All published articles of this journal are available on ScienceDirect.
Tetanus Toxoid Immunization Status and Associated Factors among Mothers in Hawzen, Eastern Zone of Tigray, Ethiopia, 2019
Abstract
Background:
Neonatal tetanus remains a significant avertable cause of morbidity and mortality in neonates. Adequate vaccination strategies, including at least two doses of tetanus toxoid for reproductive age women, can decrease neonatal mortality. In Ethiopia, a few numbers of neonates were protected at birth through this proactive intervention. Therefore, this study aimed to determine factors associated with the low coverage of tetanus toxoid immunization.
Objective:
This study aimed to determine the status of Tetanus Toxoid immunization coverage and factors associated with it.
Methods:
Community-based cross-sectional study design was implemented among 515 mothers in Hawzen, Eastern zone of Tigray. The data were entered into Epi data manager version 3.5.1 and exported to Statistical Package for Social Science version 20 software for analysis. Bivariate and multivariate logistic regression was used to identify factors significantly associated with tetanus toxoid immunization coverage.
Results:
Two hundred and seven (40.2%) mothers were protected against tetanus at last birth. Mothers whose age was less than 20 years [AOR 0.19(0.10, 0.32), had no future plan for fertility [AOR 0.30(0.17, 0.53)], mothers attended once for antenatal care visits [AOR 0.38(0.18, 0.82)] and who got information from media [AOR 4.49(1.82, 11.07] were independent predictors of tetanus toxoid immunization status of mothers.
Conclusion:
More than half of the mothers were not protected against tetanus at the time of last birth. This study found the age of mothers, future fertility plans, numbers of antenatal care visits and mothers who got information from media; these were significant factors associated with the likelihood of tetanus toxoid immunization of mothers.
1. INTRODUCTION
Tetanus is a non-communicable disease transmitted via exposure to the spores of the bacteria Clostridium tetani [1]. Around 3.3 million neonatal deaths occur globally annually, with approximately 34,000 due to neonatal tetanus [2, 3]. Neonatal tetanus is related to improperly or insufficiently immunized mothers (and through passive immunity process the infant) usually due to poor sanitation (e.g., unclean delivery environment, poor cord care) in the intra-partal and post-partal periods. The disease, sometimes called the ‘disease of the 7th day’, presents in the neonate usually within 14 days post-delivery with a nearly 100% case-fatality rate without intensive care access [4].
According to the United Nations Children’s Fund (UNICEF), in 2018, approximately 72% of reproductive age women globally were adequately immunized. Such immunity included vaccination of tetanus toxoid (TT) of at least two doses for pregnant or reproductive age women can decrease neonatal mortality by 94% (95% CI: 80-98%) [5]. Previous studies have discussed factors like age of mothers, misconceptions about immunization, educational status, residence, fear of side effects, use of modern contraceptives, as well as knowledge and awareness of vaccinations as significantly associated with the status of TT coverage [5-10].
Between 2000 and 2019, Ethiopia shifted from not meeting to meeting the WHO goals of Maternal Newborn Tetanus Elimination (MNTE) [5, 11]. Despite these efforts of extended immunizations and campaigning Tetanus Toxoid vaccinations, Ethiopia continues to have the highest neonatal tetanus morbidity and mortality rates due to low TT immunization coverage combined with a higher number of mothers who gave birth at home in the area of the unsafe and unsterile environment [11, 12]. There is a paucity of studies regarding TT status and factors associated with its low coverage in Ethiopia and specifically in the Tigray study area. Thus, this study is aimed to determine the status of TT immunization coverage and predictors of the likelihood of TT immunization in the study area.
2. METHODS
2.1. Study Area, Period and Design
A community-based cross-sectional study design was implemented among 515 mothers in Hawzen, Eastern zone of Tigray between April and May 2019.
2.3. Study Population
Sampled mothers who had given birth in the last 12 months in the selected kebeles during the data collection period.
