All published articles of this journal are available on ScienceDirect.
Systematic Literature Review on strengthening Eye Care Follow-Up Among Glaucoma Patients in Limpopo Province
Abstract
Background:
Adherence to prescribed glaucoma medications is often poor and proper adherence can be challenging for most patients
Objective:
The purpose of this systematic literature review is to identify and evaluate studies that have tested the impact of each intervention on glaucoma adherence based on their quality outcome measure.
Methods:
A comprehensive search of database was conducted from January 2009 to January 2019. We systematically reviewed the literature and identified sixteen studies that used educational interventions to improve glaucoma medication adherence. Eleven out of 16 eligible studies were subjected to Randomized Controlled Trial (RCTs) and the remaining four were reviewed as observational studies. One study was reviewed through both observational plus randomized control trial method.
Results:
Out of the eleven (68.75%) RCTs interventions done, five (31.25%) showed improvement in medication adherence and persistence with eye drop instillation, whereas (n=6) did not show any significant improvement on their medication adherence. The quality of each study was evaluated using the Jadad score calculation and the Ottawa-Newcastle.
Conclusion:
Using information from this systematic review and Health Behavior Model, we created a theoretical framework to illustrate how counseling and education can improve medication adherence amongst glaucoma patients in the country.
1. INTRODUCTION AND THEORETICAL BACKGROUND
The most contributing factor for progressive vision loss that leads to blindness is poor medication adherence. Adherence rate for patients receiving chronic glaucoma treatment is between 43% and 78% worldwide, while other studies reported that 10 - 30% of glaucoma patients often omit their prescribed doses [1]. The early manifestation glaucoma trial and Ocular Hypertension Treatment studies found that the use of medications to reduce IOP resulted in (54%) over five years and a 50% reduction in the risk of glaucomatous progression over six years among patients treated with trabeculoplasty and topical therapy as compared to their untreated control group [2]. Further, the United Kingdom Glaucoma Treatment Study has reduced the risk of glaucomatous progression by 44% in two weeks.
Appropriate glaucoma medication and follow up care are vital in preventing vision loss and can prevent blindness. The World Health Organization states that improving adherence may have a “far greater impact on the health of the population than any improvement in specific medical treatment” [2]. In addition, studies on glaucoma medication compliance also emphasize this need [2]. WHO further states that adherence to long term therapies among patients with chronic diseases in the general population is around 50%, and the percentage is much lower in developing countries. Notably, non-adherence among glaucoma patients has been reported to be as high as 80% [2, 3]. However, inconsistent adherence to recommend follow up hinders the ability of the physician to track disease progression. Patients who did not have a consistent follow up were more likely to have the mild disease than those who had consistent follow up [4].
There are no standard criteria to determine adherence and methodologies. However, various techniques have been used to detect nonadherence in glaucoma follow up [4-6]. Efforts have been made to design and evaluate various interventions to improve glaucoma adherence with mixed achievement. In addition, various intervention strategies comprised of: (1) patient education sessions; (2) written information; (3) medication reminders; (4) eye drop instillation training and (5) individualized adherence plans. Furthermore, adherence and persistence were mostly measured in different techniques such as electronic monitoring devices, pharmacy refill data and self-report [7].
Each technique has its own advantages and disadvantages. Some studies have identified and grouped risk factors for non-adherence with topical glaucoma medications into four major categories: patient-related factors, provider-factors, medication regimen and environmental factors [5, 8, 9]. It was against this background that this systematic literature review was carried out.
2. PURPOSE
The purpose of this systematic literature review is to identify and evaluate studies that have tested the impact of each intervention on glaucoma adherence based on their quality outcome measure used to assess adherence.
3. METHODOLOGY
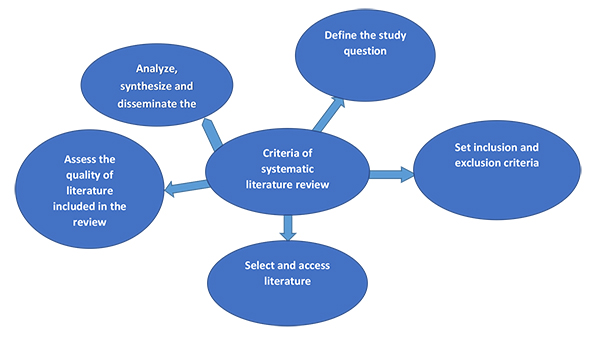
A systematic literature review is a scientific investigation that focuses on a specific question and uses clear, pre-specified scientific methods to assess, critically assess and synthesize all the literature on a particular topic. Also, the systematic review provides a starting point for clinical practice guideline developers [10]. For this study, through a systematic review method, we could identify and evaluate the scientific evidence of both qualitative and quantitative research. The search was limited to journal articles to exclude other types of publications such as book chapters, newspaper articles and conference proceedings. The following systematic steps as outlined by Cronin et al. [11] and Ramdhani et al. [12] were applied to reduce literature-review errors and bias and to produce a transparent, structured and comprehensive overview of the available literature as shown in Fig. (1).
