All published articles of this journal are available on ScienceDirect.
Enhancing Virtual Learning in Medical Education: Strategies Emerging from the COVID-19 Pandemic in Iran
Abstract
Introduction
The COVID-19 pandemic significantly disrupted medical education, forcing institutions worldwide to adopt virtual learning solutions. In Iranian medical universities, this transition posed challenges due to limited digital infrastructure and a lack of prior experience with online education. This study aims to identify and prioritize effective strategies for enhancing virtual learning in medical education, guided by the Blended Learning Model, which integrates online and face-to-face teaching methods.
Methods
A mixed-methods approach was employed in 2023. In Phase 1, a systematic review was conducted to extract best practices in virtual learning from the global literature. In Phase 2, a modified Delphi method was used to build expert consensus. Twelve experts, including medical educators, policymakers, and researchers, were purposively sampled. To minimize bias, experts from diverse fields and institutions were included, and the anonymity of responses was ensured. The Delphi process consisted of two rounds: (1) qualitative refinement of 62 initially identified strategies and (2) quantitative evaluation of 45 refined strategies using the FAME framework (feasibility, appropriateness, meaningfulness, effectiveness).
Results
The highest-rated strategies included the integration of social networks as educational tools, the development of an online IT support system, the pre-assessment of students before virtual learning interventions, the provision of psychological support services for students, the enhancement of server capacity and cybersecurity measures, and the implementation of flexible assessment methods (e.g., replacing final exams with continuous evaluation).
Discussion
Adopting blended learning strategies can enhance the sustainability and effectiveness of virtual medical education.
Conclusion
This study highlights the need for investment in digital infrastructure, faculty training, and student support services to optimize virtual learning experiences. Future research should assess the long-term impact and cost-effectiveness of these strategies across diverse educational settings.
1. INTRODUCTION
The COVID-19 pandemic has had a significant impact on global education systems, particularly in medical education, where practical training and face-to-face interaction are crucial. South Korea, Italy, and Iran were among the countries most severely affected by COVID-19 shortly after China [1]. As a rapidly evolving situation, COVID-19 has affected all communities and caused severe disruptions in people's lives [2]. This disruption forced medical universities worldwide, including those in Iran, to shift rapidly to virtual learning. Although this transition was necessary to ensure continuity of education, it exposed many challenges, such as limited infrastructure, inadequate faculty training, and student disengagement [3, 4]. According to a UNESCO report (2020), over 1.5 billion learners were affected by school closures globally, leading to an unprecedented reliance on emergency remote education [5].
In this study, virtual learning refers to technology-mediated instruction delivered synchronously (e.g., web-conferencing platforms for live sessions) and/or asynchronously (e.g., learning management systems for content, quizzes, and discussion), often combined within blended learning models to preserve hands-on components where necessary [6-8]. Across medical and health professions education, virtual and blended formats have been widely adopted and continue to expand in the post-pandemic era, improving theoretical knowledge gains and flexibility while maintaining acceptable performance in practical competencies when well designed [6, 7, 9, 10]. Recent studies and meta-analyses further show superior outcomes for blended models compared with traditional lectures, alongside implementation challenges that institutions must proactively address [6, 7, 9, 11, 12].
Given the lack of prior experience with online education in Iranian medical universities, there is a critical need to identify and implement evidence-based strategies that ensure sustainable virtual learning. This study aims to bridge this gap by leveraging the Blended Learning Model as a theoretical framework to enhance medical education. Despite numerous studies on the effectiveness of blended learning in higher education, limited research has specifically explored its application in medical education within low-resource settings such as Iran. This study addresses this gap by systematically identifying and prioritizing strategies that enhance virtual medical education in resource-constrained environments.
In Iranian medical universities, prior to the pandemic, online education was limited, and only 20% of the curriculum was delivered through digital platforms [13]. This transition to online learning posed unique challenges, especially for medical sciences, where practical training is essential. As studies have shown, student engagement and faculty preparedness were key issues that needed to be addressed [6, 14]. Additionally, faculty members faced technological and pedagogical challenges, as they were not adequately prepared for the demands of remote teaching [9, 15].
Despite these obstacles, the pandemic also provided an opportunity to rethink and reshape educational approaches. Medical universities now have the opportunity to integrate more flexible and sustainable educational models to ensure continuity during future disruptions. Blended learning, which combines face-to-face and online instruction, offers a viable solution for medical education. This model has been proven to enhance student engagement, foster collaboration, and improve learning outcomes, especially when adapted to the needs of medical curricula [7]. By utilizing the Blended Learning Model as a guiding framework, this study systematically examines how the integration of online and face-to-face methods can optimize virtual medical education and address key challenges such as student engagement, faculty preparedness, and infrastructure development.
Several studies have highlighted the effectiveness of blended learning in medical education. One study demonstrated that blended learning enhances critical thinking, collaboration, and flexibility among medical students, especially in courses such as evidence-based medicine [11, 16]. Similarly, meta-analyses have found that hybrid models improve academic performance and yield better educational outcomes compared to purely online or traditional classroom instruction alone [17, 18]. A randomised study also showed that hybrid models improve theoretical knowledge gain compared with purely online or in-person methods, especially in teaching skills such as local anaesthesia [10]. While studies have confirmed that blended learning offers substantial benefits, it also introduces challenges for educators, particularly in terms of digital and instructional skills, administrative barriers, and faculty resistance, which need to be addressed for effective implementation [12]. Incorporating the Blended Learning Model into medical curricula can help bridge the gap between digital and hands-on education, making learning more adaptive, engaging, and sustainable.