2.4. Inclusion and Exclusion Criteria
Mothers who lived in the woredas (District) for at least 6 months were included, while mothers who were critically ill or unable to respond were excluded from the study.
2.5. Sample Size Determination and Sampling Procedure
The sample size was determined using a single population proportion formula by taking the proportion of coverage of tetanus toxoid two (TT2), which indicates two doses on the TT were administered, from a study conducted in Ethiopia (72.5%)(8), Assumptions of 95% confidence interval (CI), 4% margin of error, and a 10% non-response rate, which yielded the sample size, which was 515. From the four kebelles found in Hawzen town, two of them were selected using a simple random sampling method. The number of mothers who gave birth in the last twelve months in the kebelles at the health post level from family folder and delivery registration book was registered before the field was started in order to create sampling frame, then each household was given corresponding house number according to the sorted sampling frames. Once this determination was made, study participants were selected systematically.
2.6. Data Collection Process and Instrument
The data collection tool was adapted from WHO, EDHS, and different kinds of literature and adapted to the local context. Following pre-testing, a structured questionnaire and face to face interviews were conducted.
2.7. Data Processing and Analysis
The data were entered into EpiData manager Version 3.5.1 and exported to Statistical Package for Social Science (SPSS) version 20 software for further analysis. Considering the odds ratio with a 95% confidence interval, the two-tailed P value was computed to declare the level of significance. Bivariate and multivariate logistic regression with a 95% confidence interval was used to identify factors significantly associated with TT immunization coverage. Statistical significance was declared if the P-value was <0.05.
2.9. Operational Definitions
2.9.1. Immunization Status
When mothers had received <2 TT dose (not protected at birth) or had received ≥2 TT doses (protected at birth)(4).
2.9.2. Protected at Birth
(PAB): if the mother had received documented or not, two or more doses during the current pregnancy or at least two TT doses prior to the current pregnancy of which the last dose was <3 years before the birth; or three doses within the 5 years before the current pregnancy; or four doses with the last dose <10 years before the pregnancy or receiving five doses or more before the current pregnancy (4, 5).
3. RESULTS
3.1. Socio-demographic and Health Services Related Characteristics
Five hundred and fifteen women who had given birth in the last 12 months before the survey participated yielding a 100% response rate. Regarding residence, [460(89.3%)] were urban
| Variables | Category | Frequency[N=515] | Percentage (%) |
|---|---|---|---|
| Age of mother | <20 | 322 | 62.5 |
| 20-30 | 52 | 10.1 | |
| >30 | 141 | 27.4 | |
| Residence | Rural | 55 | 10.7 |
| Urban | 460 | 89.3 | |
| Religion | Orthodox | 418 | 81.2 |
| Protestant | 58 | 11.3 | |
| Muslim | 39 | 7.6 | |
| Ethnicity | Tigray | 500 | 97.1 |
| Afar | 15 | 2.9 | |
| Marital status | Married | 373 | 72.8 |
| Single | 138 | 26.8 | |
| Divorced | 4 | 0.8 | |
| Maternal educational status | No formal education | 246 | 47.8 |
| Elementary school | 120 | 23.3 | |
| Secondary and above | 149 | 28.9 | |
| Husband educational status | No formal education | 277 | 53.8 |
| Elementary school | 136 | 26.4 | |
| Secondary and above | 102 | 19.8 | |
| Mother occupational status | Housewife | 312 | 60.6 |
| Government employee | 94 | 18.2 | |
| Self-employed | 109 | 21.2 |
and (97.1%) were Tigrian by ethnicity. Concerning educational status, [246 (47.8%)] mothers and [277 (53.8%)] husbands have no formal education, and [312 (60.6%)] mothers were housewives by occupation (Table 1).
