All published articles of this journal are available on ScienceDirect.
Collaborative Networks in Primary and Specialized Palliative Care in Switzerland - Perspectives of Doctors and Nurses
Abstract
Purpose:
To date, information about collaborative networks of doctors and nurses in palliative care is still scarce, yet of great importance in revealing gaps in collaboration. This paper investigates the collaboration frequencies of medical doctors and nurses within, and across, different settings of palliative care.
Methods:
The study was based on a Swiss national survey on “Collaboration and cooperation in Palliative Care”. The subjects surveyed included service providers in the primary and specialized palliative care sectors, as well as support services (N=1111). Information about ties between providers was gathered by asking professionals to estimate the frequency of interaction with other professionals within the last year, on a daily, weekly, monthly and yearly basis. Social network analysis was used to assess the interaction patterns of nurses and doctors (N= 728) in primary and specialized care settings.
Results:
Visual representations indicated that, contrary to primary care settings, healthcare providers in specialized care settings reported of numerous interactions with other professions. In primary care, general practitioners reported the least frequent interactions with other professions. Of all providers investigated, specialized doctors in hospitals and hospices reported the densest collaborative networks.
Implication:
Gaps regarding collaboration in Swiss palliative care provision were revealed. Based on the results of the study, recommendations on how to improve service quality by strengthening the interaction patterns of general practitioners, as well as community-based palliative care, are provided.
1. INTRODUCTION
According to the definition of the WHO, Palliative Care (PC) is a holistic approach to caregiving, which aims to improve the quality of life of patients and their families in their last stage of life [1]. Over the last decade, several European countries have invested in new strategies, which aim to foster PC, often with the focus of improving the provision of PC in local communities and rural areas [2-4]. Switzerland has followed suit and initiated two national palliative care strategies, which lasted from 2010 to 2015 [5, 6]. Considerable efforts have been made since to promote official regional and inter-organizational PC networks, aimed at improved management, collaboration and coordination of care [7].
Successful PC delivery relies on many professions, their individual expertise and collaborative exchanges across institutions and settings of care [8, 9]. The discipline of collaborative networks, to which this paper refers, is an overarching field, which addresses the structure and dynamics of networks of different organizational units, which interact with each other in order to accomplish common goals [10]. By definition, it is not just a single institution or an individual, but a PC network that is the smallest unit of regional PC [11]. Therefore, it can be reasoned that collaborative networks are the breeding ground for developing sustainable PC structures.
In Switzerland, specialized palliative care (SPC) is offered by highly specialized medical doctors and nursing staff, who provide care in the context of a complex medical and psychosocial treatment system in PC hospital wards, hospices and specialized practices. Primary palliative care (PPC), on the other hand, is typically provided for less challenging patient trajectories, by general practitioners (GPs) and nurses providing care in a home-care setting or in retirement homes [6]. In particular, PC in home care settings requires a stable network of professionals and relatives who work closely together, while the smallest professional PPC network consists of at least one general practitioner and one ambulant nurse [12]. Based on the resources available in the region, volunteer groups, physiotherapists, and pastoral and community social services are part of a PPC network as well.
It is well-known that strong collaborative networking of various medical and supporting professions can ensure cost-efficient, yet high-performance care planning in each of the two care settings [13]. On the other hand, when the formation of strong ties between professionals, especially between doctors and nurses, is being inhibited or coordination regarding the management of complex care provision is impaired, this often leads to negative patient outcomes and additional healthcare costs [8, 14].
Numerous studies have shown that collaborative patterns of healthcare providers do not necessarily follow the given organizational structure, and are often informal. Thus, gaining an understanding of how multiple specialties work together in PC provision is a challenge that should best be undertaken bottom-up [15]. One of the most popular ways to operationalize collaborative networks has been to quantify the number of mutual exchanges of information [16]. To our knowledge, this research paper is the first one to reconstruct collaborative networks of the following key professions working in PC from the bottom-up: (i) GPs in primary care, (ii) nurses in primary care, (iii) medical doctors with additional training in PC (specialists for PC, oncologists and internal medicine) working in hospitals and hospices, and (iv) nurses in PC wards in hospitals and hospices.
