RESEARCH ARTICLE
Initial Clinical Presentation of Cervical Cancer Patients at Pietersburg Hospital, South Africa (2012-2014): A Retrospective Descriptive Study
Edna Maite Mohuba1, Tebogo Maria Mothiba2, *, Livhuwani Muthelo3
Article Information
Identifiers and Pagination:
Year: 2019Volume: 12
First Page: 238
Last Page: 246
Publisher ID: TOPHJ-12-238
DOI: 10.2174/1874944501912010238
Article History:
Received Date: 17/03/2019Revision Received Date: 30/04/2019
Acceptance Date: 05/05/2019
Electronic publication date: 31/05/2019
Collection year: 2019

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Cervical cancer, compared to other types of cancers, is a leading cause of death for women; and is a serious public health problem in both developed and developing countries.
Objective:
The aim of the study was to determine the initial clinical presentation of cervical cancer patients at the Pietersburg Hospital, Limpopo Province in South Africa.
Methods:
This was a quantitative, retrospective study conducted to examine the records of cervical cancer patients from January 2012 to December 2014 at the Pietersburg hospital.
Results:
The results indicated that most patients, particularly the elderly, presented for the first time at the hospital with advanced stages of cervical cancer. Factors, such as age and place of residence contributed to late presentation. Most patients with advanced stage cervical cancer were from Sekhukhune and Vhembe Districts.
Conclusion:
There is a need for improved data capturing of information about marital status and parity to further assess the influence these variables might have on the clinical presentation of cervical cancer. Furthermore, availability and facilities for screening should be improved because early detection of cervical cancer prevents progression to advanced stage of the disease. More awareness campaigns about risk factors of cervical cancer should be implemented.
1. INTRODUCTION
Cervical cancer is a serious public health problem in both developed and developing countries which is caused by the HPV viral infection with the risk factor of multiple sexual partners and chronic infection [1]. Cervical cancer is the fourth most frequently diagnosed cancer and the fourth leading cause of cancer-related death, with an estimated 527,600 cases and 265,700 deaths worldwide in 2012 [2]. Furthermore, it is estimated that annually 85% of these deaths from cervical cancer occur in low- and middle-income countries [3]. According to de Sanjose et al. [4] it has been estimated that approximately 291 million women, or 10.4% of the population worldwide, have a cervical HPV infection at any given time. Age may have also played a role.
Cervical cancer is considered nearly completely preven-table because of the generally slow progression of the disease and the availability of screening and the HPV vaccination. Numerous prevention and early detection interventions were proven to avert cancer cases and deaths in both high- and low-resource settings [2]. Recent developments have introduced a new nonavalent HPV vaccine. A study on the impact of the nonavalent vaccine by Petersen, Restrepo Moreira et al. [5] revealed greater immunogenecity in girls and boys versus young women indicating that the anti-HPV responses generated by the nonavalent vaccine in adolescence were sufficient to induce high-level protective efficacy. The WHO recommends targeting girls ages 9 to 13 years for priority receipt of the HPV vaccine [6]. In the USA, Gardasil 9 has been approved by the FDA for women and men up to 45 years of age. This broader coverage may be challenging for developing countries. Even with improvements in coverage among adolescent girls, there are still 2 to 3 generations of women whose age precludes vaccination, including those who have already acquired the infection [7]. Screening is the principal preventive measure to reduce the burden of cervical cancer amongst women. In South Africa, pap smear screening test is recommended for cervical abnormalities, starting between the ages of 20 and 30 and in cycles of 3 – 5 years [8]. Nevertheless, there are some challenges encountered with the implementation of the pap smear test in low- and middle-income countries because of logistical obstacles in health systems and infrastructure [9].
Cervical cancer rates have increased in Uganda, Zimbabwe, and some countries of Central and Eastern Europe, as well as among younger women in many countries of Europe, Japan, and China, likely due to increased HPV prevalence associated with changing sexual practices in combination with inadequate screening; trends in factors contributing to progression of high-risk HPV infections, such as smoking, HIV, and oral contraceptive use, might have also played a role [10-13].
