All published articles of this journal are available on ScienceDirect.
Analgesia During Heel Lance in Preterm Neonates: A Systematic Review and Meta-Analysis Evaluating Non-nutritive Sucking Interventions
Abstract
Introduction/Objective
Persistent and early pain experiences, before the full development of the nervous system, can lead to enduring behavioral changes in preterm infants. This systematic review and meta-analysis were conducted to evaluate the effect of non-nutritive sucking (NNS) on pain during heel stick procedures in preterm neonates.
Methods
Registered on PROSPERO and following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we systematically searched PubMed/MEDLINE, Embase, Scopus, Web of Science, Cochrane, ISRCTN, ClinicalTrials.gov, the WHO ICTRP, and Google Scholar for RCTs of NNS analgesia in preterm NICU infants up to May. Two reviewers independently screened studies, extracted data, and assessed risk of bias using RoB-2. A meta-analysis was conducted in RevMan 5.3.
Results
From 6,216 articles retrieved, eight RCTs underwent detailed assessment, focusing on 225 preterm neonates, with 116 in the NNS group and 109 in the control group. Male neonates constituted 58.5 percent (n = 131). The findings revealed a statistically significant reduction in pain scores and heart rate (HR) in the intervention group. However, the impact of NNS on oxygen saturation (O2 sat) was not significant.
Discussion
These findings support a mechanoreceptor-mediated, gate-control analgesic effect of pacifier use in preterm infants, offering a low-cost, low-risk adjunct to NICU pain management. However, standardized NNS protocols and larger multicenter RCTs are needed to optimize dosing, timing, and long-term outcomes.
Conclusion
The results showed that NNS may be effective in improving heel stick pain and HR. However, the limited quantity and quality of included studies underscore the need for further research to comprehensively analyze the influence of NNS on pain reduction.
1. BACKGROUND
In recent years, numerous countries have witnessed a rise in the incidence of preterm births. About 15 million preterm neonates (less than 37 weeks of gestation) are born each year worldwide [1]. Substantial evidence indicates that prolonged exposure to painful stimuli in neonates before the maturation of the nervous system can result in enduring behavioral changes. Given the ongoing development of the central nervous system in preterm neonates, they exhibit heightened susceptibility to pain. Repetitive exposure to painful stimuli has the potential to modify physiological processes and stress hormone levels, activate the hypothalamic–pituitary–adrenal axis, induce alterations in pain sensitivity, and disrupt the structural and functional organization of the developing brain [2].
In this condition, unresolved pain may result in both short-term and long-term adverse effects [2-4]. Persistent exposure to painful procedures affects the neonate's nervous system development and may cause behavioral changes. The short-term effects of pain include decreased oxygenation, hemodynamic instability, increased HR, and elevated intracranial blood pressure [6-9]. The long-term effects include excessive anxiety and pain sensitivity, irritability, sleep problems, reduced nutrition, and attention deficiency, and may even result in the neonate's death [10-12].
To reduce the negative effects of necessary painful procedures on preterm infants, both drug-based and non-drug interventions are used [13]. However, due to possible side effects from medications, it is recommended to focus on non-pharmacological methods for managing pain in these infants. These non-pharmacological methods include kangaroo mother care, non-nutritive sucking (NNS), breastfeeding, sucrose consumption, massage, facilitated tucking, and exposure to the scent of breast milk [12-16].
Non-nutritive sucking refers to placing a pacifier in a newborn's mouth to encourage sucking without delivering breast milk or formula for nutrition [13]. This technique is thought to provide pain relief by stimulating oral mechanoreceptors, which alter how pain signals are transmitted or processed through the body's natural non-opioid pain control system [17]. The results of some clinical trials showed that NNS was effective in reducing the pain of procedures such as heel stick, venipuncture, blood sampling, and vaccination [7-18]. However, Perroteau et al. [1] found that facilitated tucking and NNS were ineffective during heel stick.
Although some reviews have summarized techniques for acute pain reduction during procedures in neonates and young children, ours is the first meta-analysis to isolate the effect of pure non-nutritive sucking during heel lance specifically in preterm neonates. This is due to the limited availability of high-quality evidence and the absence of a validated pain assessment tool for preterm neonates [19]. Therefore, the present systematic review and meta-analysis was conducted to evaluate randomized clinical trials (RCTs) investigating the effect of NNS on heel stick pain in preterm neonates.
2. METHODS
2.1. Aim
To assess the impact of NNS on the amelioration of heel stick pain, validated individual pain indicators and composite pain scores were employed. This review aimed to address two specific inquiries: a) the effectiveness of NNS in reducing pain during heel lance in preterm neonates, and b) the influence of NNS on HR and oxygen saturation during heel lance sampling.
2.2. Design
This systematic review and meta-analysis adhered to the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [20]. Registration for this systematic review and meta-analysis can be found on PROSPERO at http://www.crd.york.ac.uk/ PROSPERO (CRD42021219997).
2.3. Search strategy
A comprehensive search across databases such as PubMed/MEDLINE, Scopus, Web of Science, Cochrane Central Register of Controlled Trials (CENTRAL, May 2024), and the Google Scholar search engine was conducted. To identify potentially eligible randomized controlled trials (RCTs), gray literature, and unpublished studies, hand searching was performed in the ISRCTN database (www.isrctn.com), the National Institutes of Health Clinical Trials database (www.clinicaltrials.gov), and the International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp). We identified equivalent search terms through thesaurus systems (MeSH, Emtree), free-text methods, expert opinions, and examination of related articles and abstracts. Further details of the PRISMA flowchart diagram are presented in Fig. (5).
