All published articles of this journal are available on ScienceDirect.
Portuguese Health System, an Overview and a SWOT Review
Abstract
Purpose:
The aim of this work is to describe the Portuguese health system and to provide a SWOT approach of its present situation. In this way, a clear and simplified picture of the health system can be offered and some strategies are proposed to improve the functioning of the health system.
Design/Methodology/Approach:
The methodology used is descriptive, based on a literature review structured by SWOT tools and the WHO definition of a health system, and it is applied to Portugal.
Findings:
The strengths and weaknesses in the Portuguese health system are several and varied, and there are some threats and opportunities, too. The improvement of the Portuguese health system and Portuguese health population will have to consider the facts observed here.
Originality/Value:
This work contributes to the better understanding about the current situation of the Portuguese health system.
1. INTRODUCTION
The Portuguese health system (PHS) ensures compliance with the Constitution of the Portuguese Republic concerning the right to health. The goal of the health system is to protect the health of the population. It promotes equality of access to health care for all citizens, irrespective of economic condition and geographic location, ensures equity in the distribution of resources and use of health care services.
The main essence of the PHS has not changed in the last 30 years. It provides universal public coverage to all residents; it is regulated by the Ministry of Health, and it is described as a mixed type of health system. The main trends of changes in PHS for the last 30 years can be stated as follows [1]: 1985-1995: expansion of health care to the non-profit and private sector, in both financing and delivery; the slight decentralization of the national health system; increase in the number of public hospitals; 1995-2000: reinforcement of the basics of the health system by enhancing public responsibilities; reorganizing hospital and health center unit networks; introduction of health care services contracting; 2000-2005: experiences with private management of public health care units; the setting of a public health strategy and the creation of the health regulatory authority; 2005-2013: expansion and realignment of public health policy; a new view of the role of the public, private and social sectors in the health care system; bottom-up organizational changes in primary care; introduction of good governance practices in health.
The national health system is financed by taxes and coexists with i) public insurance schemes (called subsystems), based on employee/employer contributions, and ii) the private voluntary health insurance [2]. The subsystems cover around 20-25% of the population and private health insurance is purchased by 20% of the population [3]. Out-of-pocket expenditures represented 27.3% of total health spending in 2013 [4], and the total hospital debt was about €1.314 billion in 2014 [5].
2. THE PHS CLASSIFICATION FOR THE LAST 30 YEARS
Researchers and policy makers have suggested several different health systems typologies over the last 30 years [6]. A brief overview and description for Portugal is presented in Table 1.
The classification of the Portuguese health system in the last 30 years.
| Year | Author | Classification |
|---|---|---|
| 1987 | OECD1 | Beveridge model |
| 1997 | WHO2 | Mixed system in transition from insurance-financed to tax-financed system |
| 1998 | European Parliament3 | Public taxation and direct payments |
| 2000 | Moran4 | Insecure command and control state |
| 2003 | OECD5 | Public integrated model |
| 2007 | Busse et al.6 | Tax financed system with high private share |
| 2009 | Thompson et al.7 | Tax financed model |
| 2009 | Wendt8 | Low budget restricted access |
| 2010 | Reibling9 | Mixed regulation states |
| 2010 | Jourmard et al.10 | Mostly public provision and public regulation, with gate-keeping and limited choice of providers, under strict budget constraint (special case of Portugal) |
| 2012 | EU11 | Centralized but structured at the territorial level |
The historical profile of the Portuguese Health System shows that it has been classified as a health system financed by taxes, public provision and publicly controlled, as shown in table 1. In 1997, the PHS was described to shift from an insurance-financed to a tax-financed system. A significant share of out-of-pocket payments in the funding of the health system has been identified in 1998, 2007 and 2009 typologies.
In 2000, the Moran typology suggests that access to health services is based on citizenship, and provision and governance of resources are mainly public; however there is a strong private sector which is regulated by the government [2]. For instance, in 2013 there were 226 hospitals of which 107 were private, and of about 35500 hospital beds 10500 were in private hospitals; additionally, around 30% of all medical consultations take place in private hospitals [7].
Other features of the PHS are the low level of total health expenditure per capita reported by Wendt [8], the strong control of access to physicians, because of either gate-keeping or cost-sharing [9], and a relatively strict budget constraint for public health units [10].
Finally, it is worth mentioning that the PHS is centralized so that most responsibilities are controlled by the central government. However, the implementation of health policy is under regional level bodies who represent the central administration, albeit to a limited extent [2, 11].
