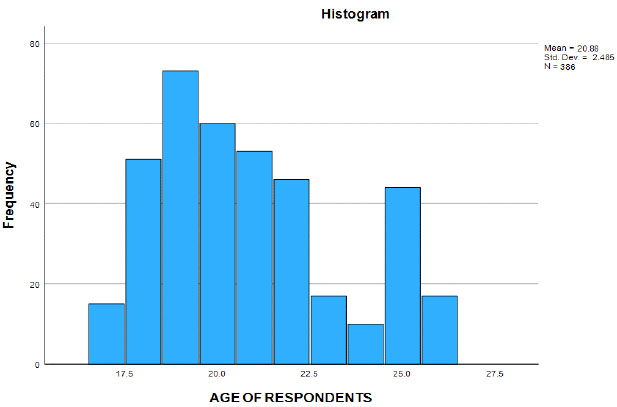
Histogram of the age of respondents.
| Demographic and clinical characteristics (NO = 386) | ||
|---|---|---|
| Characteristics | NO | Percentage |
| Gender: Male Female Other |
180 206 0 |
46,6% 53,4% |
| Marital status: Single Never married |
346 40 |
89,6% 10,4% |
| Level of study: 1st level 2nd level 3rd level 4th level |
158 121 87 20 |
40,9% 31,3% 22,5% 5,2% |
| Religion: 1. None 2. Christianity 3. African tradition 4. Other |
40 280 54 12 |
10,4% 72,5% 14,0% 12% |
| Type of degree: 1. Postgraduate. 2. Undergraduate |
85 301 |
22,0% 78,0% |
| Field of Study: 1. Faculty of Health 2. Faculty humanities, social and educational 3. Faculty of management 4. faculty of science, Agric and engineering |
47 124 70 145 |
12,2% 31,1% 18,1% 37,6% |
| Sexually active: Yes No |
287 99 |
74,4% 25,6% |
| Method of contraception: 1. Female condom 2. Male condom 3. Contraceptive injection 4. Contraceptive pills 5. Withdrawal method 6. Morning after pill 7. Does not prevent 8. Other |
34 225 15 12 63 38 77 30 |
6,88% 45.55% 3,04% 2,43% 12,75% 7,69% 15,59% 6,07% |
| Age | Frequency | Percentage % | Cumulative Percent |
|---|---|---|---|
| 17 | 15 | 3.9% | 3.9 |
| 18 | 51 | 13.2% | 17.1 |
| 19 | 73 | 18.9% | 36.0 |
| 20 | 60 | 15.5% | 51.6 |
| 21 | 53 | 13.7% | 65.3 |
| 22 | 46 | 11.9% | 77.2 |
| 23 | 17 | 4.4% | 81.6 |
| 24 | 10 | 2.6% | 84.2 |
| 25 | 44 | 11.4% | 95.6 |
| 26 | 17 | 4.4% | 100.0 |
| Total | 386 | 100.0% |
| N Valid data | 386 |
|---|---|
| Missing data | 0 |
| Mean | 20.88 |
| Std. Error of Mean | 0.126 |
| Median | 20.00 |
| Mode | 19 |
| Std. Deviation | 2.485 |
| Variance | 6.177 |
| Range | 9 |
| Minimum | 17 |
| Maximum | 26 |
5.2. Condom Usage
Total condom usage was found to be 52.43% (225), and male condoms had higher usage, 45.55%, which is six times more used than female condoms at 6.88% (34). Female condom usage is exceptionally low compared to the number of male condoms used. The male condom was found to be the most used preventive method compared to other contraceptives. Students who did not engage in preventive methods were 15.59% (77), which can also be attributed to the number of students who are not sexually active. Students who engaged in the withdrawal method were 12.75% (63), meaning they engaged in risky sexual behaviour. Most of these respondents were found to be single, which means they may have more than one partner, as they were found to be more engaged in sexual intercourse (Table 1).