2. METHODS
The main aim of this study was to explore the following collaborative networks by counting and presenting visual representations of their interaction frequencies: (i) GPs and (ii) nurses’ collaboration networks in primary care (iii) specialized doctors’ collaborative networks in hospitals and hospices and (iv) nurses’ collaborative networks in hospitals and hospices. In the model, the collaboration frequencies of nurses and medical doctors were reconstructed by depicting their weighted degree of connections to other professional groups.
3. PARTICIPANTS
This study was based on a Swiss national survey on “Collaboration and coordination in Palliative Care conducted on Palliative Care networks in Switzerland”. Regarding inclusion criteria, Healthcare Providers (HCP), who regularly cared for PC patients were eligible to participate. General practitioners obtained a link via email to the online survey through the Swiss association of general practitioners and pediatricians, “mfe”. Other PC providers had to be contacted with the support of various organizations and platforms, such as “palliative.ch”, the Swiss cancer league, curaviva and a wide number of hospitals and local nursing organizations. These organizations sent a link to the online survey to their members and three rounds of reminders were sent out in total. The survey addressed roughly 4,500 service providers in palliative care provision in Switzerland and was available in German, French and Italian languages (N=1111, mean age= 50.91, SD=10.3, f= 64.7%, n.a. = 21.0%). We assume that 21% of the respondents did not want to state their gender in order to maintain their anonymity in all circumstances. However, the anonymity of responders was ensured at all times by coding, which was clarified at the beginning of the survey. A detailed description of the demographic characteristics of the study population is given in Table 1.
3.1. Data Collection and Measurements
A pretest was conducted beforehand using HCP`s from similar fields, and survey items were reviewed for comprehensibility and validity by an expert panel. Data collection was carried out between the 19th of September and the 30th of November 2018. On average, it took participants 25 minutes to complete the questionnaire. An informed consent was needed to be signed by each participant beforehand.
For the collaborative network analysis, participants were asked to provide information about the amount of collaboration with other professions when caring for mutual PC patients, by estimating the frequencies of social interaction with professionals in the last year (2017) on a daily, weekly, monthly and yearly basis (scale: interaction at least once per day, several times per week, at least once per month, several times a year, less, never).
| n | Mean age | Mean work experience in PC in years | Mean no. of patients per year, ambulant/ long-term | |||
|---|---|---|---|---|---|---|
| Nurses in primary care | 323 | 49 +/- 9.4 | 6-10, range: 0-35 | 13.8 / 23.1 | ||
| Nurses in specialized care |
208 | 48 +/- 9.1 | 6-10, range: 0-35 | 116.7/ 128.6 | ||
| Doctors in specialized care | 73 | 53 +/- 9.0 | 16-25, range: 0-35+ | 116.2 / 112.4 | ||
| General practitioners | 94 | 58 +/- 8.6 | 26-35, range: 0-35+ | 21.7/ 19.43 | ||
A study indicated that certain doubts about the validity and reliability of network relationships obtained through self-disclosure are justified, since memories are easily distorted [17]. However, there is evidence that the ability to remember social interactions is particularly problematic when querying short-term interaction sequences, while long-term social structures seem to be adequately remembered [18]. Therefore, we specifically chose a longer time period of 12 months in our assessment, over which interactions had to be estimated. Besides collaborative networks between doctors and nurses in primary and specialized palliative care, the frequencies of social interactions of doctors and nurses with the following professional groups were assessed: members of mobile palliative care teams, psychologists, pastoral carers, social workers, nutritionists, ergo therapists and physiotherapists, pharmacists, volunteers and informal caregivers of patients (usually family or friends). Although collaboration with case managers and music, animal and art therapists has been investigated as well, these marginal groups have not been included in this study. Visual representations of the social interactions in the fields of primary and specialized PC, as well as of mobile care and support services were created.
3.2. Statistical Methods
The method of listwise deletion was used for data cleaning. Although listwise deletion can sometimes affect the statistical strength of the tests conducted [19], in this case, we had a sufficiently large sample size in all four groups, with only a few missing. For the social network analysis (SNA), separate tables in CSV-format were created four times for both the nodes and the edges, by depicting the average of the professions weighted degree of connection to other professional groups. The tables were read with Gephi [20] and traced with Adobe Illustrator for visual representation. Additionally, descriptive frequency distributions of the individual social interactions were counterchecked with histograms. Interaction frequencies have not been adapted to differing patient numbers in the different occupational fields since the primary aim of this study was to reconstruct true-to-life collaborative networks of nurses and doctors in both community and specialized palliative care.