Despite some changes that have been made, the nature of the PHS has not greatly changed in the last 30 years. The general description provided by the different typologies for this period reflects the overall features of the PHS, even today.
3. AIMS AND METHOD
The aim of this article is to present the PHS from a particular perspective. It is analyzed using a literature review based on the tools offered by SWOT analysis and the WHO definition of a health system. We also propose (possible) strategies and measures to improve it. To achieve these goals, the method used is descriptive and non-quantitative.
A traditional SWOT analysis has four steps [12], to achieve one objective: data collection; data organization in SWOT categories; development of a SWOT matrix for each member of an expert panel, and finally use of the results in a decision-making process. This work does not follow the traditional SWOT analysis. In the first place, step three is not undertaken and so no expert panel is consulted and also there is no decision making, as in step four. However, we have used the SWOT tools for a multi-objective analysis. This work may be described as a literature review structured by the World Health Organization (WHO) definition of a health system and the SWOT aspects of analysis applied to the Portuguese health system. For these reasons, the method used is called a SWOT review rather than a SWOT analysis. This work does not intend to be a complete analysis of the PHS, as it may be done is a larger space such as a book, but a particular and probably simplified view constructed by well know instruments and which has not be done before.
This article continues by describing the PHS using SWOT instruments. First, the ultimate goals of the PHS are set out. The strengths and weaknesses within the functions and intermediate goals of the PHS are then described, followed by an explanation of the opportunities and threats to the PHS. Finally, some possible strategies are suggested based on the perceived strengths and weaknesses.
4. SWOT REVIEW
A usual approach to structured planning is the SWOT analysis. SWOT stands for strengths, weaknesses, opportunities and threats. It makes it possible to identify and set objectives, to single out the positives and negatives of an organization or a system, to analyze a situation and develop suitable strategies and to assess capabilities and competences. While the opportunities and threats are external developments and influence to the improvement of the outcomes of a health system, the strengths and weaknesses are internal capabilities or features and they can be compared with other health systems. This type of analysis applied to health systems makes it possible to develop awareness of the health system’s situation and so it may help policy makers to in their strategic planning and on-the-ground decision making. Although a SWOT analysis is not widely used to analyze health systems, examples can be found in other initiatives and works [13-16]. Our work does not follow a classic SWOT analysis, instead it uses SWOT tools to provide a structured reflection and review of the Portuguese health system.
A SWOT approach applied to health systems requires explaining the concept of health system. The WHO has defined a health system as all the activities whose primary purpose is to promote, restore and maintain health. Hence, a health system has functions, intermediate and final goals [17]. The four main functions of a health system are: i) service provision, ii) generation of resources, iii) stewardship, and iv) financing [17].
The goals of any health system include final and intermediate goals. In 2000, the WHO proposed a framework that specified the final goals of a health system [17]: responsiveness to people’s expectations, social and financial risk, and fair protection and improved health. These are the goals to be considered for the SWOT approach used in this work.
The intermediate goals, which correspond to the components of the right to health [43], and could be seen as operational goals, are: improving access, improving coverage, delivering high quality and safe health services, promoting healthy behavior and improving efficiency [17, 18]. Strategies and policy measures are both designed according to these intermediate goals because operating within them and achieving them improves the likelihood of achieving the final goals.
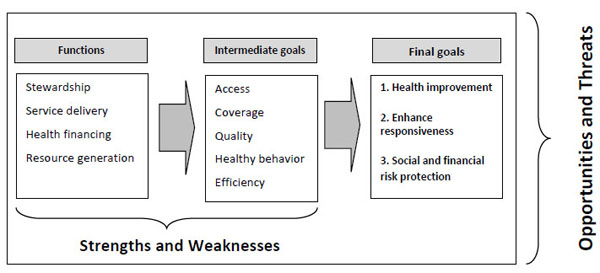
Functions and goals of a health system related with SWOT parameters.
Combining the SWOT parameters with the functions and intermediate goals of a health system, one gets the framework of analysis presented here. The strengths and weaknesses are analyzed within the functions and intermediate goals of the health system, while the opportunities and threats are the external elements which influence the functions and the goals, as represented in Fig. (1).
This analysis points out the most relevant strengths and weaknesses of, and opportunities and threats to, the Portuguese health system, thereby providing readers with an easy list of its SWOT features. Moreover, several national references are used because they analyze and publish topics about the Portuguese situation that are not covered by international works or articles.
