All published articles of this journal are available on ScienceDirect.
The Social Determinants of Healthcare Access for Rural Elderly Women - A Systematic Review of Quantitative Studies
Abstract
Objective:
This review aimed to explore and analyze the social determinants that impact rural women’s aged 60 years and older healthcare access in low or middle income and high income countries.
Methods:
Major healthcare databases including MEDLINE and MEDLINE In-Process, PsycINFO, PubMed, ProQuest, Web of Science, CINAHL and ERIC were searched from April 2016 to August 2016 and a manual search was also conducted. A rigorous selection process focusing on the inclusion of rural elderly women in study population and the social determinants of their healthcare access resulted in 38 quantitative articles for inclusion. Data were extracted and summarized from these studies, and grouped into seven categories under upstream and downstream social determinants.
Results:
Prevailing healthcare systems in combination with personal beliefs and ideas about ageing and healthcare were identified as significant determinants. Socioeconomic and cultural determinants also had a statistically significant negative impact on the access to healthcare services, especially in developing countries.
Conclusion:
Potentially, improvements to healthcare access can be achieved through consideration of rural elderly women’s overall status including healthcare needs, socioeconomic determinants and cultural issues rather than simply establishing healthcare centers.
1. INTRODUCTION
The prevalence of morbidity, comorbidities and premature deaths associated with rural elderly women (REW) is related to access to modern healthcare services (MHS) [1, 2]. Elderly women are classified as 60 years of age and over [2], and generally represent a higher proportion of all elderly people as they tend to live several years longer than men [3]. For example, elderly women accounted for 54% of the total elderly population worldwide in 2015 and 52% of these women live in rural areas [2, 3]. Many REW lack access to MHS and underutilization of MHS is identified as a major reason for premature and preventable deaths [4, 5]. This underutilization is skewed toward a lower rate of hospitalzation is skewed toward a lower rate of hospital visits, diagnosis, hospitalizations and complete treatment [2]. Thus, inadequate healthcare access for REW presents a challenge to all countries that value good health outcomes for REW, especially low and middle income countries as defined by World Bank.
The social determinants of health (SDoH) are directly related to healthy ageing for REW, and they range from social to healthcare to individual sphere [6, 7]. The determinants of REW’s access to healthcare sphere include inadequate services, a shortage of professionals, a lack of medical equipment and medications, the cost of services and long waiting times [6, 7]. A number of other determinants, originate from social, economic and cultural contexts, have specific impact on REW’s MHS utilization [6]. For example, poverty has a negative impact on the REW’s MHS access and use because of their dependency on household economy, as well as literacy levels [2]. As such, having a high level of health illiteracy, in low, middle and high income countries, means a better access to MHS for REW as it is related with care seeking beliefs and behaviors [3]. Some evidences also show that close, personal characteristics, social relationships and transportation difficulties also impact MHS use, and that typically, healthcare policy and practice ignore these aspects of daily life for REW [3, 6, 8].
Evidence about the access to MHS exclusively by REW is scant [6, 7]. Present literature either lost their focus on REW as a population group or investigated the SDoH affecting the utilization of MHS by REW concentrating on different aspects [3]. None of the study has assessed the determinants systematically and comprehensively. A systematic review of quantitative studies was, therefore, conducted to understand the SDoH impacting on healthcare access among REW in low/middle income and high income countries.
2. METHODS
2.1. Search Strategy
Literature search was undertaken (PROSPERO: CRD42016046605) across major electronic databases including MEDLINE and MEDLINE In-Process, PsycINFO, PubMed, ProQuest, Web of Science, CINAHL and ERIC. A combination of several key words along with their synonyms was used in the search including ‘healthcare access’, ‘healthcare utilization’, ‘healthcare resources’, ‘access barriers’, ‘socioeconomic factors’, ‘healthcare’, ‘health seeking behavior’, ‘elderly’, ‘older women’, ‘rural women’, ‘rural health’, and ‘remote areas’. This search was conducted from April 2016 to August 2016. A manual search was also conducted of the relevant references of retrieved articles, citations by authors, hand searched articles and experts’ opinions. The search and selection strategy was developed by the principal author and reviewed and checked by the other authors and one librarian [9].
2.2. Data Selection Strategy
Only peer reviewed empirical quantitative studies published from January 2000 to August 2016 in English were considered. To be included in this review, a study had to have REW as research participants. Additionally, studies were included if they investigated determinants of healthcare access in relation to preventive measures, communicable and non-communicable diseases, and reported at least one of the MHS access related outcomes. Studies on interventions targeted at the identification of the determinants and its association with healthcare utilization for REW were included. Studies that were excluded included literature reviews, secondary analyses of data and if the data were not specific to determinants of REW’s healthcare access. Studies were also excluded if they reported healthcare access from non-relevant aspects or specialized care such as the use of complementary and alternative medication, exercise, pre-natal care and pregnancy, reproductive healthcare, childbirth and post-natal care, dental care, cancer care, HIV and palliative care. No country or follow-up study restrictions were applied.
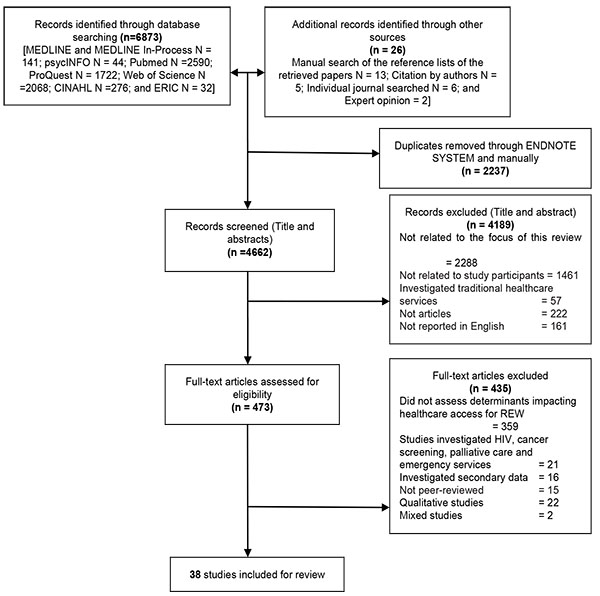
2.3. Data Extraction Process
The initial literature search identified 6899 citations. There were 473 articles of potential interest and, after examination of the full texts, 38 quantitative studies met all inclusion criteria apart from the provision of explicit healthcare outcomes for REW (See Fig. 1). A checklist was used based on the guidelines from the Centre for Reviews and Dissemination (CRD) for assessing the quality of each study [10]. The data synthesis and analysis processes followed the CRD guidelines. Each article was assessed for methodological quality following several criteria namely: relevance to this systematic review; validity and appropriateness of methodology and instruments used; quality of research evidence such as generalizability of the findings; reporting quality in terms of data analysis process; and stated limitations in the study and how these limitations were adjusted [10].
Information was extracted from each study about authors, years, settings, participants, research methods and findings on the stated determinants in relation to healthcare access and healthcare seeking (See Table 1). Most of the studies included different population groups in their investigation and only one study identified that solely investigated REW’s healthcare access in USA. Thus, the authors selected the studies that included at least 10% REW of the total study population and reported the determinants of the REW’s healthcare access differently. These determinants were related to: (i) the REW such as literacy; (ii) the economic condition such as poverty; (iii) the medical treatments including health seeking beliefs and behaviors; (iv) the healthcare system including accessibility and adequacy of healthcare facilities; and (v) sociocultural status including mobility and social relationships.
