All published articles of this journal are available on ScienceDirect.
Global Diphtheria Trends and Regional Disparities: A Narrative Review of the Influence of Vaccine Hesitancy, Surveillance Gaps, and Public Health Interventions
Abstract
Diphtheria remains a significant public health concern despite effective vaccines. This narrative review examines global trends in diphtheria incidence, with a focus on regional disparities, vaccine hesitancy, surveillance challenges, and public health interventions. This narrative review synthesizes global trends in diphtheria surveillance and vaccination coverage, drawing on reports from the World Health Organization (WHO), UNICEF, regional health organizations (e.g., ECDC, PAHO), and peer-reviewed literature from PubMed and Scopus, published in English between 2000 and 2023. This narrative review highlights marked regional disparities in diphtheria incidence, with higher burdens in Africa and Southeast Asia due to low vaccination coverage, in contrast to near-elimination in Europe and North America, where robust immunization programs have been implemented. Despite effective surveillance in some countries, underreporting, incomplete data, and inadequate laboratory capacity hinder timely responses to outbreaks, particularly in low-resource settings. Vaccine hesitancy, geopolitical factors, and surveillance gaps further complicate global control efforts. High vaccination coverage is crucial for achieving herd immunity and reducing the incidence of diseases. Community engagement and targeted vaccination campaigns are crucial for enhancing outcomes, alongside the implementation of enhanced vaccination strategies, robust laboratory infrastructure, and effective data collection practices. This narrative review underscores the need for enhanced vaccination strategies, improved surveillance, and targeted interventions to address diphtheria and other vaccine-preventable diseases.
1. INTRODUCTION
Diphtheria, an acute bacterial infection caused primarily by Corynebacterium diphtheriae, remains a significant public health concern despite the availability of effective vaccines [1, 2]. The disease is characterized by the formation of a pseudomembrane in the throat, which can obstruct the airway and lead to severe systemic complications such as myocarditis, neuropathy, and even death if untreated [3, 4]. Although the introduction of the diphtheria vaccine in the mid-20th century has drastically reduced the global burden of the disease, sporadic outbreaks persist, particularly in regions with low vaccination coverage or where vaccine hesitancy is prevalent [5, 6]. This review examines global trends in diphtheria incidence, regional disparities, and the interplay between vaccine hesitancy, surveillance gaps, and public health interventions, providing insights into strategies for enhancing disease control and management. These trends underscore the need for targeted interventions in high-risk regions to address gaps in immunization and healthcare delivery. The burden of diphtheria is not evenly distributed globally, with significant disparities between regions. Africa and Southeast Asia bear the highest burden, while Europe and North America have largely controlled the disease through robust immunization programs. For example, Sub-Saharan Africa reports DTP3 (Diphtheria, Tetanus, and Pertussis) vaccination coverage rates as low as 50% in some areas, which contributes to ongoing transmission risks [7, 8]. In contrast, Western Europe and North America maintain DTP3 coverage rates above 90%, resulting in near-elimination of the disease [5, 9].
These disparities are further exacerbated by differences in healthcare infrastructure and surveillance capabilities. In low-resource settings, underreporting and incomplete data are common, with approximately 63% of country-years reporting zero cases and 19% missing data entirely [5]. For instance, in Africa, 40% of country-years lack complete diphtheria surveillance data, highlighting significant gaps in monitoring and response efforts [5, 6]. Addressing these disparities requires strengthening healthcare systems, improving data collection, and ensuring equitable access to vaccines. Vaccine hesitancy has emerged as a critical barrier to global diphtheria control. Misinformation about vaccines has eroded trust in immunization programs, resulting in declining vaccination rates in certain regions [10, 11]. Surveillance gaps further complicate efforts to control diphtheria. Inconsistent reporting and a lack of standardized case definitions have led to discrepancies between national surveillance data and local health records. Strengthening surveillance requires standardized protocols, improved laboratory capacity, and enhanced training for healthcare workers [12]. Public health interventions play a crucial role in mitigating the impact of vaccine hesitancy and surveillance gaps. Successful strategies include community engagement campaigns to address vaccine misinformation, mobile vaccination units to reach underserved populations, and integrated surveillance systems that combine case reporting with laboratory confirmation [13, 14]. Community-based vaccination drives and partnerships with local leaders can improve immunization coverage in high-risk areas. Similarly, public health campaigns emphasizing the safety and efficacy of vaccines have helped counteract hesitancy and maintain high coverage rates [15, 16].
