All published articles of this journal are available on ScienceDirect.
Attitudes of Pregnant Women Towards Antenatal Care Services Provided in Primary Health Care Facilities of Mbombela Municipality, Mpumalanga Province, South Africa
Abstract
Background:
Pregnant woman’s personal experience of antenatal care services can either be positive or negative; however, knowledge and experience appear to be of paramount importance in shaping their attitudes towards any healthcare-related services. This implies that women's experience of antenatal care services may affect their decision for seeking antenatal care in their present pregnancy, which can lead them to delay seeking care.
Purpose:
This study sought to explore the attitudes of pregnant women towards antenatal care services provided in primary health care facilities of Mbombela Municipality, Mpumalanga Province, South Africa.
Methods:
A qualitative exploratory descriptive study design was used for this study. Purposive sampling technique was used to sample pregnant women who fail to attend antenatal services as expected. Data were collected through face to face unstructured in-depth interview. A total of eighteen pregnant women participated in the study until data saturation. Data were analysed using Tech’s method of analysis.
Results:
Results revealed the following theme and sub-themes: Attitudes of pregnant women related to individual perceptions, perceived barriers to utilizing antenatal care services,’ attitudes of healthcare providers, long waiting times in healthcare facilities, lack privacy and confidentiality in healthcare facilities and attitudes of pregnant women related to attendance of antenatal services.
Conclusion:
Attitudes of pregnant women about antenatal care are shaped by their knowledge and previous encounters with the health care services that they had previously received. It is therefore important to provide women-friendly services. It is recommended that health education regarding the importance of antenatal care services must be given to all women daily in the waiting areas of each primary health care facilities, thus, the healthcare providers should promote the active participation of pregnant women during the health education sessions and provide opportunities to ask questions.
1. INTRODUCTION
Women’s perceptions of what quality of healthcare entails do not always coincide with the technical definitions used for quality, thus, women may express some preferences towards treatment or intervention that are inappropriate or unnecessary given their experience with previous exposures. For example, a study in Indonesia found that women preferred to use the services of birth attendants, who hurried the delivery by using oxytocin to increase contractions [1]. In a qualitative study conducted in Tanzania, findings indicated that women do not perceive significant health threats during pregnancy and viewed more than one antenatal care visit as unnecessary [2]. Women perceive labour and delivery as a time of significant health risks that require drastic medical attention. Most women’s primary reason for seeking Antenatal Care (ANC) had been the ability to receive an ANC attendance card that is required to deliver at the health facility [2, 3].
1.1. Perceived Barriers to Antenatal Care
The lack of information and knowledge towards sexual and reproductive health (SRH) and rights contributes to women delaying or avoiding attending ANC services. A paradox was highlighted in the findings of a study conducted in Mpumalanga and Kwazulu-Natal [4]. Pregnant women had not received information about the importance and values of attending ANC in Primary Health Care (PHC) facilities. Furthermore, it was stated that for many women, fear related to lack of privacy and confidentiality within the PHC facilities resulted in them not willing to visit their local clinics, which made them reluctant and led them to delay seeking ANC [4-6]. Antenatal care services must be made attractive to women. This can be achieved by the way pregnant women are treated during ANC visits. If a woman was once treated offensively in a healthcare facility, the probability of that woman returning to that facility is very low and she may not be passionate about any instructions provided to her during her visit at that clinic, should she choose to revisit [7].
1.2. Awareness and Acceptance of Pregnancy
The ability of pregnant women to identify and accept that they are pregnant has been said to be one of the causes of the delay in seeking ANC services [2]. Furthermore, younger women are most likely to delay accessing ANC until late in the second trimester simply because they were unaware of typical pregnancy indicators [2, 8, 9]. Recognition of the signs and symptoms of pregnancy was often made by relatives, partners or other community members [10]. Many women struggle to accept their situation, especially if the pregnancy is unplanned, as they feel they are not prepared to make changes in their lives and they spend much time considering termination of pregnancy [11-14]. Lack of support, disapproval and reaction from family members, partners or community members have a significant effect on women’s willingness to accept their pregnancy [4, 9, 15-17].
1.3. Accessibility of Antenatal Care Services
In terms of Section 27 of the South African constitution, everyone has the right to have access to healthcare services, including reproductive health [18]. All health facilities and their services should be well known to all people, must be affordable for all individuals and be within safe and physical reach for everyone, especially the marginalised groups [19-22]. Although it was declared in 1994 that healthcare provided for children under six years and pregnant women would be for free in South Africa, the legacy of inequalities in terms of gender, race, geographic and health systems created from the apartheid era continues to have an impact on the health of women living in South Africa [4].