Step 1. Defining the Research Question.
According to Demonceau et al. [13], it is important to define the questions to be addressed in strengthening glaucoma follow up systematic review and to identify the purpose and scope of the review. Additionally, defining the questions will direct the reader on the kind of information reviewed and determine the scope of the review. The research question was defined through the discussion with the supervisor and co-supervisor. Consultation with the eye care health workers and colleagues was also done to ensure that the review is relevant to real-world challenges. The research questions were: 1) What is the current state of compliance amongst glaucoma patients in Africa? 2. What strategies can be used to ensure that glaucoma patients remain in care within the health care facilities?
Step 2. Setting for Inclusion and Exclusion Criteria
Shamseer, Moher, Clarke et al. [14] outlined that setting for inclusion and exclusion criteria ensures that the review is conducted in an organized way. Additionally, it provides for transparency on how the strengths and limitations were assessed. Primary research studies were included in this systematic review. No restriction was made on the study location. Studies were included if they were published in English language and had a sample size of more than 50 participants. Studies were restricted to those that used Randomized Controlled Trial (RCT) and observational studies. Included were also studies that used educational interventions with comparison groups and those that targeted patients diagnosed with glaucoma with age 18 years and above. Included also were all the studies that have been conducted and evaluated or assessed. All studies that focused on glaucoma surgery, children or juvenile glaucoma were excluded. If the sampled population of the study was very specific, for instance, males or females, or recruited patients from one specific class (homeless, prisoners, workers from one employer, etc.) were also eliminated because results from the study might not be generally applicable to the general population. To avoid including duplicate data, the newest and most informative articles were selected as multiple studies were conducted by the same authors.
Step 3. Conducting a Literature Search
The online database literature search was conducted by searching several for all relevant articles. The search was limited to journal articles to exclude other types of publications such as book chapters, newspaper articles and conference proceedings. The search strategy was used in collaboration with the School of Health Sciences librarian. Health and medical databases including SABINET, EBSCOHOST, SCIENCE DIRECT, MEDLINE and GOOGLE SCHOLAR were used. Key concepts and search terms were developed to capture literature related to strengthening eye care follow up among glaucoma patients. The search methodology followed a PICO (population or patient, intervention, comparison, and outcome) format. The search strategy combined sets of keywords, using AND/OR terms. The terms from the following five categories of medical subject headings (MeSH) were used to search the articles and grey literature (Compliance, glaucoma, education, intervention and adherence).
Step 4. Assessing the Quality of Literature Included in the Review
This review included all the articles and reports obtained after databases were merged. Duplicate articles were removed and additional articles provided by content experts were identified. Secondary sources, which included textbooks and review articles, description or summary by somebody other than the original researcher, were removed. Only studies that were published between 2009 to 2019 in the English language peer-reviewed journals, reports or websites were reviewed to identify gaps in the adherence to glaucoma medications and the intervention strategies used to improve adherence. Furthermore, if a study consisting of only abstracts was not included. The studies included were those that explored intervention strategies to improve glaucoma adherence. Titles and abstracts were searched against the inclusion criteria and full texts that met the criteria were retrieved.