The terms used to search the databases were (“Sucking,” “Thumb sucking,” “Feeding,” “Breastfeeding,” “nutritive sucking”) in conjunction with terms related to pain (e.g., “Pain,” “Ache,” “Pain Thresholds,” “Procedural Pain,” “Analgesia,” “heel lance,” “heel puncture,” “heel stick,” “heel blood sample,” “heel prick”). The search strategy was applied from inception to May 2024 Table 1.
2.4. Eligibility Criteria
The inclusion criteria were randomized controlled trials (RCTs) based on the PICO (Participant, Intervention, Comparison, Outcome) framework, as outlined below:
2.5. Participants
Preterm neonates (< 37 weeks of gestation) admitted to the Neonatal Intensive Care Unit (NICU) who did not have congenital problems or neurological anomalies and did not require intubation, analgesic drugs, or sedatives.
2.6. Intervention
Pure non-nutritive sucking (NNS), as well as any comparison or adjuvant therapy (sucrose or other sweet tastes, pacifier, topical anesthetics, systemic analgesics), and any NNS provider (mother, father, nurse, etc.). We focused on pure NNS to clarify its standalone mechanistic and clinical effects, independent of sweet solutions or combined interventions.
| Databases | Syntax | Results |
|---|---|---|
| PubMed /Medline | (“non-nutritive sucking”[all] OR “Sucking Behavior”[all] OR (Behaviors[tiab] AND Sucking[tiab]) OR (Behavior[tiab] AND Sucking[tiab]) OR “Sucking Behaviors”[tiab] OR (non-nutritive[tiab] AND suck*[tiab]) OR “Non-nutritional sucking”[all] OR “Non nutritional sucking”[all] OR (non-nutritional[tiab] AND suck*[tiab]) OR “Finger Sucking”[tiab] OR “Fingersucking”[tiab] OR (Sucking[tiab] AND Finger[tiab]) OR “Thumbsucking”[tiab] OR “Thumb Sucking”[tiab] OR (Sucking[tiab] AND Thumb[tiab]) OR “Pacifier”[tiab] OR “Pacifiers”[tiab] OR “Dummy”[tiab] OR “soother”[tiab] OR “nipple”[tiab]) AND (“Pain management”[tiab] OR (Management[tiab] AND Pain[tiab]) OR (Managements[tiab] AND Pain[tiab]) OR “Pain Managements”[tiab] OR “analgaesia”[tiab] OR “pain management”[tiab] OR “pain relief”[tiab] OR “analgesia”[tiab] OR “Pain Thresholds”[tiab] OR (Thresholds[tiab] AND Pain[tiab]) OR (Threshold[tiab] AND Pain[tiab]) OR “Heel stick”[tiab] OR “Heel lance”[tiab] OR “heel puncture”[tiab] OR “heel prick”[tiab] OR “blood sampling”[tiab] OR “blood collecting”[tiab] OR “blood collection”[tiab] OR “blood sample”[tiab] OR “blood specimen collection”[tiab] OR (Sampling[tiab] AND blood[tiab])) AND 1975/01/01:2024/12/15[dp] |
624 |
| Embase | ('non-nutritive sucking' OR 'sucking behavior'/exp OR 'sucking behavior' OR (behaviors:ti,ab AND sucking:ti,ab) OR (behavior:ti,ab AND sucking:ti,ab) OR 'sucking behaviors':ti,ab OR ('non nutritive':ti,ab AND suck*:ti,ab) OR 'non-nutritional sucking' OR 'non nutritional sucking' OR ('non nutritional':ti,ab AND suck*:ti,ab) OR 'finger sucking':ti,ab OR fingersucking:ti,ab OR (sucking:ti,ab AND finger:ti,ab) OR thumbsucking:ti,ab OR 'thumb sucking':ti,ab OR (sucking:ti,ab AND thumb:ti,ab) OR pacifier:ti,ab OR pacifiers:ti,ab OR dummy:ti,ab OR soother:ti,ab OR nipple:ti,ab) AND (management:ti,ab AND pain:ti,ab OR (managements:ti,ab AND pain:ti,ab) OR 'pain managements':ti,ab OR analgaesia:ti,ab OR 'pain management':ti,ab OR 'pain relief':ti,ab OR analgesia:ti,ab OR 'pain thresholds':ti,ab OR (thresholds:ti,ab AND pain:ti,ab) OR (threshold:ti,ab AND pain:ti,ab) OR 'heel stick':ti,ab OR 'heel lance':ti,ab OR 'heel puncture':ti,ab OR 'heel prick':ti,ab OR 'blood sampling':ti,ab OR 'blood collecting':ti,ab OR 'blood collection':ti,ab OR 'blood sample':ti,ab OR 'blood specimen collection':ti,ab OR (sampling:ti,ab AND blood:ti,ab)) AND [1966-2024]/py |
923 (667 + 256 conference abstract) |
| Scopus | (ALL(“non-nutritive sucking”) OR ALL(“Sucking Behavior”) OR (TITLE-ABS(Behaviors) AND TITLE-ABS(Sucking)) OR (TITLE-ABS(Behavior) AND TITLE-ABS(Sucking)) OR TITLE-ABS(“Sucking Behaviors”) OR (TITLE-ABS(non-nutritive) AND TITLE-ABS(suck*)) OR ALL(“Non-nutritional sucking”) OR ALL(“Non nutritional sucking”) OR (TITLE-ABS(non-nutritional) AND TITLE-ABS(suck*)) OR TITLE-ABS(“Finger Sucking”) OR TITLE-ABS(Fingersucking) OR (TITLE-ABS(Sucking) AND TITLE-ABS(Finger)) OR TITLE-ABS(Thumbsucking) OR TITLE-ABS(“Thumb Sucking”) OR (TITLE-ABS(Sucking) AND TITLE-ABS(Thumb)) OR TITLE-ABS(Pacifier) OR TITLE-ABS(Pacifiers) OR TITLE-ABS(Dummy) OR TITLE-ABS(soother) OR TITLE-ABS(nipple)) AND (TITLE-ABS(“Pain management”) OR (TITLE-ABS(Management) AND