This study used the weighted average compared to the item to make decisions regarding respondents’ perceptions. The weighted average value for the items was divided by the total number of items. Any weighted average higher than the weighted average equal to the average is considered high perception for items with a low weighted average, which is taken as low perception. For the Likert scale questionnaires, the researcher used a range of means for the item to fall under strongly agree. The required mean values are as follows: strongly disagree 3.25–4, disagree 2.50-3.24, agree 1.75–2.49), and highly agree 1.00–1.74.
| 1. yes | 2.no | 3. unsure | |
|---|---|---|---|
| 1. Can you ask your parents/Guardian how to use a female condom? | 55 (14,25%) | 287 (74,4%) | 44(11,4%) |
5.3. Cultural Perception
Most respondents had negative perceptions about discussing with their parents or guardians how to use a female condom, with 74.4% saying no, (Table 4). Table 5 indicates that most of the respondents strongly disagree with the notion of discussing sexual matters with their parents. Respondents had a low perception and disagreed with the statement of not discussing sexual issues with elders, as it is deemed a secret. The respondents also disagreed that if you are married, you cannot use a condom. Respondents had strong disagreement that the power to use a condom lies in the man's hands.
5.4. Social Perception
In Table 6, data analysis of respondents in social perceptions, most respondents felt they could not collect female condoms in front of people (60.4%), and 86.8% of students indicated peer opinions or behaviours had never influenced them regarding the usage of a female condom. Students showed a high perception of the comfort of giving female condoms to friends. Overall, there is a moderate level of comfort among respondents regarding sharing female condoms with friends. Respondents, on average, disagree with the statement of friends suggesting not to use condoms to build trust; they disagree with the notion that female condoms have the potential to become stuck in the vagina, but show a low perception of the statement as the mean is lower than the weighted average (Table 7).
A majority of respondents had never started using female condoms during their first sexual encounter (88.9%), and 76.7% did not currently know how to use them, according to the results on personal experience with female condoms. The majority of participants said they had never experienced difficulties using a female condom (84.7%) or thought their partners would assume they had HIV/STI if they used one (87.8%). Just 13.7% of respondents said they preferred using a condom, while a smaller percentage (37%) said it decreased sexual pleasure (Table 8). Respondents' own attitudes toward partners were largely positive. For example, a significant portion of respondents argued that they could not begin the use of condoms (53.6%) and that implying their usage meant promiscuity (61.1%). A comparable pattern was noted for submissive relationship dynamics (64.3%). But 58.3% said they were aware of how to use it (Table 9).
| - | 1 Strongly agree | 2. Agree | 3. Disagree | 4. Strongly Disagree |
Mean | Standard deviation | Decision |
|---|---|---|---|---|---|---|---|
| 1. I discuss sexual matters with my parents. | 28(7,3%) | 60(15,5%) | 147(38,1%) | 151(39,1%) | 3.09 | 0.911 | High perception |
| 2. Sex is something secret that should not be discussed with elders. | 69(17,9%) | 110(28,5%) | 131(33,9%) | 76(19,7%) | 2.55 | 1.000 | Low perception |
| 3. If you are married, you cannot use a condom. | 52(13,5%) | 96(24,9%) | 129(33,4%) | 109(28,2%) | 2.76 | 1.008 | Low perception |
| 4. The power to use a condom lies in the man's hands. | 39(10,1%) | 52(13,5%) | 122(31,6%) | 173(44,8%) | 3.11 | 0.989 | High perception |
Responses to questions about awareness and availability inside institutions were not entirely consistent: 46.4% thought awareness was either ineffective or not addressed. In comparison, 23.3% thought awareness efforts were extremely effective, and 30.3% thought they were only moderately effective (Table 10).
According to more general personal beliefs, female condom use was thought to be moderately or strongly impacted by peer dynamics (58.3%) and gender inequity (59.5%). With slightly more than half (51.3%) acknowledging their influence, women's attitudes towards the female condom were also a significant factor (Table 11).