Blended learning has gained recognition as an effective framework for medical education. It allows for the integration of theoretical content delivered through online platforms while maintaining practical, hands-on training through in-person sessions. Research highlights that blended models improve flexibility and accessibility while maintaining the quality of medical education [7]. Furthermore, studies have shown that blended learning can bridge gaps in both digital infrastructure and pedagogical strategies, ensuring that students receive the best of both worlds — online convenience and face-to-face interaction [6].
However, the effectiveness of virtual education is contingent upon several factors. Effective online education requires adequate technological infrastructure, skilled faculty, and robust student support systems. Studies on the Iranian context suggest that, while some medical institutions struggled with rapidly shifting to online formats, others leveraged innovative tools and platforms to deliver education [13, 15]. These studies emphasize the need for structured planning in transitioning to blended learning systems that combine both digital and in-person modalities.
Therefore, this study aims to identify strategies for enhancing virtual learning in Iranian medical universities during the pandemic, using blended learning as the theoretical framework. The study also intends to assess expert consensus on the feasibility and effectiveness of these strategies using the Delphi method. By integrating the lessons learned from this study, Iranian universities will be better prepared to adopt sustainable and effective blended learning models in future educational crises. This study not only addresses a gap in research on virtual medical education in resource-limited settings but also provides a structured framework for integrating blended learning strategies into medical curricula, ensuring a more resilient and adaptive educational model for future crises.
2. METHODS
This research employed a mixed-methods approach, conducted in two phases. The first phase involved a systematic review to identify strategies to enhance virtual learning in Iranian medical universities during the COVID-19 pandemic [3]. The second phase used the modified Delphi method to achieve expert consensus on the most effective strategies.
2.1. Phase 1: Systematic Review (brief)
We synthesized peer-reviewed reports on virtual education in medical schools (Dec 2019–10 Jan 2022) following the six-step Arksey & O’Malley framework [19] and PRISMA [20, 21] (for full search strings, selection steps, and the PRISMA flow, see our previously published review). Thirty-eight studies met the inclusion criteria, spanning Iran, the United States, Saudi Arabia, and other regions, with most published in 2020–2021 [3].
2.2. Key Findings
Recurrent challenges included unfamiliarity with virtual platforms, limited patient interaction, reduced faculty–student engagement, and concerns about online assessment integrity. Reported solutions emphasized psychological and financial support for students, faculty digital-skills training, strengthened IT infrastructure, and the adoption of blended/hybrid models (see also our previously published review for methodological detail and a broader evidence base) [3].
2.3. Phase 2: Delphi Methodology
The Delphi method is a structured process for collecting and synthesizing expert opinions on a specific issue through multiple rounds of questionnaires, in which feedback from earlier rounds is shared with participants for refinement. This iterative process aims to achieve consensus among experts. The Delphi technique is widely used in healthcare research and education studies to gather expert insights on complex issues, especially when empirical data may be limited or when expert judgment is crucial to understanding a phenomenon [22, 23].
In the present study, we employed the modified Delphi method to gather expert opinions on effective strategies for enhancing virtual learning in Iranian medical universities during the COVID-19 pandemic. This approach differs from the classical Delphi method, as it presents pre-identified strategies (derived from a systematic review) to experts for evaluation and consensus-building, rather than requiring experts to generate solutions from the outset [22].
2.4. Expert Panel Selection
The Delphi panel consisted of 12 experts, including sociologists, academic researchers, medical educators, and senior policymakers in health education. Experts were selected using purposive sampling based on their academic background, experience in medical education policy, and prior contributions to virtual learning research. The inclusion criteria included willingness to participate in all Delphi rounds, expertise in medical education and e-learning, and holding a senior academic or administrative position in a medical university.
2.5. Delphi Rounds
The Delphi process consisted of two rounds (Fig. 1):
Round 1: Twelve experts participated and provided inputs via an online Google Form, the invitation link to which was distributed through email and WhatsApp. A reminder was sent after five days to ensure participation. A total of 62 unique strategy statements were collected. The responses ranged from brief bullet points to detailed paragraph-style inputs. Two researchers independently carried out content analysis to convert raw inputs into clear, action-oriented strategy statements, merge overlapping or duplicate suggestions, and remove redundancy. Any disagreement was discussed until consensus was achieved.
Round 2: In the second round, the consolidated list of 45 strategies was rated by the same experts using a 5-point Likert scale based on the FAME criteria (Feasibility, Appropriateness, Meaningfulness, and Effectiveness). A consensus threshold was defined as ≥70% of respondents rating an item 4 or 5. Items below the threshold were reworded, merged, or re-evaluated in a third round. As part of this process, platform-specific duplicates (e.g., several synchronous tools) or highly similar items (e.g., various lab technologies) were merged into broader, composite strategies.