Step 5. Analyze, Synthesize and Disseminate the Findings
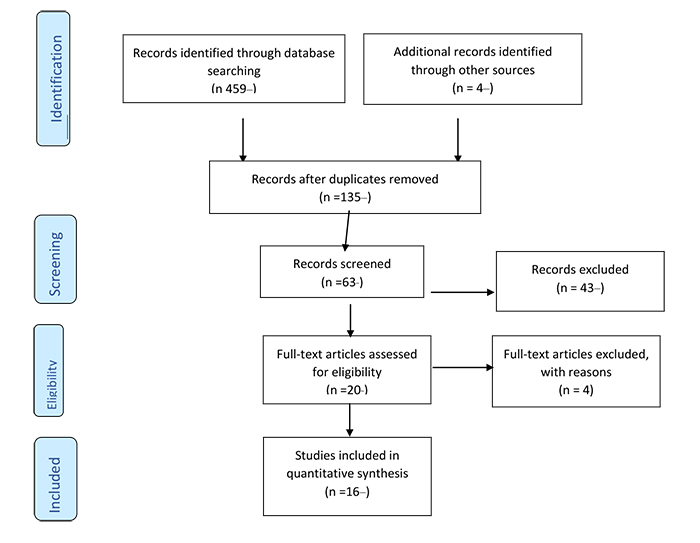
The initial search yielded a total of 459 research articles and 135 were further assessed for their relevance to the study. After screening the titles and abstracts, an additional 63 articles were excluded from the search as they did not contain adequate evidence that can effectively assess the intervention. After the full text review, two researchers agreed on sixteen articles out of twenty articles that met the inclusion criteria. Finally, sixteen articles were included in the analysis as shown in Fig. (2).
The studies which were included were clustered and organized by the concepts which emerged from themes. To provide sufficient substance to a theme, concepts from a minimum of three articles were required. Two thematic domains emerged from the literature:(i) Theme 1: The effectiveness of electronic interventions to assess treatment and procedures for glaucoma conducted. (ii) Description of observational studies measuring baseline adherence to glaucoma medication.
Most countries identified the importance of conducting educational interventions strategies in systematic literature reviews. Sixteen studies met the inclusion criteria in this literature review after doing verification using hand search. Out of sixteen articles that met the inclusion criteria, 11 of the studies were analyzed through a Randomized Controlled Trial (RCTs) process and the remaining four were put through an observational process. Only one study was subjected to a mixed method process. All the eligible intervention studies were conducted outside sub-Saharan Africa.
The quality of each study was evaluated using the Jadad score calculation for all RTCs studies, while for observational studies, Ottawa-Newcastle score was used. Jadad score is a five -point scale used in the meta-analysis literature to judge the quality of RTCs. Jadad score rewards one point based on the following criteria: (i) was the study randomized; (ii) was the method of randomization appropriate; (iii) was the study described as double-blind; (iv) was the method of double-blinding appropriate;(v) was there a description of withdrawals and dropouts [15]. One point was assigned if the study was described as single blinded and another one point was given if the study outcomes were blinded specifically for the participant who received the intervention and lastly two points were awarded if the adherence was measured by pharmacy claims data as opposed to self-report as displayed in (Table 1).
| RCT studies using Electronic adherence measurement :2009-2014 | Author | Study setting & sample size | Intervention type | Study quality |
|---|---|---|---|---|
| 1. Interventions improving poor adherence(2009) | Okeke et al | Glaucoma clinic Total:66 glaucoma |
Video,reminder phone call and Counselling | Jadad:5/5 |
| 2. Adherence to glaucoma medication(2013 | Lim et al | Academic center:80pts | Automated reminder &educational sessions | Jadad:5/5 |
| 3. Automated Telecommunicated-based reminders (2014) | Boland, et al | Glaucoma clinic:491 pts | Text messages using personal health record | Jadad:5/5 |
| 4. Improving adherence to glaucoma medication(2014) | Cate et al | Glaucoma clinic:208Pts | Behavioral counselling and motivational l support by glaucoma support assistants | Jadad:5/5 |
| 5. Adherence improvement in Dutch glaucoma patients(2014) | Becker et al | Hospital:805pts | 4 types(1)Travel Alert dosing aid,(2) patient education,(3)TravAlert aye drop guider and combination of both. | Jadad:5/5 |
|
RCT studies using pharmacy refill, self report, data chart
2011-2016 |
- | - | - | - |
| 1.Effectiveness and Cost of a personalized Reminder Intervention(2016) | Pizzi,et al | Hospital:256 glaucoma pts | Personal call and Customized letter | Jadad:5/5 |
| 2.Motivational Interviewing or reminders for glaucoma(2016) | Cook, et al | University clinic:201pts | Motivational interview, reminder call,MEMs bottle | Jadad:4/5 |
| 3. Impact of a brief educational intervention on glaucoma(2015) | Djafari et al, | Hospital :165 glaucoma pts | 60 to 90 minutes educational session on glaucoma patients | Jadad:3/5 |
| 4. Influence of health literacy level (2012) | Muir et al | Glaucoma clinic:127pts | A video was used | Jadad:5/5 |
| 5. Impact of Health Communication Intervention (2012) | Glanz et al | Hospital:312pts | I-SIGHT program. | Jadad:5/5 |
| 6. Individualized patient care controlled trial (2012) | Gray et al | Eye hospital:127 newly diagnosed pts | Personalized individual health assessment | Jadad:5/5 |
| Observational studies using pharmacy refill,self report:2011-2015 | - | - | - | - |
| 1. The eye drop chart: (2015) | McVeigh et al | Hospital:25pts | Eye drop chart. Audio reminder visual system | Ottawa-Newcastle score 4/5 |