4. RESULTS
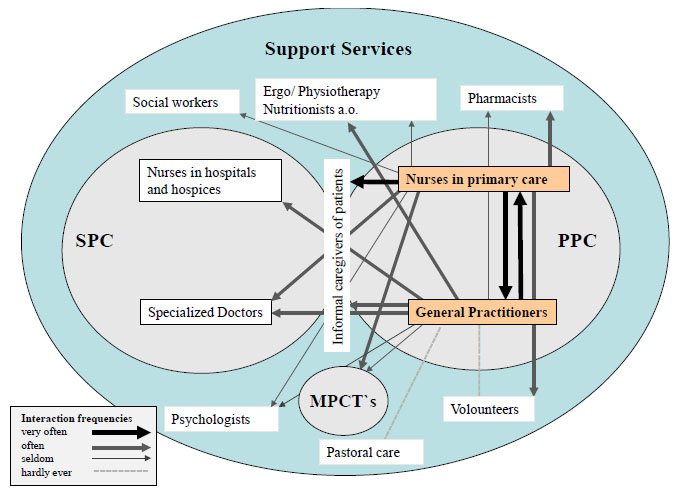
Visual representations of interaction frequencies of GPs and nurses in PPC are reported in Fig. (1). Fig. (2) shows collaborative networks of medical doctors and nurses in SPC.
Fig. (3) shows the strongest ties in the collaborative network and provides a summary of external factors that influence collaboration. It displays the main finding of this study, namely that considerably higher amounts of interactions originate from HCPs working in SPC, then from HCPs working in PPC.

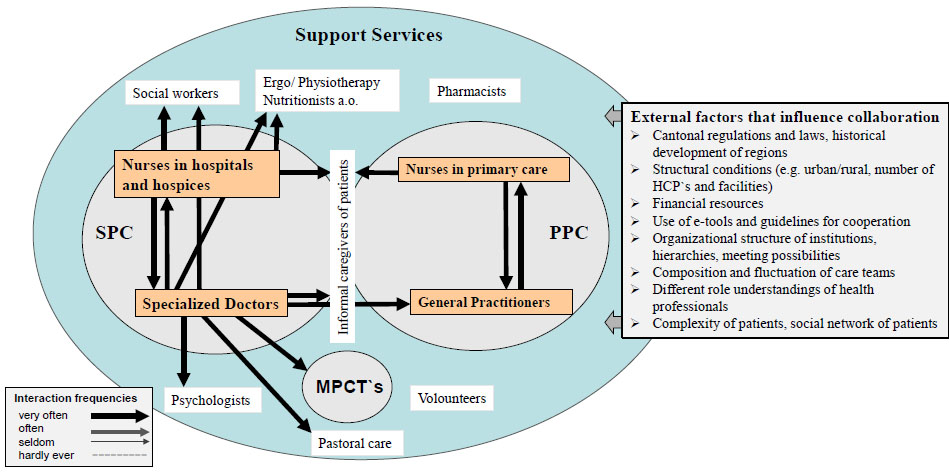
Since the organizational functioning of healthcare organizations can be limited by various other barriers to collaborative network building, a number of further external factors that strongly influence collaboration of PC providers in Switzerland have been identified via a literature search. Those are, amongst others, different regional regulations and policies, the historical development of the regions, structural conditions (e.g. urban vs. rural areas, number of specialized facilities, number of GPs etc.), financial resources and lack of reimbursement for coordinative tasks, the use of e-tools and guidelines for cooperation, the organizational structure of institutions, varying hierarchies within work teams, the composition and fluctuation of care teams, different role understandings and assignments of HCPs, and lastly, the social network of patients [8, 9, 13, 14, 21-23].