A complete audit trail mapping all 62 Round-1 items to the final 45 strategies (including merged, renamed, or excluded items) is provided in Table S1. Face and content validity of the initial Delphi questionnaire were reviewed by five senior experts from among the 12 panelists, based on their extensive professional experience (over 10 years), prior to Round 2. The study was approved by the Ethics Committee of Saveh University of Medical Sciences (IR.SAVEHUMS.REC.1401. 015).
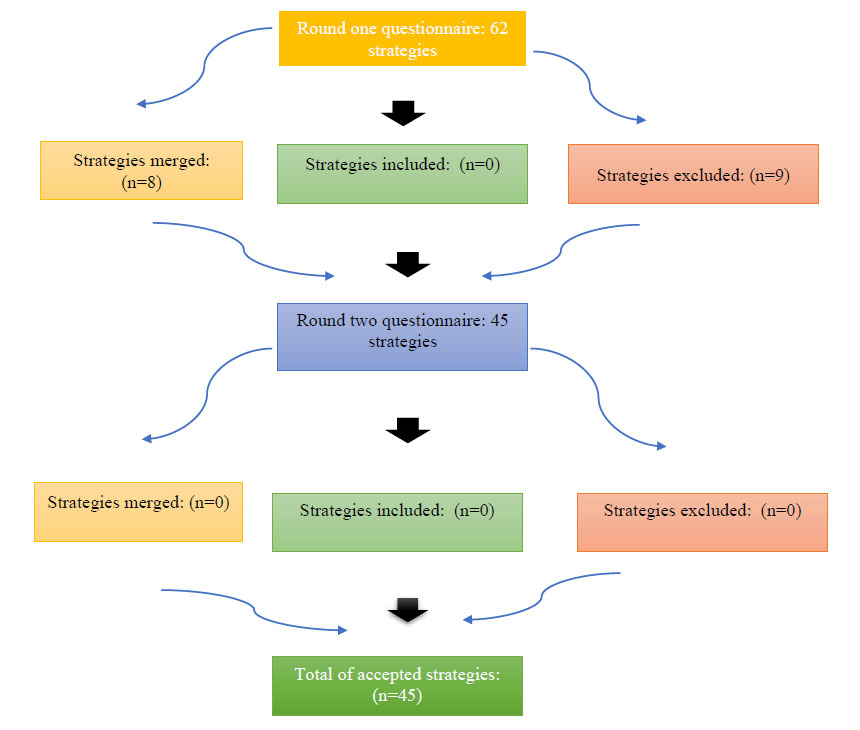
Delphi process flowchart.
3. RESULTS
3.1. Findings from the Systematic Review
A systematic review was conducted to analyze virtual education policies in medical schools between December 2019 and January 10, 2022. The review included 38 studies, with the majority published in 2020 (58%) and 2021 (39%), covering diverse geographical contexts such as Iran, the United States, and Saudi Arabia. The findings were categorized into five key domains: (1) Learner, (2) Process, (3) Technical Infrastructure, (4) Faculty Development, and (5) Assessment strategies.
Key challenges identified in the systematic review included students' unfamiliarity with virtual platforms, limited interaction with patients, reduced faculty–student engagement, and concerns over the integrity of online assessments. Solutions proposed in the reviewed studies emphasized the importance of financial and psychological support for students, digital-skills training for faculty, enhanced IT infrastructure, and the adoption of hybrid learning models [3]. Consolidated strategies and their classification are summarized in Table S1.
These findings were previously published in detail in a separate study conducted by the same research team [3], where 34 challenges, 62 solutions, and 27 advantages were identified and mapped across the five main domains. A summary of the thematic findings is presented in Table 1 [3]. Domains were consistently labeled as: Learner, Process, Technical Infrastructure, Faculty Development, and Assessment. These results served as the foundational evidence base for developing the Delphi questionnaire in the present study.
| Domain | Key Challenges Identified | Proposed Solutions Highlighted in the Review |
|---|---|---|
| Learner | Technological unpreparedness, psychological distress, and limited access to resources | Financial and psychological support, improving digital literacy, and equal access to online resources |
| Process | Reduced student engagement, suspension of clinical training, and passive learning approaches | Implementation of blended learning, flipped classrooms, team-based, and active learning strategies. |
| Technical Infrastructure | Inadequate bandwidth, server instability, and a lack of reliable educational platforms | Enhancing IT infrastructure, ensuring platform security, and 24/7 technical support systems |
| Faculty Development | Limited digital and pedagogical skills, low engagement in content development | Faculty training programs, development of electronic content tools, and continuous support mechanisms |
| Assessment | Concerns over online exam integrity, lack of standardized evaluation tools | Diversified assessment methods, formative evaluation, project-based assessments, and clinical simulations |
To build upon these findings, the present study utilized the Delphi method to refine and prioritize strategies specific to the Iranian medical education context. The subsequent sections outline the expert panel’s consensus on prioritized strategies aimed at improving virtual learning in medical education.
3.2. Expert Panel Characteristics
The Delphi panel consisted of 12 experts, with the majority being female (83.3%) and holding a PhD (66.7%). Most experts specialized in healthcare policy and management (25%) or medical education (25%) and were based in Tehran province (83.3%). The average work experience ranged between 10-20 years (75%) (Table 2).
