All published articles of this journal are available on ScienceDirect.
A Systematic Review and Meta-analysis of Depression in Postpartum Women in a Low-income Country; Ethiopia, 2020
Abstract
Background:
Maternal mental health in the postpartum period is essential for the optimal development of the newborn. Despite this, a shortage of concrete evidence exists regarding it.
Methods:
PubMed, Scopus, and EMBASE were investigated with no time limitation. A manual search for a reference list of articles was also done. Relevant data were extracted using the Meta XL package and analysis was done using Stata-11 meta-prop package. Heterogeneity was checked with Cochran's Q-statistics and the Higgs I 2 test.
Results:
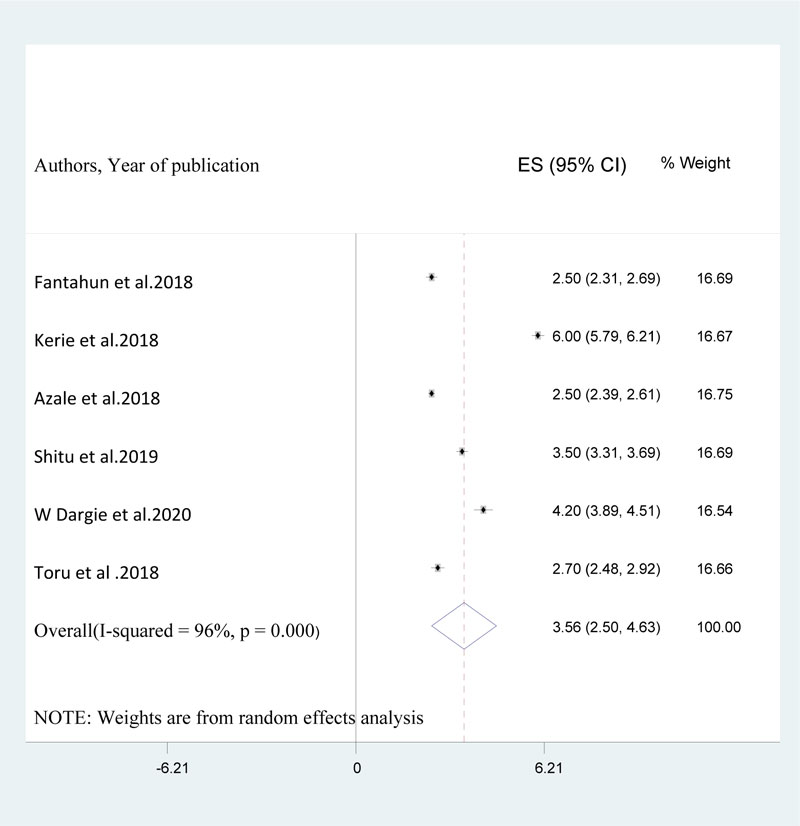
Sixteen studies were included. The average prevalence of postpartum depression was 21.9%. The pooled prevalence was found to be higher in studies assessed with SRQ-20, i.e 24.6% than studies assessed using PHQ-9, which was 18.9%. Moreover, the pooled prevalence was slightly higher in southern Ethiopia (22.6%) than Addis Ababa (21.2%). Poor marital relation (pooled aOR= 3.56) (95% CI: 2.50, 4.63), unplanned pregnancy (pooled aOR=3.48) (95% CI: 2.18, 4.79), previous history of depression (pooled aOR= 4.33) (95% CI: 2.26, 6.59), poor social support (pooled aOR= 4.5) (95% CI: 3.34, 5.56), and domestic violence were among the associated factors for postpartum depression.
Conclusion:
More than one in five women were found to have postpartum depression and factors such as poor marital relations, history of depression, poor social support, domestic violence, and unplanned pregnancy were observed to be associated with it. Therefore, maternal postnatal care services should integrate this essential health concern.