In South Africa, cervical cancer is the second most common cancer amongst women. The statistics indicate that 1 in 26 South African women will get it [14]. Cervical cancer screening guidelines are available in South Africa, which state that every woman attending public health facilities is entitled to three free Pap smears from the age of 30 years at intervals of ten years provided no smears have been taken within the previous five years [8]. However, the uptake for cervical cancer screening remains very low based on these guidelines [15]. South African data about the incidence of cancer of the cervix had been unavailable until 1999 when the Cancer Registry was established. According to South African Health Review 2013/2014 [16] the following factors are exacerbating cervical cancer incidence in South Africa which are: Absence of national cervical screening programmes for early detection and diagnosis, lack of treatment, lack of trained healthcare personnel, limited financial resources, lack of health promotion and prevention programmes, competition for limited resources and over-burdened health system.
Currently, in SA access for treatment of cervical abnormalities is very limited in the government healthcare sector. Additionally, often treatment requires the woman to travel to a referral hospital which maybe many kilometres away and she may need to wait up to 6 - 9 months for treatment. This combination often results in women being lost in the system and not getting the care they need to prevent the progression of their cervical abnormalities to cancer [14].
The current study was conducted at Pietersburg Hospital which is a referral hospital in the Limpopo Province that receives many patients, including patients suffering from different types of cancer. Most of the cancer patients, especially the ones with cervical cancer, come for treatment very late, when the cancer is already at an advanced stage. According to 2012 monthly statistics at the Oncology Department at Pietersburg Hospital 70% and 10% of cervical cancer patients present with stage III and IV, respectively. Early diagnosis, referral, and treatment of cervical cancer are of greater importance than any attempts to treat the disease in its late stages. However, at this rural tertiary hospital, the extent and nature of stage at presentation remain unknown. Therefore, this study sought to examine the correlates of initial clinical presentation of cervical cancer patients at the Pietersburg Hospital, Limpopo province, South Africa.
2. MATERIALS AND METHODS
2.1. Study Design
The quantitative retrospective cross-sectional survey was conducted to establish the stage of cervical cancer at the initial clinical presentation of patients at the Pietersburg Hospital in South Africa. The retrospective cross-sectional survey was conducted by checking the consultation records of cervical cancer patients for a period of three years from January 2012 to December 2014.
2.2. Study Site
The study was conducted in Pietersburg Hospital which is a referral hospital in the Limpopo Province that receives many patients, including patients suffering from different types of cancer. The Pietersburg Provincial Hospital, amongst other things, provides specialised care in oncology.
2.3. Population and Sampling
The records of all first time cervical cancer patients at the Oncology Unit of the Pietersburg Hospital from January 2012 to December 2014 were examined. There was an existing total of number of 938 patients presented for the first time between January 2012 and December 2014. A total of 273 records were systematically sampled by selecting every third patient record. This sample was calculated by using the Krejcie and Morgan formula for determining the sample size for research activities [17]. The calculation of the sample size of this study was:
S = 3.841 x 938 x 0.5(1 - 0.5) ÷ (0.05)2(938 - 1) + 3,841 x 0.5(1 - 0.5)
S = 900.7145 ÷ 3.30275
S = 272.7 (rounded up to 273).
2.4. Data Collection
The electronic files in the oncology unit were used to identify the records of patients who for the first time presented with cervical cancer problems at the Pietersburg Hospital between January 2012 and December 2014. The extended period of three years made it easier to determine trends. Demographic variables such as age, race, place of residence, parity, marital status, diagnosis, and initial stage of cancer presentation were extracted from the patients’ records by using a data collection tool.
2.5. Data Analysis
The three objectives of the study were to:
- Establish the demographic profile of cervical cancer patients at the initial clinical presentation at the Pietersburg Hospital;
- Identify the stage at initial presentation of cervical cancer at the Pietersburg Hospital; and
- Describe the factors that lead to the initial clinical presentation of cervical cancer patients at the Pietersburg Hospital in South Africa.
Data were analysed using the Epi Info statistical software. Data were interpreted in the format of frequencies and percentages. The Chi-square test was used to determine the association between variables. Comparison between groups (i.e. stage at presentation) was done by taking the t-test calculations into account for two groups and/or ANOVA for three or more groups. P-values of less than 0.05 were considered to be statistically significant.
2.6. Reliability and Validity
A pilot study to evaluate the data collection tool before the actual data collection of the main study was conducted. The pilot study also helped to determine whether the data collection tool was suited for accessing the patient files. Ten files were selected for the pilot study from the Oncology Unit at the Pietersburg Hospital; and the files did not form part of the main study. This approach helped the researcher to restructure the data collection tool in preparation for the main study.