Diphtheria remains a persistent public health challenge, particularly in regions with low vaccination coverage and weak surveillance systems. Global trends indicate significant progress in controlling the disease in developed regions, but disparities persist in Africa and Southeast Asia, where outbreaks continue to occur. Addressing these challenges requires a multifaceted approach that includes strengthening surveillance systems, combating vaccine hesitancy, and implementing targeted public health interventions. By learning from past outbreaks and adopting best practices, countries can enhance their capacity to prevent and control diphtheria, ultimately protecting populations from this vaccine-preventable disease. Diphtheria remains a public health challenge despite effective vaccines. This narrative review explores global trends in diphtheria incidence, regional disparities, and the interplay of vaccine hesitancy, surveillance gaps, and public health interventions. While developed regions, such as Europe and North America, have nearly eliminated diphtheria through high vaccination coverage, Africa and Southeast Asia continue to face outbreaks due to low immunization rates and weak healthcare systems. Vaccine hesitancy, driven by misinformation and inconsistent surveillance, further complicates control efforts. By examining these factors, this review aims to provide insights for improving diphtheria prevention and control strategies globally.
2. MATERIALS AND METHODS
This narrative review synthesizes global evidence on diphtheria trends, surveillance, and vaccination coverage. The review focuses on studies and reports published in English from 2000 to 2023, covering diphtheria incidence, vaccination coverage, and public health interventions. We relied on secondary data obtained from published reports and peer-reviewed scientific articles. The data sources encompassed four main categories: global reports, including the World Health Organization (WHO) and the UNICEF Joint Reporting Form (JRF); regional reports, such as those from the European Centre for Disease Prevention and Control (ECDC) and the Pan American Health Organization (PAHO); country-level reports provided by national public health agencies; and peer-reviewed literature retrieved from major scholarly databases, including PubMed, Scopus.
Relevant data were extracted from selected studies, including incidence rates of diphtheria, vaccination coverage rates (specifically DTP3 coverage), case definitions and reporting mechanisms used in different countries, laboratory confirmation methods employed, and analysis of reporting trends. The completeness of reporting was assessed by comparing the number of reported cases in the JRF with those documented in published literature. This analysis aimed to identify discrepancies and gaps in the data collection process. The analysis focused on several key aspects: incidence rates, data completeness, vaccination coverage, and geographical distribution. These outcomes were summarized using both descriptive and comparative approaches. Data on global and regional incidence trends, vaccination coverage rates, and surveillance completeness were organized into structured tables (Tables 1–4) to allow clear comparison across years and regions. A line graph (Fig. 1) was created to illustrate temporal trends in global diphtheria cases and annual incidence rates between 2000 and 2015. Tables provided precise numerical values, while the graph offered a visual representation of long-term patterns. The analysis focused on several key aspects:
| Year | Total Cases | AIR (per 100,000) |
|---|---|---|
| 2000 | 5,000 | 0.30 |
| 2005 | 4,800 | 0.28 |
| 2010 | 6,200 | 0.32 |
| 2015 | 5,750 | 0.27 |
Incidence Rates: Trends in diphtheria incidence were evaluated globally from 2000 to 2017. The analysis included calculating Annual Incidence Rates (AIR) per 100,000 population for different regions to identify patterns over time.
Data Completeness: The completeness of diphtheria surveillance data was assessed by examining the percentage of country-years reporting zero cases versus those with reported cases. This included evaluating the proportion of missing data across various regions.
Vaccination Coverage: DTP3 vaccination coverage was analyzed as a critical factor influencing diphtheria incidence. Data were compared across regions to identify areas with low vaccination rates that may be at higher risk for outbreaks.
Geographical Distribution: The geographical distribution of reported diphtheria cases was mapped using Geographic Information Systems (GIS) tools to visualize trends and identify potential outbreak hotspots. Using ArcGIS (version 10.8, ESRI, Redlands, CA, USA) and QGIS (version 3.22, OSGeo), we generated country- and region-level maps based on WHO/UNICEF JRF data.
3. RESULTS
The analysis of global diphtheria surveillance systems yielded significant insights into incidence trends, data completeness, vaccination coverage, and regional variations. The findings are organized into several key categories:
3.1. Incidence Trends
3.1.1. Global Incidence Rates
From 2000 to 2017, the global incidence of diphtheria exhibited notable fluctuations. The analysis revealed:
Total Reported Cases: Approximately 106,750 diphtheria cases were reported across 97 countries between 2000 and 2015. This data indicates a concerning persistence of the disease in various regions [6, 17].