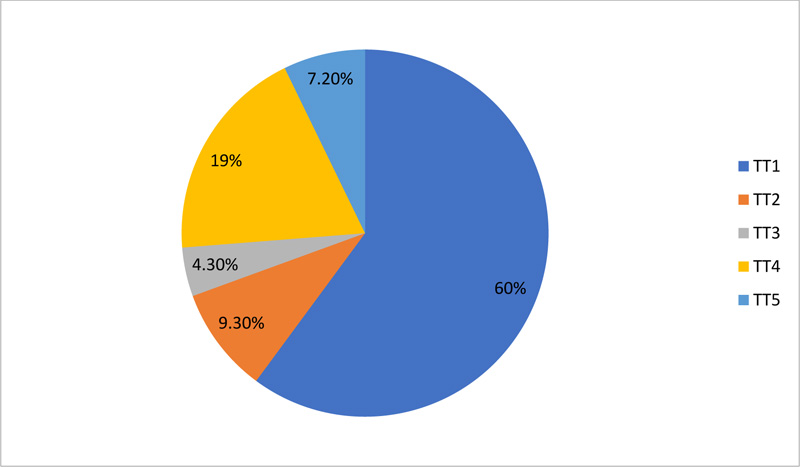
3.2. Maternal Immunization Status
The sources of information were the mother’s vaccination card and oral history. Three hundred and sixty four [70.7%] of them had vaccine cards. Two hundred and seven [40.2%] mothers were protected against tetanus at last birth (received greater or equal to two doses of TT vaccine). Thirty seven [7.2%] mothers completed the recommended vaccine and [1(0.2%)] mother never took it ever in her lifetime (Fig. 1).
3.3. Knowledge Response of Reproductive Aged Women on Tetanus and TT Vaccine
Seventy six [14.8%] women had never heard of the TT vaccine. Fifty eight [11.3%] of them did not know to whom the priority would be given and [27(5.2%)] of them did not know how many times should this vaccine be taken. Even though [453 (88%)] mothers knew the importance of TT vaccine, only [339 (65.8%)] knew that it is for the prevention of tetanus (Table 2).
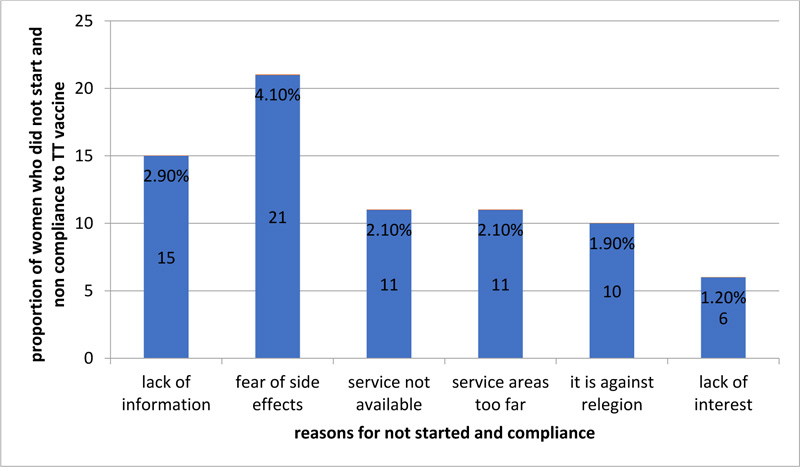
3.4. Reasons for not Starting and Non-compliance of TT Vaccination
Mothers were asked for reasons why they did not start TT vaccination and not compliant, to which [21(4.1%)] of them respond as fear of side effects due to misconceptions, lack of information about the vaccine [15(2.9%)], and service are too far away to participate[11(2.1%)]. Other women spoke of service unavailability, religious reasons, and lack of interest (Fig. 2).