4.1. PHS Final Goals
The PHS was created in 1975, so it is a young health system with 40 years of age and has not changed much ever since. It has been able to achieve good outputs and final goals as well as continuously improving them. Notwithstanding this, there is room for improvement as it is now explained.
4.1.1. Health Improvement
Female life expectancy at birth is now 84 years, which is above the OECD average [19]. The health improvement in the recent years can be observed in the increase in the number of healthy life years at 65. In 2008, at 65 women were expected to have 5.6 years and men 6.7, respectably, of healthy life. In 2012, these figures had risen, respectively, to 9 and 9.9 years of healthy life. However, in 2014, these numbers have fallen for 5.6 and 6.9, respectively, while in average for the EU is 8.6 for both men and women [4].
Infant mortality has registered a significant improvement over a 10-year period. In 2000, the infant, neonatal and perinatal mortality rates were, respectively, 5.5%, 3.4% and 6.2%. In 2011 those rates had fallen to 3.1%, 2.4% and 3.8%, respectively [4].
However, the life expectancy at birth for men is somewhat lower than for women, by just over 6 years [20]. When it comes to life satisfaction, however, which measures how people assess life as whole and not just their current feelings, the Organization for Economic Cooperation and Development (OECD) life satisfaction index shows that Portugal has a relatively low level of overall life satisfaction [21].
4.1.2. Responsiveness and Consumer Satisfaction
The Health Consumer Index [22] placed Portugal 10th out of 28 European Union (EU) countries or 13th out of 37 health systems and the patient experience with ambulatory care in Portugal is very positive [19, 23, 24].
Despite the cultural limitation, when asked “How is your health in general?” only 46% of people in Portugal reported to be in good health, much less than the OECD average of about 68% and one of the lowest scores across the OECD countries [19].
The percentage of people reporting unmet need for dental examination is very high, no matter the level of income [19]. One likely reason is that dental care is not a part of the PHS and it is therefore only used by those who can afford it.
Complementary and alternative medicine are often used by people who pay for it in full, but this is very often not reported because of the social and medical taboos around these medicines [25].
4.1.3. Social and Financial Risk Protection
The financial function of the PHS is mainly financed by taxes and some proportion by employee/employer contributions. The pool of contributors is large enough to allow the pooling of financial risk across the population. The PHS is designed to accomplish the financial policy goals of financial protection, equity in finance and equity of access. However, this design may be more utopian than real.
Catastrophic health expenditure is defined as payment for health services that exceeds 40% of household disposable income after subsistence needs are met. There are vulnerable groups subject to these expenditures, including children, people with disabilities and individuals suffering from chronic conditions [26]. The prevalence of catastrophic health expenditures in Portugal is 2.1%, which is high percentage for a developed country with a universal national health system, and the main factor associated with such expenditures is the presence of at least one elderly person in the household [27].
4.2. Strengths and Weaknesses within the Functions of the Health System
4.2.1. Strengths
i. Stewardship
The planning and resource allocation in the Portuguese health care system is centralized, even though it accounts for some territorial structures [11]. Despite some attempts at decentralization, the idea prevails that the benefits arising from decentralization are dubious, it might increase the complexity of the system and most likely it would increase inequity [28].
Hospital management has taken different forms, such as public enterprises and public and private partnerships, and the payment system is grounded on a negotiated contract, which in turn is based on DRG (diagnostic related groups). grouping, fee for services, fee per chronic patient and pay-for-performance. These models of hospital management have been giving the health system quality and efficiency [19].
Another strength of the system that should be mentioned is centralized procurement, not only for the hospital sector but for the whole set of public health units. This enables the Central Purchasing Authority to control costs through price-volume agreements [29].
Finally, the last strength of the PHS to be mentioned is the separation of the provider, regulator and payer. This contributes to the good governance of the system [2].
ii. Delivery
Considering the principles of the PHS, the constitution, the general organization and management of the health care services, the Portuguese people ought to have access to primary, hospital and long term care [2].
iii. Financing
The PHS is mainly financed by taxes, but it is also financed by occupation-based health insurance, either public or private, for some occupational categories [2]. The public insurance arrangements (the subsystems) are additional to the national public health system and cover civil servants, the military and police forces. At present, and after the change of rules for financing under the Memorandum of Understanding (MoU), these public insurance arrangements have become financially self-sustainable [29].
iv. Resource Generation
a. Resource Generation - Human Capital
The country is endowed with eight medical schools which guarantee the quality and supply of doctors. The number of doctors per capita is even above the average of the EU12 [19]. There are about forty nursing schools in the country recognized by the nurses’ professional society and by the government. Both doctors and nurses are regulated by professional societies so that the quality of health services is kept at high standards.
b. Resource Generation - Information System and e-Health
The recognized ability of Portugal to develop e-government solutions [4, 30] is also present in the health sector. There is a rich health information data system which includes setting-specific information structures, disease-specific registers, electronic patient records and unique patient identifiers [21, 31, 32].
