All published articles of this journal are available on ScienceDirect.
Mental Health Impacts and Air Pollution in Pakistan: A Small-scale Cross-sectional Study of Awareness, Coping Strategies, and Mitigation Gaps
Abstract
Introduction
Pakistan, with its deteriorating air quality, is ranked as the third most polluted country globally. It has a PM2.5 concentration of 14.7 times the WHO annual PM2.5 guideline value. It threatens both the physical and mental well-being of individuals. This study evaluates the perceived psychological impacts of air pollution on Pakistani residents, such as changes in mood, anxiety, depression, sleep quality, fatigue, as well as coping mechanisms, and public awareness concerning air pollution.
Methods
A cross-sectional survey was conducted among 160 respondents (through random sampling) from urban, suburban, and rural areas of Pakistan. The survey adapted elements from validated tools, including PHQ-4 and PHQ-9. Statistical methods, i.e., the chi-square test and Spearman’s correlation, were used to assess relationships among demographics, mental health, and pollution exposure.
Results
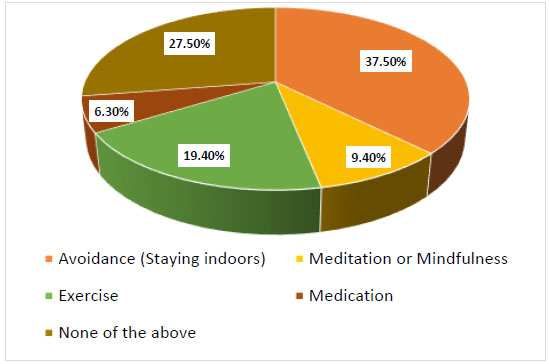
A considerable portion of those surveyed experienced air pollution regularly, and 70% reported worsening of air quality. Mental health impacts include anxiety, sadness, behavioral changes, fatigue, and sleep disturbances (p < 0.001) among 15–24-year-old females, undergraduates, and urban residents. Moreover, moderate positive associations were found between restlessness and irritability (ρ = 0.44, p = 0.001) and between perceived fatigue and mood changes (ρ = 0.46, p < 0.001). Although 83% of participants regarded vehicle emissions as a major source of pollution, only 11.9% engaged in protective behavioral routines, such as wearing masks or using air purifiers. The most frequent coping strategy was avoidance (37.5%), followed by exercising (19.4%).
Discussion
These findings show that polluted air in Pakistan significantly affects mental health, particularly among young urban females. The study highlights the awareness, health concerns, pollution sources, and self-coping strategies of the respondents.
Conclusion
The outcomes of this study suggest a crucial requirement to conduct a study with a broader sample size to assess the generalized health consequences of air pollution concurrently.
1. INTRODUCTION
Air pollution is a widespread environmental risk factor that poses a serious threat to global human health. It is a complicated mixture of particulate matters (PM2.5, and PM10), gases including nitrogen dioxide (NO2), sulfur dioxide (SO2), ozone (O3), carbon monoxide (CO), and a number of volatile organic compounds (VOCs), which mainly come from industrial emissions, vehicle exhaust, biomass combustion, and other human activities [1, 2]. Air pollution worldwide alone causes millions of deaths annually, which are mainly due to respiratory and cardiovascular disease. In addition to these established physical health outcomes, however, there is increasing evidence that air pollution also negatively influences mental health, causing a variety of psychiatric conditions and cognitive impairment [3, 4].
Long-term exposure to air pollution has been associated with a greater risk of depression, anxiety, bipolar disorder, psychosis, and even suicide [5-7]. According to previous epidemiological studies, air contamination raises the risk of dementia, Alzheimer's disease, and cerebral decline in the elderly population [8-11]. The most vulnerable individuals are children and young people because of their immature nervous system and increased liability per body weight, which can lead to sustained neuro-developmental and behavioral effects [4]. Neuroimaging and epidemiological research indicate that air pollution causes neuroinflammation and oxidative stress that impact brain areas responsible for emotion regulation, such as the hippocampus, amygdala, and prefrontal cortex [12, 13]. Such biological pathways yield a likely mechanism to connect exposure to pollutants with heightened internalizing symptoms, such as anxiety and depression [12].
Moreover, new research shows that air pollution adversely affects sleep patterns, contributing to poor sleep quality, insomnia, and sleep fragmentation. Pollutants, such as fine particulate matter (PM2.5) and nitrogen dioxide (NO2), can irritate the respiratory system, leading to sleep-disordered breathing and disrupted restorative sleep stages, which in turn cause daytime fatigue and cognitive impairments [14]. Chronic exposure to polluted air has also been associated with feelings of altered mood, irritability, anger, restlessness, and chronic sadness, many of which are symptoms that precede or exist with anxiety and depressive disorders. These impacts are hypothesized to stem from neuroinflammation, oxidative stress, or changes in stress hormones, which damage brain regions involved in emotional regulation [15]. In addition, the neurobehavioral outcomes highlighted above emphasize a more comprehensive psychological burden of air pollution beyond traditional psychiatric diagnoses.
International organizations, such as the World Health Organization (WHO), establish limits for safe concentrations of typical air pollutants, but many city dwellers remain exposed far above these thresholds, further amplifying health risks [1]. The United States Environmental Protection Agency (EPA) also places a high priority on integrating scientific evaluations to inform policy makers and promote public health [16]. Understanding the whole extent of air pollution health-related impacts, including its behavioral and psychological aspects, is necessary for comprehensive public health plans.
This study aims to investigate the relation between air pollution exposure with anxiety, depression, and behavioural changes among residents in Pakistan, a country facing significant air quality challenges. A cross-sectional online survey and strong statistical methods were utilized in this study to highlight the psychological burden of air pollution. By revealing these hidden effects, the study not only deepens the discussion on environmental health but also opens new directions for public health strategies that are more inclusive and responsive. It is important to address this gap in knowledge in order to develop interventions that not only mitigate the effects of pollution on the body but also on the psychological health of the affected people.
2. METHODOLOGY
2.1. Study Design and Study Sample
This research study is a cross-sectional, online survey investigating the association between air pollution exposure and the prevalence of anxiety, depression, and behavioural changes among residents from diverse regions across Pakistan. The survey was distributed online for anonymous collection of self-reported data on demographics, perceptions of air pollution, mental health symptoms, and coping strategies. It employs random sampling, ensuring that each participant has an equal chance to be included.