| 2. A 2 hour information session (2012) | Blondeau, et al, | Glaucoma clinic:342pts | 2hour educational session, eye drop instillation | Ottawa-Newcastle score 5/5 |
| 3. Web-based intervention for improving adherence (2011) | Lunnela ,et al | Hopsital | Glaucoma content link were emailed to the patients | Ottawa-Newcastle score 4/5 |
| Observational studies using Electronic and a questionnaire | - | - | - | - |
| 1.Glaucoma Management (2016) | Dreer, et al | Glaucoma clinic:14pts | Patient education, MI and problem solving training(PST) | Ottawa-Newcastle score 4/5 |
| Mixed RCT and Observational study | - | - | - | - |
| 1.A study to assess the feasibility of undertaking a randomized controlled (2013) | Richardson et al | Glaucoma clinic:19pts | Group based educational program. | Ottawa-Newcastle score 4/5 |
Theme 1: Effectiveness of Electronic Intervention Studies to Assess Treatment and Procedures for Glaucoma Studies Conducted
3.1. Electronic Interventions Studies Using Randomized Controlled Trial
Electronic interventions are electronic reminders (automatically sent reminders without personal contact between the healthcare provider and patient) that are now increasingly used in an effort to improve adherence. Furthermore, electronic intervention strategies include short message service (SMS), telephone, Facebook, internet, electronic reminder devices (ERD) and voice message [16]. Most of the reviewed studies were subjected to a randomized control trial (RCT) process, a trial in which subjects are randomly assigned to one of the two groups. For instance, one (the experimental group) receiving the intervention that is being tested, and the other (the comparison group or control) receiving an alternative (conventional) treatment. The two groups are then followed up to see if there are any differences between them in the outcome. The results and subsequent analysis of the trial were used to assess the effectiveness of the intervention. RCTs are the strictest way of determining whether a cause-effect relation exists between the intervention and the outcome [17]. Results from this systemic literature review have shown that, out of the eleven randomized control trial (RCT) studies, five used electronic monitoring as an adherence measurement, while five RCT used pharmacy refill, self-report and data chart. The eleventh study used both RCT and observational processes. All five RCT studies that used electronic monitoring were conducted either at glaucoma clinic or hospital clinic. None of the studies were conducted in a community setting.
3.2. Motivational Interviewing Based Glaucoma Education as Opposed to Standard Care
Motivational interviewing was used to improve glaucoma medication adherence. Patients were put in the following three groups: (1) The control group, (2) the comparison group and the (3) motivational interviewing group. Reminder call, Motivational interview (MI) and Medication Event Monitoring System (MEMS) were used. The medication event monitoring system (MEMS) is a cap that fits on standard medicine bottles and records the time and date each time the bottle is opened and closed [18]. All three groups received allocated intervention, but group 1 and 2 did not receive extra in-person visits while group 3 received three in -person visits with an ophthalmic technician (OT) trained in MI (at weeks 1, 4, and 8 after randomization) plus three phone calls from the same OT (week 2, 6 and 12). Other studies used automated reminders and educational sessions. Group 2 and 3 received three reminder phone calls from the clinic staff member asking about their level of adherence, reasons for any missed doses and their use of MEMS [19].
3.3. Automated Reminders and Educational Sessions
In this electronic intervention, automated reminders and educational sessions were used to measure medication adherence. Educational sessions were conducted by the facility caregiver. The intervention group undertook a 20-30-minutes scripted education session with a research assistant for three months, and their adherence was measured for two more months. The adherence level of the control group and the intervention group did not show any improvements. Instead, there was a decline after the intervention as reported by Lim, Watnik, Imson, Porter and Granier [20] in their study. Furthermore, some participants on the intervention group received daily messages through text or voice messages reminding them to take their medication while participants in the control group only received the usual care. Both groups were further instructed to use the MEMSCap to monitor their medication use and the study coordinator conducted a follow-up after three months on the intervention group regarding the monitoring device, their drop use and their reminders [21].