2.4. Data Analysis Process
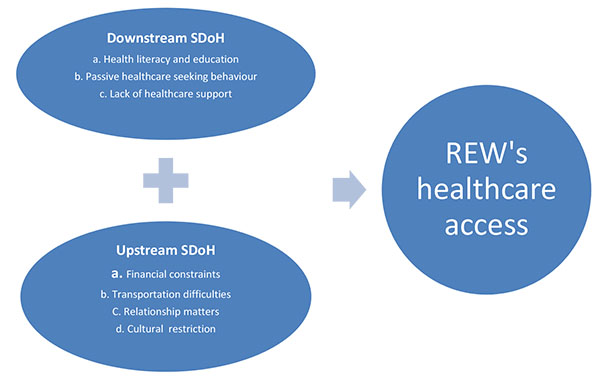
Meta-analysis of the data was inappropriate because of the heterogeneity in the studies including socioeconomic and cultural differences in low, middle and high income countries, the collected data, designs and settings. Extracted information from the selected studies was tabulated and significant SDoH were included. Multifaceted relationships between the SDoH were identified and grouped into themes using a combination of thematic and content analysis. The model developed by Braveman, Egerter & Williams in 2010 was employed because of its categorization of the SDoH that can provide structure to the identified evidence in the discussion chapter. Two broad categories in the SDoH were identified focusing on healthcare inequalities and disadvantages, including downstream and upstream SDoH [11]. Downstream SDoH mean the factors that impact on healthcare at macro level, and they include health knowledge, perceived healthcare seeking behaviors and healthcare support [11]. Upstream SDoH mean the inequalities in socioeconomic and cultural circumstances, which are fundamental causes of low healthcare access [11]. Applying this model distinguished the determinants, often intertwined in personal, healthcare, socioeconomic and cultural factors.
| Study | Country | Study design (Period of research) | Data collection tool | Representation of REW | Findings |
|---|---|---|---|---|---|
| Ameh et al. 2014 | South Africa | Cross-sectional study (2010) | Interview Simple random sampling 7870 |
74.8% | Education (six and more years of education had a twofold increased odds of using health care compared to those with no formal education) - p < 0.05 (p = 0.001) (OR: 2.49; CI:1.27 - 4.86) Medical aid cover - p < 0.05 (p = 0.001) Occupation - p < 0.05 (p = 0.001) Socioeconomic status - p < 0.05 (p = 0.001) Do not think they are sick enough – significant (P value is not reported) Could not afford the cost of health facility visit - significant (P value is not reported) Inadequate drugs and treatment - significant (P value is not reported) being treated poorly during previous visits - significant (P value is not reported) No transport available - significant (P value is not reported) Inadequate skilled staff - significant (P value is not reported) Do not know where to go - significant (P value is not reported) |
| Bell et al. 2005 | USA | Cross-sectional study (2001 – 2002) | Face-to-face survey Simple random sampling 698 |
49.1% | Education - p < 0.01 Poverty - p < 0.01 On Medicaid vs no Medicaid and income - p < 0.01 Cost of medications for diabetes - p < 0.01 |
| Byles et al. 2006 | Australia | Longitudinal population-based Study (1996, 1999 and 2002) | Survey (mailed) 8387 |
60% | Higher out of pocket costs - significant (P value is not reported) Lower satisfaction with GP services - significant (P value is not reported) Higher use of community healthcare services - significant (P value is not reported) Identified themselves as caregivers - significant (P value is not reported) |
| Chan and Griffiths 2009 | Pakistan | Comparative descriptive study (2006) | Interviewed by information table and questionnaire Convenience sample 125 |
36.0% | Feeling depressed and helpless - p < 0.001 Feeling lack of resources including Medical - p < 0.001 Food - p < 0.001 Clothes - p < 0.001 Shelter - p < 0.001 Financial support - p < 0.001 Social support - p < 0.001 Living alone - p < 0.001 Living with relative and neighbors - p < 0.01 |
| Loosing geographic access to healthcare center after earthquake - significant (P value is not reported) Travel distance - significant (P value is not reported) |
|||||
| Cheng et al. 2005 | China | Cross-sectional study (2001) | Interviewed using a standard questionnaire Randomly selected 190 |
22% | Lack of education (The median delay of patients with an educational level of middle school or above was one third of that of patients with no education) - p < 0.05 Distance from home to township health center (km) - patient delay hazard ratio at 95%CI - 1.04 (0.98-1.11) Distance from home to township health center (km) - health system delay hazard ratio at 95%CI - 1.01 (0.95-1.07) Do not know that their disease was serious (24.7% said that) Poverty (21.1% accepted that) Lack of expensive medical equipment - significant (P value is not reported) Insufficient incentives for village doctors - significant (P value is not reported) |
| Gopalan and Durairaj 2012 | India | Cross-sectional study (2008) | Household survey Multi-stage random stratified sampling 800 |
51.0% | Financial limitations - p < 0.05 (OR 2.00, 95% CI 0.84-4.80) Household response to women’s healthcare needs - p < 0.05 (OR 2.04, 95% CI 1.09-3.83) Lacking other financial support - p < 0.05 (OR 2.13, 95% CI 1.11-4.07) Perceived non-seriousness - significant (P value is not reported) Residing far from health centers (28.4% reported it as a barrier) - P value is not reported |
| Gopichandran and Chetlapalli 2013 | India | Cross-sectional study (2013) | Interview using structured questionnaire Multistage sampling strategy 640 |
11.8% | Healthcare access is determined by trust in doctors. The factors relating to trust in doctors were: Personal relation with doctors - p < 0.05 Behavior of doctors - p < 0.05 Simple appearance of doctors - p < 0.05 Cultural competence of doctors - p < 0.05 |
| Harrison and Wardle 2005 | UK | Cross sectional study (2000-2001) | Survey Comprehensive sampling approach 313 |
31.4% | People over 65 years of age are statistically significantly less likely to complete cardiac rehabilitation than people under 65 years of age, thus, Age - p < 0.05 (p = 0.02) Women have a significantly lower rate of completing cardiac rehabilitation than men, thus, Gender - p < 0.05 (p = 0.02) Access to services was the major factor, reported by 50.8% of respondents (P value is not reported) |
| Huong et al. 2007 | Vietnam | Cross-sectional survey (2002) | Pre-coded structured questionnaire Stratified sampling method 2087 |
18% | Patient delay Being female - p < 0.005 Increasing age with increasing distance - p < 0.05 |
| Initial visit to local public health facilities - p < 0.005 Patients delay is longer in rural and remote areas than urban areas - p < 0.005 Healthcare provider (HCP) delay HCP delay is longer for women aged 65 years old and over - p < 0.005 HCP delays were also longer for patients with a high level of education or who visited initially the private sector - p < 0.001 HCP delays were also longer for patients living at more than 5 km distance from the health facility - p < 0.005 HCP delays were also longer for patients living in rural areas - p < 0.0001 |
|||||
| Ingold et al. 2000 | Switzerland | Appropriateness Evaluation Protocol (AEP) (1995-1996) | Research nurse interview Patients who admitted in the hospital 196 |
63.3% | Living alone - p = 0.008 (OR 6.4, 95%CI 1.6 - 24.8) Going out of home - p < 0.05 (p = 0.003) Receive formal in-home help - p < 0.05 (p = 0.031) Depression - significant (P value is not reported) |
| Jordan et al. 2011 | Australia | Cross-sectional study (1996-2004) | Telephone survey Randomly selected 944 |
53.7% | No formal education - p < 0.005 (p = 0.02) Self-management advice for heart failure of women - significant (P value is not reported) Medication taking behavior - significant (P value is not reported) |
| Judd et al. 2006 | Australia | Cross-sectional community survey | Survey Random selection 467 |