2.2. Eligibility and Ineligibility Criteria
The eligible participants for inclusion were (a) individuals aged 15 years and above, (b) residing in urban, suburban, or rural areas, (c) who could understand and respond to the survey in English language and (d) who provided their informed consent to participate in the study. This study excluded responses from individuals under 15, incomplete or duplicate entries, and those who did not provide consent, and was omitted from the final analysis.
2.3. Recruitment and Informed Consent
Participants for this cross-sectional study were recruited primarily through online platforms, including social media, university mailing lists, and community groups, to ensure a diverse sample from various urban and rural areas of Pakistan. The survey link was shared with a brief introduction that mentions the purpose of the study, eligibility criteria, and the voluntary nature of participation. Before accessing the survey questions, all potential participants were presented with an informed consent statement that explained the objectives of the research, the types of questions they would be asked (covering demographics, experiences with air pollution, and mental health symptoms), the confidentiality of their responses, and their right to withdraw at any time without penalty. Only those who provided explicit consent were allowed to proceed to the main survey, in compliance with ethical research standards.
2.4. Study Tool Validation
The questionnaire included demographic information; section one, comprising age, gender, residence, and education level, as well as air pollution awareness and exposure; section two, in which questions were asked to assess the frequency of noticing air pollution, their perception of air quality, use of protective measures, and the concern of respondents about health impacts. Health concern is defined as the perceived level of worry reported by the participants about the effects of air contamination on their overall health. For this specific question, responses were measured on a 5-point Likert scale (Not concerned at all – Extremely concerned), highlighting a self-perceived concern rather than a clinical evaluation. Section three of mental health and behavioral changes has the questions of self-reported symptoms of anxiety, sadness, irritability, fatigue, sleep changes, and behavioral adaptations by individuals. Additionally, in Section four, participants were asked about their healthcare-seeking behaviors and coping mechanisms related to mental health symptoms in the context of air pollution. The survey questions in section three were adapted from questions of mental health assessment tools, such as the Patient Health Questionnaire-9 (PHQ-9) and Patient Health Questionnaire-4 (PHQ-4), which screen for depression and anxiety, respectively [17, 18]. From these questionnaires, the adapted mental health indicators are the items that cover anxiety/restlessness, mood disturbances, fatigue/exhaustion, sleep changes, irritability/anger, and sadness/depression are added to the corresponding section. Instead of applying clinical scoring cut-offs, responses of these variables were collected on a 5-point Likert scale (e.g., Never-Always, not at all- Significantly and Not at all-Very severe) to reflect participants’ self-perceived experiences and concerns rather than diagnostic evaluation. Refer to the Supplementary Material for the full survey questionnaire. The adaptation is specifically concentrated on mental health symptoms, such as anxiety, restlessness, sadness, fatigue, and sleep disturbance, while considering them in relation to perceived exposure to air pollution, ensuring that the items reflect environmental health concerns rather than a clinical or diagnostic frame. By adapting the tool in this manner, the mental health symptoms of concern and the environmental stressor examined improved the construct validity of the tool. To further ensure the validity and reliability of the survey instrument, a panel of experts reviewed the questionnaire for clarity, relevance, and cultural appropriateness. A pilot test was conducted with a small sample from the target population, and feedback was used to refine the wording and structure. Internal consistency of the mental health items was subsequently assessed using Cronbach’s alpha during data analysis, confirming the reliability of the composite scales.
2.5. Statistical Analysis
The data analysis was carried out using the Statistical Package for the Social Sciences (SPSS) version 22. Descriptive statistics (frequencies and percentages) were calculated for categorical variables (age group, gender, residence, and education level) and for responses related to air pollution exposure, showing the prevalence and patterns of exposure among respondents. The data were stratified according to age, gender, area of residence, and education level to examine demographic variations. In view of this, mental health outcomes (anxiety, mood disturbances, fatigue, sleep changes, irritability, and depressive feelings) were assessed in relation to two dependent variables: frequency of noticing air pollution and concern about its health impact. Crosstabulations were performed, and chi-square tests were used to assess group differences. A series of chi-square tests was used to assess associations between air pollution exposure and perceived causes of air pollution with mental health outcomes. Spearman’s correlation was applied to assess the strong, moderate, or low relationships between ordinal variables like anxiety/restlessness, sadness/depression, sleep changes, mood/behavioral changes, and irritability/anger to identify potential mental health symptoms. A p-value < 0.05 was considered statistically significant.
3. RESULTS
This cross-sectional study used a sample of 160 respondents, consisting of 35 (21.9%) males and 125 (78.1%) females. The participants were categorized into five age groups, and the majority were between the ages of 15–24 years (75.6%), followed by 25–34 years (13.1%), 35–44 years (5.6%), 45–54 years (3.1%), and 55 years or older (2.5%). To assess air pollution awareness among respondents, demographic information was further categorized by population density and level of education. As per the location of the survey participants, the majority resided in urban areas (89.4%), with fewer participants from rural areas (6.3%) and suburban areas (4.4%). Regarding educational background, most participants held an undergraduate degree (n = 103, 64.4%), followed by high school graduates (n = 27, 16.9%), postgraduate degree holders (n = 21, 13.1%), and those with less than high school education (n = 5, 3.1%), and other (n = 4, 2.5%) (Table 1).
Figure (1) shows that participants were asked whether they noticed air pollution (smog, dust, or haze) in their area on a 5-point Likert scale ranging from 1 (Never) to 5 (Always). Most respondents favored frequently noticed air pollution (35.6%) or always (30.0%). Only 2.5% of participants declared that they never noticed air pollution. The mean response was 3.82(1.04), suggesting that, on average, participants noticed air pollution between “occasionally” and “frequently,” with a greater inclination towards “frequently.”