TITLE-ABS(Pain)) OR (TITLE-ABS(Managements) AND TITLE-ABS(Pain)) OR TITLE-ABS(“Pain Managements”) OR TITLE-ABS(analgaesia) OR TITLE-ABS(“pain management”) OR TITLE-ABS(“pain relief”) OR TITLE-ABS(analgesia) OR TITLE-ABS(“Pain Thresholds”) OR (TITLE-ABS(Thresholds) AND TITLE-ABS(Pain)) OR (TITLE-ABS(Threshold) AND TITLE-ABS(Pain)) OR TITLE-ABS(“Heel stick”) OR TITLE-ABS(“Heel lance”) OR TITLE-ABS(“heel puncture”) OR TITLE-ABS(“heel prick”) OR TITLE-ABS(“blood sampling”) OR TITLE-ABS(“blood collecting”) OR TITLE-ABS(“blood collection”) OR TITLE-ABS(“blood sample”) OR TITLE-ABS(“blood specimen collection”) OR (TITLE-ABS(Sampling) AND TITLE-ABS(blood))) AND PUBYEAR > 1975 AND PUBYEAR < 2024 AND NOT PUBDATETXT (“December 2024”) |
1051 (1037 14 Conference paper) |
| Cochrane Central Register of Controlled Trials Issue 11 of 12, November 2024 |
#1 (“non-nutritive sucking” OR “Sucking Behavior” OR (Behaviors:ti,ab AND Sucking:ti,ab) OR (Behavior:ti,ab AND Sucking:ti,ab) OR “Sucking Behaviors”:ti,ab OR (non-nutritive:ti,ab AND suck*:ti,ab) OR “Non-nutritional sucking” OR “Non nutritional sucking” OR (non-nutritional:ti,ab AND suck*:ti,ab) OR “Finger Sucking”:ti,ab OR Fingersucking:ti,ab OR (Sucking:ti,ab AND Finger:ti,ab) OR Thumbsucking:ti,ab OR “Thumb Sucking”:ti,ab OR (Sucking:ti,ab AND Thumb:ti,ab) OR Pacifier:ti,ab OR Pacifiers:ti,ab OR Dummy:ti,ab OR soother:ti,ab OR nipple:ti,ab) = 8349 #2 (“Pain management”:ti,ab OR (Management:ti,ab AND Pain:ti,ab) OR (Managements:ti,ab AND Pain:ti,ab) OR “Pain Managements”:ti,ab OR analgaesia:ti,ab OR “pain management”:ti,ab OR “pain relief”:ti,ab OR analgesia:ti,ab OR “Pain Thresholds”:ti,ab OR (Thresholds:ti,ab AND Pain:ti,ab) OR (Threshold:ti,ab AND Pain:ti,ab) OR “Heel stick”:ti,ab OR “Heel lance”:ti,ab OR “heel puncture”:ti,ab OR “heel prick”:ti,ab OR “blood sampling”:ti,ab OR “blood collecting”:ti,ab OR “blood collection”:ti,ab OR “blood sample”:ti,ab OR “blood specimen collection”:ti,ab OR (Sampling:ti,ab AND blood:ti,ab)) 104478 #3 #1 AND #2 743 |
657 traials |
| Web of Science | (ALL=”non-nutritive sucking” OR ALL=”Sucking Behavior” OR ((TI=Behaviors OR AB=Behaviors) AND (TI=Sucking OR AB=Sucking)) OR ((TI=Behavior OR AB=Behavior) AND (TI=Sucking OR AB=Sucking)) OR (TI=”Sucking Behaviors” OR AB=”Sucking Behaviors”) OR ((TI=non-nutritive OR AB=non-nutritive) AND (TI=suck* OR AB=suck*)) OR ALL=”Non-nutritional sucking” OR ALL=”Non nutritional sucking” OR ((TI=non-nutritional OR AB=non-nutritional) AND (TI=suck* OR AB=suck*)) OR (TI=”Finger Sucking” OR AB=”Finger Sucking”) OR (TI=Fingersucking OR AB=Fingersucking) OR ((TI=Sucking OR AB=Sucking) AND (TI=Finger OR AB=Finger)) OR (TI=Thumbsucking OR AB=Thumbsucking) OR (TI=”Thumb Sucking” OR AB=”Thumb Sucking”) OR ((TI=Sucking OR AB=Sucking) AND (TI=Thumb OR AB=Thumb)) OR (TI=Pacifier OR AB=Pacifier) OR (TI=Pacifiers OR AB=Pacifiers) OR (TI=Dummy OR AB=Dummy) OR (TI=soother OR AB=soother) OR (TI=nipple OR AB=nipple)) AND ((TI=”Pain management” OR AB=”Pain management”) OR ((TI=Management OR AB=Management) AND (TI=Pain OR AB=Pain)) OR ((TI=Managements OR AB=Managements) AND (TI=Pain OR AB=Pain)) OR (TI=”Pain Managements” OR AB=”Pain Managements”) OR (TI=analgaesia OR AB=analgaesia) OR (TI=”pain management” OR AB=”pain management”) OR (TI=”pain relief” OR AB=”pain relief”) OR (TI=analgesia OR AB=analgesia) OR (TI=”Pain Thresholds” OR AB=”Pain Thresholds”) OR ((TI=Thresholds OR AB=Thresholds) AND (TI=Pain OR AB=Pain)) OR ((TI=Threshold OR AB=Threshold) AND (TI=Pain OR AB=Pain)) OR (TI=”Heel stick” OR AB=”Heel stick”) OR (TI=”Heel lance” OR AB=”Heel lance”) OR (TI=”heel puncture” OR AB=”heel puncture”) OR (TI=”heel prick” OR AB=”heel prick”) OR (TI=”blood sampling” OR AB=”blood sampling”) OR (TI=”blood collecting” OR AB=”blood collecting”) OR (TI=”blood collection” OR AB=”blood collection”) OR (TI=”blood sample” OR AB=”blood sample”) OR (TI=”blood specimen collection” OR AB=”blood specimen collection”) OR ((TI=Sampling OR AB=Sampling) AND (TI=blood OR AB=blood))) AND PY=(1975-2024) |
716 (690+26 Gray literature) |
| Google scholar | allintitle: “non-nutritive sucking” + (premature | preterm) = 165 allintitle: pacifier + (preterm | premature) = 46 allintitle: “non-nutritive sucking” + heel = 32 allintitle: “non-nutritive sucking” + pain = 73 |
336 |
2.7. Comparison
Preterm neonates who received no intervention or received other intervention(s) in addition to NNS.