1. BACKGROUND
Women with depression in the postpartum period show manifestations like sleep disturbance, change in appetite patterns, feeling of sadness, recurrent guilty feeling, crying, low energy, and unease feelings of anxiety and suicidal ideas [1]. Nowadays, postpartum depression plays a major role in the burden of disease among women of 15 to 49 years of age [2]. Globally,10-20% of postnatal women develop depression at one point in time [3]. A survey by the World Health Organization (WHO) identified that 20-40% of childbearing women in the developing world sustained depression in the antepartum and postpartum period at a given time [4]. Besides, 19% of postnatal women in low and middle-income countries [5, 6] and one among twenty postnatal women in Ethiopia [7] develop postpartum depression.
Different studies across the world have reported different prevalence rates for postpartum depression.
A systematic review and meta-analysis study in 2018 by S Shorey et al. [8] reported the worldwide estimated prevalence of postpartum depression to be 17%. Besides, a study that assessed 34 studies reported that 19.8% of postpartum women have a common mental disorder [9]. Furthermore, another study that incorporated 38412 women and 23 studies in low and middle-income countries [6] reported 19.2% of women as having postpartum depression. Another systematic review and meta-analysis study in India which assessed 38 studies reported a pooled prevalence of postpartum depression to be 22% [10]. Moreover, other individual studies reported earlier showed that the prevalence of postpartum depression was 17.6% in Portugal [11], 27.3% in China [12], 61.4% in Korea [13], 18.6% in Qatar [14], 34.8% in Iraq [15], 34% in Jamaica [16], 15.4% in Turkey [17], 13.5% and 10.3% in Oman [18], 31.7% in South Africa [19], and 43% in Uganda [20]. In Ethiopia, the preva- lence of postpartum depression varies between 12.2% to 33.8% [21-36].
Poor social support [37], poverty [38], and childbirth without the presence of relatives [39], history of depression [40], and poor woman autonomy [41] due to socio-demographic variables, multi-parity [42], prime-parity [43, 44], multiple children at home [45], negative attitude toward one's pregnancy [22, 46-49], depression during pregnancy [42, 50], premarital pregnancy [51, 52], miscarriage [53], and prenatal high anxiety [47] due to pregnancy and newborn related factors, alcohol use in the husband [54], intimate partner violence [22, 55, 56], poor education of the husband [45], husbands' unemployment [46, 57], and psychiatric problems in the husband [58] were among the associated factors for the development of postpartum depression. In the context of Ethiopia too, poor marital relation [27, 29, 32, 34, 35, 59], unplanned pregnancy [21, 22, 24, 27, 29, 32, 34], previous history of depression [21, 27, 28, 34], domestic violence [21, 22, 27, 34], poor social support [21, 32-35], and family history of mental illness [24, 28, 31] were among the documented factors responsible for the development of Postpartum Depression (PPD).
Postpartum depression in women has a great impact on the health of both the mother and her baby. Early discontinuation of breastfeeding [60], negative emotion and poor health care utilization [61], cognitive impairment, and behavioral defects [62], poor mother-infant bonding resulting in rejection of the infant [63], and suicidal behaviors [64] are common complications leading to postpartum depression. Furthermore, a community-based cross-sectional study in Ethiopia [23] revealed that maternal postnatal depression strongly affects a child's nutritional status leading to stunting and underweight as well as inappropriate complementary feeding practices of infants.
Even though maternal mental health problems in the postpartum period are much more prominent in poorly developed nations including Ethiopia, there still exists a gap in the pooled magnitude of postpartum depression and the associated factors. The objective of the present meta-analysis was, therefore [1] to determine the pooled estimated prevalence of postpartum depression among women in the postnatal period in Ethiopia and [2]: to determine the pooled odds ratio of the associated factors for postpartum depression in Ethiopia.