Some instances of the information systems available are now outlined. One of the e-platforms is the monitoring microsite which includes several indicators for access, efficiency, affectivity, production and satisfaction and which may be used as a hospital benchmarking tool. Another e-tool is the Health Dashboard which monitors the health of the Portuguese population each month. Finally, there is the electronic prescription platform for primary and hospital care which allows prescription by international nonproprietary names (international common denomination) and so it eases and permits the control of the prescription process [33].
4.2.2. Weaknesses
i. Stewardship
The organization of the health care services reflects a weak rationalization of the whole system. The PHS is over reliant on hospital care [20]: it is estimated that around 30% of hospital intervention could be handled in primary care [34]. However, the primary care level has failed to develop the provision capacity to respond to demand (more than a million people have no assigned family doctor) and long-term care is insufficient and inadequately developed to match the community’s needs [20].
Another potential weakness of the health system design is the way the public and private sectors are interrelated without their boundaries being precisely defined, financial and equity problems are raised [2].
The management of the system is, in general, weak and it needs improvement at both the organizational and leadership levels [1]. It is often argued that health professionals tend to be inflexible in their roles within the healthcare system and also that leaders and health professionals work with their backs turned to one another, without the communication needed to improve quality and efficiency [e.g.: 1]. Good governance, transparency and accountability as well as performance orientation and effective collaboration are organizational goals yet to be achieved.
ii. Delivery
Despite the extensive network of primary care units in Portugal, there is a large number of people who are not enrolled with a family doctor and do not have easy access to primary care. Dental care and complementary and alternative medicines such as acupuncture and homeopathy are not included in the Portuguese health system [2]. Moreover, long term, integrated and continuous care, as well as palliative care are clearly in short supply [20]. In 2014, there were 110 355 people dependent on someone else due to poor health status and of these about 44% are confined to bed. But the number of available beds for integrated and continuous care was only 6642 [35].
iii. Financing
Total health expenditure as a percentage of the Gross Domestic Product (GDP) was about 9.8% in 2010 and 9.1% in 2013, which is not far from the OECD average. However, the health expenditure per capita in 2013 was about 2514 USD PPP, while the OECD average is around 3450 USD PPP [19].
Other financial weaknesses worth mentioning are:
- a reduction of nearly 10% in real public health expenditure in 2012 [36]
- a reduction of 2.2% in the annual real average growth rate of health expenditure per capita between 2009 and 2011 [37]
- debts and arrears in hospitals continue to be a significant problem. Hospital debts were around €1.314 billion in 2014. Fortunately, in this same year there was a €271 million fall in debts; the amount of arrears has fallen nearly 70% since 2011 [5].
- out of pocket expenditures, as a percentage of the total health expenditures, has been increasing and it is one of the highest in Europe [4, 19, 38]
iv. Resource Generation
a. Resource Generation - Human Capital
The country is a net exporter of nurses [39], nursing graduates are lower in number than the OECD average, the number of practicing nurses is small [19] and there are no family nurses. The density of General Practitioners (GPs) is relatively low (and getting worse as doctors retire [40]). Moreover, the nurse-to-physician ratio is small: about 1.4 nurses for each doctor, whereas the EU28 average is 2.3 [3, 20, 29, 35]. GPs are unequally distributed around the country and are mainly concentrated in large cities [20, 35].
b. Resource Generation- Information System and e-Health
Human resources, including doctors, nurses, and patients, are not properly trained to use the information system and e-health features offered so as to improve quality and efficiency [41]. The information systems often run slowly and/or collapse. Moreover, several information systems [33] are used in each healthcare unit and often they are not interconnected, which leads to accounting discrepancies and waste of resources [41, 42].