3. RESULTS
3.1. Demographic Profile of the Patients
A total of 273 of cervical cancer patients’ records were studied. Table 1 presents the demographic profile of the patients. The mean age of the patients was 56.3 years (SD = 13.7), the youngest patient was 25 years old and the eldest 89 years. Sixty-six percent of the women were 50 years and older, 32% were younger than 50 years, while 2% of the women’s ages were unspecified. That indicated that the women aged 50 years and older were presenting late with initial presentation of cervical cancer. The results also indicated that many of the women were younger than 50 years old. The mean age of the patients that presented with FIGO stage III cervical cancer was 56.9 years and for the patients that presented with FIGO stage IV was 62.5 years. That concurred with the study in Sudan that has found that nearly 46% of advanced cervical cancer cases (FIGO stages III and IV) were older than 55 years [18].
The regions of residence of the women whose files were reviewed and are also see Table 1. A greater proportion of the cases (25%) were from the Capricorn district, 24% from the Vhembe district, 22% from the Mopani district, 17% from the Sekhukhune district, and 12% were from the Waterberg district. Table 1 also shows the hospitals in the Limpopo Province where the patients were initially assessed before being referred to Pietersburg hospital for diagnosis, as well as the distribution per hospital. The hospitals that the patients were referred from represented the place of residence. Therefore, the results indicate that most patients with initial presentation of cervical cancer who are admitted at the Pietersburg Hospital are residing in the district where the hospital is situated.
3.2. Stage at Initial Presentation of the Cervical Cancer Patients
The FIGO stages at initial presentation are shown in Table 1. Almost two-thirds (62.2%) of the patients were at stage III at initial presentation followed by 27.8% at stage II, 7.3% at stage IV, and only 1.8% at stage I. The stage of cervical cancer was unspecified for 0.7% of the patients. Furthermore, Table 2 presents the detailed description of the stages at presentation. Stage II was dominated by IIB, while IIIB was the commonest in stage III. In stage IV, the most dominant stage was IVA. Therefore, the results revealed that most of the patients who at initial presentation of cervical cancer were on stage III. A study about factors associated with diagnosis of cervical cancer in Nepal has found that 80.9% of the patients have a late stage diagnosis (stage ≥ IIB) [19].
| Demographic Variables | Frequency | Percentage |
|---|---|---|
| Age (years) | ||
| 20-29 | 6 | 2.2 |
| 30-39 | 23 | 8.4 |
| 40-49 | 58 | 21.2 |
| 50-59 | 75 | 27.5 |
| 60-69 | 54 | 19.8 |
| 70-79 | 40 | 14.7 |
| Above 80 | 12 | 4.4 |
| Unspecified | 5 | 1.8 |
| Place of residence (District) | ||
| Waterberg | 33 | 12 |
| Capricorn | 69 | 25 |
| Vhembe | 66 | 24 |
| Mopani | 60 | 22 |
| Sekhukhune | 45 | 17 |
| Hospitals of initial assessment | ||
| Belabela | 6 | 2.2 |
| Botlokwa | 3 | 1.1 |
| Dilokong | 6 | 2.2 |
| Donald Fraser | 7 | 2.6 |
| Dr C. N. Phatudi | 5 | 1.8 |
| Elim | 15 | 5.5 |
| Ellisras | 5 | 1.8 |
| F. H. Odendaal | 2 | 0.7 |
| George Masebe | 1 | 0.4 |
| Groblersdal | 2 | 0.7 |
| Helena Franz | 9 | 3.3 |
| Jane Furse | 4 | 1.5 |
| Kgapane | 6 | 2.2 |
| Lebowakgomo | 12 | 4.4 |
| Lephalale | 1 | 0.4 |
| Letaba | 26 | 9.5 |
| Louis Trichardt Memorial | 2 | 0.7 |
| Malamulele | 12 | 4.4 |
| Mankweng | 18 | 6.6 |