Figure (2) shows that the majority of people (70%) perceived a worsening of air quality over the past year, while 19.4% were not sure and 10.6% reported no worsening of air quality in their area. The mean response is 1.49, indicating that most participants perceived a decline in air quality. However, this awareness didn’t consistently translate into protective behavior, as shown in Fig. (3). Participants were inquired about the frequency of using a face mask or an air purifier to protect against air pollution on a 5-point Likert scale ranging from 1 (Never) to 5 (Always). A larger proportion of the participants responded Rarely (31.9%), followed by Occasionally (23.8%). Only 11.9% of participants declared “Always” using protective measures such as a face mask or an air purifier. The mean response was 2.78 (SD = 1.24), suggesting that participants, on average, adopted infrequent protective measures. This relatively low average is concerning, suggesting a general lack of consistent protective behavior against air pollution.
| Demographics | Frequency (n = 160) | Percentage (%) | ||
|---|---|---|---|---|
| Age | 15-24 | 121 | 75.6 | |
| 25-34 | 21 | 13.1 | ||
| 35-44 | 9 | 5.6 | ||
| 45-54 | 5 | 3.1 | ||
| > 54 | 4 | 2.5 | ||
| Gender | Male | 35 | 21.9 | |
| Female | 125 | 78.1 | ||
| Area of living | Urban area | 143 | 89.4 | |
| Suburban area | 7 | 4.4 | ||
| Rural area | 10 | 6.3 | ||
| Level of education | Less than high school | 5 | 3.1 | |
| High school graduate | 27 | 16.9 | ||
| Undergraduate degree | 103 | 64.4 | ||
| Postgraduate degree | 21 | 13.1 | ||
| Other | 4 | 2.5 | ||
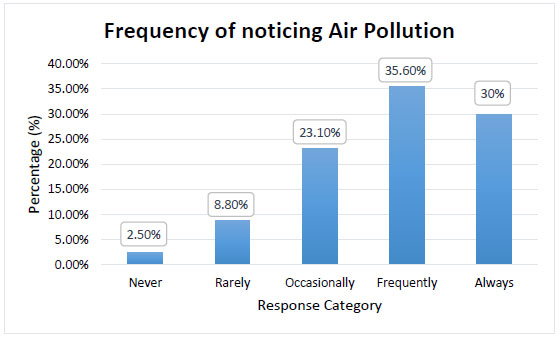
5-point Likert Scale to determine the frequency of noticing air pollution (smog, dust, haze) by respondents.
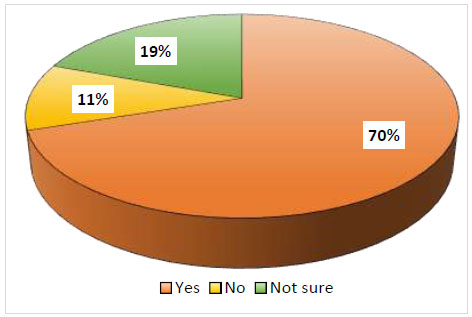
Percentage of participants who experienced the worsening of air quality over the last year.
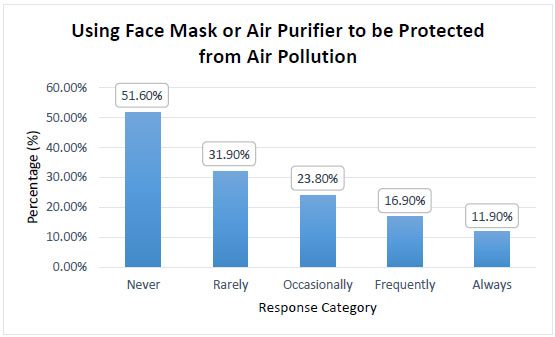
5-point likert scale to check the frequency of using protective gears (face masks or air purifiers) as a prevention from air pollution consequences.
Figure (4) shows that the mental health impact of air pollution emerged as a significant concern. Participants were asked to rate the overall impact of air pollution on their mental health, compared to other stress factors (like work, personal life, etc.) on a Likert scale ranging from 1 (Minimal impact) to 5 (I don’t know). The majority of respondents selected significant impact (34.4%) or moderate impact (32.5%) of air pollution. Only 8.1% of participants reported “I don’t know”, indicating their uncertainty about the impact of air pollution on their psychological health. The mean response was 2.66 (SD = 1.10), suggesting that, on average, participants perceived the impact of air pollution as moderate to significant, with a slight tendency toward the moderate end. The relatively high proportion of participants reporting moderate to significant effects shows a concerning trend regarding the psychological burden of air pollution.
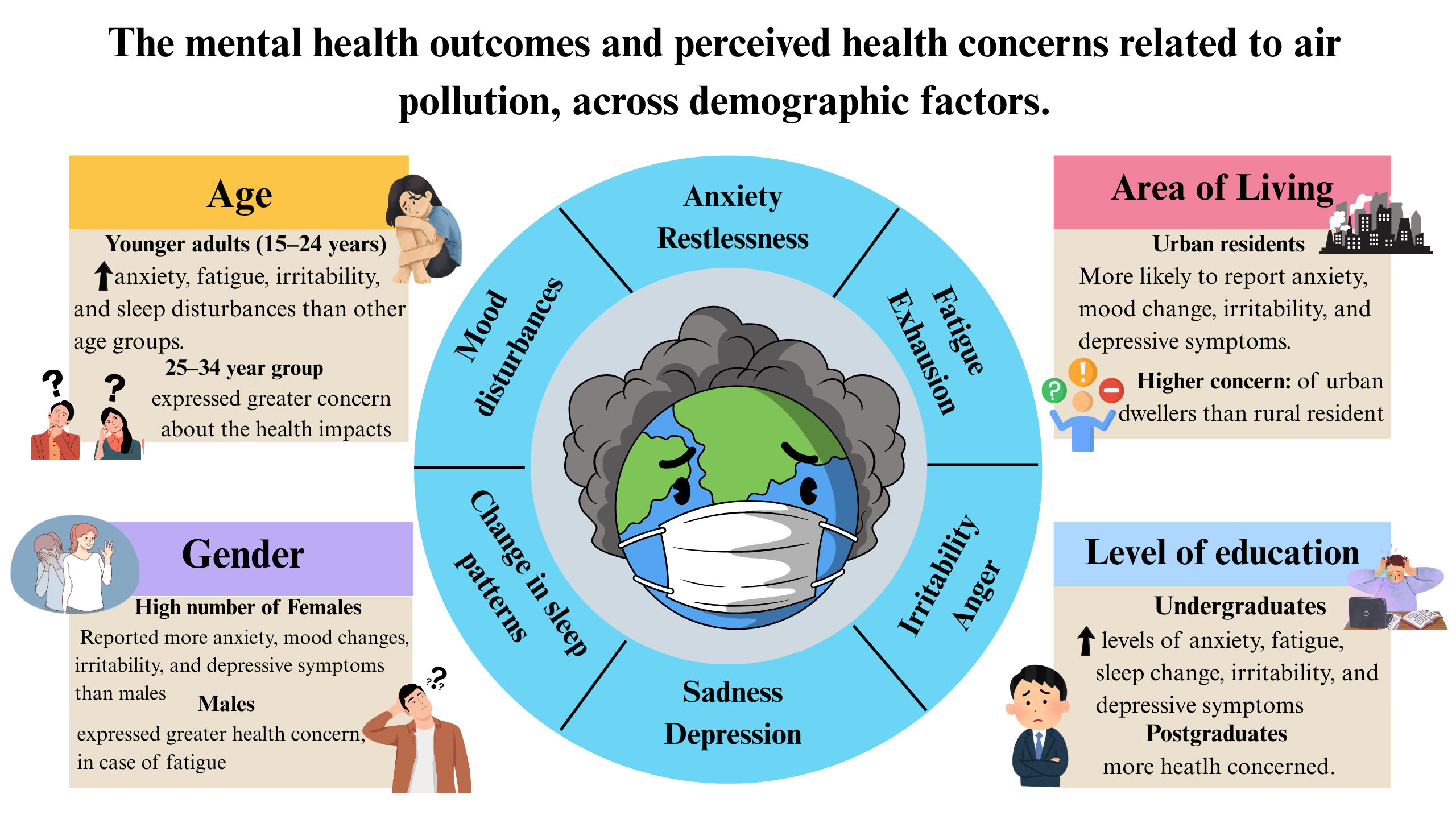
Results pertaining to the analysis of mental health outcomes show significant demographic variations in terms of age, gender, area, and level of education of the sample population in both the frequency of experiencing poor air quality and the perceived level of concern about air pollution’s health impact. Also, the p-values are presented in Table 2. Strong associations were found between demographic characteristics and mental health outcomes related to air pollution. In terms of the age factor, the younger adults (15–24 years) consistently reported higher levels of anxiety, fatigue, irritability, and sleep disturbances compared with the older groups, while the 25–34-year-old group expressed greater concern