4.3. Strengths and Weaknesses within the Intermediate Goals of the Health System
4.3.1. Strengths
i. Access
The right to health [43], the core of any health system, is guaranteed by the Portuguese constitution. The PHS is defined by universal access to all residents and with low payments at the point of use. Its goal is to protect the health of the population living in Portugal. Health policies should promote equal access to health care for the citizens, irrespective of economic condition and geographic location, and they should ensure equity in the distribution of resources and use of health care services.
ii. Coverage
The design and definition of the PHS accomplishes the four values listed in the Statement on Common Values and Principles [44], which underpin all the European health systems: universal coverage; solidarity in financing; equity of access; and provision of high quality health care.
iii. Quality
Patient experience of ambulatory care is quite positive in terms of doctors spending enough time with patients at appointments, providing easy-to-understand explanations, giving the opportunity to ask questions and raise concerns and involving patients in decisions about care and treatment [19].
A quality competitive context has been created within hospitals with the publication of a Ranking of Hospitals. This ranking aims to measure hospital performance for admitted patients and it covers all public hospitals [45].
iv. Healthy Behavior
The amount of daily smoking has shown a declining trend for male adults [4, 32]. The average amount of fruit and vegetables eaten per person is about 275 kg/year which is above the EU28 average [38].
v. Efficiency
The WHO proposal on how to assess a health system’s performance is based on sophisticated statistical analysis. The overall healthcare system performance was measured for 191 countries [46]. The PHS ranked 12th best out of 191 WHO members and 6th within the EU countries.
Bloomberg rankings [47], in 2014, have rated countries according to the quality of the health system. Based on the efficiency of their healthcare systems (140 countries), the PHS comes 12th out of 40 European countries, but is below the median score.
PHS has shown a strong resilience during economic and financial crisis. Despite the strong cuts, the reported statistics on health have not followed an identical path of worsening [20, 36].
4.3.2. Weaknesses
i. Access
The most common reason cited to justify unmet health care needs is tight disposable income. In 2013, the percentage of people self-reporting unmet needs for medical examination because they could not afford it is 2.4%, which is the EU average [4]. But the figure for England is 0.1%.
In 2014, 5.5% of the population over 16 y.o. reported unmet health care needs and 18.8% reported unmet dental care. Of these, 53.5% reported financial constraints on obtaining medical care, while 82.5% said the same for dental care [48].
In Portugal, the figure for care needs unmet due to financial constraints, transport costs or waiting time, for the lowest level of income, is the same as the OECD average [19]. Concerning unmet dental care, the figure for Portugal is higher (23.7%) than the OECD average (9.6%), in the population with the lowest income. Additionally, the weight of medical expenditures in the final household consumption is greater in Portugal than in other European countries. On average it represents 3.9%, while the figure for the OECD is 2.8% and 1.4% for the UK [19].
Another noteworthy weakness of the Portuguese health system concerns access to new drugs and therapies. New drugs are very often launched considerably later than in higher-priced EU markets [49], one well known example being the hepatitis C drug [50]. The result is poorer public health, and even higher patient mortality.
ii. Coverage
The PHS fails to public cover most dental care and almost every complementary and alternative medicine. People using these health services have to pay for them in full. Moreover, most public health services charge some fee at the point of use [51] and most pharmaceuticals offer only a small rate of reimbursement [2].
iii. Quality
Regarding primary care, a significant number of people do not have family doctor. About 12% of Portuguese do not have an assigned family doctor [52], which means that nearly 1233236 of people face some difficulty in accessing primary care.
On the other hand, in hospital care, a major weakness is the high number of hospital infections, one of the worst in Europe [53] and post-operative sepsis in abdominal surgeries is the second highest in the OECD countries [19]. The numbers have increased so much that Fundação Calouste Gulbenkian (FCG Foundation)1 has decided to create a contest called Stop hospital infections [1] which aims to reduce infections by 10% in the next three years.
Another weakness that is to be noted is that the deaths following an acute myocardial infarction and after admission for ischemic stroke are higher than the OECD average [20].
iv. Healthy Behavior
The trend for female smoking on daily basis has been increasing [4, 38]; the alcohol consumption per capita is one of the highest in the OECD countries [19]; child obesity is a current problem, reflecting unhealthy lifestyles chosen by
parents; the prevalence of adult obesity is also an issue, the rate being the third highest in the EU15 in 2006 [54]; physical activity is one of the lowest in the European Union, while the number of those who never exercise is one of highest, around 64% of adults never do any physical exercise [55]. Mental health has declined over the last few years. The prevalence of mental disorders in Portugal is one of the highest in Europe at about 22.8% [56, 57].
v. Efficiency
In 2010, Joumard et al. [10] compared health care systems from different countries. They placed the PHS in Group 5, which has the following features: public provision and public insurance, gate-keeping, limited choice of providers and soft budget constraint. The ranking of countries in this Group, from best to worst, is as follows: Denmark, Finland, Spain, Portugal and Mexico. Across the all set of country groups, it can be observed that Portugal performs below the OECD average and it is among the 10 worst performing countries, out of 29 OECD countries.