In PPC (Fig. 1), GPs reported comparably low interaction frequencies with other professionals and only reported daily contact with nurses. Interactions with relatives, doctors in specialized practices, specialized doctors in hospitals or hospices and physiotherapists and allied professions occurred at least a few times per week. Mobile palliative care services (MPCTs) and psychosocial professions seem to be of subordinate importance in the GPs’ professional networks when caring for PC patients. GPs particularly reported little to no contact with pastoral carers, psychologists and volunteers.
In contrast to GPs, nurses in primary palliative care reported a much higher frequency of interaction with other HCPs and relatives. Nurses in the primary palliative care sector were in contact with relatives, other nurses and GPs on a daily basis when caring for PC patients. Moreover, they collaborated with some supporting services, such as pharmacists or social workers, several times per month. Nurses in PPC were hardly ever in contact with psychologists, pastoral carers and physiotherapists.
Looking at the sphere of SPC (Fig. 2), nurses showed significantly higher frequencies of collaboration with other professions than nurses in PPC. They reported very high (daily) frequencies of collaboration with a lot of different actors, such as doctors and nurses from SPC, relatives, psychologists, pastoral care and various support services when caring for PC patients. Further, they reported contact with GPs, nurses from PPC, MPCT`s and volunteers on a weekly basis. Interestingly, most well-connected participants investigated in this study were medical doctors who worked in hospitals and hospices [Fig. 2]. They stated that they were in close contact with numerous people from the listed professions on a daily basis, except for volunteers and pharmacists.
In summary, the reconstructed networks showed that HCPs in SPC shared considerably higher interaction frequencies with a large number of HCPs than was the case for doctors and nurses in PPC. Within both fields, doctors and nurses appeared to be very well connected to each other; however, at the interfaces of SPC and PPC, there was room for further improvement of professional networking. By far, as measured by the self-statements, the least well-connected group was that of GPs, who indicated a significantly lower degree of networking than the other three investigated professional groups. GPs showed especially low interaction rates with support services.
5. DISCUSSION
The main findings of the study revealed strong networks within the two fields of SPC and PPC, but rather weak ties between the two fields, as well as limited contact of GPs with other HCPs in PC, especially support services.
One of the main results of our study showed that both doctors and nurses working in a hospital or hospice reported more interactions with other HCPs than doctors and nurses in PPC.
This is in line with a study by Wensing and colleagues, who investigated the collaboration of HCPs for Parkinson patients, and found that professionals working in PPC showed significantly lower frequencies of interaction with other care professionals than those who were working in a hospital [24].
The main reason for this lies in the fact that fixed organizational structures are more present in certain fields of SPC, which facilitate interprofessional collaboration through predetermined exchange mechanisms, such as case discussions, round tables and supervisions [25, 26]. Furthermore, hospitals and hospices usually feature detailed guidelines and standards as well as training programs, which are known to foster inter-professional collaboration, and which challenge traditional role models and hierarchies [25]. Previous studies also found that the mere geographic proximity of healthcare suppliers in hospitals and hospices leads to higher frequencies of interaction since logistic interconnections are easier to make when HCPs are more visible to each other [27].
Contrary to doctors in SPC, GPs reported limited contact with members of MPCT teams, pastoral care teams, psychologists, volunteers and pharmacists when caring for PC patients. Some of the reasons for low interaction frequencies originating from GPs in this study might include the lower complexity levels of patients in PPC, GPs’ unfamiliarity of fellow HCPs and psychosocial services, as well as less use of e-tools, less possibilities for inter-professional exchange and insufficient remuneration for collaborative tasks [28-30].
However, strengthening GPs’ collaborative interactions with other professions in PC is vital, since up to 80% of all PC patients in Switzerland are currently being treated in primary care [6]. A Swiss population survey from 2017 reports that GPs are the first point of reference for 72% of responders with palliative care needs [31]. Being the first point of reference for a majority of the population, it is essential for GPs to be aware of the wide range of palliative care services available, including psychological and pastoral care. Besides physicians, who are strongly linked to their external professional environment are also associated with better clinical performance [32].
The authors suggest that inter-professional collaboration of GPs should be fostered by establishing standardized communication structures appropriate for the setting of PPC, which specifically caters for the needs of GPs and nurses working in ambulant settings. Shared online tools for reporting and assessment do not only promote common ground between various professional groups in the same area but reduce the barriers for GPs of reaching out to unknown colleagues or professionals. This is supported by a study from Australia, which demonstrated that GPs that frequently used information technologies and e-tools revealed sustainable network structures and stronger ties to other professional groups in healthcare, which in turn resulted in better clinical performance [33].