3.3. Delphi Round 1 Findings
In Round 1, experts reviewed 62 initial strategies, providing qualitative feedback. After merging overlapping responses and removing redundant items, the strategies were refined to 45 key solutions. These were categorized into five main domains:
(1) Learner strategies (e.g., psychological support, financial aid).
(2) Process strategies (e.g., digital course updates, interactive platforms).
(3) Technical Infrastructure strategies (e.g., connecting to the net, server difficulties).
(4) Faculty Development strategies (e.g., faculty training, mentorship programs).
(5) Assessment strategies (e.g., short-term evaluations, replacing final exams with assignments).
3.4. Delphi Round 2 Findings
In Round 2, panelists rated the 45 refined strategies using the FAME framework (Feasibility, Appropriateness, Meaningfulness, Effectiveness). Strategies scoring ≥3.5 (70% consensus) were retained. In Table 3, the strategies identified for enhancing virtual learning in Iranian medical universities during the COVID-19 pandemic are presented. Each strategy was evaluated by a panel of experts through a Delphi method, and the average ratings are shown for each strategy. Additionally, the consensus percentage reflects the level of agreement among the experts, while the challenges/implementation needs highlight the key factors necessary for the successful adoption of these strategies. The strategies are organized by dimensions, including learner support, process improvement, technical infrastructure, and instructor development, with the goal of providing actionable insights for improving virtual learning environments in medical education.
| Variable | Category | Frequency (%) |
|---|---|---|
| Gender | Female | 10 (83.3%) |
| Male | 2 (16.7%) | |
| Age | 30-40 years | 5 (41.7%) |
| 40-50 years | 7 (58.3%) | |
| Degree | PhD | 8 (66.7%) |
| MSc | 4 (33.3%) | |
| Field of Expertise | Healthcare Policy & Management | 3 (25%) |
| Medical Education | 3 (25%) | |
| Educational Management | 1 (8%) | |
| Medicine | 1 (8%) | |
| Sociology | 1 (8%) | |
| Health Economics | 1 (8%) | |
| Nursing/Crisis Management | 2 (18%) | |
| Experience | 10-20 years | 9 (75%) |
| <10 years | 3 (25%) | |
| Institution | Ministry of Health & Medical Education | 7 (58.3%) |
| Universities of Medical Sciences | 5 (41.7%) |
| Dimensions | Strategy Title | F | A | M | E | Total | Consensus | Challenges/Implementation Needs |
|---|---|---|---|---|---|---|---|---|
| Learner | Providing psychological support for students | 4.5 | 4.5 | 4.6 | 4.5 | 4.5 | 90% | Need for online counselors and psychological resources |
| Providing personal protective equipment to medical teams and interns | 4.3 | 4.2 | 4.3 | 4.4 | 4.3 | 86% | Need for sufficient PPE supplies and distribution channels | |
| Issuing certificates and licenses for students volunteering in various departments | 3.8 | 3.6 | 4 | 3.7 | 3.8 | 76% | Need for clear criteria for certification and coordination with departments | |
| Providing financial aid to disadvantaged students (tuition discounts, free education, electronic equipment with the help of donors, free internet access) | 3.8 | 3.3 | 3.7 | 3.5 | 3.8 | 76% | Need for partnerships with donors and telecommunication companies | |
| Setting a schedule for students’ stay in the dormitory and issuing licenses for practical and clinical sessions | 3.7 | 3.6 | 3.5 | 3.6 | 3.7 | 74% | Need for coordination with accommodation services and clinical departments | |
| Creating safe retreats for students in hospitals | 3.7 | 3.3 | 4 | 3.4 | 3.7 | 74% | Need for designated safe spaces and health protocols for students | |
| Using learner-centered anagogical approaches | 3.7 | 3.9 | 4.1 | 3.8 | 3.7 | 74% | Need for designated safe spaces and health protocols for students | |
| Process | Creating a social network of officials and intermediaries for better communication and information transfer | 4.7 | 4.6 | 4.5 | 4.5 | 4.6 | 92% | Need for clear communication protocols and platform management |
| Updating course materials and content, preparing widely used content in advance with various topics and courses | 4.4 | 4.2 | 4.4 | 4.6 | 4.4 | 88% | Need for coordination between instructors and content management teams | |
| Using discussion, assignment, test, and messaging modules in educational platforms such as Microsoft Teams and Google Classroom | 4.5 | 4.3 | 4.6 | 4.4 | 4.4 | 88% | Need for ensuring ease of access for students and faculty members | |
| Development of the National Electronic Library of Medical Sciences | 4.6 | 4.4 | 4.2 | 4.4 | 4.4 | 88% | Need for collaboration with academic and research institutions | |
| Integrating similar general courses into one virtual class to save time | 4.6 | 4.3 | 4.4 | 4.5 | 4.4 | 88% | Need for coordination between faculty members and course planners | |
| Using interactive modules for regular monitoring of educational performance in terms of the number of professors, students, and active courses | 4.5 | 4.3 | 4.5 | 4.5 | 4.4 | 88% | Need for advanced analytics tools and data integration across platforms | |
| Providing part of the practical and internship courses through educational videos | 4.5 | 4.4 | 4.4 | 4.1 | 4.3 | 86% | Need for high-quality video content and proper video hosting infrastructure | |
| Applying the lessons learned from virtual learning and addressing the weaknesses of practical courses and internships | 4.4 | 4.3 | 4.3 | 4.1 | 4.3 | 86% | Need for feedback mechanisms and curriculum adjustments | |