The international comparisons continue to show that there is room for improvement in both quality and efficiency.
4.4. Opportunities and Threats to the Portuguese Health System
4.4.1. Threats
Most European health systems face common challenges arising from new risk factors such as aging populations, health inequalities, people’s higher expectations, rising healthcare expenditures, technological innovation and scarce human resources [24]. The Portuguese health system is no exception.
The economic and financial crisis which started in 2008, resulting in the bail-out of 2011 and the following austerity, has produced both direct and side effects on the health system and on the population’s health that are yet to be understood, measured or properly assessed. Moreover, the medium run economic and social impacts on Portuguese society are yet to be fully understood. Despite these areas of uncertainty, some trends can be identified.
i) The demographic evolution shows that the population is aging, as is the European population (the old age dependency ratio in Portugal is above 30%). The fertility rate is not high enough to replace the previous generation; the fertility rate in Portugal is 1.2 while in the UK is 1.8 and in France and Ireland it is 1.9 [4].
Adding another demographic threat to this picture, Portugal has suffered a high emigration rate for the last few years. This is a new wave of emigration. Portuguese emigrants are young and educated, which is causing a brain drain from the country [58, 38], including doctors and nurses.
ii) A second threat to the Portuguese health system is how health population is tending to progress and change. There are two very significant trends. Firstly, the high prevalence of diabetes, about 9% in 2013 [37], is one of the highest in European Union. This represents an economic burden of 1% of Portuguese GDP and about 10% of health expenditures [59].
This diabetes trend may become exponential if we take the high rate of child obesity in Portugal into account [60]: for instance, among 7-year-olds, 40.5% of boys and 35.5% of girls are overweight and 16.7% and 12.6%, respectively, are obese [61].
The second trend that deserves attention is the mental health status of people. Portugal has one of the highest consumptions of antidepressants in Europe. Figures for 2013 show that the Defined Daily Dose (DDD) of antidepressants, in Portugal, is equal to 88, per 1000 people per day, while the average for the OECD28 is equal to 58 DDD [20]. The economic crisis, the lack of psychologists in primary care and over-prescription by GPs could explain this excessive consumption of antidepressants.
iii) Another threat is the detrimental economics and social dynamics that have been observed in Portugal: slow or absent economic growth, high unemployment rate and increasing income inequity and poverty. Portugal has the highest proportion of people living in absolute poverty in the EU15; a high proportion of people living in rural areas with poor access to health services and the Gini coefficient is 34.5%, higher than the EU28 average, which is 31% [4, 62]. The Morgan Stanley Inequality Indicator Ranking, which is multi-faceted and aggregates several indicators, especially labor market ones, captures different aspects of inequality and places Portugal at the top, indicating it as the country with the strongest level of inequality [63].
Alongside the unfavorable economic and social dynamic, the pressure to increase the health budget threatens its fiscal sustainability. Health spending is difficult to control both because the public perceive health care as a priority and because of the large number of health care stakeholders. Despite the slowdown of spending during the economic and financial crisis, OECD projections show that public spending on health and long-term care is on course to reach almost 9% of GDP in 2030 and as much as 14% of GDP by 2060 [64].
iv) Last, the threat of increasing prices of health technology and innovation. This results in rising costs and increasing health expenditure. Not only is this rise tending to be higher than the GDP growth rate, it also has to be supported by constrained health budgets imposed by the EU requirement for balanced public budgets.
4.4.2. Opportunities
The opportunities presented to the PHS [1, 20] may be properly managed, as challenges, leading to an improvement in the quality of the health system and population health.
i. Healthcare is Becoming More Focused on the Person
First, patient empowerment means that people need to be engaged with health strategies to prevent illnesses and they need to feel empowered to manage their own health. Educating people for health issues can contribute to a smoothly functioning health system, but providing accredited high-quality information also helps people to manage their own health condition [65, 66].