3.4. Health Literacy Modified Glaucoma Education against Standard Care
The impact of an educational intervention was modified to health literacy on glaucoma medication adherence. Participants in the intervention group used informational video about glaucoma at 4th, 7th, or 10th grade level, depending on the participants. Additionally, the intervention group members were further taught on the instillation of eye drops and they had to demonstrate to the study coordinator the proper technique on eye drop instillation. The control group only received standard care. Participants whose health literacy level was less than 10th grade were shown eye diagrams while the coordinator reviewed the educational information. Participants in the intervention group received a phone call once per month to check if they were experiencing any problems with glaucoma medication. After evaluating the intervention, the study showed that patients with low level of health literacy skills might benefit from educational efforts tailored to address their health literacy level [22].
3.5. Behavioral-counseling Interventions
Behavioral-counseling interventions empower patients to participate in their care while positively changing their skill levels or normal routines. For example, skill building by a health care professional and problem solving are helpful [23]. The counseling comprise of glaucoma education and motivational support from trained para-professional staff called glaucoma support assistants (GSAs). Throughout the intervention, the GSA met three times for eight months with the patients while the control group received standard care with their physician. Each brief-MI counseling technique done by the GSA was assessed for fidelity using standard measures [24].
3.6. Interventions Based on Technical Reminder Systems
The participants whose baseline level of medication adherence was less than 75% were either put in an intervention group or control group (usual care). The intervention group watched a ten-minute educational video, reviewed prevailing barriers and possible solutions to eye drop taking with the study coordinator. The participants further received regular phone call reminders and had audible and visible reminders activated on their Dosing Aid (DA) devices. Furthermore, coordinators taught participants on their medication record keeping. In addition, study coordinators reminded patients to take their weekly and biweekly medication over a period of three months while the control group was told to take their eye drops as prescribed and received no additional intervention [22, 25].
3.7. RCT using Customized Letter and Personal Telephone Outreach
The groups were divided into two groups, that is the usual care that served as the control group and the intervention group. The control group did not receive any reminder letters or phone calls. The intervention groups were sent customized letters two weeks preceding their appointment and telephone calls 2-3 days before the appointment. If the subject failed to attend the scheduled appointment, the researcher made two additional personal telephone calls. In the event where the subject responded positively and agreed to the scheduled appointment, a telephone reminder was made 2-3 days prior to the scheduled appointment. In cases where the subject was not reached after two phone calls, the subject was not contacted again [26].
3.8. Impact of Brief Educational Intervention on Glaucoma Medication Adherence
Patients were randomized to either an immediate intervention or normal care. The two 60-90 minute educational sessions on glaucoma and its management were led by a trained non-practicing ophthalmologist. The two sessions were conducted within two weeks apart. Sessions were given in small formats. Persistence to glaucoma medication was examined for a period of one year using hospital and pharmacy claims records. Questionnaires were administered and medication possession ratio was calculated (that is taking eye drops as prescribed) in all the patients at the end of the study [7].
3.9. RCT using Self-report, Pharmacy Refill and Chart Review
This is a randomized controlled trial using self-report, pharmacy refill data and chart review as a means of adherence measurement. The participants should all be non-adherents. The study described a patient to be glaucoma nonadherent if the patient failed to report for clinic appointment or failed to collect glaucoma medication in the past year. While adherence was measured using patient self-report, chart review of refill adherence, physician assessment of medication adherence and appointment adherence. The treatment group received an automated, interactive voice recognition, tailored telephone intervention and tailored printed materials. The control group received the usual care of recommendations of medical appointments and prescription refill on each visit [27].
3.10. Impact of Individualized Patient Care as an Aide to Standard Care
Randomization was generated using a computer to get the intervention group and the control group (standard care). The trained glaucoma nurse implemented standard care and individualized care plan. The intervention began with a 45-minute counseling session of healthcare needs and beliefs, followed by a 20-minute educational session and then a 10-minute training session on eye drop instillation and proper technique.