| Integrating educational management systems | 4.4 | 4.2 | 4.2 | 4.3 | 4.2 | 84% | Need for system integration and training for staff | |
| Promoting team-based, active, and self-directed learning, and assigning team activities and online projects to students | 4.2 | 4.1 | 4.1 | 4.3 | 4.2 | 84% | Need for collaborative tools and effective group work management | |
| Redefining the educational landscape, strategic planning, mission, values, goals, and plans to turn challenges into opportunities | 4.4 | 4 | 4.1 | 4 | 4.1 | 82% | Need for engagement with key stakeholders and alignment of institutional goals | |
| Developing accreditation standards for clinical education by the Liaison Committee on Medical Education (LCME) | 4.2 | 4.2 | 4.1 | 4.1 | 4.1 | 82% | Need for collaboration with accreditation bodies and alignment with international standards | |
| Providing regular reports to the appropriate faculty vice-chancellors and the COVID crisis management committee | 4.2 | 4.2 | 4.1 | 3.9 | 4.1 | 82% | Need for a streamlined reporting system and data collection tools | |
| Flexibility in defining the quality standards for courses, prerequisites, and electronic content | 4.3 | 3.9 | 4.1 | 4 | 4 | 80% | Need for clear guidelines and flexibility in course design | |
| Managing the change of educational practices with local, national, and international cooperation to create a safer, healthier work environment | 4 | 4.1 | 4 | 3.9 | 4 | 80% | Need for strong partnerships and international cooperation for effective change management | |
| Developing a collaborative/interactive learning model | 4 | 4 | 4 | 4 | 4 | 80% | Need for collaborative platforms and active student participation | |
| Postponing internships until COVID-19 is fully contained | 3.5 | 3.3 | 2.9 | 2.9 | 3.1 | 62% | Need for flexibility in internship scheduling and ensuring students' readiness | |
| Technical Infrastructure |
Developing an online IT support system to answer questions and solve technical problems | 4.6 | 4.7 | 4.7 | 4.6 | 4.6 | 92% | Need for 24/7 support systems and well-trained IT staff |
| Server enhancement | 4.5 | 4.3 | 4.6 | 4.6 | 4.5 | 90% | Need for upgraded hardware and cloud infrastructure | |
| Improving the security of systems and platforms | 4.6 | 4.7 | 4.3 | 4.6 | 4.5 | 90% | Need for enhanced security protocols and compliance measures | |
| Integrating online education technologies | 4.4 | 4.5 | 4.5 | 4.5 | 4.5 | 90% | Need for integration with existing platforms and staff training | |
| Using alternative technologies to improve remote learning of anatomy and laboratory work, such as remote robotic microscopy, artificial intelligence, digital libraries, clinical simulation laboratories, and virtual haptic laboratory | 4.3 | 4.1 | 4.4 | 4.6 | 4.3 | 86% | Need for investment in advanced technologies and training for instructors | |
| Using various technologies and social media to streamline and optimize virtual conferences | 4.3 | 4.4 | 4.3 | 4.4 | 4.3 | 86% | Need for proper coordination between platforms and ease of use for participants | |
| Using Adobe Connect and other software programs to create and manage virtual classes, including BigBlueButton, Skype, Skyroom, and Zoom | 4.3 | 4.3 | 4.5 | 4.2 | 4.3 | 86% | Need for faculty training on virtual classroom tools and smooth technical operation | |
| Assessing the diagnostic skills of dentistry students by performing clinical procedures during examinations, clinical reasoning, and critical thinking in the absence of clinical procedures | 4.3 | 4.4 | 4.2 | 4.2 | 4.2 | 84% | Need for alternative assessment methods and practical evaluation tools | |
| Faculty Development | Providing training (online, offline, face-to-face) on how to work with software and electronic infrastructure for faculty members less familiar with virtual learning | 4.7 | 4.3 | 4.6 | 4.5 | 4.5 | 90% | Need for specialized training programs and user-friendly materials |
| Producing electronic content creation software for teachers to prepare multimedia educational materials | 4.6 | 4.5 | 4.5 | 4.5 | 4.5 | 90% | Need for easy-to-use software and ongoing training for instructors | |
| Ability to contact academic staff to solve problems and transfer information | 4.5 | 4.6 | 4.4 | 4.5 | 4.5 | 90% | Need for a streamlined communication platform and quicker response times | |
| Encouraging faculty participation in preparing electronic content and educational packages | 4.7 | 4.5 | 4.3 | 4.4 | 4.5 | 90% | Need for incentives and support for faculty in content creation | |
| Conducting needs assessment to control the quality of e-content by contacting students/trainees and preparing them before starting online learning programs | 4.3 | 4.3 | 4.5 | 4.5 | 4.4 | 88% | Need for effective feedback mechanisms and regular assessments | |
| Giving faculty members and educational groups the authority to decide on the volume of synchronous/asynchronous face-to-face and online training based on the course and student/faculty conditions | 4.3 | 4.4 | 4.3 | 4.5 | 4.1 | 82% | Need for clear guidelines and flexibility in managing teaching methods | |
| Assessment | Evaluating the number of uploaded contents, assignments, exercises, formative tests, activities provided by instructors, and feedback exchanges with professors | 4.7 | 4.6 | 4.6 | 4.6 | 4.6 | 92% | Need for comprehensive tracking systems and faculty involvement in feedback loops |