The authors further suggest that the services of specialized MPCTs should be further promoted and strengthened from a professional basis, in order to fill in gaps in provision, and to facilitate high-standing PC provision in the community and in remote areas. Not only are MPCTs needed for GPs and informal caregivers to consult with when challenging decisions have to be made, but they might serve as an effective coordinating interface between SPC and PPC in the future, since MPCTs are mostly commissioned by, or affiliated with, hospitals and hospices [34]. MPCTs are not yet available comprehensibly throughout the whole country of Switzerland; however, it is to be expected that these services will be expanded in the near future [35].
One of the main barriers towards more interprofessional collaboration in PC concerns overall healthcare reimbursement. Previous research indicated that especially the collaborative services of GPs are not adequately remunerated if they concern activities apart from immediate contact with the patient [30]. However, GPs should ideally be able to take their time to consult with, and refer patients to other HCPs and allied services, as well as to advise family members on important decisions [30]. Recent literature suggests that the number of GPs who are willing to do home-visits in Switzerland is declining, which could be a hint of dissatisfaction with their reimbursement for time-consuming responsibilities [28, 36]. Therefore, new concepts for remunerating GPs’ collaborative activities are required to foster collaborative activities in PC within Switzerland.
Last but not least, experts from the field have recommended the development of innovative, community-based and community-owned models that facilitate palliative care delivery to patients in a home care setting [37, 38]. These community networks are typically built up by residents in close cooperation with healthcare facilities while following certain educational and ethical standards that strengthen the resident’s capacity to provide appropriate PC at home [38-40]. Community-based care networks can consist of, amongst others, family members, neighbours, case managers, local organisations, faith groups and volunteers with special training in PC. Evidence suggests that community-networks for PC are not only cost-saving and sustainable, but they also relieve the workload of HCPs working in PC and promote patients` autonomy at the end of life [38, 40].
CONCLUSION
This study has provided insight into collaborative patterns of doctors and nurses in primary and specialized PC provision in Switzerland. Examples on how to improve service quality by strengthening the interaction patterns of GPs, as well as community-based palliative care, are provided.
This information is relevant in order to plan healthcare provision more efficiently, by highlighting possible shortcomings in inter-professional communications. It is important to emphasize that each individual network of palliative care providers may substantially differ from the visual networks portrayed in our study. Compared to other medical areas, much more variance can be expected regarding the professional network building of HCPs in PC [22]. This is mainly due to the complex care situation of PC patients, who require an individually tailored treatment plan according to their present physical and psychosocial needs. Depending on the severity of the patient’s condition, frequent transfers between, and within SPC and PPC settings may occur, which are a major contributing factor to the changes in professional network formation [13].
This research did not aim to directly compare the quality of collaborative networking between the two areas of PPC and SPC. This claim cannot be fulfilled, since the two areas handle different numbers of patients and treat patients with different degrees of severity.
Self-reported measures, as used in this study, can have certain disadvantages, such as an increased probability that events or interactions are not being recalled correctly. Thus, over or under estimation of interaction frequencies are possible and the question arises as to whether the survey primarily measures the actual, or subjectively perceived, professional networks. Nevertheless, literature suggests that effects on the behavior of individuals can be expected in both cases [41]. For future social network studies in healthcare, the authors recommend an observational approach in order to avoid self-ratings. Moreover, future research should aim at analyzing the impact of frequency of collaboration of HCPs on patient outcomes, as well as on data security. External factors, which influence collaborative networking on an individual level, should be taken into account as well.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the the Ethics Committee of Northwestern Switzerland (EKNZ) on the 29th of August 2018 (Req-2018-00490).
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [R.S], upon reasonable request.
FUNDING
The study was funded by the Swiss National Research Foundation SNF within the National Research Programme NRP 74 "Smarter Healthcare", grant No. 167345.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors thank Eveline Degen for her assistance in conducting this research and all participating healthcare providers for their contributions.