Nurses collaborated with the patients to form a tangible plan of how to integrate eye drop regimen into the patients daily routine. Individualized follow up care according to each person’s need was done. The same nurse met with the patients for approximately 15 minutes either in person or telephonically to discuss glaucoma information, give feedback on adherence and to address other concerns. Patients could call the nurse in-between visits for additional support. The intervention group showed a significantly stronger belief in the importance of eye drops and had more personal control over their condition. Therefore, an intervention had a positive effect on adherence behavior to glaucoma therapy. Thus, adherence was significantly higher in the intervention group as compared to the control group after 12 months [28].
Theme 2 Description of Observational Studies Measuring Baseline Adherence to Glaucoma Medication
3.11. Assessing the Feasibility and Preliminary Effectiveness of a Health Promotion Program
Studies had a pre-post design in which the baseline adherence was measured prior to the implementation of an educational intervention and again after an intervention. The program wanted to improve adherence using three approaches: (1) patient education, (2) motivational interviewing, and (3) problem solving training (PST). The program focused on African-Americans (AAs) due to their higher risks of developing glaucoma. Furthermore, AAs are also at risk for poor medication adherence as compared to Caucasians [29]. The health educator (who is a licensed clinical psychologist) carried out the intervention. The health educator met separately with patients at glaucoma clinics. Each patient participated in a four-weekly session tailored to the overcome patient barriers and glaucoma medication adherence. The first session of face-to-face was conducted at the clinic, and the additional sessions took place over the phone [30].
3.12. Assessing the Efficacy of the Eye Drops Chart in Improving Patients’ Glaucoma Medication Adherence
The study used Eye Drop Chart (EDC) type of intervention which was an audio-visual reminder system for glaucoma medications. An EDC consists of a chart signifying medication, instillation times, and the eye that needs treatment. The medication schedule was followed by eye instillation instruction, then each medication was placed underneath the chart. Therefore, the study did not show any significant difference in self-reported adherence before and after using EDC as an intervention [31].
3.13. Group Based Educational Program using Observational and Randomised Control Trial
It was a quasi-experimental pre-post analysis of a two sequential groups-based education program. The group used educational intervention and practical medical events monitoring system (MEMS) data. Baseline assessment of the outcome questionnaires was taken one month before the group-based educational program and again three months after the delivery of the program. Continuous observation on eye drops adherence was made from one month before to three months after the intervention. A glaucoma trained nurse supported by other health professionals led the educational programme which lasted less than two and a half hours. The session allowed time for the participants to describe their experiences with glaucoma and had time to ask questions [32]
3.14. Two-hour Nurse-led Educational Session Observational study
Researchers measured the persistence with glaucoma medication for two years before and one year after a group of educational sessions. The glaucoma nurse used a PowerPoint presentation for patients and their invited family members. The sessions were limited to fifteen people (including patients and family members). Patients demonstrate back on how to instil eye drops and glaucoma handouts were distributed after the session. Participants were each contacted three times over a period of ten months to address any questions, encourage adherence and plan follow up visits [33]
3.15. An Observational Case-control Study on Web-based Glaucoma Education
The intervention group received an email with two kinds of web sites links with glaucoma information and its management. The other link was based on the personal information of the patient. Participants in the control group filled out their surveys regarding their adherence behaviour and were then given standard care by their ophthalmologist [34].
4. DISCUSSION
Regular follow up is critical in glaucoma care to monitor the disease and adjust treatment when necessary. Systematic review of the literature was conducted to determine the effectiveness of educational intervention strategies in strengthening glaucoma eye care follow up. The primary outcomes measured were glaucoma medication adherence. Various literature databases and grey literature were searched, resulting in the inclusion of sixteen studies after three level of screening. Results suggest that there is significant improvement with medication adherence after an educational intervention. Most (8/11) of the RCT studies reviewed showed some improvement in glaucoma medication adherence. However, three (3/11) studies showed that a trend towards an improvement in medication adherence was not statistically significant. Types of educational interventions that were used differ from one study to another. Therefore, it is not easy to determine which specific characteristics of the educational intervention had the most effect on medication adherence.
Overall, eleven studies focused on improving knowledge to improve Medication compliance. Patients who received automated text messages and voice calls treminding them to take their medication improved their adherence. Furthermore, patients who were shown educational videos on the instillation of eye drops using Dosing Aid devices had their medications improved as compared to the control group. All studies that used electronic monitoring only as their adherence measures showed significant improvement in glaucoma medication as shown in Table 1. Such studies used educational sessions, videos, automated reminder calls, counselling in form of motivational interviewing, text messaging using personal health record and eye drop guide.