| Pre-assessment of students to determine their knowledge and skills prior to intervention | 4.6 | 4.5 | 4.8 | 4.5 | 4.6 | 92% | Need for standardized tools and initial assessment frameworks | |
| Reviewing academic achievement strategies across programs to ensure academic accuracy | 4.5 | 4.5 | 4.5 | 4.4 | 4.5 | 90% | Need for periodic curriculum reviews and alignment with learning outcomes | |
| Diversifying and changing teaching/evaluation methods | 4.4 | 4.4 | 4.8 | 4.4 | 4.5 | 90% | Need for faculty training and flexibility in adopting various teaching strategies | |
| Replacing exams with short-term tests of materials taught online and student reports of previous sessions | 4.7 | 4.6 | 4.6 | 4.2 | 4.5 | 90% | Need for clear guidelines on short-term assessments and adapting to new formats | |
| Examining students’ satisfaction and experience with e-learning through surveys | 4.5 | 4.4 | 4.5 | 4.4 | 4.4 | 88% | Need for well-designed surveys and continuous monitoring of e-learning experiences | |
| Holding exams online | 4.4 | 4.1 | 4.2 | 4 | 4.2 | 84% | Need for robust online exam platforms and addressing security concerns |
Table 4 presents the highest-rated strategies (FAME Score ≥4.5) identified through expert consensus in the Delphi study. The most highly rated strategies focused on four key areas: technical infrastructure, student support, instructor support, and flexible assessment methods.
The consensus percentage indicates the level of agreement among experts on the importance of each strategy. These findings highlight the crucial role of technology, student well-being, and adaptive assessment in ensuring the success of virtual learning in medical education.
| Strategy | Total Score | Consensus |
|---|---|---|
| Using social networks for virtual learning | 4.6 | 92% |
| Developing an online IT support system | 4.6 | 92% |
| Pre-assessment of students before intervention | 4.6 | 92% |
| Enhancing the evaluating and feedback system | 4.6 | 92% |
| Providing psychological support for students | 4.5 | 90% |
| Enhancing server infrastructure | 4.5 | 90% |
| Enhancing security infrastructure | 4.5 | 90% |
| Integrating online education technologies | 4.5 | 90% |
| Specialized training programs and user-friendly materials | 4.5 | 90% |
| Providing easy-to-use software and ongoing training for instructors | 4.5 | 90% |
| Providing streamlined communications | 4.5 | 90% |
| Enhancing instructors' incentive and support system | 4.5 | 90% |
| Providing periodic curriculum reviews | 4.5 | 90% |
| Adopting various teaching strategies | 4.5 | 90% |
| Replacing final exams with short-term assessments | 4.5 | 90% |
4. DISCUSSION
This study identified key strategies for enhancing virtual learning in Iranian medical education, focusing on technological infrastructure, student support, and adaptive assessment methods. These strategies were developed and refined based on the experiences and challenges faced during the COVID-19 pandemic, which forced a rapid transition to virtual learning environments. The findings of this study reinforce the principles of the Blended Learning Model by demonstrating how integrating online and in-person components can effectively address student engagement, faculty preparedness, and technological infrastructure deficiencies. This aligns with previous research indicating that blended learning enhances collaboration, critical thinking, and accessibility in medical education, particularly in resource-limited settings such as Iran [24-26]. The adoption of blended learning models appears to be particularly effective in overcoming these challenges by combining online content delivery with in-person practical training, which is essential in medical education. While the Blended Learning Model provides a strong theoretical foundation for virtual medical education, its success heavily depends on the availability of robust digital infrastructure and continuous IT support.
Along with pedagogical strategies, the technical infrastructure of virtual learning environments plays an equally important role in ensuring seamless learning experiences for students. One of the most highly rated strategies in this context was the development of online IT support systems and the enhancement of server security. As research confirms, lack of technical support is a major barrier to effective e-learning, especially in medical education, where continuous access to reliable platforms is crucial [27]. Previous studies have found that universities that implemented 24/7 technical support systems saw increased student satisfaction and higher engagement levels [28]. Implementing robust IT support systems and secure online platforms is essential for sustaining virtual medical education. Studies have shown that institutions with well-established digital infrastructure report higher student satisfaction and academic performance. A scoping review on the impact of COVID-19 on medical education found that inadequate digital infrastructure posed significant challenges for universities, particularly in low- and middle-income countries, affecting curriculum delivery, student engagement, and assessment processes [29]. These findings suggest that medical schools must invest in robust IT support, including cybersecurity measures and AI-driven troubleshooting systems, to ensure the sustainability and reliability of virtual learning environments. Beyond infrastructure, effective virtual learning also requires strong faculty–student communication to ensure student engagement and academic success.