| Maphutha L Malatji | 5 | 1.8 |
| Matlala | 5 | 1.8 |
| Mecklenburg | 8 | 2.9 |
| Mokopane | 13 | 4.8 |
| Musina | 4 | 1.5 |
| Nkhensani | 8 | 2.9 |
| Philadelphia | 8 | 2.9 |
| Pietersburg | 7 | 2.6 |
| Sekororo | 7 | 2.6 |
| Seshego | 8 | 2.9 |
| Siloam | 11 | 4.0 |
| St. Ritas | 12 | 4.4 |
| Tshilidzini | 15 | 5.5 |
| Van Velden | 3 | 1.1 |
| Voortrekker | 4 | 1.5 |
| W. F. Knobel | 8 | 2.9 |
| Witpoort | 1 | .4 |
| Zebediela | 4 | 1.5 |
| FIGO stage at presentation | ||
| I | 5 | 1.8 |
| II | 76 | 27.8 |
| III | 170 | 62.2 |
| IV | 20 | 7.3 |
| Stages | Frequency | Percentage |
|---|---|---|
| Unknown | 2 | 0.7 |
| IA2 | 1 | 0.4 |
| IB | 2 | 0.7 |
| IB1 | 1 | 0.4 |
| IB2 | 1 | 0.4 |
| IIA | 14 | 5.1 |
| IIB | 61 | 22.3 |
| IIB2 | 1 | 0.4 |
| IIIA | 32 | 11.7 |
| IIIB | 95 | 34.8 |
| IIIB1 | 16 | 5.9 |
| IIIB2 | 27 | 9.9 |
| IVA | 15 | 5.5 |
| IVB | 5 | 1.8 |
| Total unspecified | 2 | 0.7 |
| Total I | 5 | 1.8 |
| Total II | 76 | 27.8 |
| Total III | 170 | 62.2 |
| Total IV | 20 | 7.3 |
| Stage | Description |
|---|---|
| 0 | Carcinoma in situ, intraepithelial neoplasia. |
| I | Carcinoma confined to the cervix. |
| Ia | Pre-clinical carcinoma that is diagnosed only by microscopy. |
| Ia1 | Stromal invasion no deeper than 3 mm and no wider than 7 mm in extension (so-called micro invasive carcinoma). |
| Ia2 | Maximum depth of invasion of stroma deeper than 3 mm and no deeper than 5 mm taken from the base of the epithelium; horizontal invasion not more than 7 mm. |
| Ib | Histologically invasive carcinoma confined to the cervix and greater than stage Ia2. |
| Ib1/2 | Tumour is clinically visible and greater than 4 cm. |
| IIa | Carcinoma extends beyond the cervix but not onto the pelvic wall. Carcinoma involves the vagina but not the lower third. |
| IIa1/2 | Tumour is clinically visible and greater than 4 cm. |
| III | Carcinoma has extended onto the pelvic wall. On rectal examination, there is no cancer-free space between the tumour and the pelvic wall. The tumour involves the lower third of the vagina. |
| IIIa | Tumour involves the lower third of the vagina with no extension to the pelvic side wall. |
| IIIb | Extension to the pelvic side wall or causing obstructive uropathy. |
| IV | Carcinoma has extended beyond the true pelvis or has clinically involved the mucosa of the bladder or rectum. This stage also includes cancers with metastatic dissemination that is spread to other organs. |
| Iva | Extension beyond pelvis or rectal/bladder invasion. |
| IVb | Distant organ spread. |
The clinical staging system for cervical cancer remains one of the key principal recommendations by the international Federation of Gynecology and Obstetrics (FIGO). Despite the known limitations (such as accuracy) of these recommen-dations with this system in comparison with pathological and surgical data, this system addresses fundamental parameters [20]. Testa et al. [20] indicate that the FIGO classification includes important parameters; such as distant metastases, tumour diameter, vaginal spread, parame- trial involvement, infiltration of rectum mucosa or bladder wall, hydronephrosis, and hydoureter. Kumar, Abbas, Fausto and Aster [21] support Testa, Di Legge, De Blasis et al. [20] when they describe the stages of cervical cancer according to the FIGO classification (Table 3 and Fig. 1). Thus, Fig. 1 and Table 3 outline a more detailed reflection of the parameters (spread of cancer cells and affected organs) at the different stages that the patients presented with initially at Pietersburg hospital.