about the health impacts. Whereas, in terms of gender, females generally reported heightened anxiety, mood changes, irritability, and depressive symptoms compared to males, although in the case of fatigue, males expressed greater health concerns. According to the area of living, the urban residents were more likely than rural residents to report anxiety, mood disturbances, irritability, and depressive symptoms, and also expressed greater concern about the health consequences of air pollution, particularly regarding fatigue, sleep, and anger. While the educational differences were also notable, undergraduates showed higher levels of anxiety, fatigue concerns, sleep disturbance concerns, irritability, and depressive symptoms, but postgraduates tended to express concern rather than symptoms, particularly regarding mood changes.
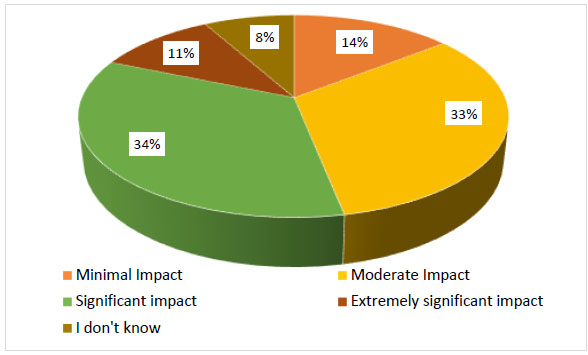
Rating of the overall impact of air pollution on an individual's mental health compared to other stress factors.
| Mental Health Outcomes/Indicators | Demographic Factor | p-value | Key Findings | |
|---|---|---|---|---|
| Frequency of Noticing Air Pollution | Concern about Health | |||
| Feelings of anxiety or restlessness | Age | <0.001 | 0.009 | 15–24 years old most anxious; 25–34 years old most concerned |
| Gender | <0.001 | 0.008 | Females show higher anxiety and concern | |
| Area | <0.001 | 0.09 | Urban residents most affected and are more concerned | |
| Level of education | <0.001 | 0.004 | Undergraduates are more anxious; postgraduates are more concerned | |
| Mood disturbances | Age | 0.01 | 0.14 | Significant mood changes in 15–24 years old, but the concern is not significant |
| Gender | 0.009 | 0.126 | Females show more mood changes; no major differences. | |
| Area | 0.002 | 0.24 | Urban residents report mood changes, but not concern | |
| Level of education |
0.007(UG) 0.005(PG) |
0.016 | Both undergraduates (UG) and postgraduates (PG) show mood change; only postgraduates express concern | |
| Fatigue and exhaustion | Age | 0.023 | 0.001 | 15–24 years old report high fatigue and concern |
| Gender | 0.014 | 0.005 | Fatigue is higher in females, but health concerns are higher in males | |
| Area | 0.01 | 0.002 | Exhaustion/Fatigue is not different by area, but urban residents show greater concern. | |
| Level of education | 0.09 | <0.001 (UG) | Feelings of fatigue not significant by education; undergraduates express most concern. | |
| Change in sleep patterns | Age | 0.008 | 0.001 | 15–24 years old show reduced sleep and health concerns |
| Gender | 0.203 | 0.09 | No significant differences | |
| Area | 0.164 | <0.001 | Sleep changes are not significant, but urban residents report higher concern | |
| Level of education | 0.008 | <0.001 (UG) | High school graduates report disturbed sleep; undergraduates (UG) show more concern | |
| Experiencing irritability or anger | Age | 0.001 | 0.006 | 15–24 years old most irritable and concerned |
| Gender | 0.001 | 0.09 | Females report more irritability and concern | |
| Area | <0.001 | 0.007 | Urban residents show higher anger and concern | |
| Level of education | 0.001 | 0.001 (UG) | Undergraduates are more irritable and concerned compared to postgraduates/others | |
| Feelings of sadness or depression | Age | <0.001 | 0.15 | 15–24 years old more sad/depressed, but not more concerned. |
| Gender | <0.001 | 0.35 | Females are more depressed, but not more concerned | |
| Area | <0.001 | 0.31 | Urban residents are more depressed, but not more concerned | |
| Level of education | <0.001 | 0.12 | Undergraduates are more depressed, but not more concerned | |
The main findings of the mental health outcomes, according to stratified demographic factors (age, gender, area, and level of education).