| - | 1. Yes | 2. No | 3. Unsure | Mean | Standard Deviation |
|---|---|---|---|---|---|
| 1. Can you collect female condoms in front of people? | 233 (60,4%) | 109 (28,2%) | 44 (11,4%) | 1.51 | 0.692 |
| 2. Have you ever felt influenced by peer opinions or behaviours regarding the use of a female condom? | 39 (10,1%) | 335 (86,8%) | 12 (3,1%) | 1.93 | 0.357 |
| 3. Are you comfortable giving female condoms to friends? | 185 (47,9%) | 115 (29,8%) | 86 (22,3%) | 1.74 | 0.799 |
| - | 1. Strongly Agree | 2. Agree | 3. Disagree | 4. Strongly Disagree |
Mean | Standard Deviation | Decision |
|---|---|---|---|---|---|---|---|
| 1. Have friends ever suggested that to build trust in a relationship, you must not use condoms with your partner | 43 (11,1%) | 49 (12,7%) | 198 (51,3%) | 96 (24,9%) | 2.90 | 0.902 | High perception |
| 2. Female condoms can get stuck inside the vagina | 21 (5,4%) | 152 (39,4%) | 170 (44,0%) | 43 (11,1%) | 2.61 | 0.756 | Low perception |
| 1. Yes | 2.No | Mean | Standard Deviation | |
|---|---|---|---|---|
| 1. Have you ever initiated the use of a female condom on your first encounter? | 43(11,1%) | 343(88,9%) | 1.89 | .315 |
| 2. Are you currently aware of how to use a female condom | 90(23,3%) | 296(76,7%) | 1.77 | .423 |
| 3. I can't use a female condom because my partner may think I have STI/HIV. | 47(12,2%) | 339(87,8%) | 1.88 | .327 |
| 4. Have you personally faced any challenges in using female condoms | 59(15,3%) | 327(84,7%) | 1.85 | .360 |
| 5. Do you believe that a female condom takes away pleasure during sex | 143(37,0%) | 243(63,0%) | 1.63 | .484 |
| 6. Do you prefer a female condom | 53(13,7%) | 333(86,3%) | 1.86 | .345 |
| - | 1. Strongly Agree | 2. Agree | 3. Disagree | 4. Strongly Disagree | Mean | Standard Deviation | Decision |
|---|---|---|---|---|---|---|---|
| 1. I cannot suggest and initiate the use of a female condom to my partner | 34 (8,8) | 145 (37,6) | 142 (36,8) | 65 (16,8) | 2.62 | .867 | High perception |
| 2. If I suggest the use of a female condom, they may think I have started to sleep around | 56 (14,5%) | 94 (24,4%) | 170 (44,0%) | 66 (17,1%) | 2.64 | .930 | High perception |
| 3. Being in a submissive relationship led to me not using a condom | 51 (13,2%) | 87 (22,5%) | 162 (42,0%) | 86 (22,3%) | 2.73 | .953 | High perception |
| 4. I don't have any knowledge of how to use the female condom | 85 (22,0%) | 140 (36,3%) | 105 (27,2%) | 56 (14,5%) | 2.34 | .979 | Low perception |
| - | Very Effectively | Moderately Effective | Ineffectively | Not Addressed at all |
|---|---|---|---|---|
| How is female condom awareness and availability addressed within your tertiary institution? | 90 (23,3%) | 117 (30,3%) | 79 (20,5%) | 100 (25,9%) |
| - | Significantly | Moderately | Slightly | Not at all | Mean | Standard Deviation |
|---|---|---|---|---|---|---|
| 1. What extent do you think peer dynamics influence perceptions of female condom usage in higher education settings? | 118 (30.6%) | 107 (27.7%) | 71 (18.4%) | 90 (23.3%) | 2.34 | 1.143 |
| 2. What extent do you think gender inequality contributes to challenges in female condom usage | 99 (25,6%) | 131 (33,9%) | 70 (18,1%) | 86 (22,3%) | 2.37 | 1.093 |
| 3. What extent do you believe men's attitudes influence female condom usage among females | 71 (18,4%) | 127 (32,9%) | 120 (31,1%) | 68 (17,6%) | 2.48 | .986 |
6. DISCUSSION
Tertiary institutions are essential members of the community as they contribute a lot to the number of people suffering from sexually transmitted diseases. Most students start to participate in sexual activities when they begin to move to University. It is essential to be knowledgeable about the female condom, as this may assist women in preventing sexually transmitted infections. When students are knowledgeable about the female condom, it may help them change their attitudes towards the female condom.
6.1. Theoretical Framing
Although this study did not initially employ a formal theoretical model, the findings of this study align with the health belief model and the theory of planned behaviour. These frameworks provide a useful perspective for interpreting the personal, cultural and social perceptions identified in this study.