3.3. Risk Factors that Lead to Late Presentation
3.3.1. Age
Table 4 presents the relationship between the stage of cervical cancer at presentation and the age of the patients. There was no statistical association between the stage of cervical cancer at presentation and age (p > 0.05); however, the FIGO stage at presentation increased in relation to the age of the patients. The mean age of the patients who presented with FIGO stage III cervical cancer was 56.9 years and for the patients who presented with FIGO stage IV, it was 62.5 years. This finding concurs with a study in Sudan which has found that nearly 46% of advanced (FIGO stages III and IV) cervical cancer cases were older than 55 years [18].
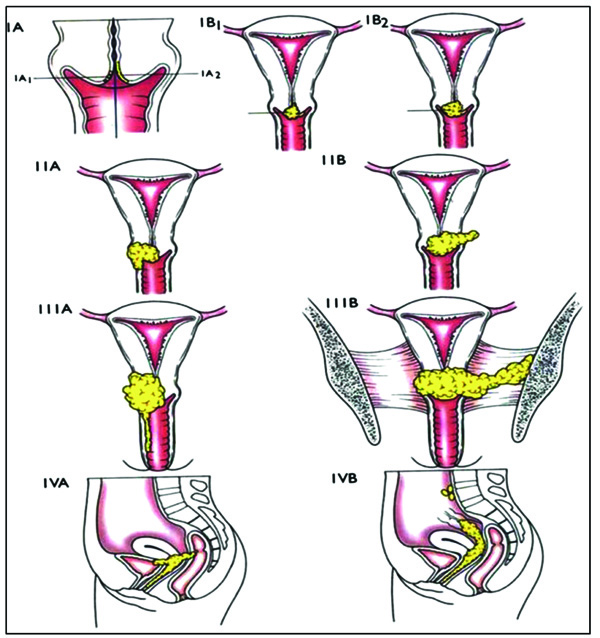 |
Fig. (1). Reflection of FIGO stages of cervical cancer [20]. |
| FIGO Stage | N | Mean ± SD | p-value |
|---|---|---|---|
| I | 5 | 52.4±16.2 | |
| II | 75 | 53.6±12.7 | |
| III | 165 | 56.9±14.1 | 0.0931 |
| IV | 21 | 62.5±11.3 |
According to Ibrahim et al. [18] older women are less often diagnosed at an early stage of cervical cancer due to the lack of seeking obstetric and gynaecological services during their post-menopausal years. This normally happens with women in rural areas where health care services are not readily accessible. Another factor might be a lack of awareness about cervical cancer and screening services that are available. In another study about the screening history, presentation, diagnosis, pathway, treatment and outcomes of patients diagnosed with cervical cancer in Ireland, have found that the most patients (74%) who present with stage I cervical cancer are between the ages of 25 and 49 years and their survival rate was 100% [22]. A large number of older patients (41.7%) who are 70 years and older present with stage IV cervical cancer and their survival rate is 30%. Their conclusion indicates that of the older patients, 92% have no record of a Pap smear compared to only 14% of the younger women. Thus, patients with a history of Pap smear tests present earlier.
3.3.2. Place of Residence
The relationship between the FIGO stage at initial presentation and place of residence is shown in Table 5. A greater proportion of the patients from the Sekhukhune and Vhembe districts were at stage III and IV compared to other districts (p > 0.05). However, no statistical significant associated was observed between the stage of cervical cancer at the initial presentation and place of residence. These results might be influenced by the fact that the two districts (Sekhukhune and Vhembe) are more rural and less developed than the other three; accessibility to health care services in these two districts might be limited. This concurs with a study of predictors of cervical cancer at an advanced stage at diagnosis in Sudan in which Ibrahim et al. [18] has found that spatial disparity exists between the urban and rural areas of Sudan. Furthermore, it was discovered that the lack of access to health care services in rural areas contributes to late presentation resulting in diagnosis of cervical cancer at an advanced stage.
3.3.3. Histological Diagnosis
In this study, squamous cell carcinoma was the commonest histological diagnosis accounting for 82.3% with Grade 2 invasive type being the highest (43.6%) as shown in Table 6. Adenocarcinoma accounted for 6.3% of the cervical cancer cases. The results were congruent to the study of factors associated with tumour stage at presentation in invasive cervical cancer done at government tertiary referral institutions in Harare, Zimbabwe have found that squamous cell carcinoma is the commonest type of histological diagnosis (96.0%) while adenocarcinoma constitutes only 4% [23]. Their study concludes that intrinsic tumour characteristics are the most important indicator of late stage at diagnosis.