Annual Incidence Rate (AIR): The overall AIR for diphtheria during this period was approximately 0.29 cases per 100,000 population; however, this figure masks significant regional disparities and variations over time [18].
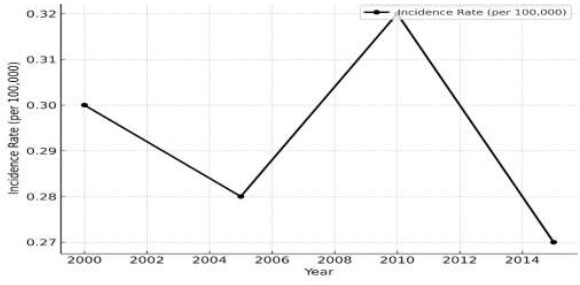
The global incidence trends and annual incidence rates of disease cases from 2000 to 2015.
3.2. Incidence Trends
3.2.1. Global Incidence Rates
- Total Reported Cases: 106,750 cases from 2000 to 2015 across 97 countries.
- Annual Incidence Rate (AIR): Approximately 0.29 per 100,000 population.
Table 1 illustrates the global incidence trends and annual incidence rates of disease cases from 2000 to 2015
3.3. Regional Variations
Africa: The African region reported the highest incidence rates, with outbreaks occurring in countries such as Nigeria and the Democratic Republic of the Congo. Some areas experienced AIRs reaching as high as 3.5 per 100,000 population during outbreaks [19, 20].
Southeast Asia: Countries such as Indonesia and Myanmar have experienced sporadic outbreaks due to low vaccination coverage; the incidence has fluctuated significantly, with some years reporting over 1,000 cases [21].
Europe and North America: In contrast, Europe and North America have seen a dramatic decline in diphtheria cases due to high vaccination rates; however, isolated outbreaks still occur, primarily among unvaccinated populations or communities with vaccine hesitancy [22].
3.3.1. Regional Variations
- Africa: The highest incidence, with some regions reaching 3.5 cases per 100,000.
- Southeast Asia: Sporadic outbreaks, significant fluctuations.
- Europe & North America: Low incidence due to high vaccination rates.
Table 2 shows the average annual incidence rates and notable disease outbreaks in different regions.
| Region | Average AIR | Notable Outbreaks |
|---|---|---|
| Africa | 1.5 | Nigeria, DRC |
| Southeast Asia | 0.5 | Indonesia, Myanmar |
| Europe & N. America | 0.01 | Isolated cases |
3.4. Data Completeness
3.4.1. Reporting Gaps
The completeness of diphtheria surveillance data varied significantly across regions:
Zero Reporting: Approximately 63% of country-years reported zero cases during the study period, indicating a lack of active surveillance or underreporting in many areas [18].
Missing Data: Globally, approximately 19% of country-years had missing data on diphtheria cases; in Africa, this figure was around 40%, indicating substantial gaps in surveillance efforts [17].
3.4.2. Inconsistencies in Reporting
Cross-referencing JRF data with published literature revealed discrepancies:
In several instances, published studies reported more cases than those recorded in JRF submissions; for example, local health authorities documented significantly higher case numbers than those reported to WHO in India [23].
These inconsistencies highlight potential weaknesses in national reporting systems, underscoring the need for standardized case definitions and reporting protocols.
3.4.3. Data Completeness
- Zero Reporting: 63% of country-years reported zero cases.
- Missing Data: 19% globally, 40% in Africa.
Table 3 presents the data completeness, including zero reporting and Missing Data, by Region.
| Region | % Zero Reporting | % Missing Data |
|---|---|---|
| Global | 63% | 19% |
| Africa | 50% | 40% |
| Other Regions | 70% | 10% |
3.5. Vaccination Coverage
Vaccination coverage remains a crucial determinant of diphtheria incidence:
3.5.1. DTP3 Coverage Rates
Global Coverage: As of 2020, global DTP3 vaccination coverage was estimated at approximately 86%, but it varies widely by region [24]. High coverage is essential for maintaining herd immunity.
3.5.2. Regional Disparities
In Sub-Saharan Africa and parts of Southeast Asia, DTP3 coverage rates fell below 70% contributing to ongoing transmission risks; Nigeria reported DTP3 coverage as low as 50% in certain states.