The key findings of the stratified demographic analysis in Table 2 are depicted in Fig. (5).
Further evaluation of the survey variables was conducted by conducting a series of chi-square tests of independence. Table 3. shows that the individuals who frequently notice contaminated air in their area were more likely to report several indicators of psychological impact. Participants recognize a significant change in their mood or behavior, due to frequent awareness of air pollution (p < .001). A marginally significant association (p = .028) was also found between noticing air pollution and feelings of fatigue or exhaustion. Similarly, most respondents feel sad or depressed (p < .001), as well as report the worsening of their anxiety or depressive symptoms (p < .001) after exposure to smog, dust, and haze. This relationship suggests that increased perceptual awareness of poor air quality is linked to negative emotional states and mental health distress.
Table 4 presents the relationship between the concern of respondents about the health impacts of air pollution and related perceptual and behavioral factors. A significant association was found (p = .013) between experiencing worsening air quality in one's area and concern about the health impacts of poor quality of air quality. Additionally, a significant relationship was identified between concern about air pollution's health effects and the use of protective behaviors, such as air purifiers or wearing face masks (p = .004). These results suggest that individuals who perceive air quality as deteriorating are more likely to exhibit concern about health consequences and to take self-protective actions.
| Mental Health Indicators/Outcomes | Frequency of Noticing Air Pollution | |
|---|---|---|
| χ2 (df) | p-value | |
| Change in mood or behavior | 29.21 (4) | 0.001 |
| Fatigue or exhaustion | 10.85 (4) | 0.028 |
| Sadness or depression | 38.10 (8) | 0.001 |
| Worsening of anxiety or depressive symptoms | 25.73 (8) | 0.001 |
In Table 5, the analysis found the influence of health-related concerns on mental health outcomes. A significant portion of participants who were concern about air pollution’s health effects exhibited perceived changes in mood or behavior (p = .045). An even stronger association was observed between health concern and reported changes in sleep patterns (p < .001). These strong findings suggest that individuals experience both emotional disturbances and disrupted physiological patterns, such as sleep concerns due to air contamination in the surrounding atmosphere. As depicted in Table 6, the Pearson chi-square value (p = .055) showed a significant relationship between the feelings of sadness or depression and the likelihood of consulting a healthcare professional. The individuals experiencing emotional distress due to air pollution may be more inclined to seek therapeutic support. However, in reality, only a small number of participants reported consulting a doctor, highlighting that while they are aware of the depressive effects of air pollution, they need to begin engaging with mental health services. Table 7 examines the associations between worsening psychological symptoms of anxiety or depression and both environmental and health-related perceptions. Concern about the health effects of air contamination (p = .050) and how individuals rated the overall health impacts of air pollution (p < .001) were significantly associated with the belief that air pollution worsens anxiety or depressive symptoms, which negatively affects their mental health. These concerns and belief systems surrounding air pollution contribute to the internalization of its psychological burden, consistent with cognitive-affective models of mental health distress.
| Perceived Health Concern (Variable) | χ2 (df) | p-value |
|---|---|---|
| Worsening air quality in the area | 19.41 (8) | 0.013 |
| Use of face masks | 35.34 (16) | 0.004 |
| Psychological Outcome | χ2 (df) | p-value |
|---|---|---|
| Mood or behavior change | 15.84 (8) | 0.045 |
| Changes in sleep patterns | 67.99 (16) | 0.001 |
| Variable | Have you consulted Health care professional (HCP) for mental health symptoms in the past year? | χ2 (df) | Pearson chi-square | |
|---|---|---|---|---|
| In the past month, have you experienced feelings of sadness or depression? | Yes | No | - | - |
| 20 | 140 | 5.81 (2) | 0.055 | |
For the assessment of the strength and direction of a relationship between two variables, Spearman’s rank-order correlation was conducted. Table 8 shows the relationship between feelings of anxiety or restlessness and experiencing anger and irritability due to air pollution, along with believing that air pollution worsens anxiety or depression symptoms. There is a moderate, positive correlation, which is statistically significant for both, i.e., (ρ (160) = 0.44, p = 0.001) and (ρ (160) = 0.49, p < 0.001), respectively. This correlation suggests that participants who felt anxiety or restlessness are more prone to higher levels of irritability or anger, and air pollution has made their anxiety and low mood worse.
Table 9 shows the relationship between the contribution of air pollution to any changes in mood or behavior and feeling fatigued or exhausted due to it. There is a moderate, positive correlation that is statistically significant (ρ (160) = 0.46, p < 0.001). When participants noticed their mood changes, many connected the poor air quality with rising fatigue and a heavy, worn-out feeling throughout the day.
| Belief of Mental Health Symptoms (Anxiety or Depression) Worsening | χ2 (df) | p-value |
|---|---|---|
| Health impacts concern | 9.46 (4) | 0.050 |
| Health impacts rating | 83.39 (16) | 0.001 |
| In the past month, have you experienced feelings of anxiety or restlessness? | ||
|---|---|---|
| - | Correlation Coefficient | p-value |
| Have you experienced more irritability or anger due to air pollution? | 0.44 | 0.001 |
| Do you believe that air pollution worsens your anxiety or depression symptoms? | 0.49 | 0.001 |
Table 10 shows the relationship between changes in sleep patterns and feeling fatigued or exhausted due to air pollution. There was a moderate, positive correlation that was statistically significant (ρ (160) = 0.40, p < 0.001). Participants linked poor air quality to both changes in sleep patterns and feelings of fatigue throughout the day.