Costs diminish the potential for women to access ANC services early and regularly. The inability to travel to and from ANC facilities may put a strain on the limited financial resources of women from relatively deprived communities who then find ANC services difficult to access [23]. Access to ANC services is a critical factor, especially in low and middle-income countries.
In a study conducted in Pakistan, a significant relationship between wealth and institutional delivery, and the effect of wealth led the authors to conclude that many Pakistani women chose to deliver at home because of their inability to pay the high cost of delivery at a healthcare facility [24].
Although in South Africa, pregnant women access health services for free in public PHC institutions, in 2013, the South African Human Rights Commission (SAHRC) found the Mpumalanga Department of Health in violation of the constitutional rights of women to access healthcare services and the right to dignity. Reasons given for these findings were that there were ineffective management structures and infrastructure, inadequate access to PHC facilities and insufficient human resources required to deliver quality healthcare services [4].
The Demographic and Health Survey (DHS) shows that 94% of all pregnant women attend ANC facilities at least once. It further states that ANC coverage is worst in poor areas and best in urban areas. However, the urban or rural location has no impact on the attitudes of pregnant women to health programmes [25].
1.4. Privacy at Facilities Including Fear of HIV Testing
Healthcare personnel is trained to respect privacy and to practice confidentiality with their patients; no one is subjected to procedures or treatment without their full consent [18, 26]. A study conducted in Kwa-Zulu Natal and Mpumalanga revealed that pregnant women fear that healthcare workers will not keep their HIV status confidential, they perceive HIV testing to be mandatory and fear that if they refuse to be tested, they will be denied access to ANC services [4]. This is because they are concerned about how to share the information with partners and families, also, they fear discrimination, stigma, abandonment and other social and medical consequences of living with HIV [4].
The study aimed to explore the attitudes of pregnant women towards ANC services provided in Primary Health Care (PHC) facilities.
2. METHODS
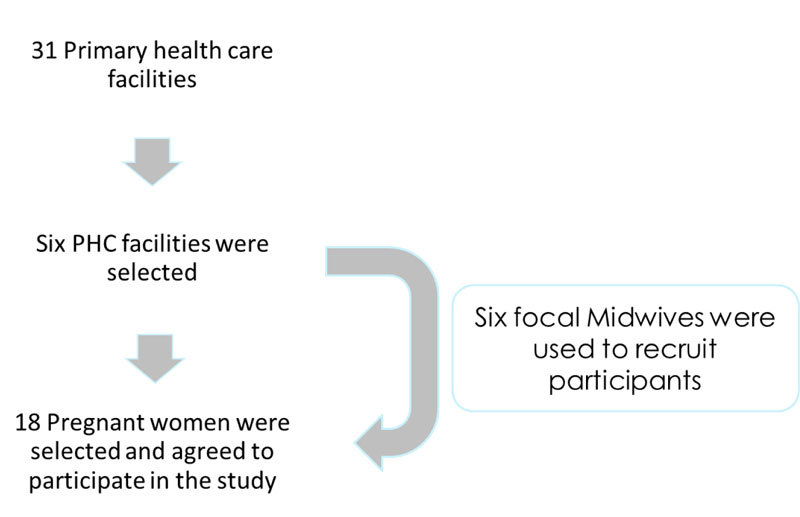
A qualitative, exploratory-descriptive design was used to explore the attitudes of pregnant women towards ANC services provided in Primary Health Care (PHC) facilities. The study setting was PHC facilities in Mbombela Municipality, Mpumalanga province, South Africa. Mbombela Municipality has two district hospitals and 31 Primary Healthcare facilities, of which six of them are where the study was conducted. The six PHC facilities selected were those found in the deep rural areas as it was assumed that communities in those areas still have strong cultural values and norms. Mbombela Municipality was reported in 2018 to have the highest number of maternal deaths in Mpumalanga Province [27]. The use of cultural practices could be a contributing factor.
2.1. Participants
The population comprised of all pregnant women attending ANC at the PHC facilities of Mbombela Municipality. The targeted population was inclusive of pregnant women who fail to attend ANC services as expected. Pregnant women were interviewed in their natural setting. Six professional nurses from the selected six primary healthcare facilities identified the participants who failed to attend ANC as expected. The researchers contacted the participants telephonically and those who agreed signed informed consent and date for the interview was identified Fig. (1).
2.2. Data Collection
Data were collected through face to face interview using an open-ended unstructured central question which was, “what are your attitudes towards ANC services provided at the PHC facilities?”. Probing, follow up questions and paraphrasing were used to deepen the discussions. Observations and field notes were made. An audiotape was used to capture the discussions. Data were collected in Isiswati because all pregnant women were comfortable discussing in their home language. A total of eighteen pregnant women participated in the study until data saturation.