4. DISCUSSION
4.1. Demographic Profile of Cervical Cancer Patients
The study found that the mean age of the patients was 56.3 years. The patients came from the following districts: Capricorn (25%), Vhembe (24%), Mopani (17%), Sekhukhune (12%), and Waterberg (12%). Most of the patients’ records (90.5%) did not contain any information about marital status. Of the information that was available, 4.0% of the women were single, 5.1% married and 0.4% divorced. A large number of patient records did not have information on parity either, constituting a total of 95.6%. The distribution parity was: 0.4% had no children, 0.7% had two children, 1.1% had three children, 0.4% had five children, 1.8% had six children, and 0.4% had eight children.
| - | - | Stage at Presentation | - | |||
|---|---|---|---|---|---|---|
| Place of residence | N | I n(%) |
II n(%) |
III n(%) |
IV n(%) |
p-value |
| Capricorn | 69 | 3(4) | 22(32) | 40(58) | 4(6) | |
| Mopani | 60 | 1(2) | 21(35) | 36(60) | 2(3) | |
| Sekhukhune | 45 | - | 7(16) | 30(66) | 8(18) | 0.150 |
| Vhembe | 64 | 1(2) | 15(23) | 43(67) | 5(8) | |
| Waterberg | 33 | - | 11(33) | 20(61) | 2(6) | |
| Diagnosis | Frequency | Percentage |
|---|---|---|
| Adenocarcinoma | 1 | 0.4 |
| Grade 1 invasive squamous cell carcinoma | 18 | 6.6 |
| Grade 1 squamous cell carcinoma | 2 | 0.7 |
| Grade 2 invasive adenocarcinoma | 8 | 2.9 |
| Grade 2 invasive squamous cell carcinoma | 119 | 43.6 |
| Grade 2 squamous cell carcinoma | 8 | 2.9 |
| Grade 3 adenocarcinoma | 1 | 0.4 |
| Grade 3 endometrial adenocarcinoma | 2 | 0.7 |
| Grade 3 Infiltrating differentiated squamous cell carcinoma | 2 | 0.7 |
| Grade 3 invasive adenocarcinoma | 12 | 4.4 |
| Grade 3 invasive clear cell carcinoma | 1 | 0.4 |
| Grade 3 invasive squamous cell carcinoma | 60 | 22.0 |
| Grade 3 large cell invasive squamous cell carcinoma | 1 | 0.4 |
| Grade 3 large cell neuroendocrine carcinoma | 1 | 0.4 |
| Grade 3 squamous cell carcinoma | 7 | 2.6 |
| Grade 3 squamous cell carcinoma keratinizing int. nuclear | 1 | 0.4 |
| High grade invasive squamous cell carcinoma | 1 | 0.4 |
| Infiltrating differentiated squamous cell carcinoma | 5 | 1.8 |
| Invasive intermediate glandular papillary adenocarcinoma | 1 | 0.4 |
| Invasive squamous cell carcinoma | 3 | 1.1 |
| Large cell neuroendocrine invasive carcinoma | 1 | 0.4 |
| Moderately differentiated invasive keratinizing squamous cell carcinoma | 1 | 0.4 |
| Moderately differentiated squamous cell carcinoma | 1 | 0.4 |
| Non-keratinizing high grade squamous cell carcinoma | 1 | 0.4 |
| Non-keratinizing invasive squamous cell carcinoma | 1 | 0.4 |
| Squamous cell carcinoma | 3 | 1.1 |
| no information on cell type | 11 | 4.0 |
| Total | 273 | 100.0 |
4.2. The Stage of Cervical Cancer Patients at Presentation at the Hospital
The study found that a total of 62% of the patients presented with stage III, 27.8% with stage II, 7.3% with stage IV, 1.8% with stage I, and 0.7% were unspecified. It was evident that most of the patients presented with advanced stage cervical cancer at the hospital.