2.8. Outcome
Pain score measured using any type of neonatal pain assessment tool. The secondary outcomes were HR and SpO2.
The exclusion criteria were as follows: (a) review articles, commentaries, and articles published in languages other than English; (b) absence of detailed information regarding clinical efficacy; and (c) duplicate publications reporting the same results. The specifics of the included studies are presented in 2.
2.9. Study Selection and Screening
Following the import of search results into EndNote software (Version X21; Clarivate Analytics Inc., Philadelphia, PA, USA), duplicate records were removed. The remaining articles were transferred to Rayyan, an AI-powered systematic review management platform (https://new.rayyan.ai/), where titles and abstracts underwent preliminary screening against predefined eligibility criteria. Studies were categorized as “include,” “exclude,” or “maybe” for inclusion. Following this initial phase, full-text versions of potentially eligible articles were independently evaluated by two reviewers (NA, JN) to confirm relevance prior to data extraction. Additionally, we held online discussions to share search results, determine next steps, resolve discrepancies regarding articles labeled “maybe,” and achieve consensus on the inclusion of selected articles.
2.10. Data Extraction
Data extraction was independently conducted by two researchers using a structured table in Microsoft Word. This table included details such as the publication year, first author's name, study country, participant demographics (sample size, gestational age, birth weight), number of study groups, intervention methods, pain measurement tool, and the study's results and outcomes.
2.11. Risk of Bias Assessment
Methodological quality assessment for the included trials was conducted independently by NA and JN using the Cochrane RoB-2 tool [21]. Reviewers evaluated five specific aspects: randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Extracted trial data informed the assignment of one of three judgments to each aspect: “low risk” (no obvious error detected), “high risk” (appropriate methods not employed), or “some concerns” (insufficient data to determine risk). Any disagreements between reviewers were resolved by a third investigator (ZS) Table 3.
| Author/Year | Country | N | Gestational Age (Week) | Birth Weight (kg) | Groups and Interventions | Method | Pain Measurement Tool | Results |
|---|---|---|---|---|---|---|---|---|
| Fathia A (2009) [27] | Saudi Arabia | 36 | 32.4 Range: 27 to 36 |
1.7 ± 0.6 | 1. W*+P*)n=36) 2. W)n=36) 3. OS*+P)n=36) 4. OS)n=36) 5. P)n=36) 6. Control group)n=36) |
1. W+P: 0.5 mL sterile water with a pacifier 2. W: 0.5 mL sterile water without pacifier 3. OS+P: 0.5 mL sucrose 24% with pacifier 4. OS: 0.5 mL sucrose 24% without pacifier 5. P: pacifier alone given to the neonate 2 minutes before the procedure 6. Control group |
PIPP* | A combination of oral sucrose and non-nutritive sucking was more effective in reducing heel stick pain compared to the control group |
| Jen-Jiuan Liaw (2010) [17] | Taiwan | 104 | 33.15 Range: 28.86 to 37 |
1.7 ± 0.38 | 1. NNS*(n=52) 2. Control group(n=52) |
1. NNS: An appropriately sized and standard silicone pacifier, provided to the experimental group before and during heel stick procedures. 2. Control group: No intervention was done |
PIPP | NNS effectively reduced mild to moderate pain. |
| Jen-Jiuan Liaw (2012) [18] | Taiwan | 102 | 33.06 ± 2.02 Range: 29 to 37 |
1.7 ± 0.36 | 1. Control group +NNS+FT (n=34) 2. NNS+FT+ Routine care (n=34) 3. FT+ Routine care +NNS (n=34) |
1. Control group 2. NNS: neonates were given a standard silicone. 3. FT: Infants were gently held by a nurse in a flexed position, with one hand on the head and the other on the buttocks, during the heel stick procedure by the physician assistant. |
PIPP | FT reduced heel stick pain more than two other groups. |
| Anne Perroteau (2018) [1] | France | 59 | 29.0 (28.0, 31.0) Range: 28 to 32 |
1.3 (1.13, 1.53) | 1. NNS, control group(n=29) 2. NNS+FT(n=30) |
The facilitated tucking was performed by a nurse or nursing assistant, with the infant's arms and legs held in a flexed position close to the midline of the chest, and the nurse's hands gently placed under the neck and on the buttocks. This was maintained for at least 15 seconds before the heel-stick procedure and for 3 minutes after. | PIPP DAN* |
There was no significant difference between the three groups. |
| Hiroko Uematsu (2019) [30] | Japan | 25 | 33.8 ± 1.5 Range: 32 to 35 |
1.9 ± 0.38 | 1. Music +NNS +FT +Holding (n=15) 2. Control group (FT+Holding) (n=10) |
1. After an initial assessment, the infant was given a pacifier and placed in a flexed position. Then, A CD player softly played Brahms' lullaby at a volume of 65-75 dB, positioned 20-25 cm from the infant's head. 2. control group: they received only facilitated tucking and holding. |
PIPP | The participants in the intervention group experienced less pain compared to the control group. |
| Haixia Gao (2018) [28] | China | 86 | 31.7 ± 0.9 | 1.7 ± 0.26 | 1. Control group (n = 21) 2. NNS (n = 22) 3. OS (n = 21) 4. OS + NNS (n = 22) |