The Health Belief Model focuses on how people view health risks and decide how to proceed based on how much they value a specific objective and how likely actions taken to achieve that objective will be successful [16]. Perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and cues to action are the six main cognitive constructs, “dimensions”, that impact behaviour [16]. In this study, the limited usage of female condoms and the widespread lack of knowledge of how to use them reflect perceived barriers. The discomfort and embarrassment of obtaining them publicly reflect psychosocial barriers. The low perceived risk of HIV or pregnancy among students may reduce perceived susceptibility.
A social psychologist's theory, the Theory of Planned Behaviour (TPB), describes how personal factors affect people's choices to engage in certain behaviours, including health-related ones [17]. It implies that intentions and perceived behavioural control (PBC) are the proximal determinants of behaviour. PBC is a person's expectation of control, whereas intentions are what drive them to work hard. Intentions have greater effects when PBC is strong and reflects actual control, according to the theory that control is a continuum [17]. In this study, negative attitudes towards female condoms, such as the belief that they reduce sexual pleasure or imply promiscuity, were observed. Subjective norms, such as peer opinions regarding sexual discussion, affect students’ female condom usage. A lack of confidence in using female condoms can also point towards perceived behavioural control. Incorporating these two theories enhances the interpretability of these findings.
In this study, the knowledge was insufficient, and some students had a bad attitude towards the use of female condoms.
This study noted that female condom usage was 6.88% and male condom usage was 45.55%, which is six times more than female condoms. A study conducted in Nigeria found similar disparities in condom usage between genders [18]. Cultural perception. The study's findings showed that most respondents had a negative perception of discussing with their parents or guardians how to use female condoms, with 74.4% saying no. The data analysis in Table 4 indicates that most of the respondents strongly disagree with the notion of discussing sexual matters with their parents. This concurs with the study performed on University of Sudan students, who reported that the respondents were not able to discuss sex with their parents as they were not close to them as friends [19]. Respondents had a low perception and disagreed with the statement of discussing sexual matters with elders, as it is deemed secret. This concurs with a study done in Cameroon that reported that most of those surveyed were sexually experienced and had positive perceptions regarding the family-adolescent discussion on whether condoms were appropriate [20]. This suggests that students are not willing to discuss their sexuality with elders, but do not have any cultural belief in not discussing sexual activities with their elders [19]. The study also found that respondents disagreed that if one is married, one cannot use a condom. This differs from the survey done six years ago, which suggested that people in long-term relationships do not use condoms, as it may show a lack of trust and faithfulness [21]. Respondents strongly disagreed that the power to use a condom lies in the man's hands. This supports the study by Firoza, who reported that female and male students had a positive attitude in negotiating condom usage [22].
6.2. Social Perception
According to the survey, most of the respondents felt they could not collect female condoms in front of people (60.4%). This result differs from the analysis done 13 years ago, which reported that female condom users who had positive experiences influenced others positively [23]. In the current study, 86.8% of students indicated that peer opinions or behaviours have never influenced them regarding the usage of a female condom. This concurs with the study conducted on African American women, which discovered that women are more inclined to use a female condom if they are aware of its benefits [24]. Students showed a high perception of the comfort of giving female condoms to friends. Overall, there appears to be a moderate level of comfort among respondents regarding sharing female condoms with friends. This result concurs with the study in 2014, which revealed that 69.4% said they would propose it to friends and peers [20].
Respondents, on average, disagree with the statement of friends suggesting not to use condoms to build trust; they also disagree with the belief that a female condom can get stuck inside the vagina. This study differs from the study conducted by Kenya high school students, who disclosed the existence of a close relationship between peer pressure and high-risk sexual behaviours among students [25]. Another study showcased that those ladies with a strong background in the insertion and usage of female condoms increased their utilisation [26].