Second, the development of a person-centered model of healthcare is a challenge that has emerged from the increasing prevalence of chronic diseases in the population. New models of providing health care services will be developed or enlarged, where the patient can become the stakeholder in their care, where home can be the preferred location, where information technology plays a significant role and coordination across the health care services is central [65, 66].
ii. Healthcare is Becoming a Highly Digitalized Sector
Patient records create a huge amount of information and this digitalized information feeds the possibilities of person-centered and personalized health care. This large amount of information supplies a medicine based on prediction and prevention instead of a breaking and fixing approach. In addition, health authorities may be able to gather plenty of electronic information about patients, such as, information provided by health monitors, ventilators or wearable devices; geographic information system technology, wireless communications and GPS provide more data that can be used to improve both the individual’s health and how the health system functions. A wide range of technology, from apps to personal health devices, which gathers information and helps to monitor peoples’ health; the electronic patient record centralizes a set of health information which contributes to faster and easier decisions on one’s health [65, 66].
Finally, big data analysis is already at stack level. Almost everything that determines health can be stored in databases. This information can be used to identify patterns of diseases, links between causes and symptoms, efficacy of treatments and adverse event drivers. Big data analysis will help to improve the efficiency of the health system [67].
The PHS has much to gain in quality and performance by improving its ability extract the benefits offered by the digitalization of the health sector.
iii. Health Technology Assessment (HTA) is Highly Used in the Health Sector
HTA has been used to search for the best value for money in health care for some years now and the experiences in other countries favor using it. HTA does not only apply to pharmaceuticals, it is for medical technologies and de-investment decisions, too [62]. The importance of health technology assessment in recognizing the value of innovation within limited health system resources justifies the creation or implementation of an organization, body or exploiting the more usual university consulting services to support decision making in the health care sector.
Portugal has a national system of health technology assessment, called SiNATs, which was created in 2014. At present, the assessment is mainly restricted to drugs but it aims to assess health technologies and health programs [68]. Other countries’ experience, such as National Institute for Health and Care Excellence (NICE) in the United Kingdom (UK) [69] provide a source of information about the good practice and governance of HTA. Moreover, having a national body for HTA and the European cooperation on this issue through the EUnetHTA encourages the exchange of information and the harmonization of decision making about coverage [70].
iv) A final point to highlight one more opportunity for the PHS: continuous quality improvement. This includes quality governance [71], and the provision of primary and hospital care. This both improves quality, efficiency and efficacy. The adoption of good clinical practices and the use of evidence based practices together with forward-looking leadership and the involvement of society as a whole support such quality improvement.
They demand transparency of data and processes. As a consequence, healthcare organizations will need to focus on how quality outcomes can be published in a meaningful way for patients. Patient safety is the major focus of patient advocacy groups and healthcare leaders. They will enforce deeper investigations of medication errors, hospital acquired infections, wrong site surgery and pressure sores, like never before.
4.5. Some (Possible) Recommendations for Strategies and Policy Measures
Having set out the features describing a SWOT view of the PHS, some strategies can be outlined according to the relationship between the different SWOT components and also the final aims of the health system. Four types of strategy can be found:
i) use of strengths to take advantage of opportunities ii) minimize weaknesses by taking advantage of opportunities, iii) use of strengths to avert threats, and iv) minimize weaknesses and avert threats.
Without aspiring to describe all strategies possible within the SWOT approach just presented, we suggest some strategies as an example.
-
The use of strengths to take advantage of opportunities:
- The increasing adoption of information and communication systems in the health care system is the path to establishing the foundations for the health digitalization opportunity. Person-focused medicine, whether for managing healthy people or those with chronic disease, both in primary and hospital care, helps to improve the health of the population and to meet people’s expectations about the functions of the health system and their freedom of choice.
- The centralized organizational structure of the health system can gain from having a centralized body running health technology assessment (HTA) because information and good practice can easily be properly disseminated; centralization of the HTA has proved to be effective in other countries (for instance, NICE in the UK) and also within the EUnetHTA.
-
Overcoming weaknesses by taking advantage of opportunities:
- Person-centered medicine and digital health might be better explored when health care is more focused on primary care rather than on hospital care. This requires a change in where the emphasis is placed within the PHS, in particular, the expansion of primary and integrated care. The change in health care emphasis from hospital care to primary and integrated care is a priority in the PHS, which will clearly help propel the health system towards its final goals. Moreover, this strategy is strongly linked with the strategy outlined previously, to encourage person-focused medicine.