1. Control group: The preterm neonate received only routine comfort through gentle touch when he cried after the heel stick procedure. 2. NNS: A standard silicone pacifier was given to the neonate two minutes before the procedure and throughout the procedure. 3. OS: Sucrose 20% (0.2 ml/kg) was administered orally by a 1 ml syringe without the needle in 2 min before the heel stick procedure 4. OS+NNS: The combination of sucrose 20% (0.2 mL/kg) administered orally 2 minutes before the heel stick, followed by non-nutritive sucking using a standard silicone newborn pacifier until the recovery phase. |
PIPP | A combination of non-nutritive sucking and oral sucrose was more effective in reducing pain than either one alone. |
| Hsueh-Fang Peng (2018) [29] | Taiwan | 109 | 31.21 ± 2.87 | 1.56± 0.48 | 1. Control group(n=36) 2. NNS+BM (n=37) 3. NNS+BM+FT (n=36) |
1. Control group: Before, during, and after the heel stick, neonates in the control condition received routine care. The neonates were gently touched if they started to cry. 2. NNS: pacifier alone given to the neonate 2 minutes before the procedure. 3. For the breast milk condition, neonates were orally fed 0.5–2.0 ml of expressed breast milk through a syringe 2 min before a heel stick. 4. FT: The infant was gently held in a flexed, midline position by the nurse before the heel stick procedure. |
PIPP | A combination of NNS, breast milk, and FT reduced moderate to severe pain during heel stick. |
| Defi Efendi (2018) [8] | Indonesia | 30 | Range 26-36 | - | 1. Pacifier + swaddling (n=15) 2. Routine care(n=15) |
1. Pacifier swaddling: NR** 2. Control group: NR |
PIPP | A combination of pacifier and swaddling prevented an increase in pain during intensive procedures. |
** NR: not reported
| Bias domain | 1-Bias arising from the randomization process | 2-Bias due to deviations from intended interventions | 3-Bias due to missing outcome data | 4-Bias in the measurement of the outcome | 5-Bias in the selection of the reported result | Overall risk of bias judgement | |
|---|---|---|---|---|---|---|---|
| ID | Author | ||||||
| 1 | Haixia Gaoa 2018 | LR | LR | LR | LR | LR | LR |
| 2 | Hiroko Uematsu 2018 | LR | UR | LR | UR | LR | UR |
| 3 | Hsueh-Fang Peng 2018 | LR | LR | LR | UR | LR | UR |
| 4 | Anne Perroteau 2018 | LR | UR | LR | HR | LR | HR |
| 5 | Jen-Jiuan Liaw 2012 | LR | UR | LR | LR | LR | UR |
| 6 | Jen-Jiuan Liaw 2010 | LR | LR | LR | LR | LR | LR |
| 7 | Fathia A. Elserafy 2010 | UR | LR | LR | LR | LR | UR |
| 8 | Defi efendi | UR | UR | LR | LR | LR | UR |
2.12. Statistical Analysis
All statistical analyses were performed using Review Manager (RevMan 5.3) software (The Nordic Cochrane Centre, Copenhagen, Denmark). Continuous data are presented as mean ± standard deviation (SD), and pooled rates with 95% confidence intervals (CI) are reported for each group. Standardized mean differences (SMDs) comparing the non-nutritive sucking (NNS) group to controls are provided alongside 95% CIs. Statistical significance was set at a P-value less than 0.05. The DerSimonian and Laird random-effects model was applied for the meta-analysis, and forest plots were created for both primary outcomes (pain scores) and secondary outcomes (heart rate and oxygen saturation). Heterogeneity among studies was assessed using the I2 statistic, with thresholds of 0–30%, 31–60%, 61–75%, and 76–100% indicating low, moderate, substantial, and considerable heterogeneity, respectively.
3. RESULT
A total of 6,216 articles were retrieved through database and manual searches, with an additional 28 references identified through manual searching. After removing duplicates and excluding irrelevant studies based on title and abstract screening, eight full-text articles were assessed and selected for meta-analysis. Furthermore, the reference lists of the included studies were manually reviewed, but no additional relevant papers were identified (Diagram 1).
These studies included 225 newborns, with 116 in the NNS group and 109 in the control group. Male neonates comprised 58.5 percent of the subjects (n = 131). The mean gestational age (GA) was 31.6 ± 2.02 weeks, and the mean birth weight was 1632.2 ± 322.8 g.
The characteristics of the NNS interventions were reported in most of the studies Table 2. Eight randomized clinical trials were included in the systematic review. One study compared NNS with oral sucrose and the combination of both techniques. A second study compared a combination of music, NNS, facilitated tucking, and holding versus a combination of facilitated tucking and holding. A third study compared sucking + breast milk and sucking + breast milk + tucking versus routine care. A fourth study compared a combination of NNS and facilitated tucking with NNS alone. A fifth study compared combined NNS and facilitated tucking with routine care. A sixth study compared NNS with routine care. A seventh study compared pharmacologic measures with non-pharmacologic measures. The final study compared NNS and swaddling with routine care.