3. MEASURE TO ENSURE TRUSTWORTHINESS
Measures to ensure trustworthiness using the following criterion was ensured: Credibility was ensured through prolong engagement with participants as contact with participants was maintained before, during and after data collection. Persistent observation of all data processes and non-verbal cues were done. Peers were consulted and the audio recorder was used, and data were presented to participants for verification. Transferability was ensured through the dense description of the setting and by the use of purposive sampling of the participants. Conformability was maintained by the use of qualitative design where the data represent the information provided by the participants. A tape recorder was used to record the in-depth individual interviews, the research methods were well planned to ensure the audit trail. Dependability was ensured by exposing data to the external reviewer/independent auditor. Data was also coded and recorded by the researcher, independent coder, and supervisors to ensure consistency.
4. RESULTS
The study was carried out in selected six primary healthcare facilities of Mbombela Municipality. Three pregnant women participated in each of the selected facilities, with a total of eighteen women participating. The age of the participants ranged between 18 and 38 years. There was no association between the age and the knowledge of pregnant women about ANC, as many of the participants booked late and they gave vague explanations about the procedures of ANC. The average time spent on the interview was 45 to 60 minutes. Analysed data yielded the following theme and sub-themes as reflected in (Table 1): attitudes of pregnant women related to individual perceptions; perceived barriers to utilising ANC services; healthcare workers’ attitudes; long waiting times in healthcare facilities; lack of privacy and confidentiality in healthcare facilities and attitudes of pregnant women related to attendance of ANC services.
4.1. Theme: Attitudes of Pregnant Women Related to Individual Perceptions
In the study context attitude refers to pregnant women's effective feelings of likes and dislikes towards the ANC services. The attitudes of pregnant women were assessed about how they perceive ANC services, procedures, the importance of ANC services and their health-seeking behaviour. Pregnant women’s perceptions regarding pregnancy or their personal experiences relating to ANC services determine their attitudes towards the services. The pregnant women’s previous or current experience to ANC services can be positive or negative. The women had negative attitudes towards the healthcare providers which could have affected their attendance at ANC facilities. Healthcare workers’ attitudes play a great role in determining how pregnant women perceive ANC services and bad attitudes form a barrier for utilising ANC services.
| Attitudes of pregnant women related to individual perceptions | Perceived barriers to utilising ANC services • Healthcare workers’ attitudes • Long waiting times in healthcare facilities • Lack of privacy and confidentiality in healthcare facilities |
| Attitudes of pregnant women related to attendance of ANC services |
4.2. Sub-theme 1: Perceived Barriers to ANC Services
Possible barriers that prevented women from attending ANC facilities were raised during the interviews. Among other matters which were of concern in the study area were the nurses’ attitudes towards patients, long queues in clinics, lack of privacy and patient confidentiality.
4.2.1. Healthcare Workers’ Attitudes
All women have the right to be treated with respect and dignity. The care which is provided to them should be provided in a respectful and dignified manner. Most of the participants (n=11) mentioned that one of the things that put them off from visiting healthcare facilities or made them delay ANC was the nurses’ attitudes. The women said that they were sometimes badly treated by the nurses.
“Sometimes there are things that we don’t like when we come here, like the nurses shouting at us because we come here looking for help but the nurses are moody sometimes…this is my second pregnancy, I have been attending ANC here, the nurses at this facility are moody especially the ones working at maternity section. I had to go and attend another clinic because of their attitude but because one of the nurses knew me from the other facility they told me to come back here since I have a file here…I had to take a taxi and go attend there to avoid what is happening here because you see now we have been here since morning but we will leave here around five in the evening. These things affect us a lot because sometimes you feel like you can just leave without receiving any assistance” (Participant 6).
This was reiterated by another participant:
“We are scared of asking the nurses anything since most of them they answer you with an attitude when you ask something. Most of them they frown when you ask them questions so you become scared to ask them because you tell yourself that she/he will not answer you well. They get angry especially if they see that we are many, they start saying things like these patients are so many when are we going to finish working and they get angry, you even get scared of telling them your problems. We end up going to the private pharmacy and buy medications there” (Participant 8).
Another participant added that:
“We do not ask anything, we are scared because some nurses are rude, they do not answer you well when you ask them questions, so we just keep quiet, this is my third pregnancy and things have been like this”(Participant 1).