28% | Distress - significant (P value is not reported) Lower stoicism - significant (P value is not reported) |
| Judd et al. 2008 | Australia | Cross-sectional community survey | Survey Random selection 579 |
25% | Education equal or less than 12 years of schooling - p < 0.05 Stoicism - significant (P value is not reported) Perceived stigma - significant (P value is not reported) |
| Mariolis et al. 2008 | Greece | Cross sectional study (2006) | Survey questionnaire Stratified randomization 375 |
30% | Lack of education - p < 0.001 Distance to healthcare centers - p < 0.001 Lack of primary healthcare services - significant (P value is not reported) |
| Melese et al. 2004 | Ethiopia | Population-based survey | Interview Multistage cluster sampling 850 |
35% | Direct cost (inability to pay for the medical care) (25.6% respondents reported it as a barrier) - p < 0.05 Indirect cost (lack of money to cover the cost of transport, food and lodging expense for the patient and accompanying person) - (35.4% respondents reported it as a barrier) - p < 0.05 No one to give company - (9.4% respondents reported it as a barrier) - significant (P value is not reported) Distance and lack of transport - significant (P value is not reported) |
| Onwubiko et al. 2014 | Nigeria | Population based, cross sectional descriptive survey (2011) | Researcher administered questionnaire Multi stage cluster random sampling 501 |
40% | Possession of formal education - p < 0.001 (OR 0.3; CI 0.1-0.5) Living alone - p = 0.01 (OR 2.26; CI 1.41-3.63) Ignorance (56.5% respondents reported it as a barrier) - (P value is not reported) Healthcare cost (59.2% respondents reported it as a barrier) - (P value is not reported) Restricted spatial access (67.9% respondents reported it as a barrier) - (P value is not reported) Self-assessment of eye diseases as not serious enough (31.3% respondents reported it as a barrier) - (P value is not reported) Belief that ageing has no cure (20.2% respondents reported it as a barrier) - (P value is not reported) Preference to spiritual treatment (0.9% respondents reported it as a barrier) - (P value is not reported) |
| Peltzer 2004 | South Africa | Empirical study Health belief model given by Brown and Segal (2000) |
Face to face interview with self-administered questionnaire 100 |
30% | Took something else for high blood pressure apart from prescription medication - p < 0.001 Faith healing - p < 0.001 Using over the counter drugs - p < 0.05 Cost of medications - p < 0.001 Forgetting to take medications - - p < 0.001 Ignorance of side effects - p < 0.001 Has not explained the medical problems to patients - p < 0.01 |
| Pullen et al. 2001 | USA | Descriptive correlational design (Health Behavioral models) | Computer-assisted interviewing system (Telephone survey) Convenience sampling 102 |
100% | The influence of providers’ recommendations on service utilization - p < 0.001 Distance - significant (P value is not reported) Sources of health information - significant (P value is not reported) |
| Masud et al. 2005 | Bangladesh | Baseline survey (Health Behavioral model) (2003) | Structured interviews Random selection 966 |
62% | Self-care tendency - significant (P value is not reported) Education to seek healthcare from formal allopathic healthcare providers - p < 0.01 (OR 1.50; CI 1.15 - 1.96) Poverty to seek healthcare from formal allopathic healthcare providers - p < 0.05 (OR 0.75; CI 0.60 - 0.95) |
| Weaver and Gjesfjeld 2014 | USA | Cross-sectional study (Multivariate logistic regression) (2002-2003) |
Telephone survey Second-stage randomization 4,311 |
35% | Education- p < 0.01 Household income - p < 0.01 No insurance in the past year - p < 0.001 Easy source of care - p < 0.01 Contact doctor as last resort - p < 0.05 |
| Xu and Borders 2003 | USA | Longitudinal survey (Behavioral model) (2001) | Telephone interview Random selection 1062 |
71.56% | Education less than high school - p = 0.05 Employment (not working) - p = 0.04 Insurance coverage (no insurance) - p < 0.01 Not taking prescription drugs - p < 0.01 Lack of pharmacies - p < 0.01 |
| Yamasaki-Nakagawa et al. 2001 | Nepal | Cross-sectional study | Face-to-face interviews 336 |
15% | Education (illiteracy) - p < 0.001 Travelling time - p < 0.001 (Women had a longer total delay than men, p = 0.034) Initial visit to a traditional healer - p < 0.001 (P = 0.012) Fees paid to healthcare providers - significant (P value is not reported) |
| Young et al. 2000 | Australia | Longitudinal Study (1996 – 1997) |
Postal questionnaire Community sampling 4,577 |
40% | Out of pocket payment - significant (P value is not reported) Shortage of female GPs - significant (P value is not reported) Poor access to afterhours care – significant (P value is not reported) Waiting times - significant (P value is not reported) Cost of GP visit - significant (P value is not reported) |
| Young et al. 2001 | Australia | Longitudinal Study (1997) | Baseline survey through HSS questionnaire Random selection 4452 |
47% | Out of pocket payment per GP visit - p < 0.001 Distance - p < 0.001 Skepticism (the value of medical care) - p < 0.001 |
| Abdulraheem 2007 | Nigeria | Cross-sectional study (2004) | Survey & Interviews Proportional sampling 1125 |
54% | Poverty reduces the number of seeking healthcare from qualified medical practitioner - 0.46 (0.38 - 0.67) Education increases the number of seeking healthcare from qualified medical practitioners - 0.59 (0.48-0.87) Distance - significant (p value is not reported) Waiting times - significant (p value is not reported) Availability of services - significant (p value is not reported) Living alone - significant (p Value is not reported) |
| Adu-Gyamfi and Abane 2013 | Ghana | Human ecology of disease triangle model (Life-cycle determinant model given by (Meade & Earickson in 2000) |
Questionnaire and interview guide Multi-stage sampling 120 |
10% | Place of residence in terms of healthcare centers - p < 0.05 (p = 0.021) Utilization of healthcare facilities outside one’s locality considering time, distance, cost of transport and the nature of the roads - p < 0.05 (p = 0.001) Education - significant (p value is not reported) Married women utilize local healthcare facilities more than single people p< 0.05 (p = 0.027) Health insurance coverage - significant (p value is not reported) Inadequacy of health care facilities such as personnel, equipment and medicine significant (p Value is not reported) |
| Blay et al. 2008 | Brazil | Cross-sectional study (1995-1996) | Structured in-person interviews Multi stage random sampling 7040 |
66.0% | Education (< 4 years / 4+ years) - Demographic+ Health Conditions - for outpatient visit: 0.88 (0.74 - 1.05) Education (< 4 years / 4+ years) - Demographic+ Health Conditions - for any hospitalization: 1.34 (1.08-1.65) |
| Education (< 4 years / 4+ years) - Demographic+ Health Conditions - for more than one hospitalization: 1.12 (0.73-1.72) Income (0 = low, 1 = high) - Demographic+ Health Conditions – for outpatient visit: 1.16 (1.01–1.34) Income (0 = low, 1 = high) - Demographic+ Health Conditions – for any hospitalization: 1.03 (0.89-1.20) Income (0 = low, 1 = high) - Demographic + Health Conditions - for more than one hospitalization: 1.01 (0.76-1.35) Employment (0 = No, 1 = Yes) - Demographic + Health Conditions - for outpatient visit: 0.72 (0.60-0.85) Employment (0 = No, 1 = Yes) - Demographic + Health Conditions - for any hospitalization: 0.84 (0.68-1.04) Employment (0 = No, 1 = Yes) - Demographic + Health Conditions - for more than one hospitalization: 0.66 (0.42-1.05) Private health insurance (0 = No, 1 = Yes) - Demographic + Health Conditions - for outpatient visit: 2.42 (2.11-2.77) Private health insurance (0 = No, 1 = Yes) - Demographic + Health Conditions - for any hospitalization: 1.18 (1.03-1.36) Private health insurance (0 = No, 1 = Yes) - Demographic + Health Conditions - for more than one hospitalization: 1.18 (0.91-1.52) |