In one study, the control group received no intervention. In the remaining studies, the control group received NNS, facilitated tucking, or routine care. Facilitated tucking, holding, and routine comfort through gentle touch were considered inactive control interventions.
4. SYNTHESIS OF RESULTS
4.1. Pain Score
Eight studies exclusively provided data based on the Premature Infant Pain Profile (PIPP). All included articles utilized the Premature Infant Pain Profile (PIPP), a 7-indicator composite measure designed to evaluate acute pain in both preterm and term neonates. The PIPP incorporates three behavioral (facial actions), two physiological (HR and oxygen saturation), and two contextual (gestational age and behavioral state) items, all derived theoretically and experimentally [24]. Due to unavailable data regarding changes in pain scores in three studies, these studies were excluded from the analysis.
The combined analysis using a random-effects model across five studies (total n = 225) showed a significant difference in mean effect size between the non-nutritive sucking (NNS) and control groups (overall Z = 5.79, P < 0.001; standardized mean difference [SMD] = -0.83, 95% CI: -1.11 to -0.55), with substantial heterogeneity (I2 = 77%). These findings indicate that pain scores were markedly lower in the NNS group compared to the control group Fig. (1).
4.2. Heart Rate (HR)
In a collective analysis involving 98 preterm neonates across three studies, the impact of NNS on heart rate reduction was assessed. The combined results from a random-effects model demonstrated a statistically significant effect of NNS in reducing HR in preterm neonates compared to controls (overall effect Z = 2.50, P = 0.01; SMD = -0.52, 95% CI: -0.92 to -0.11; I2 = 0.0 percent) Fig. (2). This reduction was considered clinically significant.
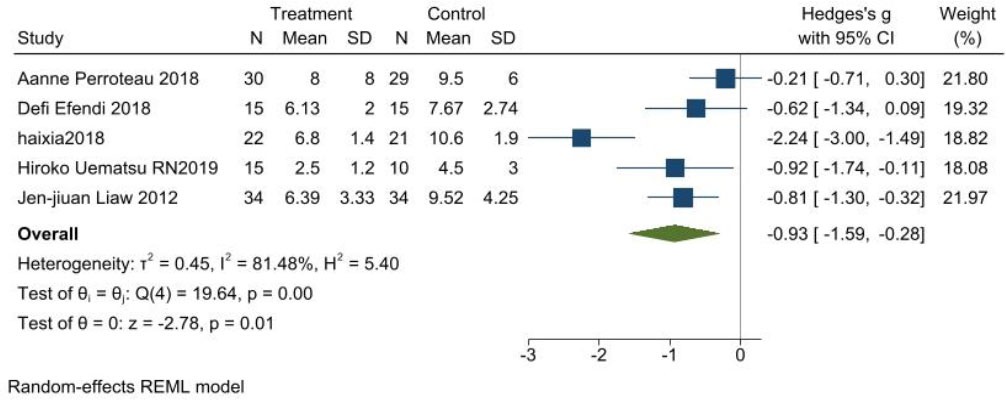
Meta-analysis of pain score.
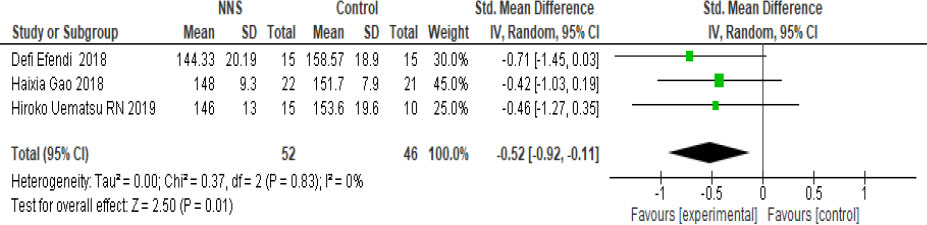
Meta-analysis of heart rate (HR).
4.3. Oxygen Saturation (O2 Sat)
A meta-analysis of three trials (n = 98) revealed no significant difference in oxygen saturation between the NNS and control groups (SMD = -0.04, 95% CI: -0.44 to 0.36; Z = 0.20, P = 0.84), with negligible heterogeneity (I2 = 0 percent) (Fig. 3).
4.4. Publication Bias
To evaluate publication bias in the five included studies, a funnel plot was generated. The absence of asymmetry in the Premature Infant Pain Profile (PIPP) funnel plot indicated no publication bias among the included studies (Fig. 4).
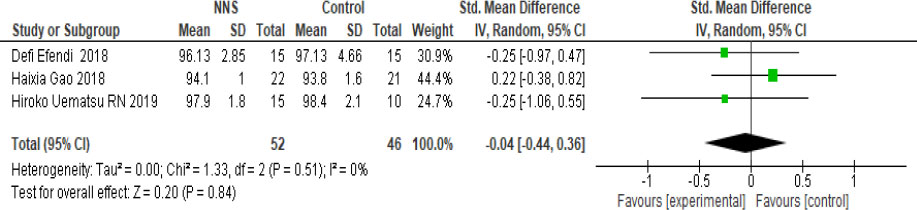
Meta-analysis of oxygen saturation (O2 sat).