4.2.2. Long Waiting Times in Healthcare Facilities
In addition to the unacceptable healthcare workers’ attitudes, the pregnant women (n=15) mentioned that the long waiting times in healthcare facilities kept them from visiting ANC facilities or made them delay seeking maternal healthcare since they did not have time to wait for long hours at the healthcare facilities as they had other important tasks to do. In all the facilities that were visited, the pregnant women were very disappointed with the time they spent in facilities before they could receive assistance or be seen by a healthcare worker. This could result in them seeking ANC late. Several women mentioned that they preferred using private doctors but owing to the lack of financial support, they couldn’t afford it. Some pointed out that owing to the occasional long waiting times they felt they left without receiving the services.
“They need to improve, we come here early in the morning but they attend us very late, we get mixed with people who are sick while we on the queue but they attend the problem in time, we stay here for longer, we arrive early in the morning and leave late and things change every time we come here. Last we had our own queue to follow as ANC patients but now we mix with everyone who comes here even with those who are sick. Now it is eleven, but we have not received help yet since we got here at 7 o’clock” (Participant 15)
“You come here early in the morning around six o’clock and you will receive help at five o’clock in the evening. The nurses here take their time to assist us, they go for their tea breaks, lunch breaks and even change shifts while we are just sitting here” (Participant 9).
4.2.3. Lack of Privacy and Confidentiality in Healthcare Facilities
Patients have a right to privacy and confidentiality. Healthcare workers are trained to respect the privacy of patients; they have to ensure that a patient’s privacy and confidentiality are protected and that information on the health status of the patient is not disclosed to third parties without the consent of the individual. One of the factors that delayed women from visiting ANC facilities was found to be a lack of privacy and confidentiality, especially when visiting facilities nearer to home. This was verbalised in this way:
“…I ran away from Clinic X because there was a nurse who did not keep my status confidential. I did not attend the clinic because of a certain reason and she just came in front of everyone at the queue and asked me why I didn’t come to the clinic because now my baby has missed the nevirapine dose that he was supposed to get, that did not sit well with me. I became pregnant when my first baby was still young and the nurse asked me why was I back at the clinic so soon and she said that in front of everyone, the other people didn’t know that my baby was still young. Now I ran away from that clinic and I have to take a taxi all the way to attend this clinic. There is no privacy there, I wish the department can put cameras so they see how they treat us, they don’t know how to speak to people, from the matron to the staff. There is another woman outside who also ran away from that clinic because there is no privacy. We come here because no one knows us here so no one can judge us” (Participant 4).
Privacy is a key requirement for women seeking ANC services. Lack of privacy during physical examinations and counselling processes brings a sense of shame and discomfort to women and leads to poor adherence or dissatisfaction with the services. Hence these women prefer to consult private doctors; owing to the financial constraints, it becomes difficult for them and they delay the initiation of ANC at health facilities.
“When we go inside the consulting room they tell us to undress and they start pressing your tummy [sic] but they don’t have a machine to check the baby (frowning) eish they tell us to be naked and I don’t think that it’s supposed to be done…I don’t like it because when you go to the doctor they don’t tell you to be naked and there is no privacy here because we go inside the room being two or three women at the same time and they do it every time we come here” (Participant 1).
Women rate the quality of care provided to them according to how they are treated during their visits. Improving the quality of ANC services should be the leading priority in Mbombela primary healthcare facilities. Improving ANC services is most likely to contribute to the increase in women seeking ANC earlier in pregnancy.
4.3. Sub-theme 2: Attitudes of Pregnant Women Related to Attendance of ANC Services
Findings revealed that pregnant women (n=9) had an unfavourable attitude towards ANC services since they did not like attending ANC or visiting the health facilities repeatedly. This led them to feel that ANC was unnecessary since they perceived that pregnancy is a normal physiological process and not some sort of sickness.
“I have not seen anything that ANC has helped me with because you just come here they check on you and give you medication after that you go home, they don’t even ask you if you are fine or not. I think that we should just stay at home and start attending when we are about to give birth, I don’t see the importance of coming here earlier” (Participant 10).
“I come to attend because of the ANC booklet/maternity case record because if I don’t come, I will not have it and they want it when you come for childbirth” (Participant 1).
“Coming to the clinic it is useless because you just come here and they palpate your abdomen nothing more, at least at the private doctor because they have a sonar machine to check if your baby is fine. We just come here because we don’t have money to consult in private facilities. Here it is just a waste of time because they don’t see if the baby is having abnormalities, how are they going to identify the abnormalities by palpating my abdomen? We come here because there is a medication that we need to take, and they also give us injections to help the baby to develop. But it is also useless because you get the medication and you don’t even know what it is for unless you are educated then you can know which is what” (Participant 9).