| Items | Category | Frequency | Percentage |
|---|---|---|---|
| Have you ever heard of TT vaccine? | Yes | 439 | 85.2 |
| No | 76 | 14.8 | |
| Do you know the importance of TT vaccine? | Yes | 453 | 88 |
| No | 62 | 12 | |
| Which type of disease is prevented by TT vaccine? | TB | 118 | 22.9 |
| Tetanus | 339 | 65.8 | |
| Measles | 31 | 6 | |
| Others* | 27 | 5.3 | |
| Who is given priority for the vaccination? | Female of any age | 152 | 29.5 |
| Male of any age | 29 | 5.6 | |
| Women of reproductive age | 276 | 53.6 | |
| I do not know | 58 | 11.3 | |
| How many times should this vaccine be taken? | One dose | 31 | 6 |
| Two dose | 2 | 0.4 | |
| Three dose | 29 | 5.6 | |
| Four dose | 54 | 10.5 | |
| Five dose | 372 | 72.2 | |
| I do not know | 27 | 5.2 |
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Distance travelling to health facility | <1km | 270 | 52.4 |
| >1km | 245 | 47.6 | |
| Travelling time from home to health facility | <1 hour | 410 | 79.6 |
| >1 hour | 105 | 20.4 | |
| Availability of TT vaccine service at every health facility | yes | 371 | 72 |
| no | 144 | 28 | |
| Where did you get information about the vaccine? | Health institution | 224 | 43.5 |
| School | 232 | 45 | |
| Media | 59 | 11.5 |
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| ANC follow up | Yes | 409 | 79.4 |
| No | 106 | 20.6 | |
| Number of antenatal visits | 1 | 174 | 33.78 |
| 2-3 | 181 | 35.14 | |
| ≥4 | 54 | 10.48 | |
| Number of children | 1 | 21 | 4.1 |
| 2-4 | 281 | 54.6 | |
| >4 | 213 | 41.4 | |
| Using of modern contraceptive | Yes | 269 | 52.2 |
| No | 246 | 47.8 | |
| Future fertility plan | Yes | 331 | 64.3 |
| No | 184 | 35.7 |
| Variables | Category | <TT2 No (%) |
≥TT2 No (%) |
COR(95% CI) | AOR(95% CI) |
|---|---|---|---|---|---|
| Age of mother | <20 | 224(72.7) | 98(47.3) | 0.25(0.16, 0.38) | 0.19(0.10, 0.32)* |
| 20-30 | 33(10.7) | 19(9.2) | 0.33(0.17, 0.63) | 0.29(0.12, 0.69) | |
| >30 | 51(16.6) | 90(43.5) | 1 | 1 | |
| Distance travelling to health facility | <1Km | 145(47.1) | 125(60.4) | 1 | 1 |
| >1Km | 163(52.9) | 82(39.6) | 0.58(0.408, 0.83) | 0.8(0.49, 1.32) | |
| Future fertility plan | No | 147(47.7) | 37(17.9) | 0.24(0.16, 0.36) | 0.30(0.17, 0.53)* |
| yes | 161(52.3) | 170(82.1) | 1 | 1 | |
| Using of modern contraceptive | No | 158(51.3) | 88(42.5) | 0.7(0.49, 1.00) | 0.66(0.40, 1.08) |
| Yes | 150(48.7) | 119(57.5) | 1 | 1 | |
| Antenatal care | No | 78(25.3) | 28(13.5) | 0.46(0.28, 0.74) | 1.65(0.18, 15.49) |
| Yes | 230(74.7) | 179(86.5) | 1 | 1 | |
| Number of ANC visit | 1 | 126(54.3) | 50(27.6) | 0.25(0.13, 0.48) | 0.38(0.18, 0.82)* |
| 2-3 | 85(36.6) | 98(54.1) | 0.73(0.39, 1.36) | 0.75(0.37, 1.51) | |
| ≥4 | 21(9.1) | 33(18.2) | 1 | 1 | |
| Place to get information | Health institution | 136(44.2) | 88(42.5) | 1 | 1 |
| School | 132(42.9) | 100(48.3) | 1.36(0.74, 2.50) | 1.32(0.59, 2.95) | |
| Media | 40(13) | 19(9.2) | 1.56(0.87, 2.92) | 4.49(1.82, 11.07)* | |
| Mothers educational status | No formal education | 167(54.2) | 79(38.2) | 0.4(0.27, 0.62) | 0.79(0.45, 1.39) |
| Elementary school | 72(23.4) | 48(23.2) | 0.58(0.35, 0.94) | 0.64(0.32, 1.29) | |
| Secondary and above | 69(22.4) | 80(38.6) | 1 | 1 | |
| Husband educational status | No formal education | 161(52.3) | 116(56) | 0.64(0.40, 1.01) | 1.33(0.64, 2.75) |
| Elementary school | 99(32.1) | 37(17.9) | 0.33(0.19, 0.57) | 1.02(0.45, 2.32) | |
| Secondary and above | 48(15.6) | 54(26.1) | 1 | 1 |
3.5. Health Service-Related Factors on Tetanus Toxoid Immunization
3.5.1. Status
Related to traveling time from home to health facility, [410 (79.6%)] of them walked less than 1 hour on foot to reach the nearest health facility. For those who had heard of the vaccination, 88.5% had received the information from either health or school institutions (Table 3).