|||||
| De-Guzman et al. 2014 | Philippine | Health Belief Model and Healthcare Utilization Model conjoint analysis (2012) |
Survey 304 |
64.14% | Quality of health care service - p < 0.05 Cost of health care services - p < 0.05 Extent of information received from health care provider - p < 0.05 A weak positive relationship was identified between private practice and educational attainment (r =.152) and income (r =.206) A weak negative correlation was noted in terms of preference to seek health care from a health center, (r =.173) |
| Heinrick et al 2008 | Germany | Cross-sectional study | Health economic interview Randomly selected 452 |
64.0% | Healthcare costs (95% CI 3203-4257) with no significant difference between sexes. This healthcare cost includes: Inpatient care cost - no significant difference identified between men and women Pharmaceuticals cost - p < 0.05 (p = 0.002) Cost for outpatient physician services - no significant difference identified between men and women Assisted living - p < 0.05 (p = 0.008) Medical supply and dentures - p < 0.05 (p = 0.019) |
| Outpatient non-physician services - p < 0.05 (p = 0.023) Transportation cost - no significant difference identified between men and women - significant (p value is not reported) |
|||||
| Iecovich and Carmel 2009 | Israel | Behavioral model (2006) | Face-to-face interviews Stratified sample 1255 |
56.8% | Economic difficulties in visiting specialists - p < .01 Mobility difficulties in visiting specialists - p < .001 Transportation difficulties in visiting specialists - p < .001 Education - significant (p value is not reported) |
| Odaman and Ibiezugbe 2014 | Nigeria | Behavioral model | Face to face interview Systematic random sampling 514 |
50.8% | Females have less financial responsibility than males for medical needs - significant (p value is not reported) Financial dependency increases on children with age (30.6% to 50.6% and 80.0% at ages 65-74 years, 75-84 years and 85+ years respectively) - (p value is not reported) |
| Ruthig et al. 2009 | USA | Cross sectional study | In-person interviews Systematic random sampling 6813 |
61% | Education - p < .001 Income - p < .001 Lack of health insurance - p < .001 Absence of regular care provider - p < .001 |
| Sharma, Mazta and Parashar 2013 | India | Cross-sectional study (2010-2011) | Interview Simple random sampling 400 |
25% | Perception that disease due to age (49.6% respondents reported it as a barrier) - p value is not reported Health services too far (19.1% respondents reported it as a barrier) - p value is not reported Use of over the counter drugs (12.5% respondents reported it as a barrier) - p value is not reported Trust god for healing (15.8% respondents reported it as a barrier) - p value is not reported Lack of money (6.0% v) - p value is not reported No body to take to hospital (3.5% respondents reported it as a barrier) - p value is not reported Poor attitude of healthcare workers (6.0% respondents reported it as a barrier) - p value is not reported |
| Sudore et al. 2006 | USA | Cross-sectional study (1999-2000) | An in-person clinic assessment of health literacy Random sampling 2512 |
52% | Limited health literacy - p < .01(OR 51.55; CI 51.03-2.34) Income - p < .001 Depression - p < .001 Lacking insurance for medications (OR51.73; CI 51.23-2.43) Shortage of doctors - p < .01 |
| Liu et al. 2007 | China | Cross sectional study (2006) | Standardized questionnaire Random sampling 550 |
45.8% | Women living alone had visited or telephoned a physician less than the women living with children - p < .05 Women living alone have lower income than women living with children - significant (p value is not reported) Cost (64% empty nesters reported it as a barrier) - p < .01 |
| Lack of coverage by the health plan (37% empty nesters reported it as a barrier) - p < .01 Inability to find someone to take the individual to the provider’s office (28% empty nesters reported it as a barrier) - p < .01 Lack of healthcare information (24% empty nesters reported it as a barrier) - significant (p value is not reported) Long waiting time for an appointment (24% empty nesters reported it as a barrier) - significant (p value is not reported) Bad experience with healthcare system (21% empty nesters reported it as a barrier) - significant (p value is not reported) Distance to healthcare centers (18% empty nesters reported it as a barrier) - significant (p value is not reported) Did not think visiting a doctor could help (18% empty nesters reported it as a barrier) - significant (p value is not reported) Could not contact a familiar physician (12% empty nesters reported it as a barrier) - significant (p value is not reported) |
|||||
| Borders 2004 | USA | Behavioral Model | Telephone survey 2,097 |
70.0% | Always see personal doctor/nurse - p < 0.05 Always see specialists - p < 0.001 Getting care after long waiting times (Always/usually see doctor/nurse as soon as want for routine care) - p < 0.05 Health insurance coverage - p < 0.05 Transportation difficulties - p < 0.001 |
| Hong et al. 2004 | USA | Cross sectional study | Interviewed by telephone Random digit dialing sampling 586 |
52% rural women, however, the number of elderly women were not specified | Health insurance coverage - p < 0.05 (p = 0.0001) Transportation - p < 0.05 (p = 0.02) |
| Nipun et al. 2015 | India | Cross sectional study (2013-2014) | Face-to- face interview Systematic random sampling 200 |
50% | Education - p < 0.05 (p = 0.0298) Socioeconomic status - p < 0.05 (p = 0.0409) Cannot afford (36% respondents reported it as a barrier) - significant (p value is not reported) Long waiting time (16% respondents reported it as a barrier) - significant (p value is not reported) Long distance (16% respondents reported it as a barrier) - significant (p value is not reported) |
3. RESULTS
Of the 38 studies, 19 were conducted in high income and 19 in middle/low income countries. Each study used varying research paradigms and designs and included; cross sectional research methods (n = 23), longitudinal research methods (n = 5), comparative descriptive methods (n = 2), an evaluation method (n = 1) and a survey method (n = 2). Other studies used different healthcare research processes from human ecology and behavioral approach. The data collection method in the studies was mostly via. interviews (n = 23) and surveys (n = 13) and one study was clinical assessment and another study used a combination of survey and interviews. Sample sizes across all of these studies ranged from 100 to 8387 participants. Synthesizing the evidence based on the SDoH model resulted in an identification of seven categories (see Table 2) and included the downstream SDoH category such as health literacy and education, passive healthcare seeking behaviour and lack of healthcare support, and also the upstream SDoH category comprising financial constraints, transportation difficulties, relationship matters and a culture of restriction as represented in the diagrammatic model seen in Fig. (2). The synthesized categories are described in detail in the following section.