Figure (6) illustrates coping strategies as a preventive measure for psychological well-being among people from air pollution. The most frequently reported coping strategy for managing mental health symptoms related to air pollution was avoidance, such as staying indoors, endorsed by 37.5% of participants. 19.4% reported exercise, followed by meditation and mindfulness being reported by 9.4%. Only 6.3% of participants reported using medication, while 27.5% indicated that they did not use any of the listed coping strategies. The mean response is 2.77, suggesting a modest inclination toward behavioral coping strategies, such as avoidance and exercise, rather than clinical or mindfulness-based approaches.
| Do you believe that air pollution has contributed to any changes in your mood or behavior? | ||
|---|---|---|
| - | Correlation Coefficient | p-value |
| How often do you feel fatigued or exhausted due to air pollution in your area? | 0.46 | 0.001 |
Table 11presents a multiple-response cross-tabulation (frequencies and percentages) of recognized causes of air pollution against preferred mitigation measures. The most commonly identified cause was vehicle emissions, selected by 133 (83.12%) respondents. From that sample, 95% selected improved public transportation as a preferred mitigation strategy, while 90% supported stricter government regulations on industries. Similarly, 86.3% chose increasing green spaces, and 87.8% supported public awareness campaigns.
| How often do you feel fatigued or exhausted due to air pollution in your area? | ||
|---|---|---|
| - | Correlation Coefficient | p-value |
| Have you noticed any changes in your sleep patterns due to air pollution? | 0.40 | 0.001 |
Industrial emissions were recognized by 67 (41.9%) respondents as the second main cause of air pollution. Of those, 60% preferred stricter regulations on industries by the Government, 50% picked improved public transportation, and 51.1% supported public awareness campaigns. Construction activities were selected by 87 (54.4%) respondents, with 64.4% opting for stricter regulations, 63% supporting improved transportation, and 66.7% favoring public awareness campaigns. This implies developing policy and making educational interventions to alleviate construction-related pollution. Crop burning, reported by 41 participants, showed a lower trend for each mitigation measure, with the highest at 38.9% for public awareness campaigns. This indicates either limited awareness or less consensus on effective strategies to combat crop-related pollution. A small group of survey participants (n = 9) selected “Others” as the cause of air pollution. These participants mentioned sources such as garbage burning, timber cutting, hotel smoke, dust from damaged roads, and wood burning. All respondents (100%) also selected “Others” as the solution category, suggesting alternative perspectives, including government-led efforts to build proper roads and improve sanitation services (Table 11).
4. DISCUSSION
The current survey-based study assessed the awareness of air pollution and its related mental health symptoms by using self-reported, custom-made questionnaire partly adapted from PHQ-4 and PHQ-9 criteria along with coping strategies among general population in Pakistan, offering crucial insights into how air pollution exposure impacts participant’s quality of life and what strategy they choose to mitigate it [17, 19] Using an online survey, the study involved 160 participants, predominantly 125 females followed by 35 males. Demographically, individuals were primarily students (64.4% pursuing undergraduate degrees), indicating a younger cohort aged 15-24 years, with a larger proportion residing in urban areas.
| Causes of Air Pollution | Preferred Mitigation Strategies for Prevention of Air Pollution-related Mental Health Symptoms | |||||
|---|---|---|---|---|---|---|
| Stricter Government Regulations on Industries | Improved Transport | Increasing Green Spaces | Awareness Campaigns | Others | Total | |
| Industrial Emissions | 60.0% | 50.0% | 44.6% | 51.1% | 0.0% | 67 |
| Vehicle Emissions | 90.0% | 95.0% | 86.3% | 87.8% | 0.0% | 133 |
| Construction Activities | 64.4% | 63.0% | 59.0% | 66.7% | 0.0% | 87 |
| Crop Burning | 33.3% | 29.0% | 27.3% | 38.9% | 0.0% | 41 |
| Others | 4.4% | 5.0% | 5.0% | 5.6% | 100.0% | 9 |
Self-coping strategies adopted by the survey takers to prevent from health effects of air pollution.
According to demographic factors, this study shows that the younger adults were the most anxious, depressed, with low mood and sleep changes, although they show lesser concern than the early-working-aged adults (25-34 years old). However, a stark contrast emerges when compared to previous studies in Bangladesh, Italy, and Brazil, in terms of age categories mentioned that older adults are more prone to mental and respiratory disorders due to air pollution [20-22]. Similarly, in terms of gender, it was found that a greater number of female participants reported anxiety, fatigue, irritability, and behavioral changes than males. But males showed more concern regarding their health due to poor air quality. The same finding was reported in the study of Al-Shidi, H.K., and colleagues [23]. In view of respondents' area of living, urban dwellers recognized elevated anxiety, anger, mood changes, and sadness. Also, they reported concern about health than the rural residents, which aligns with previous evidence [24, 25]. The level of education factor also determines the increased anxiousness, exhaustion, depressive symptoms, and fidgety behavior among undergraduates, but the concern regarding mental health was more in postgraduate students [26]. Participants' awareness of air contamination in their living areas was significant in the present study, as they frequently (35.6%) notice smog, haze, and dust in their everyday routine, though this is less than an online study conducted in Bangladesh, where 90% respondents reported air-polluted environments and associated health problems [20]. A majority (70%) of participants in the survey reported experiencing a worsening of poor air quality over the past year, which is validated by the 2024 report of Pakistan’s Air Quality Index (AQI) with an average of 164, placing it in the red zone and ranking it the third worst country with contaminated air. The PM2.5 concentration is 14.7 times the World Health Organization PM2.5 guideline value. The major urban cities top the list of unhealthy air, including Sialkot (119 AQI), Islamabad (117 AQI), followed by Lahore and Karachi, both at 96 AQI [26].
A significant to moderate impact of air pollution was found on an individual’s mental health symptoms as compared to other stress factors like personal life difficulties, trauma, workload, etc., and this aligns with previously reported data [27, 28]. The matter of fact is that this awareness didn’t consistently translate into protective behavior, as most participants, i.e., Pakistanis, were found to be using a face mask or air purifier “rarely” (31.9%) as protection from impure air, which is concerning and contradictory to the research from China [29]. That study revealed that the behavior of Chinese people was more promising, with 54.5% using all types of masks and 70.6% using anti-PM 2.5 masks to prevent unclean air hazards to their health [29, 30]. This highlights the need for awareness and the development of a habit of taking protective measures among Pakistanis to combat the health effects of polluted air [31].