4.3. Factors that Lead to Late Presentation
The study found that age had an effect on late presentation of the patients at the hospital. The mean age of the patients who presented with stage III cervical cancer was 56.9 years and for the ones who presented with stage IV was 62.5 years. The place of residence also played a role in late presentation of the patients at the hospital. More patients from remote areas of the province presented with advanced stage of cervical cancer as opposed to the ones who resided in areas that are nearer to the capital city of the province. Patients from the Vhembe District which is more rural and the furthest from the capital city of the province, presented with stage III (67%) and stage IV (8%) cervical cancer. Patients from the rural Sekhukhune District presented with stage III (66%) and stage IV (18%) cervical cancer. Patients from the Waterberg District presented with stage III (61%) and stage IV (6%) cervical cancer. Patients from the Mopani District presented with stage III (60%) and stage IV (3%) cervical cancer. Patients from the Capricorn District where the capital city of the Limpopo Province and the Pietersburg Hospital are situated presented with stage III (58%) and stage IV (6%) cervical cancer. In this study, there was no information recorded for 99.3% of the patients about their previous exposure to Pap smear tests. Of the 0.7% of patients who were previously exposed to a Pap smear test, one presented with stage II and the other one with stage IV cervical cancer. In this study, squamous cell carcinoma was the commonest type of histological diagnosis.
4.4. Limitations of the Study
The study was limited to public health care institutions and did not include any private sector facilities. Despite this limitation, the results can be generalised to the province due to the fact that Limpopo Province is a poor province, therefore, most patients consult at public hospitals. Lack of information about parity, marital status, and previous exposure to Pap smear tests was also a limiting factor.
4.5. Recommendations
Based on the findings of this study, the following are recommended for the improvement of initial clinical presentation of cervical cancer at health care institutions:
• Marital Status
Data capturing of information about marital status to further assess the influence this element might have on the clinical presentation of cervical cancer.
• Parity
It is important to have the parity of the patients captured in order to determine the effect that parity has on cervical cancer.
• Pap smear
Availability and improved facilities for screening because early detection of cervical cancer prevents progression to advanced stage of cervical cancer.
• Age
More awareness campaigns about the risk factors of cervical cancer, especially at educational institutions, should be conducted for people in communities to become well informed and aware of the signs and symptoms of the disease.
• Place of residence
A study should be conducted to determine why most patients with advanced stage cervical cancer are from the Sekhukhune and Vhembe districts, particularly the former Venda and Gazankulu regions, since most of the patients with advanced stage cervical cancer are from these districts.
CONCLUSION
The study found that the place of residence and age play an important role in the late presentation of cervical cancer patients at the Pietersburg Hospital. Most of the patients who came from more rural areas presented with stage III and stage IV cervical cancer. This might be due to factors, such as the lack of availability of screening facilities and a lack of awareness about the risk factors of cervical cancer. In order to reduce late stage presentation of cervical cancer at health institutions and thus reducing mortality due to cervical cancer, methods to encourage early detection should be improved.
ETHICS APPROVAL AND CONSENT TO PARTI-CIPATE
Ethical clearance was obtained from the Turfloop Research Ethics Committee (TREC) of the University of Limpopo (No: TREC/47/2015:PG). Permission to conduct the study was obtained from Limpopo Department of Health Research Committee and the Pietersburg Hospital management. Confidentiality was maintained by not writing the names of the patients in the data collection tool and in the final research report.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
STROBE guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
The study is financially supported by University of Limpopo.
CONFLICT OF INTEREST
The authors declare that they have no financial or personal relationships which may have inappropriately influenced them in writing this article.
ACKNOWLEDGEMENTS
The authors thank the Pietersburg hospital management and Oncology clinic managers who gave permission for collecting data in the clinic.
EM Mohuba responsible for conceptualisation of the research study, data collection, design, analysis and finalisation of the article, Mothiba TM supervisor of master dissertation, conceptualisation and writing up of the article.