Conversely, Western Europe and North America reported DTP3 coverage exceeding 90% correlating with lower incidence rates of diphtheria [25].
3.5.3. Vaccination Coverage
- Global DTP3 Coverage: 86% as of 2020.
- Regional Disparities: Sub-Saharan Africa and parts of Southeast Asia were below 70%.
Table 4 shows the Vaccination Coverage: Global and Regional DTP3 Rates.
| Region | DTP3 Coverage (%) |
|---|---|
| Global | 86% |
| Sub-Saharan Africa | 65% |
| Southeast Asia | 70% |
| Western Europe | 95% |
| North America | 92% |
3.6. Impact of Vaccine Hesitancy
Vaccine hesitancy has emerged as a significant barrier:
Surveys indicate that misinformation about vaccines significantly contributes to parents' hesitancy regarding childhood immunizations; this has been particularly evident during the COVID-19 pandemic, when trust in health systems eroded [26].
Recent outbreaks have been directly linked to areas with low vaccination rates, primarily due to individuals' hesitancy. Romania’s outbreak in 2016 serves as an example, where declining vaccinations fueled a resurgence among unprotected populations [27, 28].
3.7. Summary of Findings
Overall results indicate that while some regions have established effective surveillance systems, significant challenges remain; high completeness and timeliness rates observed within developed nations contrast sharply against lower performance indicators seen throughout low-resource settings; successful identification management during recent outbreaks demonstrates the critical role effective monitoring plays in controlling incidences, guiding public health interventions moving forward. Findings emphasize the need for continuous investment in strengthening infrastructure, training healthcare providers, and community engagement efforts aimed at increasing vaccine uptake and improving overall outcomes related to prevention and control measures against diseases such as diphtheria globally.
4. DISCUSSION
This narrative review highlights the persistent challenge of diphtheria in regions with low vaccination coverage and weak surveillance systems. While developed regions have successfully controlled the disease, Africa and Southeast Asia face ongoing outbreaks due to inadequate immunization and healthcare infrastructure. Vaccine hesitancy, fueled by misinformation, remains a critical barrier, as seen in recent outbreaks. Public health interventions, including community engagement and mobile vaccination units, are crucial for addressing these challenges. Continued investment in surveillance, laboratory capacity, and public trust in vaccines is crucial for global diphtheria control.
4.1. Strengths of Current Surveillance Systems
Implementation of Case-Based Surveillance: Countries such as India and Brazil have adopted case-based approaches, enhancing both quality and response capabilities, allowing for better tracking of individual cases and facilitating timely interventions during outbreaks [29].
Global Reporting Mechanisms: The WHO/UNICEF Joint Reporting Form provides a standardized framework that enables countries to report annual aggregate data, allowing for regional comparisons and facilitating the identification of areas needing targeted interventions, thereby effectively combating disease spread over time [30].
Increased Awareness Response Capacity: Recent outbreaks have prompted governments and health organizations to prioritize their respective monitoring and response efforts, leading to increased funding resources dedicated to controlling diseases like diphtheria. Yemen’s resurgence due to conflict has resulted in international support aimed at bolstering vaccination campaigns, enhancing overall monitoring capabilities [31].
4.2. Challenges Surveillance Systems Face
Underreporting of Incomplete Data: One major challenge identified remains underreporting, particularly prevalent in low-resource settings where access to healthcare is limited, resulting in approximately sixty-three percent of country-years reporting zero cases, indicating a lack of active monitoring and inadequate mechanisms present, hindering effective response measures against potential threats posed by diseases like Diphtheria [32].
Variability in Laboratory Capacity: The capacity to confirm diagnoses through laboratory testing varies widely among nations, resulting in many low-income regions lacking sufficient access to diagnostic facilities. This ultimately leads to lower percentages of suspected cases being confirmed, thereby impacting the overall quality and effectiveness of monitoring [33].
Vaccine Hesitancy Critical Barrier Achieving Optimal Coverage Rates: Misinformation regarding vaccines, especially prevalent on social media platforms, contributes to declining trust in immunization programs, posing a significant risk of resurgence of diseases previously controlled through established protocols [34]; addressing hesitancy requires targeted communication strategies engaging communities, building confidence, and public health initiatives effectively combating misinformation spread throughout populations [35].