6.3. Personal Perception
The study reported that 88.9% of respondents responded that they had never initiated the usage of a female condom on their first encounter, and 76.7% of respondents were not aware of how to use a female condom. This outcome is consistent with the study conducted in 1997, in which 231 people were instructed to use female condoms, and only 29% tried the condom, which showed most people are not open to trying the female condom on first encounter [27]. These results showed similarities to the study conducted in 2018, as it mentions that women often put on condoms before engaging in sexual activity, and occasionally, males may not show up even after the women have done so [28]. Most respondents showed that they are not afraid of using female condoms even if their partners may think they have an STI/HIV. This report agrees with a study conducted in 2016, which reported that most females used a condom when infidelity was suspected [29]. Respondents had a low perception regarding the statement, with 84.7% of respondents agreeing they had never faced any challenges in using female condoms. This result differs from the Italian study, which was conducted 16 years ago, as most respondents expressed difficulties with the insertion of female condoms, showing an inadequate understanding of their usage [30]. The high percentage of not facing challenges with the usage of female condoms could be associated with the results of most respondents not using female condoms in this current study. Respondents also disagreed that the female condom takes away pleasure. A study conducted at TVET College indicated that students discovered that using female condoms was more complex and less intriguing [4]. Many students do not prefer using a female condom. A study conducted at KwaZulu-Natal reported that female condoms interfere with sexual pleasure, which brought inconsistency to the use of female condoms [31].
The current study reported that students mostly agree that they cannot suggest the usage of a female condom to their partner, and showed a low perception. A study showcased that culturally open purchase of female condoms is perceived as promiscuity, as stated by 85% of the participants in the survey [32]. Some raised statements, such as initiating sexual matters, are male responsibility, which has led to being submissive to their men and accepting any decision they make, leaving their health at risk [32]. High perception on suggesting the usage of female condoms regarding the belief that their partners may think they have started to sleep around, mostly disagree. A study conducted in 2015 stated that the stigma attached to using female condoms fuels unfavourable opinions and may imply adultery in committed partnerships [33]. Students also disagreed that a submissive relationship led to their not using a condom. This result differs from a study conducted at Kenyatta University, where respondents expressed that it is a man's responsibility to initiate sexual matters, which makes women submissive to their men [28]. Students showed positive perception regarding knowledge on the usage of female condoms, as they also agreed that they do not have any knowledge on how to use them. Another study conducted in KwaZulu-Natal also concurs with these results, as it reported that women believed that there was a dearth of information and understanding about female condoms [33].
The current study shows that 30.3% of students expressed that female condom awareness and availability are moderately effectively addressed within their tertiary institutions. This shows the similarity to a study done 11 years ago that University-age young adults continue to have mixed attitudes and understanding on condoms being made available among several populations at risk of HIV in South Africa, encompassing young people [32]. This result also concurs with the study done in 2019, which revealed one factor influencing usage was whether female condoms were available where one lived, as the survey reported that 98% verbalised that female condoms were not readily available [34].
In this study, students indicated that peer dynamics influence perceptions of female condom usage in higher education settings significantly, and 33.9% of students believe gender inequality moderately contributes to challenges related to female condom usage. According to Kenyan research, young women who feel their friends use contraceptives are more inclined to use another contemporary technique than not to use any at all [35]. In a study conducted in Zimbabwe, peer support can strongly encourage potential users to consider the female condom [36]. Many respondents showed fair perceptions that the belief in the men's attitudes moderately influences female condom usage among females. A study done in 2019 reported that 66.4% of males have reported they disliked female condoms; this has led females to shy away from female condoms, thinking of how their male partners will react when they find out about the condom [34]. In this study, 11.1% students were found to have ever initiated the use of female condoms, which is very low. This study concurs with the study done in Nigeria, which highlighted that almost 8.9% students have ever used female condoms [18]. Most of the students disagreed that they did not use female condoms because their partner may think they have an STI (76.7), which differs from a study done in 2022, which showcased that partner stigma for acceptance was another barrier for female condom usage [37]. This study also highlighted that 84.7% have difficulty inserting female condoms and have a low preference for the usage of female condoms, which concurs with a study done in 2014, which highlighted that students face challenges with cost and difficulty with its insertion and low usage [18]. The difficulty of inserting a female condom can be attributed to a lack of knowledge on how to use it, as most students agreed they are not knowledgeable about it (58,3%). This study showed confidence of students in suggesting female condoms, as the students disagreed that suggesting female condoms may lead to their partners having a bad perception about them, such as believing they have started sleeping outside. These results differ from the study done in Dodoma, as students fear being labelled promiscuous and the stigma of STI [38]. Most students in this study (64.3) revealed that being in a submissive relationship has never led them to not use a condom, which does not agree with the study done in 2011, as it revealed that the theory of gender and power highlights inequitable relationship dynamics which tend to reduce protective behaviour [39]. Almost 50% students felt female condom awareness and availability are not addressed well, which supports the study done in KwaZulu-Natal, where students reported inadequate supply and lack of institutional attention to female condoms [33]. This study also revealed that peer dynamics influence most students (58,3%) in their perception of female condom usage. A study conducted in 2015 also revealed that peer influence was a major facilitator that shapes the usage of female condoms [40]. Most students believe that gender inequality contributes to challenges in female condom usage, which also concurs with a study done in 2023, which found that harmful gender norms strongly limit female condom usage and also hinder condom negotiation [41]. The results of this study highlighted that male attitudes influence condom usage among females the most. Another study done in 2022 revealed that male acceptance is one of the top barriers to its usage, while a study done in Cape Town differs with these results as it suggests that some males found female condoms easier to use [37, 29].