The current evidence suggests a strong association between frequent detection of air pollution and the emergence of negative emotional states, indicating poor mental health indicators among participants. They recognize marked changes in their mood or behavior, and many reported suffering from sadness and depression, as also recognized by previous research [12, 32]. Similarly, most respondents experienced feelings of fatigue or exhaustion and reported worsening of their anxiety or depressive symptoms. This same significant pattern was mentioned by the CHARLS study [33, 34]. These relationships suggest that increased perceptual awareness of poor air quality is linked to mental health distress [35].
A growing number of studies confirm that, as in this survey, a majority of respondents living in regions with high air pollution complain about irregular sleeping patterns and poor-quality sleep. PM2.5, NO2, and O3 are some of the harmful pollutants that have been known to reduce sleep efficiency and increase sleep latency, along with causing fragmented sleep architecture [36]. In one of the reviews, it has been discussed that air pollution disrupts melatonin regulation and inflammatory pathways, leading to poor sleep health and disruption of circadian rhythms [36, 37]. A cohort study conducted in China revealed that heightened concentrations of PM2.5 and NO2 are associated with some symptoms of insomnia, such as trouble falling asleep and early waking habitually [38]. These subjective findings are bolstered by objective measures from actigraphy-based sleep studies that demonstrate decreases in sleep duration and sleep efficiency with exposure to pollutants [14]. Moreover, it is observed that circadian rhythm is disturbed due to altered melatonin production following pollutant exposure, causing delays in sleep onset and daytime fatigue [39]. These findings collectively strengthen the assertion that air pollution significantly influences sleep quality, a major concern with moderate positive significance (ρ = 0.40, p < 0.001) expressed by respondents in our survey.
It is becoming more apparent how air pollution can contribute to mental health issues, such as anxiety and depression. Research indicates that short-term exposure to air pollutants like SO2, NO2, PM2.5, and PM10 is linked to increased outpatient and emergency department visits for anxiety and depressive episodes [40-42]. These observations demonstrate that the misery caused by polluted air is not restricted to subclinical thresholds, nor is it momentary, but rather long-lasting and severe enough to motivate seeking medical care. Sustained exposure is also critical, especially for older adults, as chronic exposure to pollutants increases the likelihood of developing anxiety and depression [6]. A systematic review provides additional support, noting that most studies reported biological alterations in the brain alongside mental health symptoms, underscoring the validity of considering air pollution as a potential psychiatric risk factor [12]. These findings corroborate the results of the survey, which showed that participants who reported consulting primary healthcare doctors to address emotional distress attributed to poor air quality, reinforcing the notion that the environment is directly shaping mental health care-seeking behaviors, and the chi-square value (p = .055) showed a significant relationship. Rating their health poorly due to air pollution increases the likelihood of experiencing depression, anxiety, and psychological distress (p < .001). This indicates that perceptions of negative air quality impact mental health and self-rated health in particular. It does support the idea that self-rated health acts as a mediator of the relationship between environmental exposure and mental well-being [43].
Monitoring the health of 422 Mexican-American adolescents for two years showed that exposure to air pollutants, such as NO2 and CO, resulted in increased fatigue and emotional distress. These associations were strong for both symptoms occurring on the same day and the next day. Moreover, even when temperature and humidity were included as additional confounding factors, the results still showed a strong effect [44]. This showed the association between air quality and mood-related fatigue as well as energy levels in children and adolescents.
Additionally, this research indicates the coping strategies based on the personal choices of the participants to deal with the mental health implications of air pollution. A substantial portion (37.5%) of respondents choose to stay indoors to avoid the air pollutants from outdoor air, this aligns with the meta-analysis and review that previously mentioned the actions, such as reduced personal exposure to ambient air pollution by staying indoors, reducing outdoor air infiltration to indoors, cleaning indoor air with air filters, and limiting physical exertion outdoors on high air pollution days and near air pollution sources, reducing near-roadway exposure while commuting, utilizing air quality alert systems to plan activities, and wearing facemasks in prescribed circumstances which can be taken at the individual level to lower exposure-related health risks from air pollution [45, 46]. A reasonable number of respondents (19.4%) reported performing exercise regularly to address air pollution health consequences in the survey. This aligns with the comprehensive review, which includes studies of large samples of Korean and Swedish individuals who perform moderate to vigorous exercise >5 times/week, who experienced decreased risk of stroke and cardiovascular disease incidence, even when exposed to high levels of PM2.5 and PM10 [47-49]. Quite a few people in the present investigation, i.e., 9.4% and 6.3%, chose meditation/mindfulness and use of medications, respectively, to prevent the negative health influences of contaminated air. This corresponds to the earlier qualitative analysis done that explains the effect of mindfulness on pro-environmental behavior [50]. Similarly, the specific medicine was not reported by the participants, and the use of air pollution-related mental symptoms-specific drugs is not much explored. Instead, one study reported that nonsteroidal anti-inflammatory drugs (NSAIDs), like aspirin, may lessen the adverse effects of air pollution exposure on lung function [51]. Lastly, subsequent majority (27.5%) of members answered using none of the mentioned coping strategies, suggesting the lack of seeking professional help like therapy, which points out that there might be insufficient mental health care services or a lack of promotion of available services in this situation. With regard to the air pollution-associated mental health symptoms, participants predominantly use behavioral strategies, especially avoidance, as their coping mechanism [45].
The biggest debate in the present world about air pollution is its leading causes and possible mitigation strategies to cope with potential health risks and glitches [52]. The multiple survey responses demonstrated that participants selected vehicle emissions (83.15%), construction activities (54.4%), and industrial emissions (41.9%) as the top three causes of air pollutants, an existence with past studies in Pakistan that referred to the same outcomes [53, 54]. A plethora of prior studies also outlined these principal contributors to air quality deterioration. Research conducted in Iran cited a number of different emission sources, but motor vehicles and industrial processes contribute the major proportion of air pollution in Iran [55]. Geopolitical neighbors of Pakistan in South Asia, like India and Afghanistan, also cited the causes of air pollution. The main contributors to India's particulate air pollution include industrial and vehicular emissions, construction dust and debris, and waste burning etc [56]. Similarly, the primary sources of ambient air pollution in Afghanistan encompass motor vehicles, agricultural burning, and industrial activities [57]. A sparse participant pool chose crop burning (n=47) and other causes (n=9), i.e., damaged roads dust, timber cutting, hotel places smoke as pollutant-generating activities. These observations reinforce earlier scientific literature [58-60].