| Domain | Specific factors | Total number of studies | References |
|---|---|---|---|
| Downstream SDoH | |||
| Health literacy and education | Lack of education | 19 | Yamasaki-Nakagawa et al. 2001; Xu and Borders 2003; Bell et al. 2005; Cheng et al. 2005; Masud et al. 2005; Sudore et al. 2006; Abdulraheem 2007; Blay et al. 2008; Mariolis et al. 2008; Iecovich and Carmel 2009; Ruthig et al. 2009; Jordan et al. 2011; Adu-Gyamfi and Abane 2013; Ameh et al. 2014; De-Guzman et al. 2014; Onwubiko et al. 2014; Weaver and Gjesfjeld 2014; Nipun et al. 2015 |
| Lack of knowledge about health and healthcare services | 3 | Pullen et al. 2001; Abdulraheem 2007; Ameh et al. 2014 | |
| Passive healthcare seeking behaviors | Do not think as sick enough | 6 | Cheng et al. 2005; Judd, Komiti and Jackson 2008; Ruthig et al. 2009; Gopalan and Durairaj 2012; Ameh et al. 2014; Onwubiko et al. 2014; Nipun et al. 2015 |
| Self-treatment tendency | 3 | Masud et al. 2005; Jordan et al. 2011; Weaver and Gjesfjeld 2014 | |
| Mistrust to MHS | 11 | Yamasaki-Nakagawa et al. 2001; Young et al. 2001; Xu and Borders 2003; Peltzer 2004; Byles et al. 2006; Liu et al. 2007; Huong et al. 2007; Gopichandran and Chetlapalli 2013; Sharma, Mazta and Parashar 2013; De-Guzman et al. 2014; Onwubiko et al. 2014 | |
| Depression | 5 | Ingold et al. 2000; Judd et al. 2006; Sudore et al. 2006; Judd, Komiti and Jackson 2008; Chan and Griffiths 2009 | |
| Perceived stigma | 3 | Judd, Komiti and Jackson 2008; Sharma, Mazta and Parashar 2013; Onwubiko et al. 2014 | |
| Lack of healthcare support | Limited healthcare services | 9 | Young et al. 2000; Xu and Borders 2003; Abdulraheem 2007; Heinrich et al. 2008; Mariolis et al. 2008; Chan and Griffiths 2009; Adu-Gyamfi and Abane 2013; Weaver and Gjesfjeld 2014; De-Guzman et al. 2014 |
| Inadequate healthcare professionals | 8 | Young et al. 2000; Borders 2004; Cheng et al. 2005; Sudore et al. 2006; Chan and Griffiths 2009; Ruthig et al. 2009; Adu-Gyamfi and Abane 2013; Ameh et al. 2014 | |
| Scarcity of medical equipment and medications | 5 | Cheng et al. 2005; Heinrich et al. 2008; Chan and Griffiths 2009; Adu-Gyamfi and Abane 2013; Ameh, Gomez-Olive et al. 2014 | |
| Long waiting times | 5 | Young et al. 2000; Borders 2004; Abdulraheem 2007; Liu et al. 2007; Nipun et al. 2015 | |
| Attitude of healthcare professionals | 4 | Peltzer 2004; Liu et al. 2007; Sharma, Mazta and Parashar 2013; Ameh et al. 2014 | |
| Health insurance coverage | 11 | Xu and Borders 2003; Borders 2004; Hong et al. 2004; Bell et al. 2005; Sudore et al. 2006; Liu et al. 2007; Blay et al. 2008; Ruthig et al. 2009; Adu-Gyamfi and Abane 2013; Ameh et al. 2014; Weaver and Gjesfjeld 2014 | |
| Upstream SDoH | |||
| Financial constraints | Poverty (Individual & household poverty) | 16 | Xu and Borders 2003; Melese et al. 2004; Bell et al. 2005; Cheng et al. 2005; Masud et al. 2005; Sudore et al. 2006; Abdulraheem 2007; Liu et al. 2007; Blay et al. 2008; Chan and Griffiths 2009; Iecovich and Carmel 2009; Ruthig et al. 2009; Gopalan and Durairaj 2012; Ameh et al. 2014; Weaver and Gjesfjeld 2014; Nipun et al. 2015 |
| Cost of treatments | 12 | Young et al. 2000; Young et al. 2001; Yamasaki-Nakagawa et al. 2001; Melese et al. 2004; Peltzer 2004; Bell et al. 2005; Byles et al. 2006; Liu et al. 2007; Heinrich et al. 2008; Onwubiko et al. 2014; De-Guzman et al. 2014; Nipun et al. 2015 | |
| Lack of financial support | 3 | Chan and Griffiths 2009; Gopalan and Durairaj 2012; Sharma, Mazta and Parashar 2013 | |
| Transportation difficulties | Distance and travel | 16 | Pullen et al. 2001; Young et al. 2001; Yamasaki-Nakagawa et al. 2001; Melese et al. 2004; Cheng et al. 2005; Harrison and Wardle 2005; Abdulraheem 2007; Huong et al. 2007; Liu et al. 2007; Mariolis et al. 2008; Chan and Griffiths 2009; Gopalan and Durairaj 2012; Adu-Gyamfi and Abane 2013; Sharma, Mazta and Parashar 2013; Onwubiko et al. 2014; Nipun et al. 2015 |
| Transportation | 7 | Borders 2004; Hong et al. 2004; Melese et al. 2004; Harrison and Wardle 2005; Iecovich and Carmel 2009; Adu-Gyamfi and Abane 2013; Ameh et al. 2014 | |
| Relationship matters | Living alone | 8 | Ingold et al. 2000; Melese et al. 2004; Abdulraheem 2007; Liu et al. 2007; Chan and Griffiths 2009; Adu-Gyamfi and Abane 2013; Sharma, Mazta and Parashar 2013; Onwubiko et al. 2014 |
| Decreased social networks | 3 | Liu et al. 2007; Chan and Griffiths 2009; Sharma, Mazta and Parashar 2013 | |
| A culture of restriction | Restriction in mobility | 5 | Ingold et al. 2000; Harrison and Wardle 2005; Huong et al. 2007; Liu et al. 2007; Iecovich and Carmel 2009 |
| Dependency on male family members | 3 | Ingold et al. 2000; Heinrich et al. 2008; Odaman and Ibiezugbe 2014 | |
3.1. Health Literacy and Education
The association of the health literacy of REW and their healthcare access was significant, which was closely related to a lack of general education and lack of knowledge about health and healthcare among REW [12, 13]. Nineteen studies found that schooling was a statistically significant determinant in REW’s access to MHS. The REW with formal education were more likely to visit MHS early and regularly than women with no formal education in low/middle and high income countries [14-18]. In contrast, education attainment showed a weak positive relationship with the utilization of MHS among Filipino elderly women (r = 0.152), while 66.78% had at least a high school level of education [19]. Differences in the level of education among the REW living in South Africa [six and more years of education had a twofold increased odds of using healthcare compared to those with no formal education: p < 0.05 (p = 0.001) (OR: 2.49; CI: 1.27 - 4.86)] and Israel [3% in the variability among the age groups] were identified as significant in using MHS [12, 18]. As such, education levels of REW was a strong indicator in access and utilisation of MHS.
Three studies indicated that the utilization of MHS by REW increased with the knowledge about health and healthcare services [12, 20]. Knowledge about health conditions and availability of MHS was a determinant for REW [0.6%] in MHS use in low/middle income countries like South Africa [12]. Less than one-third (28.7%) of the REW were aware of their health needs in Nigeria [14]. Pullen, Fiandt, & Walker (2001) also highlighted that there was a lack of information about the existing availability of MHS among REW, where healthcare practiners’ recommendations made significant contribution to regression equation [Beta weight - 69] in a high income country like USA, which impacted on visits to the healthcare centres and also influenced healthcare seeking behaviours.
3.2. Passive Healthcare Seeking Behavior
A significant relationship between passive healthcare seeking behavior of REW and healthcare access was identified in several studies, and these behaviors included: a feeling of not being ill enough, self-treatment tendencies, mistrust of modern healthcare services, depression and perceived stigma.