7. LIMITATIONS OF THE STUDY
This study has limitations regarding the sample size of students in the selected tertiary institution. This led to the study analysis of the perception of a small percentage of the students. Response bias might have been introduced by using self-reported data, particularly when discussing delicate subjects. Furthermore, inferences regarding causality are not possible due to the cross-sectional design. The generalisability of this study is limited due to its single-institution design and use of convenience sampling. As the participants were drawn from one tertiary institution, the findings may not reflect the country's broader population of university students across different regions, institutions, or cultural contexts. The cross-sectional, self-reported design could introduce bias and prevent causal conclusions. Future researchers should include more diverse samples, multiple sites and mixed methods to strengthen findings.
CONCLUSION
The study reveals that social stigma, cultural discomfort, and lack of knowledge significantly hinder the use of female condoms among tertiary students at the University of Venda. Many participants expressed openness to gender-equitable condom negotiation, but low confidence in initiating female condom use and a scarcity of targeted awareness campaigns within their institutions limited their participation. The findings highlight the need for universities and public health stakeholders to invest in structured and inclusive sexual health education, addressing misconceptions about female condoms, promoting open communication, and empowering students, particularly women, to take control of their reproductive health. Universities should incorporate comprehensive, evidence-based sexuality education into their curricula, focusing on the use and benefits of female condoms. Campus clinics and health programs should ensure that female condoms are readily available, accessible without stigma, and promoted equally alongside male condoms. Public health policymakers can use this study's findings to guide national strategies for female condom distribution and education among youth. Future research should incorporate larger and more diverse samples, apply inferential statistical methods, and explore qualitative dimensions to deepen understanding.
AUTHORS’ CONTRIBUTIONS
M.C.R.: Conducted this study while completing a master's in public health (occupational and environmental health) at the University of Limpopo;. M.C.R.:, The researcher, contributed fully to the study's design and implementation, the analysis of the results, and the manuscript;. N.S. M.: Acted as a supervisor and supervised all aspects of the study, including revising, editing, and administering the study.
LIST OF ABBREVIATIONS
| STIs | = Sexually Transmitted Infections |
| STDs | = Sexually Transmitted Diseases |
| WHO | = World Health Organisation |
| HIV | = Human Immunodeficiency Virus |
| TPB | = Theory of Planned Behaviour |
| PBC | = Perceived Behavioural Control |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The ethical review committee of the University of Venda, South Africa was responsible for revising the research proposal. Data was collected after ethical approval was obtained (ethical clearance number: FHS\23\PH\45\3011).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
The respondents were informed that responding to the survey was completely voluntary and that they could stop answering the questionnaire at any time if it caused discomfort. They can voice concerns on the questionnaire if they need clarification on any points. Following an appropriate interaction between the researcher and the respondents, each respondent received and signed a consent form attesting to their readiness to engage in the study. The responders were informed precisely of what was expected of them by the researcher. Publication of this study was also obtained while the researcher was collecting the data.
AVAILABILITY OF DATA AND MATERIAL
The data sets used and/or analysed during this study are available from the corresponding author [M.R] upon request.
CONFLICT OF INTEREST
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
ACKNOWLEDGEMENTS
The researcher would like to acknowledge the University for ethical clearance for this project. The researcher also thanks the students/respondents of the selected tertiary institution for contributing to this research project.