In response to the noxious air pollutants arising from emission sources, a range of advised mitigation approaches has been developed [61]. According to the collected data, participants shared several intervention strategies to counteract these toxic atmospheric pollutants. 95% of survey takers preferred improved transportation to control vehicle emissions, while 60% of respondents recommended strict government regulations on industrial emissions. These perspectives resonate with previously structured recommendations, including the benefits of effective vehicle management and emission control through regular maintenance [62]. It has been emphasized that policymakers should collaborate closely with regulatory bodies, industries, and local communities to implement environmentally responsible practices more efficiently [63]. The remaining mentioned secondary contributors are crop burning and construction activities, for participants opted for awareness campaigns and increasing green spaces across Pakistan. Initiatives, such as reducing air pollution from urban residential buildings and enhancing green spaces, have also been recognized for their role in filtering airborne particles [64, 65]. Increased plantation, in particular, plays a significant role in reducing city air pollution [66]. Besides that, public awareness campaigns regarding the health threats posed by air pollution present both challenges and opportunities, underscoring the need for comprehensive communication strategies to enhance environmental health literacy [67]. In addition to resisting the air contamination caused by issues such as damaged roads, dust, smoke from hotels, and the burning of garbage, it is essential to implement waste classification to enhance air quality in municipal solid waste management [68]. Implementing effective sanitation to prevent disease transmission, safeguards the air-polluted environment, enhances the quality of life, and promotes the overall well-being of the community [69].
4.1. Significance of the Study
This extensive study is among the first in Pakistan to assess how poor air quality contributes to mental health ramifications, including the risks of depression and anxiety, and direct impacts on mood change, restlessness, and disturbed sleep patterns, highlighting a neglected public health concern [12, 70]. This survey investigates the significant detrimental impact of air pollution, particularly smog dust and haze, on the psychological distress of residents in urban Pakistan [70]. With Pakistan ranked as the third most polluted country globally in 2024 and cities like Lahore, Karachi, Sialkot, and Islamabad consistently exceeding safe AQI levels, the timing of this investigation is both urgent and relevant [71]. Research highlights various ways in which frequent exposure to pollutants contributes to mental health consequences manifesting as sadness, anxiety, low mood, fatigue, and sleep disturbances that align with global data showing that PM2.5 and NO2 exposure contribute to psychiatric risks and biological changes in the brain [7, 72, 73].
Despite awareness of worsening air quality, most participants failed to adopt protective behaviors, revealing a critical awareness-action gap in Pakistan [74]. However, individuals noticed the key generators of air pollutants and pinpointed effective interventions, i.e., better public transport, stricter industrial regulation, and increased plantation, providing community-based observations for climate-resistant urban planning and public health programs [75, 76]. Overall, this analysis positions air pollution not just as an environmental crisis, but a mental health emergency in Pakistan, underscoring the urgent need for longitudinal studies to develop the inter-sectoral public health action [77].
4.2. Study Limitations
While this research provides valuable perspectives about adverse mental health effects due to air pollution, several limitations must be considered. The sample demographic composition is primarily young females who reside in urban areas, which limits generalizability to broader populations, including rural communities, older adults, and occupationally exposed groups that experience differential air particulate matter and harmful gases. Additionally, the sample size is relatively small because of the time and resource constraints of a student-led project, which further limits the generalizability of the findings. The survey data is pragmatic and expandable, but it may lead to over- or under-reporting of symptoms due to recall error, subjective perception, or mental health stigma, in a culturally conservative society. In order to reduce bias and improve accuracy, it is important that future research should complement self-reports with clinical assessments, structured interviews, or mixed-method approaches. Ultimately, the temporal sequence between air pollution exposure and mental health outcomes is not fully addressed in this study, limiting the ability to develop the directionality of these associations and precluding conclusions. Future longitudinal or panel-based studies are essential to explore cumulative or lagged effects of air quality on psychological well-being tailored to specific individuals.
CONCLUSION
This study serves as a preliminary investigation into the intricate and strong relationship between air quality decline and mental health. It concludes that prolonged exposure and perceptual awareness of smog, haze, and dust were associated with elevated symptoms of depression, irritability, anxiety, fatigue, and sleep disturbances, which contribute to a decreased quality of life and overall well-being in the Pakistani population. Despite this psychological burden, the protective behavior of the participants, i.e., the use of masks or air purification, was inconsistently practiced, highlighting a critical public health gap. In order to understand this critical issue, future longitudinal studies are required to establish causality and guide appropriate interventions. The findings of this study can be taken as baseline evidence highlighting an emerging public health concern rather than prescription policy recommendations.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: M.A.: Study concept and design; S.S.H.R.: Data collection; M.B., A.I.U.: Data analysis and interpretation; M.B., A.I.U., S.S.H.R.: Writing- Original draft preparation; R.A.: Writing-reviewing and editing; S.S.: Validation; R.N.: Methodology; S.E., U.K.: Investigation. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| PM2.5 | = Particulate matter 2.5 |
| PM10 | = Particulate matter 10 |
| NO2 | = Nitrogen dioxide |
| O3 | = Ozone |
| SO2 | = Sulphur dioxide |
| UG | = Undergraduates |
| PG | = Postgraduates |
| AQI | = Air Quality Index |
| PHQ-4 | = Patient Health Questionnaire-4 |
| PHQ-9 | = Patient Health Questionnaire-9 |
ETHICAL STATEMENT
Formal ethical approval was not required for this study according to the policies of the Faculty of Pharmacy, Salim Habib University, as the research was survey-based and involved anonymized data collection.
AVAILABILITY OF DATA AND MATERIALS
The data sets used and/or analysed during this study are available from the corresponding author [M.A] upon request.
ACKNOWLEDGEMENTS
Declared none.