Another crucial finding of this study is the role of effective faculty–student communication in virtual learning environments. Studies have shown that students greatly value the accessibility of their instructors through digital platforms, which helps facilitate timely assistance and information exchange. Such regular communication is key to reducing feelings of isolation and enhancing student engagement with the curriculum [30]. Learner-to-instructor engagement strategies, such as sending regular announcements and providing grading rubrics, were found to be particularly effective in promoting student engagement and satisfaction in online courses [28]. Such communication helps ensure that students do not feel disconnected and continue to feel supported in their learning. Effective faculty–student communication plays a crucial role in reducing isolation and directly impacts student satisfaction, as demonstrated by improved engagement and academic success in virtual learning environments. Strong communication channels not only support academic success but also play a crucial role in shaping students' overall satisfaction with virtual learning environments.
Understanding students' satisfaction and experiences in virtual learning settings is essential for enhancing online education. Research from the United States has shown that student satisfaction is closely linked to the quality of online course delivery and the effective use of technology [31]. Furthermore, students have expressed appreciation for flexible learning environments but also concerns about the lack of interaction with peers and instructors [32]. Addressing these concerns is crucial for designing engaging and effective online education systems. Research from Indonesia has found that student engagement, which is influenced by interaction between students, teachers, and content, plays a significant role in boosting satisfaction [33]. Ensuring that students can maintain connections with both their peers and instructors can significantly improve their overall experience in virtual learning environments. In addition to fostering communication, alternative assessment strategies like continuous evaluations help to reduce the anxiety associated with high-stakes exams, thus enhancing overall student satisfaction. To further enhance student satisfaction and engagement, many educational institutions have integrated social networks as an informal yet powerful learning tool.
Social networks were rated as the most effective tool for virtual learning. Prior studies have shown that social media platforms enhance peer-to-peer learning, facilitate instructor–student communication, and provide access to diverse educational resources [24-26]. Social networks, as an informal learning environment, can create opportunities for students to share knowledge and ideas beyond formal classroom settings. However, over-reliance on these platforms can lead to information overload, decreased academic focus, and potential challenges in content credibility [26, 34]. Medical universities should therefore integrate social platforms into formal learning systems, ensuring alignment with blended learning principles to optimize student engagement and interaction. Implementing structured guidelines will help maintain credibility and accuracy of shared educational content, ultimately enhancing the virtual learning experience. In line with these blended learning models, social networks have emerged as a powerful tool to enhance peer-to-peer learning and facilitate communication between students and instructors, further improving engagement in virtual environments. However, while students benefit from digital tools and online collaboration, faculty members have faced significant challenges in adapting to these new teaching methods.
The abrupt shift to online education due to the COVID-19 pandemic highlighted several challenges, especially for faculty members who were less familiar with virtual learning environments. Many lacked the necessary skills to effectively utilize online platforms, and institutions that invested in comprehensive training for faculty members reported better adaptation to online teaching and improved student satisfaction [35]. Similarly, a study conducted in Islamabad found that universities that modified instructional practices based on student feedback saw significant improvements in student satisfaction and engagement with online learning [36]. This finding aligns with existing literature emphasizing the importance of faculty preparedness in medical education, where practical, interactive learning is critical. In addition to faculty preparedness, assessment methods also needed to evolve to align with the demands of virtual learning.
The shift from high-stakes exams to continuous and formative assessments, such as assignments, projects, and class activities, was another significant strategy identified. Previous research suggests that replacing final exams with continuous assessments can enhance learning outcomes and foster a more collaborative learning environment [8, 37]. Additionally, hybrid assessment models, where continuous evaluation replaces final exams, have proven effective in enhancing student participation and reducing anxiety [38, 39]. Furthermore, adapting assessment methods to the challenges of online learning is crucial, with studies emphasizing the importance of flexible and adaptive evaluation strategies [40]. Given the challenges students faced in adapting to virtual learning, including heightened anxiety and reduced motivation, medical education should consider incorporating more flexible and formative assessment methods. Peer reviews and interactive simulations not only provide an alternative to high-stakes exams but also align with the blended learning approach by reinforcing student-centered, competency-based education. This shift allows students to engage with the material in a more meaningful and practical way, reducing stress and fostering a deeper understanding of the content. Beyond academic performance, the shift to virtual learning also had profound psychological effects on students, necessitating additional support mechanisms.
The importance of addressing students' psychological well-being cannot be overstated, as mental health challenges significantly hinder motivation and academic performance in online education. Studies show that the isolation associated with online education, coupled with the mental health challenges exacerbated by the pandemic, can negatively impact motivation, increase stress, and hinder academic performance [41, 42]. Providing psychological support, such as virtual counseling and peer support groups, has been shown to improve both well-being and academic outcomes [43, 44]. Medical universities should ensure the availability of mental health resources to help students cope with the stresses of virtual learning environments. By addressing mental health needs, institutions can better support students in maintaining motivation and academic performance. To mitigate some of these psychological challenges, educational institutions are increasingly turning to digital innovations, such as AI-driven support systems and virtual reality simulations, to create more engaging and interactive learning experiences.