Geopolitical Factors Impacting Healthcare Infrastructure: Ongoing conflicts and political instability in certain areas severely impact the ability to maintain adequate levels of service delivery, thereby disrupting routine activities necessary ensuring continued protection vulnerable individuals against threats posed by infectious agents like Diphtheria [36]; global health organizations must prioritize support nations facing such crises ensuring continued disease control efforts amidst challenging circumstances [37].
4.3. Recommendations
To strengthen global Diphtheria Surveillance Systems, several recommendations can be made:
(1) Enhancing Data Collection Practices: Standardizing reporting protocols across nations improves quality comparability, ultimately leading to better decision-making processes based on reliable evidence obtained through accurate identification of suspected cases [38]; training healthcare providers to understand the definitions and requirements essential to ensure proper identification occurs consistently throughout all levels of healthcare delivery systems involved in managing these infectious diseases effectively.
(2) Investing Laboratory Capacity: Expanding laboratory capabilities, training programs, resource allocation, and partnerships with regional facilities significantly improve diagnostic accuracy and the turnaround time of test results, ultimately enhancing the overall effectiveness of monitoring activities performed within respective jurisdictions involved in combating threats posed by infectious agents such asdiphtheria [39]; Mobile laboratories and telemedicine solutions also help bridge gaps in rural areas, improving accessibility to essential services needed to respond to emerging situations that require immediate attention promptly.
(3) Community Engagement Initiatives: Public health campaigns aimed at increasing awareness of the importance of vaccinations should be prioritized, engaging community leaders, healthcare workers, and local organizations to help address hesitancy effectively and foster trust in initiatives designed to protect populations vulnerable to diseases previously controlled through established protocols [40]. Tailored communication strategies that resonate well at the local level are essential for fostering confidence and participation in programs designed to improve uptake levels among targeted demographics most at risk of contracting illnesses preventable through routinely offered immunizations.
(4) Utilizing Technology Surveillance: Implementing electronic health record systems streamlines processes, enhances real-time capabilities, and ultimately improves efficiency and effectiveness of monitoring activities conducted throughout jurisdictions involved in managing infectious diseases like Diphtheria [41]; mobile applications facilitate community reporting of suspected cases, improving overall coverage and ensuring timely responses occur whenever necessary.
(5) Strengthening Global Collaboration: Enhanced collaboration among nations facilitates sharing information regarding best practices management outbreaks, ensures uniformity standards are upheld globally, ultimately benefiting everyone involved in combating threats posed by infectious agents, effectively protecting vulnerable individuals and communities worldwide [42].
5. LIMITATIONS
This narrative review is subject to several limitations that warrant consideration. First, variability in reporting standards across countries, stemming from differences in case definitions and data collection practices, may compromise the comparability of diphtheria surveillance data across regions. Second, underreporting remains a significant challenge, particularly in low-resource settings where surveillance systems are often inadequate and access to healthcare services is limited. Third, the availability of published literature on diphtheria surveillance is constrained in certain regions, potentially limiting the comprehensiveness of this review. Finally, although the review encompasses a broad temporal scope (2000–2023), emerging trends post-2020 may not be fully captured due to the cutoff date for available literature, which could affect the representation of recent developments in diphtheria epidemiology and control.
CONCLUSION
This narrative review underscores the ongoing challenge of diphtheria in regions with low vaccination coverage and surveillance gaps. Strengthening public health interventions, addressing vaccine hesitancy, and improving healthcare infrastructure are critical for global diphtheria control. By adopting best practices from successful regions, countries can better protect populations from this preventable disease.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contributions to this paper as follows: the study conception and design were conducted by ary and rr; conceptualization was carried out by aaa; methodology was developed by ea; data collection was performed by jmk; analysis and interpretation of the results were conducted by kh; and the draft manuscript was prepared by sd. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| AIR | = Annual Incidence Rate |
| COVID-19 | = Coronavirus Disease 2019 |
| DTP3 | = Diphtheria, Tetanus, Pertussis (three-dose primary vaccination series) |
| ECDC | = European Centre for Disease Prevention and Control |
| GIS | = Geographic Information System |
| JRF | = Joint Reporting Form (WHO/UNICEF) |
| PAHO | = Pan American Health Organization |
| UNICEF | = United Nations International Children’s Emergency Fund |
| WHO | = World Health Organization |
ACKNOWLEDGEMENTS
Declared none.