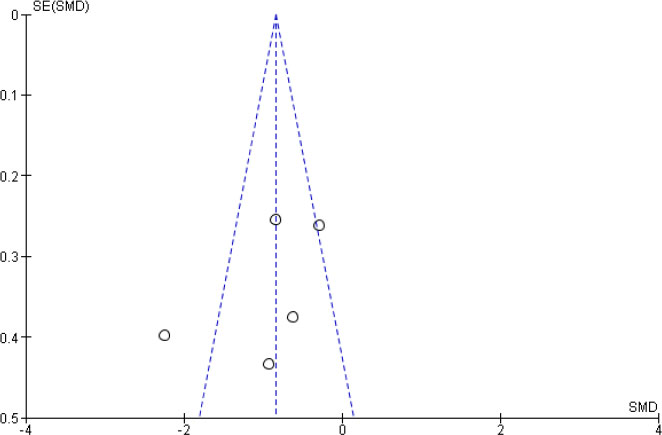
Funnel plot evaluating publication bias
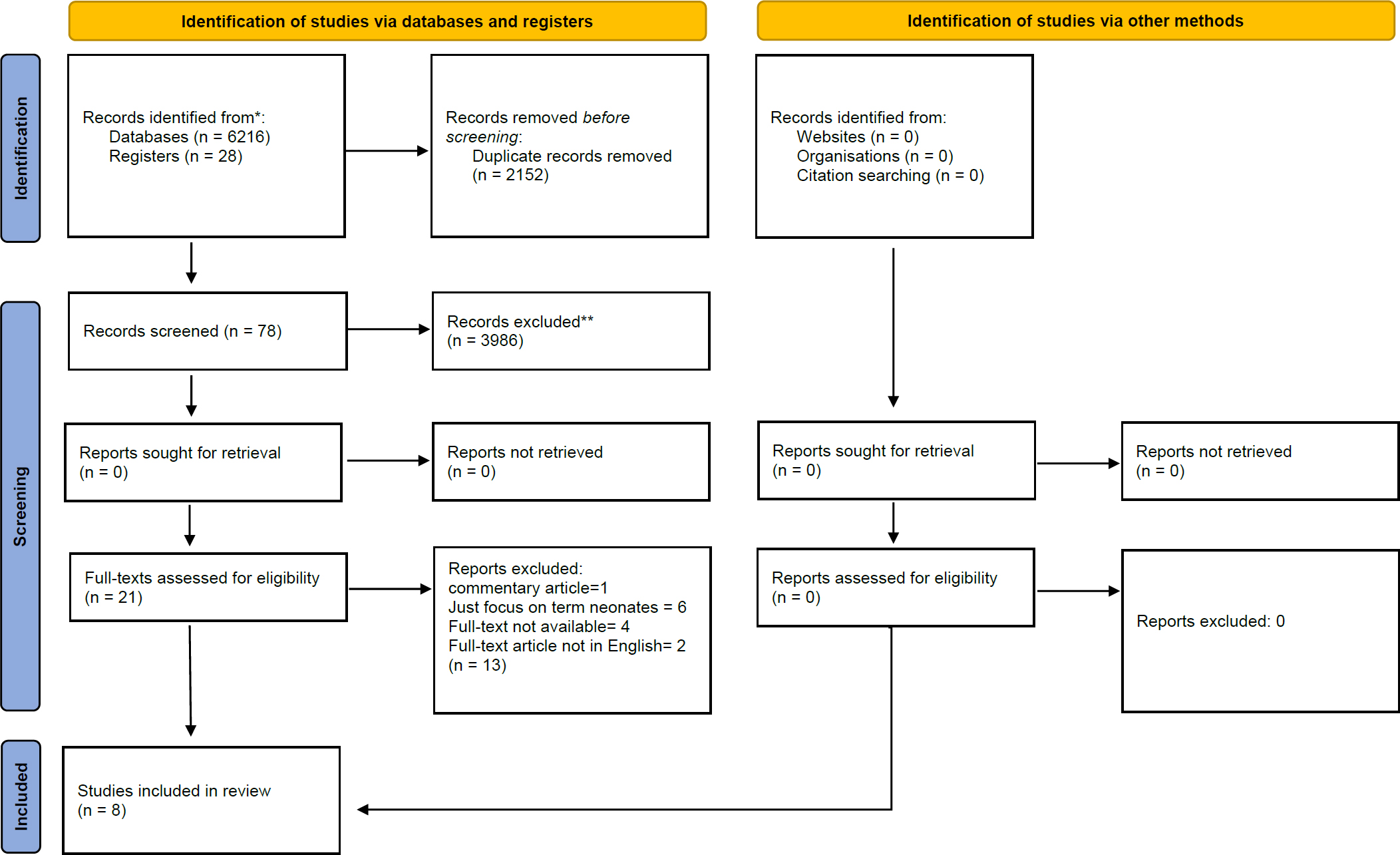
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. Doi: 10.1136/bmj.n71.
5. DISCUSSION
Neonates, particularly preterm infants, exhibit heightened sensitivity to pain [1, 22]. Consequently, effective pain management is a critical component of care in the Neonatal Intensive Care Unit (NICU). Several studies have demonstrated the effectiveness of Non-Nutritive Sucking (NNS) in pain control [14-23]. The proposed analgesic effect is thought to involve stimulation of oral mechanoreceptors, which may modulate nociceptive transmission or perception through endogenous non-opioid pathways. This intervention should be used only when neuromuscular coordination has sufficiently developed to initiate oral feeding [17].
Heel stick is one of the most common procedures in NICUs [7, 15, 17], yet the analgesic effects of NNS in neonates, especially preterm infants, remain unclear. Therefore, this meta-analysis was conducted to evaluate the effectiveness of NNS in reducing heel-stick pain severity among preterm neonates.