3.6. Reproductive and Behavioral Factors of Reproductive Aged Women
One hundred and eighty-one [35.14%] mothers attended two to three antenatal care visits, whereas 106 [20.6%] were not participating in antenatal care. Over 40% had more than four children; with [269 (52.2%)] mothers reporting using modern family planning methods and, [331(64.3%)] of them had fertility plans for the future (Table 4).
3.7. Factors Associated with TT Immunization Status (Bivariate and Multivariate Analysis)
In bivariate logistic regression, nine variables showed an association with TT immunization status at P value of <0.2. In multivariate logistic regression, four variables were significantly associated with TT immunization status at a P value <0.05.
Mothers aged less than 20 years old were 81% less likely to receive two doses of TT vaccine injection than mothers whose age was greater compared to 30 years old with [AOR 0.19[0.10, 0.32].
Those mothers who had no future plan for fertility were 70% less likely to receive two doses of TT vaccine injection compared to mothers who had a future plan for fertility with [AOR 0.30[0.17, 0.53].
Mothers who attended one time antenatal care visits were 62% less likely to receive two doses of TT vaccine injection compared to mothers who attended four times and above antenatal care visits [AOR 0.38(0.18, 0.82)].
Mothers who got information from media were 4.49 times more likely to receive two doses of TT vaccine injection compared to those who got information from health institutions with [AOR 4.49(1.82, 11.07] (Table 5).
4. DISCUSSION
This community-based cross-sectional study aimed to determine the status of TT immunization and associated factors. The study identified low utilization of TT immunization among reproductive aged women, while the age of mothers, future fertility plan, number of antenatal care visits and places where information to get were found to be significantly associated with the status of TT immunization.
This study revealed that more than half of mothers were not protected against tetanus at their last birth, which is comparable to findings from the Ethiopian Demographic Health Survey 2016 [11]. This is lower than the WHO target of over 90% and the Ethiopian Ministry of Health recommendations of greater than 90% compliance at the national and greater than 80% compliance at the district level [4, 11, 13]. The finding of this study is also lower than the previous studies, which ranged from 55% to 75.5% compliance conducted in Ghana [10], Kenya [14], Tselemit (Tigray) [12], Pakistan [15], and KembataTembaro [8]. This might be due to a difference in sample size, socio-demographic and topographic accessibility of health services. This low coverage of TT vaccination might be contributed by poor knowledge of women about the disease and the vaccine as evidenced from the finding of this study, though a significant number of mothers know the importance of the vaccine, still many women remain unaware for the prevention of neonatal tetanus. Due to this, a significant number of women are not protected at their last birth for neonatal tetanus, particularly it is worst in rural, low socio economic and who did not receive a formal education. All efforts of extended immunizations and campaigning Tetanus Toxoid vaccinations took place in the country, however, did not bring improvements from the morbidity of neonatal tetanus, perhaps more than 50% of women still gave birth at home in an unsafe, unsterile environment easily prone to the bacteria. Hence forward, empowering and educating women on the importance of the vaccine, severity and fatality of the disease is paramount.