Six studies found that the reason women did not seek assistance from MHS for ailments was because the women did not consider their ailment sufficiently serious until they appeared as physical symptoms. In their view, they were not feeling unwell enough [12, 21-24]. Cheng et al. (2005) identified that 25% of REW living in China did not know whether their health problems were serious enough to visit a hospital. In Nigeria, 57% of REW indicated the non-seriousness of the ailment was a reason to not use a MHS [24]. Additionally, REW who did receive healthcare were less likely to use medication in a timely manner as prescribed [21, 22]. Studies by Onwubiko et al. (2014) and Nipun et al. (2015) established that the feeling of not being ill enough substantially increased the chances of REW’s reluctance to visit healthcare centers and use medications in two low income countries (i.e., Nigeria and India).
Three studies identified a significant relationship between self-treatment tendency and the utilization of MHS [25-27]. Jordan, Wilson, & Dobson (2011) indicated, in Australia, that only 48% REW received advice about diet, 20% about exercise and 10% having been advised to weigh them daily. This resulted in an interest in home remedies, traditional healers and over-the-counter medications for self-treatment rather than visiting hospitals, especially in low income country like Bangladesh [26]. The tendency of self-care was also statistically evident in USA [p < 0.05], however, not as significant as in low income countries like Nigeria [P < 0.05; OR: 1.7 (95% CI= 0.38-0.67] [14, 27]. This healthcare seeking behavior in combination with a mistrust of MHS had a negative impact on REW’s access to MHS.
Several studies demonstrated that mistrust was directly related with a decrease in the use of MHS [19, 24, 28-31]. Rural elderly women living in Australia who visited healthcare centers stated a lower satisfaction with GP, specialist or allied health professional than urban women and this was significantly associated [p < 0.01] with their access to MHS [28]. In India, REW most often visited healthcare professionals who were well-known to them and were perceived as having a simple approach and being culturally competent [6.0% reported as a barrier] [30]. Additionally, there was a positive belief among REW women about the use of spiritual healing in low/middle income countries such as Nigeria [20.2% reported as a barrier], South Africa [p < 0.001], and India [15.8% reported as a barrier] [24, 29, 30]. This lack of faith in doctors and nurses and the positive beliefs about spiritual healing led REW to visit traditional healers rather than MHS.
The mental health of REW also had an influence on healthcare access with those suffering from depression less likely to use MHS [32-36]. In Pakistan, depression of elderly women was also evident which contributed to not using MHS [p < 0.001], but this depression was related to natural calamity [32]. Living with depression increased a sense of helplessness for REW in seeking MHS even in high income countries such as Switzerland [p = 0.008 (OR 6.4, 95% CI 1.6 - 24.8] and Australia [P value is not reported] and in USA [p < .001] [33-35]. This state of depression resulted in REW not seeking MHS.
Three studies identified that perceived stigma was involved in access to MHS and this stigma is associated with having any illness impacted on the REW healthcare access to MHS in Nigeria [20.2% reported as a barrier] and India [49.6% reported as a barrier] [24, 30]. Discrimination of REW in the form of dominance and disempowerment contributed to perceive stigma in these low income countries. The REW who attributed stigma as a factor in not seeking healthcare at a MHS significantly related this stigma as being the reason for a lack of healthcare support.
3.3. Lack of Healthcare Support
The prevailing healthcare system played a statistically significant role in restricting REW’s use of MHS. Determinants identified in relation to MHS included limited care services, inadequate healthcare professionals, a scarcity of medical equipment and medications, long waiting times, poor attitudes of care workers and lack of health insurance coverage. Each of the determinants had an association with limited access for REW.
Studies showed that healthcare access was associated with the availability of services for REW and acknowledged the limitation of healthcare centres and services for REW [27, 31, 37, 38]. In contrast, only one quantitative study conducted in Nigeria reported that most REW [89.4%] received treatment with the availability of MHS for themselves [14]. Whilst two seperate studies conducted in a USA [p < 0.01] and Germany [p < 0.05 (p = 0.023)] reported a lack of pharmacies and outpatient non-physician services, studies conducted in low income countries confirmed that there were a small number of hospitals or clinics in rural areas of Nigeria [2.8% reported as a barrier] and Ghana [47.8% reported as a barrier] [14, 15, 31, 37]. Rural elderly women who lived near a rural care centre were more likely to access and receive adequate healthcare than the women without a close healthcare centre in both low/middle and high income countries [15, 32]. Healthcare services not being close by and a shortage of doctors and nurses in healthcare centres were identified in the studies as impacting negatively on healthcare access for REW.
Inadequate numbers of doctors and nurses in rural healthcare centers were attributed to the use of MHS [12, 21, 32, 38]. A shortage of healthcare professionals identified impacted on REW’s access to MHS in Nigeria [2.8% reported as barrier], Ghana [54.2% reported as a barrier] [14, 15]. Moreover, there was a reported significant shortage of specialist doctors and nurses in rural healthcare centers in the USA [p < 0.001 ] and they were rarely available in low income countries like Ghana [61.7% reported it as a barrier] and South Africa [3.4% reported as a barrier] [12, 15, 39]. As such, a shortage of healthcare professionals impacted on healthcare access for REW and this access was further hindered by the supply of medical equipment and medications.
A number of the studies identified an association between the lack of supply of medical equipment and medications and the use of MHS. Rural elderly women living in low income countries like Ghana [54.2% reported as a barrier] and South Africa [7.3% reported as a barrier] were less likely to use local healthcare services due to a lack of medical equipment and medications [12, 15]. Healthcare utilization was also impacted on by a poor supply of medications in rural healthcare centers in Germany [p < 0.05 (p = 0.019)] [15]. Living in rural areas of low income countries was positively affected by an inadequate supply of equipment and medications that in turn resulted in a poor utilization of MHS.
Association of waiting a long time to be seen and treated in care centers also affected the use of MHS. The experience of long waiting times impacted negatively on REW’s visits to local public healthcare centers in Nigeria [3% reported as a barrier], India [16% reported as a barrier], USA [p < 0.05] and China [24% empty nesters reported as a barrier] [14, 23, 39, 40]. No study found in both low income and high income countries that reported the the avarage waiting times in seeking care [23, 38, 39, 41].
The attitude of healthcare professionals had a negative and statistically significant effect on MHS use [12, 40]. Ameh et al. (2014) highlighted that the attitudes of doctors and nurses at first visit [6.7% empty nesters reported as a barrier] were significantly associated with the use of healthcare services in subsequent visits in South Africa. Rural elderly women expressed their dissatisfaction with the way they were treated by doctors and nurses in a number of low income countries including South Africa, China and India [29, 30, 40]. Experience of mistreatment included receiving no or little attention, as well as a perception of receiving incorrect medical treatment [30, 40]. This experience of mistreatment by REW was a negative factor impacting on subsequent access to healthcare centres.
Lack of healthcare insurance coverage was another important barrier in the use of MHS. Rural elderly women who had healthcare insurance were more likely to use healthcare than non-policy holders in low income countries such as Brazil [(outpatient: 2.42 (2.11–2.77); (any hospitalization: 1.18 (1.03-1.36) and more than one hospitalization: 1.18 (0.91-1.52)] and Ghana [75% of health insurance policy holders said they utilize care facilities as against 56.2% of non-policy holders] [15, 17]. Healthcare insurance also had a positive affect on improving access for REW living in the USA [p < 0.05 (p = 0.0001)] [31, 42]. However, Ameh et al. (2014) identified that a small number of REW, who received free consultations and medications under government schemes in South Africa, better utilised MHS. Only three studies assessed the effect of health insurance on REW’s MHS use in low income countries [12, 15, 22]. Those REW with healthcare insurance were more likely to access MHS and access was also influenced by free healthcare and the financial resources available to them.