2. MATERIALS AND METHODS
2.1. Search Strategy
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [65], we performed both an electronic and manual search of eligible articles. Our search of electronic libraries in Scopus, PubMed, and EMBASE and manual exploration of the reference list of articles was the backbone of the current meta-analysis. For searching articles on postpartum depression among women in the postnatal period using the PubMed database, we used the following search terms: (Prevalence OR Epidemiology OR magnitude AND depression OR PPD OR “depressive disorder” AND mothers OR females OR women AND postpartum period AND factor OR “risk factor” OR determinant AND Ethiopia). Besides, the search for literature in EMBASE and Scopus was done according to database-specific searching guidelines. Furthermore, the reference list of included studies was made and there was no specification for studies based on the study period.
2.2. Eligibility Criteria
Data refining was done according to the inclusion and exclusion criteria. Articles were eligible for inclusion if [1] they assessed the outcome of interest among women in the postpartum period, [2] their primary outcome of interest was the prevalence of postpartum depression and its associated factors, [3] the design of the study was community and institution-based cross-sectional, case-control and cohort study design, [3] and [4] the study has been piloted in Ethiopia. Previously studied reviews, studies on women with an already known psychiatric problem, studies on animals, editorials, and studies reporting depression solely during pregnancy were excluded. MN and YG screened the topics and abstracts of searched articles stored in an endnote reference manager depending on the primary and pre-specified eligibility criteria independently. After that, the next stage was a detailed exploration of the screened articles in the first step by the two review authors stated above. Any disagreement between the two authors regarding the eligibility of articles was settled through discussion in line with available logical evidence.
2.3. Methods for Data Extraction and Quality Assessment
The two authors (MN and MA) extracted the relevant data from the articles included in the final analysis autonomously using a standardized data extracted template. The included studies were extracted and summarized in the form of a table. Information that was extracted and has been summarized in the table includes the author's name, publication year, study setting, study population, sample size, study design, and the assessment instrument for postpartum depression. Data from incorporated studies was extracted based on a template structured as suggested by PRISMA guidelines [65].
The modified Newcastle-Ottawa Scale (NOS) [66] was employed for the evaluation of the quality of studies. The domains of the NOS scale for assessing the quality of studies include comparability between participants, representativeness of sample and sample size, statistical quality as well as ascertainment of cases.
2.4. Data Synthesis and Analysis
In this study, we employed a random-effect model to evaluate the aggregate prevalence of postpartum depression and the associated factors for postpartum depression with their 95% CIs [67]. Meta-XL version 5.3 [68] was employed to extract relevant data from included studies and the STATA11 Meta-prop package [69] was implemented to estimate the pooled prevalence of postpartum depression and pooled odds ratio of the associated factors for Postpartum depression. Cochran Q-statistics and Higgs I2 statistics [70] were also used to diagnose heterogeneity. The I2 statistical values of zero, 25, 50, and 75% connote absence, little, moderate, and great heterogeneity, respectively [70]. Furthermore, subgroup analysis and sensitivity analysis tests were also done to explore the source of heterogeneity between the included studies. A funnel plot test [71] and eggers publication bias test were used to detect publication bias.