The present systematic review and meta-analysis found that NNS is an effective method of managing pain in preterm neonates. A previous systematic review examining distraction techniques for young children undergoing medical procedures reported that toy-based distraction did not reduce post-needle pain scores. This may be attributed to inconsistent implementation and the fact that some children perceive physical contact from medical staff as intimidating; initiating distraction only at the moment of contact may have limited its effectiveness. In contrast, the present review focused exclusively on preterm infants and used NNS to minimize the influence of physical contact on outcomes [24].
Another systematic review on oral sucrose for neonatal pain relief showed that sucrose effectively reduces procedural pain. However, the optimal dosage was not established due to variability across studies. The present review focused solely on NNS as a safer and more accessible technique that does not require administration of additional substances or dose adjustments [23]. A similar systematic review on full-term neonates also confirmed the analgesic benefits of NNS during heel stick procedures [13]. However, unlike that review, our study specifically targeted preterm neonates, who are more sensitive to pain and whose pain management needs are especially critical.
Other evidence supports the analgesic role of NNS in various neonatal procedures. For example, NNS has been shown to significantly reduce pain during retinopathy screening [25] and to have a longer duration of action than sucrose [26]. Haixia Gao et al. [27] reported that while both NNS and sucrose reduced the duration of crying during heel stick in preterm neonates, neither intervention reduced the physiological response to pain. Other studies have suggested that NNS and sucrose have comparable effects on heel stick pain reduction.
Overall, there is strong evidence that NNS reduces pain behaviors during procedures such as heel stick and injections [28]. Although combined interventions such as NNS plus sucrose are effective, sucrose intake is restricted in preterm neonates [23]. Therefore, identifying methods that minimize pain with minimal risk is a major priority for clinicians. According to the Gate Control Theory, the use of a pacifier may inhibit transmission of pain impulses along the spinothalamic tract, thereby reducing pain perception. NNS may further decrease pain-related behaviors and mitigate associated complications [8]. Additionally, it is cost-effective, requires no advanced technology, and can be administered by parents.
The present meta-analysis also found that NNS was relatively effective in stabilizing heart rate (HR) during the recovery phase following heel stick compared with routine care. In three included studies, no baseline differences were observed between groups, and both groups demonstrated HR increases during the procedure due to pain. However, our findings differed from those of Yi Liu et al. [22], who reported no effect of NNS on HR after painful interventions. This discrepancy may be explained by the combined use of sucrose and NNS in their study. The limited number of comparative studies available in the literature highlights the need for further research. Hiroko Uematsu et al. [29] found that NNS combined with music (Brahms’ lullaby) decreased HR following heel stick in preterm neonates and resulted in fewer abnormal HR fluctuations.
Regarding oxygen saturation, baseline levels did not differ significantly between groups. Consistent with Yi Liu et al. [22], our meta-analysis found no significant difference in oxygen saturation between the NNS and control groups during the recovery period after heel stick.
6. STRENGTHS AND LIMITATIONS
This meta-analysis is the first comprehensive synthesis focusing exclusively on the effects of pure NNS interventions for reducing the severity of heel-stick pain in preterm neonates. However, the findings highlight a significant shortage of high-quality research in this area. Several limitations should be acknowledged. First, most included studies had relatively small sample sizes, which may influence effect size estimates, the statistical power of findings, and the methodological rigor required to minimize bias. Second, the presence of single-center studies limits the generalizability of the results, particularly in the context of small study populations. Third, the potential influence of confounding variables—such as neonatal hunger or discomfort, and prior exposure to painful procedures—may affect behavioral and physiological pain responses, underscoring the need for future research to monitor and control these factors. Finally, because this review included only English-language publications, relevant studies in other languages may have been inadvertently excluded.
CONCLUSION
Recognizing the heightened sensitivity to pain among preterm neonates, effective pain management is essential for this vulnerable population. Findings from this systematic review and meta-analysis indicate that NNS may be effective in reducing heel-stick–related pain behaviors; however, the limited number of available studies and their relatively small sample sizes restrict the generalizability of these results. Therefore, future research should prioritize larger, multicenter randomized controlled trials to validate and further elucidate the comparative effectiveness of non-pharmacological interventions for procedural pain in preterm infants. Overall, these findings offer meaningful guidance for nurses and clinicians, supporting the use of NNS as a practical, accessible strategy to minimize repeated procedural pain in preterm neonates.
AVAILABILITY OF DATA AND MATERIALS
Data openly available in a public repository that issues datasets with DOIs.
AUTHORS’ CONTRIBUTIONS
The authors confirm contribution to the paper as follows: J.N. and N.A.: Contributed to the study design, data collection, and data analysis; NA, Z.S. and J.N.: Contributed to quality assessment; J.N., L.A. and B.K.: Contributed to manuscript writing and supervised the study. All authors agreed on the final version.
LIST OF ABBREVIATIONS
| PRISMA | = Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| NICU | = Neonatal Intensive Care Unit |
| FT | = Facilitated Tucking |
| OS | = Oral Sucrose |
| NNS | = Non-Nutritive Sucking |
| BM | = Breast Milk |
| PIPP | = Premature Infant Pain Profile |
| DAN | = Douleur Aiguë du Nouveau-Né (Acute Neonatal Pain) |
USE OF ARTIFICIAL INTELLIGENCE
In this study, we used Microsoft Copilot, an AI-powered tool designed by Microsoft to assist with translating Farsi to English, ensuring accuracy, efficiency, and consistency in converting original Farsi texts into high-quality English-language content.
REGISTRATION OF SYSTEMATIC REVIEWS
It can be found on PROSPERO at http://www.crd.york .ac.uk/PROSPERO (CRD42021219997).
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Sayeh Miri and Dr. Nahid Dehghan Nayeri, Methodologists from the University of Ilam and Tehran, for their critical review of the final version.