REFERENCES
| [1] | Villain P, Gonzalez P, Almonte M, Franceschi S, Dillner J, Anttila A, et al. European code against cancer 4th edition: infections and cancer. Cancer Epidemiologyr 2015; 39(Suppl 1): S120-38. |
| [2] | Torre LA, Islami F, Siegel RL, Ward EM, Jemal A. Global cancer in women: Burden and trends. Cancer Epidemiology, Biom Prevention 2017; 26(4) |
| [3] | World Health Organization. Facts sheet. Human papillomavirus (HPV) and cervical cancer. 2018 [Retrieved 24 September 2018];https://report.nih.gov/nihfactsheets/viewfactsheet.aspx?csid=76 |
| [4] | de Sanjosé S, Diaz M, Castellsagué X, et al. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: A meta-analysis. Lancet Infect Dis 2007; 7(7): 453-9. |
| [5] | Petersen LK, Restrepo J, Moreira ED Jr, et al. Impact of baseline covariates on the immunogenicity of the 9-valent HPV vaccine - A combined analysis of five phase III clinical trials. Papillomavirus Res 2017; 3: 105-15. |
| [6] | Human papillomavirus vaccines: WHO position paper, October 2014. Wkly Epidemiol Rec 2014; 89(43): 465-91. [OpenUrl]. |
| [7] | Campos NG, Castle PE, Wright TC Jr, Kim JJ. Cervical cancer screening in low-resource settings: A cost-effectiveness framework for valuing tradeoffs between test performance and program coverage. Int J Cancer 2015; 137(9): 2208-19. [OpenUrl]. |
| [8] | Department of Health. National guidelines for cervical cancer screening programme. Pretoria: Government Printers 2000 [Retrieved 26 November 2018];screening.iarc.fr/doc/SAcervical-cancer.pdf |
| [9] | Sankaranarayanan R. Screening for cancer in low- and middle-income countries. Ann Glob Health 2014; 80(5): 412-7. [OpenUrl]. |
| [10] | Vaccarella S, Lortet-Tieulent J, Plummer M, Franceschi S, Bray F. Worldwide trends in cervical cancer incidence: Impact of screening against changes in disease risk factors. Eur J Cancer 2013; 49(15): 3262-73. |
| [11] | Bray F, Lortet-Tieulent J, Znaor A, Brotons M, Poljak M, Arbyn M. Patterns and trends in human papillomavirus-related diseases in Central and Eastern Europe and Central Asia. Vaccine 2013; 31(Suppl. 7): H32-45. [OpenUrl]. |
| [12] | Chokunonga E, Borok MZ, Chirenje ZM, Nyakabau AM, Parkin DM. Trends in the incidence of cancer in the black population of Harare, Zimbabwe 1991-2010. Int J Cancer 2013; 133(3): 721-9. [OpenUrl]. |
| [13] | Wabinga HR, Parkin DM, Wabwire-Mangen F, Nambooze S. Trends in cancer incidence in Kyadondo County, Uganda, 1960-1997. Br J Cancer 2000; 82(9): 1585-92. [OpenUrl]. |
| [14] | Health 24. Cervical cancer. New South African research accelerates cervical cancer treatment. 2015 [Retrieved 24 September 2018];www.health24.com/Medical/Cervical-cancer/.../New-South-African-research-ac |
| [15] | Smith N, Moodley J, Hoffman M. Challenges to cervical cancer screening in the Western Cape province. S Afr Med J 2003; 93(1): 32-5. |
| [16] | South African Health Review. . Cervical cancer in South Africa: Challenges and opportunities. 2013/2014 [Retrieved 24 September 2018];www.hst.org.za/publications/Kwik%20Skwiz/KWIK%20SKWIZ_Vol3_Iss11.pdf |
| [17] | Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas 1970; 30: 607-10. |
| [18] | Ibrahim A, Rasch V, Pukkala E, Aro AR. Predictors of cervical cancer being at an advanced stage at diagnosis in Sudan. Int J Womens Health 2011; 3: 385-9. |
| [19] | Gyenwali D, Pariyar J, Onta SR. Factors associated with late diagnosis of cervical cancer in Nepal. Asian Pac J Cancer Prev 2013; 14(7): 4373-7. |
| [20] | Testa AC, Di Legge A, De Blasis I, et al. Imaging techniques for the evaluation of cervical cancer. Best Pract Res Clin Obstet Gynaecol 2014; 28(5): 741-68. |
| [21] | Kumar V, Abbas A, Fausto N, Aster J. 2010.Robbins and Cotran Pathologic Basis of Disease. |
| [22] | Ranaghan L, Gavin A. Cervical Cancer Presentation, Diagnosis and Treatment.2010. |
| [23] | Ndlovu N, Kambarami R. Factors associated with tumour stage at presentation in invasive cervical cancer. Cent Afr J Med 2003; 49(9-10): 107-11. |