3.4. Financial Constraints
Most studies indicated a statistically significant association between financial constraints and REW’s healthcare access. The economic factors identified included levels of poverty, the cost of treatments and a lack of finances whether personal, from the family or the government. The impact of each of these determinants negatively affected healthcare access for REW.
The association between poverty and access to MHS was identified as one of the most important SDoH in the non-use of MHS and included individual poverty and household poverty [14, 16, 17, 21]. Elderly women who had no or low incomes and personal savings were less likely to use healthcare from MHS in rural Bangladesh [p < 0.05 (OR 0.75; CI 0.60 - 0.95)] and in India [p < 0.05 (OR 2.00, 95% CI 0.84-4.80)] [26]. There was no difference identified between low/middle and high income countries in relation to the impact of personal income on healthcare use, which was also determined by the household’s economic status [12, 16, 21, 23]. The higher the household economic status meant the more positive and statistically significant impact on the adequate use of MHS in Nigeria [OR: 0.46 (0.38 - 0.67)] and India [p < 0.05 (p = 0.0409)] [14, 23, 26]. Poverty was also statistically significant in meeting the costs of medical treatments and this led to less health seeking and a low use of MHS.
Some studies indicated an association of the costs of seeking treatments (i.e. transportation, fees for physicians, laboratory tests and medications) with MHS use. For example, REW who sought healthcare were restricted in using MHS regularly because of the high cost of treatments [24, 28, 43]. In contrast, free and/or subsidized healthcare support enhanced the utilization of MHS in Nepal, which more men received free care than women [(56% of men, 35% of women, P= 0.073)] [43]. This subsidized healthcare support was also evident in Australia that contributed to the increase of the rate of MHS utilization among REW [38, 44]. A low economic capacity influenced REW seeking healthcare and was identified as due to a lack of financial support from family members and the governments.
Three studies found that REW who perceived they had adequate support from family members and the government were more likely to use MHS [22, 30, 32]. Disinterest of younger family members in spending money on elderly women in the family also resulted in REW reduced use of MHS in India [p < 0.05 (OR 2.04, 95% CI 1.09-3.83)] and Pakistan [p < 0.001] [22, 32]. Furthermore, REW who did not receive financial support from the government in India were less likely to use MHS than elderly women who had such support [p < 0.05 (OR 2.13, 95% CI 1.11-4.07)] [22]. Living in a low income country was statistically associated with a lack of financial support from both the family and the government, and this significantly impacted on their access.
3.5. Transportation Difficulties
Access to MHS was affected by geographical accessibility factors including distances, travelling and transportation [18, 21, 23, 32, 44, 45]. A long distance to healthcare centers reduced the number of regular visits for REW in both low/middle and high income countries [14, 15, 44, 46]. Long distances caused increased travel time and led REW to fewer visits to healthcare centers in Ghana [p < 0.05 (p = 0.021)], India [28.4% reported as a barrier] and Vietnam [p < 0.05] [15, 22, 47]. Several studies reported an association of inconvenient transportation with the non-use of MHS and this inconvenience was related to the unavailability in low/middle income countries like South Africa [1.1% reported it as a barrier] and Ghana [p < 0.05 (p = 0.001)] and also discomfort in using transportation in USA [p < 0.05 (p = 0.02)] [12, 15, 42]. Consequently, the distance and travel time in combination with an inadequate transportation system were significant barriers [32, 40]. Thus, living in rural areas was positively associated with the problems of transportation that impacted on visits to healthcare centers. Being reliant on family members for transportation and access to MHS made family relationships another important factor for REW accessing healthcare.
3.6. Relationship Matters
A reliance on social and family relationships had a statistically significant impact on REW’s access to MHS with poor quality relationships negatively influencing the access [30, 33, 48]. Chan & Griffths (2009) and Onwubiko et al. (2014) found that REW who had a feeling of social loneliness were less likely to use MHS in Pakistan [p < 0.01] and Nigeria [p = 0.01 (OR 2.26; CI 1.41-3.63)]. Isolation from intimate relationships increased the chances of vulnerability and an unwillingness to utilize medical treatments as REW often needed someone to help them in travelling and seeking healthcare [24]. Three studies also indicated a relationship between healthcare access and social networks [30, 32, 40]. Liu et al. (2007) reported that decreasing social networks also led REW to use medical treatments in an inappropriate way in China [p < .05]. Dependency of REW on their friends, family and neighbors in seeking healthcare was compounded when they were more likely to lose their friends as they aged that then resulted in less access.
3.7. Culture of Restriction
The cultural determinants included family restrictions on mobility and or a dependency on male family members. Being an aged woman, resulted in limited autonomy to travel alone to healthcare centers in both Switzerland [p < 0.05 (p = 0.003)] and Vietnam [p < 0.005 ] [33, 47]. Though the causes were not clear, this restriction in movement impacted on the use of MHS, and in some countries was also influenced by being dependent on male family members. Three studies indicated that REW were dependent on family members, male family members in particular, in relation to receiving in-home help, accompaniment in travelling to the healthcare centers and in managing healthcare [33, 37, 49]. Rural elderly women who were mostly dependent on family members were less likely to use MHS in Switzerland [p < 0.05 (p = 0.031)] and in Germany [p < 0.05 (p = 0.008)] [33, 37]. Additionally, refusal from family members to help the REW was an important factor for the non-utilization [49]. Such dependent circumstances for REW did not improve their healthcare access in these communities both in developing and developed countries.
In summarizing the findings, the review suggested a number of determinants in relation to REW’s access to MHS. It was evident that REW were disadvantaged by individual, institutional, economic, social and cultural determinants under seven categories described above. This review confirmed that not only did healthcare systems impact on outcomes, but also individual, socioeconomic and cultural barriers influenced REW’s access. These constraints in healthcare and social environments shaped REW’s personal healthcare seeking behaviors. Thus, individual circumstances in combination with healthcare, cultural and social environments and reliance on others were significant determinants in the utilization of MHS for REW.
4. DISCUSSION
This review identified a number of statistically significant SDoH of REW’s access to MHS. Although these determinants were country and context specific, they can be seen in an integrated manner with common factors impacting on healthcare access. The use of MHS is mainly mediated by personal, socioeconomic, cultural and health systems that shape the way REW perceive their health and healthcare access. Personal healthcare seeking behaviors and cultural issues in low/middle income countries may or may not be similar in high income countries, however, they are significant in understanding the overall status of REW’s access to MHS globally. The authenticity and consistency across the findings in the reviewed studies have led to conclusions on the SDoH including downstream and upstream SDoH that impact on REW’s access.
Downstream SDoH spatially and provisionally influence REW’s access to MHS [50]. As such, this review found a number of downstream determinants that are grouped into three categories: health literacy and education, care seeking behavior and lack healthcare support. Regardless the country difference, health illiteracy and educational levels emerged as the most dominant determinant in MHS use. Because of higher education rate in high income countries, REW are more likely to have better healthcare knowledge leading to an increased realization of the benefits of MHS use [51-53]. In contrast, REW living in low/middle income countries experience more drop out from the school in their early life than male children [26, 53]. This lack of education is the result of social positioning of women in the rural society, and this could be a reason of the REW’s increased dependency and lack of confidence in making decisions regarding healthcare access [41, 53, 54]. Interventions aimed at maximizing health literacy of REW may increase their hospital visits, and also improve their health seeking behaviors in accessing MHS.