Furthermore, patients who received short text messages (SMS) were more likely to attend their glaucoma appointments as compared to those who had not received an SMS [21]. A study that used MI as an educational intervention showed slight effect on the intervention group. Motivational interventions had smaller effect than reminder calls. But MI needs more training and practice because most ophthalmologists do not have ophthalmic technicians who are trained in MI. Therefore, reminder calls led to better adherence than usual care even though most studies support MI [19]. Cook et al., 2016 [19] focused on using motivational interviewing to improve self-efficacy to improve glaucoma medication adherence. The effects of multiple interventions such as reminder devices, patient education and eye drop guide on glaucoma medications adherence failed to improve adherence over a period of six months. Patients who received dropper guide were significantly more nonadherent than those without the dropper guide. Instead, it made it harder and led to reduced medication adherence [22]. Muir et al. [36] tailored their intervention to patients’ level of health literacy. They were concerned with patients with low and marginal health literacy as compared to patients with 10th grade health literacy level. Patients with low level of health literacy skills may benefit more from education efforts tailored to address their health literacy level.
There were four observational studies that took place from 2011 to 2016 that met our inclusion criteria for this systematic review. All the studies that were reviewed had a pre-post design in which the adherence was measured prior to the implementation of an educational intervention, and the adherence was measured again after the educational intervention. Most observational studies used pharmacy refill.
An observational study of glaucoma knowledge and persistence conducted by Blondeau et al. [33] did not show any improvement in persistence within one year. This was a nurse-led educational session where glaucoma medication was measured after a two-hour educational session by means of pharmacy refill. Furthermore, there was no significant difference in self-reported adherence before and after by the patients who were using eye drop chart as an intervention. Also, participants that received web sites link with glaucoma information and its management via email for the intervention group did not show any adherence improvement [32, 34]. The only observational study that showed improvement in medication adherence after intervention was that it assessed the feasibility and effectiveness of health promotion. Overall patient satisfaction and suitability were high for the program, interactions with the health educator, program materials and the length of sessions. The limitation of this study was that the time spent when counselling the patients was not described [30]. However, the group based glaucoma educational program did not improve adherence at either one month or three months after the intervention, but 58% of the participants showed improvement in adherence after electronic medication monitoring as this was the only study that used RCT and observations in this systematic literature review [32].
5. ASSESSMENT OF OUTCOMES
The most used measurement assessment of medication adherence was an electronic medication monitoring. Out of the six randomised control trials, five used electronic medication monitoring in their studies [19, 22, 24, 25 ]. Electronic medication monitoring is also called the gold standard for assessment of medication adherence because of its accuracy [15]. Another utmost commonly accepted measure of medication adherence was the use of medication pharmacy refill data as reported by Muir et al. [36].
From the five observational studies that were reviewed in this systematic review, two studies conducted by McVeigh and Vakros [31] and Lunnela et al. [34] used self-report and one used electronic medication monitoring (Dreer et al [30]) as an assessment measure for adherence while Blondeau et al’s [33] assessment of nurse-led group education session used prescription refill data. Only one observational study used a combination of both electronic medication monitoring and self-report [32]. However, the challenge that came with self-report as a measure of adherence was that it was often inaccurate although it can identify those who are nonadherent. It is most likely that those reporting nonadherence are being truthful.
CONCLUSION
Most of the systematic reviewed studies used electronic interventions and were hospital/pharmacy based. Few studies used motivational interviews and others used a combination of both electronic and pharmacy refill data. None of the studies were conducted in the community or family setting. Most of the studies that used self-report showed no significant improvement in medication adherence between the control group and the treatment group. However, with the electronic intervention, most showed an increase in glaucoma medication adherence between the two groups. During this study, a gap was identified that no publications or sources addressing detailed strategies used in glaucoma adherence in South Africa / Africa were found. Some of the studies that were found were not evaluated to find out the outcome, such as the study protocol that was conducted in Nigeria on motivational interviewing to improve treatment uptake for glaucoma patients. All studies that have outcomes were conducted in developed countries. This necessitated consultation of unpublished dissertations and theses. Significantly, a lot of material is available on the knowledge attitude and self-care practices regarding glaucoma disease. This suggests that there are no known studies conducted on the intervention strategies to strengthen eye care follow up among glaucoma patients in Limpopo Province of South Africa.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS FOR REPORTING
PRISMA guideline and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