5. DISCUSSION
Women sought ANC mainly to check their HIV status since they believed that they are susceptible to the virus and wanted to prevent transmission to their unborn babies. Some who attend do so to obtain maternity case records because they believe that they won’t be helped when they go to the facility to give birth without it. The reason why pregnant women visited ANC facilities late was reported to be due to the nurses’ negative attitudes towards pregnant women [28]. In the 2012 audit of health facilities, only 30% of healthcare facilities were found to comply with the criteria for positive and caring staff attitudes nationally, and 25% in primary healthcare facilities [29]. This shows that there is still great work that needs to be done in terms of improving nurses’ attitudes and compassionate care. Antenatal care must be made attractive to the pregnant woman and all females in general as this can promote and stimulate their willingness and desire to be part of the ANC services. This can be achieved through the way pregnant women are treated during their ANC visits. If a pregnant woman is treated badly during her ANC visit, the likelihood of her not returning to the facility is very high and she may not be enthusiastic about the instruction given to her at the clinic [7]. The negative attitudes of pregnant women may result from previous pregnancy experiences. The researcher maintains that it is not likely for women to seek ANC if they perceive pregnancy danger signs to be harmless or to be of no importance. However, how pregnant women react when they experience danger signs depends on whether they are aware and possess the knowledge of danger signs and if they are aware of the risks that are involved if not treated.
This is in line with the findings from a Tanzanian study which reported that the lack of maternal health information at healthcare facilities led to most of the pregnant women not aware of benefits and having negative attitudes toward the quality of maternal health provided during ANC visits [30]. These negative attitudes toward ANC services may be a result of the poor provision of maternal services. A pregnant woman who experiences a bad attitude will share her uncomfortable experience with her peers and community members and that will lead pregnant women to delay seeking ANC [31]. Hence the provision of quality maternal services in rural areas is key to increase utilisation because once pregnant women are satisfied with the services, they receive the more likely they are to change their attitudes towards healthcare services [32].
Owing to the poor service provided to pregnant women during their visits, the reputation of the health system gets compromised. This was emphasized by a Tanzanian study that reported that poor birth experiences undermined the reputation of the health system, lowered community expectations of the efficacy of delivering in a healthcare institution and contributed to the high number of home deliveries. Women who had experienced poor-quality services had low trust in health facilities and were pressured to deliver at home [33].
The researchers argue that if pregnant women were provided with proper health education and were made to understand the importance of ANC their attitude would be favourable towards ANC services. This calls for intensive health education about the benefits of ANC. The knowledge that pregnant women have regarding ANC determines how they think or feel about ANC services. If they have proper knowledge regarding the danger signs or complications that may arise during pregnancy, they would develop favourable attitudes towards ANC services and start ANC earlier in pregnancy to avoid complications.
Additionally, fear of breach of the right to privacy by health care workers can also have financial implications, as some people feel that they must attend a clinic further from their home to minimise the chance of meeting someone they knew. In confirmatory, KwaZulu-Natal and Mpumalanga struggled to achieve maternal health goals and the main cause incorporated barriers to ANC (Amnesty International (2014) [4]. Many women and girls who were interviewed said that their fears about lack of privacy and patient confidentiality in health facilities which prevented them from visiting their local clinic and promoted their reluctance towards access sexual and reproductive services. Consequently, it led pregnant women to delay seeking ANC services. Evidently, some of the primary healthcare facilities that the pregnant women visited were in unsuitable buildings which lacked privacy, the rooms were small and overcrowded making it impossible to protect the patient or client confidentiality.
CONCLUSION
Based on the findings from this study, it is recommended that to improve the knowledge and attitudes of pregnant women regarding ANC, materials such as pamphlets or brochures and other forms of media (television, radio) should be made available to pregnant women to enhance their knowledge and raise awareness about the importance of ANC services; health education regarding ANC services must be given to women every day in the waiting areas of healthcare facilities, thus, the healthcare workers should promote the active participation of pregnant women during the health education sessions and provide opportunities to ask questions so that they can identify the level of the women’s knowledge; workshops and training should be conducted for healthcare workers to improve those observed weaknesses which were barriers to the utilisation of ANC services; and that traditional practitioners should be involved in maternal healthcare programmes so that they can be equipped with information to improve their skills needed for maternal care.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The ethical approval was provided by the University of Venda, South Africa with the reference number SHS/ 16/PDC/37/0802.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants in the research.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [L.M], upon reasonable request.
FUNDING
The study was funded by the University of Venda, Research and Publication Committee (RPC) with grant no.SHS/16/PDC/37/0802.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors thank all healthcare workers for their assistance and the participating pregnant women for their contributions.