Passive behaviors were identified as important determinants in this review, especially for REW living in low/middle income countries. The passive behaviors included self-care tendencies, their mistrust of MHS and staff, whether depression was present and any perceived stigma. While the seriousness in seeking healthcare, mistrust to MHS, stigma and self-care tendencies were common in the REW living low/middle income countries, REW who live in high income countries presented their depression. Studies examining the passive behaviors reported on the coping strategies employed by REW, rather than on the REW’s autonomy and recognition within healthcare system, especially in low income countries [41, 55, 56]. Taking universal healthcare seriously did not confirm the consideration of individual determinants such as self-care tendencies and trust on MHS at policy and research levels in low income countries [56-58]. Such determinants could be demotivating factors in the cultures where dominance and disempowerment are prevalent [59]. The impact of these determinants in using MHS is furthered when considering the life-long depression and perceived stigma among REW [60, 61]. Thus, the individual circumstances in using MHS require attention, together with the systemic, economic and social circumstances.
Healthcare support was a key downstream determinant in MHS utilization. This review identified a range of scarcities including lack of services, healthcare professionals and medical equipment and medications. Lack of services and shortage of healthcare professionals were important even in high income countries as REW live away from mainstream populations [16, 62]. Rural elderly women with comorbidities and/or chronic conditions may find it difficult to use MHS especially when resources are limited, and lengthy waiting periods in healthcare centers can make this situation worse [56]. Though there was no evidence between low/middle and high income countries relating to the difference in average waiting time, this lengthy waiting period demotivated REW in low income countries because of their chronic health condition, dependency in managing healthcare and limited healthcare professionals [5]. The attitude of healthcare professionals towards REW was cited as a significant determinant in low/middle income countries and it was clear that the relationships between REW and healthcare professionals impacted on MHS use [41, 58]. The cultural competent approach of the healthcare professionals may contribute to the increase of the number of visits of REW at hospitals. Even though health insurance coverage had a positive effect on MHS use, there was a lack of focus on this issue in low/middle income countries [41, 55]. Accordingly, the role played by staff in MHS in REW’s healthcare access was of particular interest. These downstream determinants were further shaped by a number of upstream determinants.
The fundamental factors impacting on access can be defined as upstream determinants [50]. This review identified a number of fundamental determinants grouped into four themes including financial constraints, transportation difficulties, relationship matters and cultural restrictions. Financial constraint was a result of poverty, the cost of services and a lack of support from family members and the state and this has been supported by other reports [54]. Poverty and the cost of services were important for REW seeking healthcare or not, especially where there was no or limited support from family members or the government in low/middle income countries [63]. Possessing savings from employment and having support from the governments in high income countries encouraged the people including REW to access healthcare [64]. However, the financial constraints of REW were reinforced in low income countries where local cultural values and customs denied employment for REW and make independent decisions in seeking MHS [64-66]. Other studies have also found rural households with low financial security had less access
to social resources such as education and healthcare, and this was especially true for REW in low income countries because of their low income and savings and an economic dependency on family members.
Transportation difficulties were also central concerns in MHS use in the forms of distance, travel time and convenience. Living at a distance from healthcare centers demotivated REW to access MHS as it involved time, money, transportation and accompaniment [67, 68]. While high income countries like USA, UK, Canada and Australia progressed in ensuring universal healthcare access for rural people including REW, the main focus of low/middle income countries was on urban infrastructures including education, employment, healthcare and transportation [68]. As a result, transportation emerged as an important determinant in low/middle income countries in accessing socioeconomic and healthcare resources. Apart from the debate about the location and the use of MHS, most studies found REW have less access due to transportation difficulties [68, 69]. Living far away has been associated with REW’s low level of education and a poor access to MHS resulting in mistrust to MHS and a dependency on home-remedies and traditional healers [63, 68]. Rural elderly women living in poor households in low income countries where family members failed to recognize and meet the needs of the women in relation to manage time and accompany them to MHS use [41]. Especially, REW with a disability may find it difficult to travel to healthcare services especially when the transportation was not available and no accompany [52]. In general, the issue of distance and transportation along with social exclusion was vital determinant in using MHS, especially in low/middle income countries.
Social relationship was another major upstream determinant in the utilization of MHS. Though social exclusion of REW was common in developed and developing countries, the causes were different. In high income countries, poor social networks decreased the number of visits to MHS and also reduced the chance of getting information from others [70, 71]. In low/middle income countries, most REW were living with family members and their low status in the patriarchal family structure caused isolation in the family leading to diminished use of MHS [71]. This social isolation as a result of patriarchy plays a role in shaping the healthcare beliefs and behaviors such as superstitions, understanding of the importance of using MHS, self-care, feeling of loneliness and home-centeredness [8].
Cultural value was significant upstream determinant in MHS use. Though there was a lack of focus in quantitative studies conducted in low/middle and high income countries about the cultural obstacles, underutilization of MHS as a result of REW’s lack autonomy in moving out alone and travelling to healthcare centers was evident. Male dominance in the cultures of low income countries may have influenced a woman’s decision to use MHS [8, 72]. Rural elderly women living in a patriarchal context were less likely to use MHS because of a restriction in movement [73]. Moreover, the control of monetary issues by men can make it difficult for REW to independently pay for transportation [73]. Thus, experience of inequality by REW compared to men in low income societies has direct effects on their MHS use and this should be explored further [74, 75].
Overall, this study highlighted the complex downstream and upstream ways in which REW’s healthcare access affect. The downstream SDoH including health literacy and education, passive health seeking behavior and a lack of healthcare support had direct influence on the REW’s access to MHS. And the upstream SDoH such as financial constraints, transportation difficulties, relationship matters and cultural restrictions shaped the healthcare behaviors of the REW and an inequality in their access to education and resources. Because of the interrelationships, there is requirement for a holistic policy and practice for healthcare system based on the understanding of the SDoH. Construction of the determinants suggests the healthcare practice to be more inclusionary and comprehensive that can able to provide institutionalized, complete and sustainable care rather than disease centered care. Interventions at policy level should focus on different determinants at once to ensure the women’s recognition and their adequate and equal access to MHS. Low/middle income countries can follow the high income country’s policies and practices in developing healthcare and social policies and practice guidelines considering the local socioeconomic and cultural vulnerability of the REW in accessing MHS.
The review has several limitations as it was limited to peer-reviewed quantitative articles. A review of qualitative studies would add to the body of knowledge regarding REW access to healthcare. The decision to reject book chapters, grey literature and non-English language studies was made because of practical reasons including the complexity of synthesis and analysis and time constraints. There is a need to consider that research conducted in low income countries may not be published in peer-reviewed journals which may have impacted in identifying the determinants across the quantitative studies reviewed.
CONCLUSION
This review raised a number of practical and research issues in relation to MHS access and use by REW. Low utilization of MHS by REW was often caused by several downstream and upstream determinants. Adequate and quality access to MHS for REW that is respectful of the woman is not assured, particularly in low and middle income countries. The common and different issues identified across low/middle and high income countries suggest that access to MHS by REW was a global health priority. This review on the SDoH of REW’s healthcare access has substantial importance in the development of relevant policies and practices. At the policy level, increasing the REW’s participation in health education and ensuring adequate financial assistance and transportation will improve access, and sustainable healthcare and social support could bring a positive change in using MHS. At practice level, consideration of the SDoH may be helpful for developing an institutionalized and sustainable care management for the REW. Further research is recommended into REW’s experiences and perceptions in relation to the impact of cultural determinants on MHS use.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