3. RESULTS
3.1. Identification of Studies
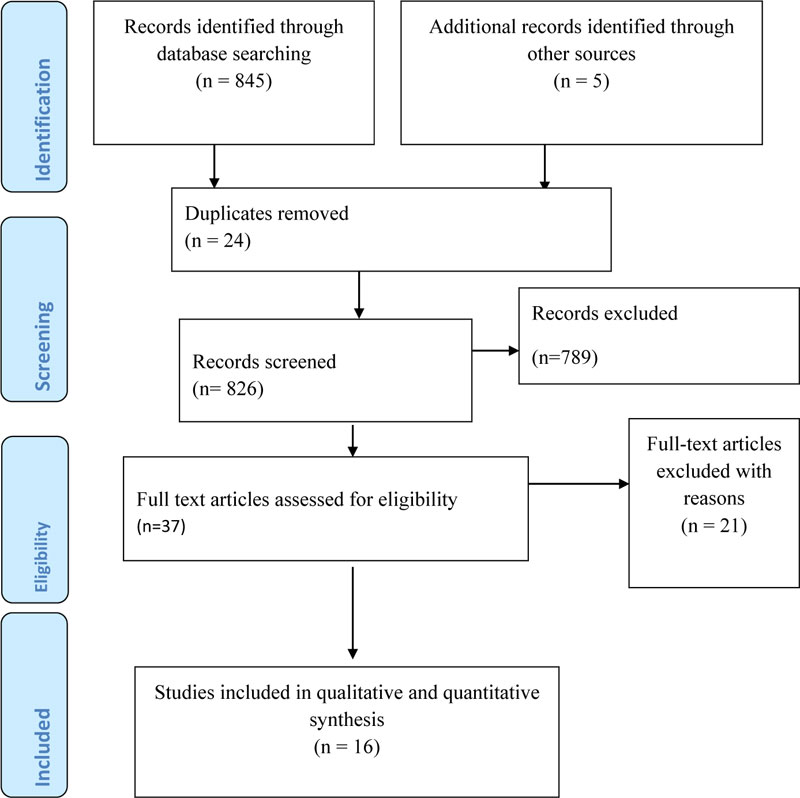
Our search with the pre-specified search strategies resulted in an overall of 845 articles. Besides, 5 articles were obtained from the reference list of included articles making the total number of retrieved articles to be 850. Of this, we removed 24 duplicated studies before further screening. In the next stage, we excluded 789 of the articles simply by observing their titles. Therefore the leftover 37 articles had been completely inspected for eligibility to be included in the current systematic review and meta-analysis study; nevertheless, only 16 articles were tailored in the final meta-analysis since the rest 21 articles were also excluded due to various methodological and technical flaws (Fig. 1).
3.2. Characteristics of Included Studies
In this meta-analysis, a total of sixteen studies that assessed the prevalence of postpartum depression [21-36] and fourteen studies that assessed the associated factors [21, 22, 24, 26-35, 59] had been analyzed. A total of 11400 postpartum women had participated in this analysis. Region-wise, six [26, 28, 29, 34, 36, 59], six [22-25, 32, 35], three [21, 31, 33], one [27] and one [30] of the studies were from the southern part of Ethiopia, Amhara region, Oromia region, Addis Ababa and Tigray, respectively. Of included studies, three [26, 34, 36], ten [21-24, 27, 29-32, 35], and another three [25, 28, 33] utilized PHQ-9, EPDS, and SRQ-20 to assess depression in the postnatal women. Besides regarding the design of the study, eight [21, 23, 25, 28, 32-34, 36], seven [22, 24, 27, 29-31, 35] and one [26] were community-based cross-sectional, institution-based cross-sectional and cohort studies in their respective order. Besides, six of the studies [23, 25, 27, 28, 30, 34] employed a multi-stage sampling method during data collection. All of the studies have reported a response rate for the study (Table 1) [21-36].
| Author, Year | Location of the Study | Study Design | Sample Size | Tool | Study Population | Depression (%)(n) | Sampling Method |
Time of PPD Assessment | Response Rate (%) |
|---|---|---|---|---|---|---|---|---|---|
| Fantahun et al.,2018 [1] | Addis Ababa, Ethiopia | CS | 618 | EPDS(≥13) | Postnatal women | 23.3 (n=144) | Multi-stage | Up to 6 weeks of delivery | 97.6 |
| Toru et al.2018 [2] | Southern Ethiopia | Community CS | 456 | PHQ-9 | Postnatal women | 22.4 (n=102) | Multi-stage | Up to 12 months of delivery | 99 |
| Abadiga,muktar 2019 [3] | Oromia, Ethiopia | Community CS | 287 | EPDS(≥10) | Postnatal women | 20.9 (n=60) | Simple random | Up to 12 months of delivery | 97.3 |
| Abebe et al.2019 [4] | Amhara region | CS | 511 | EPDS(≥13) | Postnatal women | 22.1(n=114) | Systematic sampling | Up to 6 months of delivery | 97.3 |
| MM Asaye et al 2020 [5] | Amhara region | CS | 526 | EPDS(≥13) | Postnatal women | 25 (n=129) | Cluster sampling | Up to 6 weeks of delivery | 100 |
| Kerie et al.2018 (6] | Southern Ethiopia | CS | 408 | EPDS(≥10) | Postnatal women | 33.8 (n=138) | Systematic sampling | Up to 12 months of delivery | 96.7 |
| Bitew et al.2019 [7] | Southern Ethiopia | Prospective cohort | 1240 | PHQ-9 | Postnatal women | 22.1(n=274) | NA | 4–12 weeks after childbirth | 94.6 |