The integration of advanced technologies such as AI-driven assessments, virtual reality (VR), and simulation tools can significantly enhance the quality of medical education, offering interactive learning experiences that are difficult to replicate in traditional settings. For example, AI-driven assessments can help evaluate students' clinical reasoning and decision-making skills more accurately [45]. Research suggests that these tools can significantly enhance practical learning, especially when integrated into blended learning models [46, 47]. Medical institutions should explore innovative digital tools to complement traditional methods, ensuring that students receive a holistic educational experience that aligns with the Blended Learning Model. By leveraging a combination of digital resources and face-to-face instruction, medical education can become more resilient and adaptable to future disruptions.
Our top-ranked strategies, robust IT support and security, systematic faculty training, psychological support for learners, and flexible assessment, mirror findings reported internationally across health professions and broader higher education. Meta-analytic and comparative studies indicate that blended formats generally outperform lecture-only approaches for theoretical knowledge while maintaining comparable practical performance when hands-on components are deliberately scaffolded [7, 9-11]. Parallel work on online assessment underscores the value of diversified, lower-stakes, continuous assessments for reducing anxiety and improving engagement, provided that integrity safeguards are in place [35].
The findings suggest that while strategies are context-specific, many are transferable to other disciplines and international settings. Beyond the Iranian context, these strategies are transferable to other disciplines that require both cognitive and psychomotor outcomes. However, implementation success hinges on local capacity (e.g., bandwidth, platform reliability), faculty digital-pedagogical readiness, and institutional policies that enable adaptive, student-centered design. Recent qualitative evidence also highlights faculty skill gaps and administrative barriers that must be addressed through ongoing development and change management [12, 37]. These findings highlight the need for medical institutions to develop long-term strategies that integrate blended learning models with strong technological and psychological support systems, ensuring sustainable and effective medical education beyond the COVID-19 pandemic.
5. STUDY LIMITATIONS AND FUTURE DIRECTIONS
Despite the promising findings, this study has several limitations. First, the sample size of experts in the Delphi process was limited to 12 participants, which may not fully represent the diversity of perspectives in the broader medical education community. Future studies should aim to expand the sample size and include international experts to ensure a more comprehensive understanding of effective strategies. Additionally, while this study focused on the Iranian context, it is essential to assess the generalizability of the identified strategies to other educational settings.
Further research should explore the long-term impact of blended learning models on student performance and faculty development. Studies should also assess the cost-effectiveness of implementing technological innovations and mental health support programs in medical education.
CONCLUSION
This study highlights the importance of integrating blended learning models into medical education to address the challenges posed by the COVID-19 pandemic. Strengthening technological infrastructure, providing psychological support, and implementing flexible assessment methods can enhance the sustainability and effectiveness of virtual learning. Future research should explore the long-term impact of these strategies to ensure that medical education remains adaptable and resilient in the face of future challenges.
KEY CONTRIBUTIONS
Technological infrastructure, including IT support systems and secure platforms, was recognized as essential for ensuring the smooth delivery of online education. Psychological support, such as counseling services and mental health resources, was seen as vital for addressing student stress and maintaining motivation in a virtual learning environment. Flexible assessments (e.g., replacing final exams with continuous evaluation) were advocated to reduce student anxiety and promote deeper learning.
These strategies have important implications for medical education, not only in Iran but also globally, as the COVID-19 pandemic has underscored the necessity of adaptable and resilient learning systems. Medical universities worldwide must adopt a holistic approach to virtual learning, integrating technology, student support, and assessment innovations to improve educational outcomes and ensure the continuity of medical training in future crises.
FUTURE IMPLICATIONS
The strategies outlined in this study provide a roadmap for enhancing the quality and sustainability of virtual learning in medical education. However, future research should explore the long-term effects of these strategies, their cost-effectiveness, and their scalability in different global contexts. Further studies can also focus on assessing the real-time implementation of these solutions and their impact on student engagement, retention, and clinical competencies.
By embracing these strategies, medical institutions can ensure that virtual education becomes a complementary tool rather than a substitute, enhancing both the learning experience and the quality of healthcare education in the digital age.
AUTHORS' CONTRIBUTIONS
The authors confirm contribution to the paper as follows: P.I., M.S., and M.A.: Designed the research; M.A., F.K., and P.I.: Conducted it; M.S., F.K., S.T., P.I., and M.A.: Collected the data; M.S., F.K., S.T., and M.A.: Wrote the paper; M.A. and S.T.: Primary responsibility for the final content. All authors read and approved the final manuscript.
ABBREVIATION
| LCME | = Liaison Committee on Medical Education |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval for all experimental protocols was obtained by the Research Ethics Committee of Saveh University of Medical Sciences (IR.SAVEHUMS.REC.1401.015).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated and/or analyzed during the current study are not publicly available due to the qualitative nature of these data, but are available from the corresponding author on reasonable request.
ACKNOWLEDGEMENTS
We gratefully acknowledge our Delphi panelists. Without their time and expertise, we would not have been able to conduct this work.