- A properly performed HTA, applied to drugs, medical equipment, and other investments, can improve the efficiency of the health system and control its cost. HTA thus helps to balance the public health budget and to protect people against social and financial risk.
- Improvement in quality requires quality resources, in particular, sound human capital, which can be created in the nursing and medical schools in the country and attracted to stay in Portugal. Human resources in the PHS have been under a great strain in recent years. It is not enough to produce health care professionals with degrees, we also have to create conditions to keep them in Portugal and prevent them from feeling frustrated. The incentives are both pecuniary, like pay for performance, and non-pecuniary, like holidays and due appreciation.
- Improved quality is also promoted by good governance of the health system, meaning the cultivation of openness, transparency and integrity, performance orientation and effective collaboration. This is based on human resources duly trained in leadership, teamwork and management skills, and also consolidated and interoperable information systems.
-
The use of strengths to avert threats:
- The funding source used to finance the PHS is based on taxes and on occupation-based contributions and creates a big pool of contributors. This allows for a good cross subsidization and risk share among all people and so provides the strength to deal with the social and economic challenges that the country faces. Fiscal sustainability seems more achievable with this method of financing the health system - more from taxes and workers’ contributions and less from out of pocket payments. Financing equity is also implicit in fiscal sustainability as it helps to protect people against catastrophic health expenditures.
- The improvement and motivation of people’s health behaviors do contribute to the prevention of chronic diseases. Education and the person-focused approach of primary care and related policies, in line with “health in all policies” approach fuels the good health status of people in general [81].
- The job market opportunities could well be filled by the doctors and nurses graduating from training schools each year. The management of human resources starts at the point of graduation and on-the-job training, as well as the coordination with opening positions. Moreover, the improvement of the doctor-nurse ratio requires more nurses in the system, such as family health nurses, a category yet to be created that would definitely improve general public health.
-
To minimize weaknesses and avoid threats:
- These strategies mainly aim to reduce barriers to access, minimize the shortage of primary care, cut the catastrophic expenditures and change unhealthy behaviors.
LIMITATIONS AND CONCLUSION
The limitations of classic SWOT analysis can be also be noted in this work [72, 73]. The SWOT perspective identifies issues but does not provide solutions; it does not prioritize the concerns identified, information gathered may be oversimplified and crucial data overlooked, and it does not accommodate trade-offs. Moreover, the issues discussed here, under the SWOT instruments, do not follow any structured literature review, because it would not be possible due to the limited available space, and therefore some bias may be introduced. Additionally, this type of work may be imprinted by the authors view on the subject.
Despite the limitations, this work has reviewed the description of the Portuguese health system and provided an overview of how it has been classified in the last 30 years. Its main characteristics have not changed significantly in that period. The PHS is mainly financed by taxes and partially by professional contributions, provision and control are mainly responsibility of the government, but there is also provision of health care services by the private sector.
The economic and financial crisis that hit the country, in 2008 ended with a bail-out in 2011. Some changes were imposed on the health system, in particular, reducing expenditures. By forcing the reduction of expenditures, the MoU introduced and induced changes in the health system. This new picture of where the Portuguese health system is placed brings in new thoughts and reflections. A SWOT approach to the Portuguese health system provides a simple and clear way of thinking about the most appropriate strategies to improve the quality and efficiency of the PHS.
The SWOT factors presented are based on the definition of a health system proposed by WHO [15], that is, according to the functions and goals. The strengths and weaknesses were identified within the functions and the opportunities and threats within intermediate goals. We have concluded by presenting some possible strategies that take the SWOT factors into account. These strategies combine the strengths, weaknesses, opportunities and threats to design a suitable strategy to improve the final goals of the Portuguese health system and the likelihood of achieving them.
The analysis provided here is unique of its kind and it contributes to better health policy design and potential reforms. Any improvement expected for the Portuguese health system and for the health of the Portuguese population will have to take into account the SWOT analytical perspective or at least some part of it.
CONFLICT OF INTEREST
The author confirms that this article content has no conflict of interest.
NOTES
1 The FCG is an international charitable foundation with cultural, educational, social, and scientific interests. The Foundation, the largest in Portugal, is highly respected and influential and thus well placed as an independent space to convene and lead discussions on future direction.
ACKNOWLEDGEMENTS
Declared none.