The current study also found mothers whose age was less than 20 years were less likely to receive two doses of TT injection compared to mothers whose age was greater than 30 years. The result was in line with the finding of research conducted in Kembata Tembaro (Ethiopia), Kenya, Vientiane, and India [6, 8, 9]. Possible reasons for this age-related variance may be due to this age group not actively participating in different health-related issues, immaturity concerning taking responsibility for child health care, and lacking past exposure such that they will not develop practical knowledge towards their health care, hard to find them in the involvement of TT immunization.
Those mothers who had no future plan for fertility were less likely to receive two doses of TT injection compared to mothers who had a future plan for fertility. This is consistent with a study conducted in Bangladesh [16]. Mothers who had future fertility plans were aware of taking responsibility for child health care, their health seeking behavior is raised to have a healthy child and those with future fertility plans may use family planning, as health information is given during family planning services due to service integration.
Mothers who attend only one antenatal care visit were less likely to receive two doses of TT injection compared to mothers who attended four or more antenatal care visits. This finding is further supported by research done in Kembata Tembaro (South Ethiopia), Kenya, and Pakistan [8, 14, 15]. Repeated health facility visits for ANC follow-up give an opportunity for TT vaccine injections and avoidance of missed vaccinations.
Furthermore, those mothers who got information from the media were more likely to receive two doses of TT injection compared to those who got information about TT vaccine from health institutions. This might be explained as those who had access to media outlets can receive information without restriction and without limitation and they can be more active and decision-maker about their health care, rather information gained from health institutions may be limited due to poor counseling technique and incompetence of health care providers.
CONCLUSION AND RECOMMENDATION
This study concluded that more than half of the mothers were not protected against tetanus at their last birth. This study also revealed that the age of mothers, future fertility plans, number of antenatal care visits and places where to get information were significant factors associated with TT immunization uptake of mothers. To increase the proportion of mothers protected at birth, awareness creation and immunization campaigns should be directed to school-aged groups, during preconception care, and antenatal care should also be strengthened. Furthermore, more studies are needed to determine the absolute proportion of mothers protected from tetanus at birth by antibody testing.
LIMITATIONS OF THE STUDY
Immunization status was collected, including self-report of mothers; this made it susceptible to recall bias. Though vaccine cards in some of the mothers were reviewed, further institutional card or registration book review was not conducted to those who had no vaccine cards to reduce recall bias.
LIST OF ABBREVIATIONS
| AOR | = Adjusted Odds Ratio |
| CI | = Confidence Interval |
| COR | = Crude Odds Ratio |
| EDHS | = Ethiopian Demographic Health Survey |
| SPSS | = Statistical Package for Social Science |
| TT:Tetanus Toxoid, UNICEF | = United Nations Children’s Fund, WHO: World Health Organization |
AUTHORS’ CONTRIBUTIONS
MeresaBerwo Mengeshawas the principal investigator who contributed to the conception and design of the study, collected, entered, analyzed, interpreted the data, prepared the manuscript and acted as a corresponding author. DestaAbraha Weldegeorges, NatnaelEtsay Assefa, HagosDegefa Hidru, Hirut Teame, Yared Hailesilassie, and Senait Gebreslasie Gebremeskel contributed to data analysis, interpretation and drafted the manuscript. All authors approved the final draft of this manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from a research and ethical approval committee of the College of Health Sciences of Adigrat University, Ethiopia with a code number of ADU/CMHS/855/11.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed written consent was obtained from all study participants.
AVAILABILITY OF DATA AND MATERIAL
The datasets used and/or analyzed during this study are available from the corresponding [M.B.M] on reasonable request.
FUNDING
The source of funding for this research was Adigrat University. The funding organization has no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
CONFLICT OF INTEREST
The researcher declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors of this research would like to thank Adigrat University, Hawzen woreda health bureau administrators, study participants, data collectors and supervisors for unreserved cooperation.