| Azale et al.2018 [8] | Southern Ethiopia | Community CS | 3147 | PHQ-9≥5 | Postnatal women | 12.2(n=385) | Population census | 1 up to 12 months of delivery | 100 |
| Anato et al .2019 [9] | Amhara, Ethiopia | Community CS | 232 | EPDS(≥13) | Postnatal women | 22.8 (n=53) | Multistage | 5–10 months of delivery | 97.5 |
| Shewangizaw et al.2018 [10] | Harar, Ethiopia | CS | 122 | EPDS | Postnatal women | 13.11 (n=16) | Convenience | 1 week of delivery | 100 |
| Mariam et al.2016 [11] | Tigray , Ethiopia | CS | 616 | EPDS(≥8) | Postnatal women | 19 (n=117) | Multistage | 6 weeks of delivery | 97.3 |
| Author, year | Location of study | design | Sample size | Tool | Study population | Depression(%)(n) | Sampling Method |
PPD assessed at | Response rate (%) |
| Shitu et al.2019[12] | Amhara, Ethiopia | Community CS | 596 | EPDS(≥8) | Postnatal women | 23.7(n=141) | Cluster sampling | Up to 12 months of delivery | 97.4 |
| W Dargie et al.2020 [13] | Amhara, Ethiopia | CS | 308 | EPDS(≥13) | Postnatal women | 15.6(n=48) | Systematic | Within 6 weeks of delivery | 100 |
| Teferra benti et al.2015[14] | Oromia ,Ethiopia | Community CS | 340 | SRQ-20 ≥ 6 | Postnatal women | 31.5(n=107) | Simple random | During px & 1-year after birth | 95.2 |
| G gebremichael et al.2018 [15] | Southern Ethiopia | Community CS | 704 | SRQ-20 ≥ 6 | Postnatal women | 22.6(n=159) | Multi-stage | 1-year after birth | 96.7 |
| JN baumgartner et al.2014 [16] | Amhara, Ethiopia | Community CS | 1294 | SRQ-20 ≥ 7 | Postnatal women | 19.8(n=256) | Multi-stage | Within 2 years of delivery | 98 |
3.3. Quality of Included Studies
For assessing the quality of included studies, we used the modified Newcastle Ottawa quality assessment as a gold standard. The quality of the studies varied from 7 to 10, implying that none of the studies were of poor quality. One of the studies was of moderate quality [31] and the remaining fifteen were of good quality (Table 2).
| No | Study ID | Representation | Sampling | Random Selection | Non-response Bias | Data Collection | Case Definition | Reliability and Validity | Method of Data Collection | Prevalence Period | Numerator and Denominator | Summary |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Fantahun et al.,2018 [1] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| 2 | Toru et al.2018 [2] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| 3 | Abadiga,muktar 2019 [3] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| 4 | Abebe et al.2019 [4] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 5 | MM Asaye et al 2020 [5] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| 6 | Kerie et al.2018 [6] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| 7 | Bitew et al.2019 [7] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| 8 | Azale et al.2018 [8] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| 9 | Anato et al .2019 [9] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| 10 | Shewangizaw et al.2018 [10] | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 7 |
| 11 | Mariam et al.2016 [11] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| 12 | Shitu et al.2019 [12] | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 13 | W Dargie et al.2020 [13] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| 14 | Teferra benti et al.2015[14] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| 15 | G gebremichael et al.2018 [15] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| 16 | JN baumgartner et al.2014 [16] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
3.4. The Pooled Prevalence of Postpartum Depression in this Study
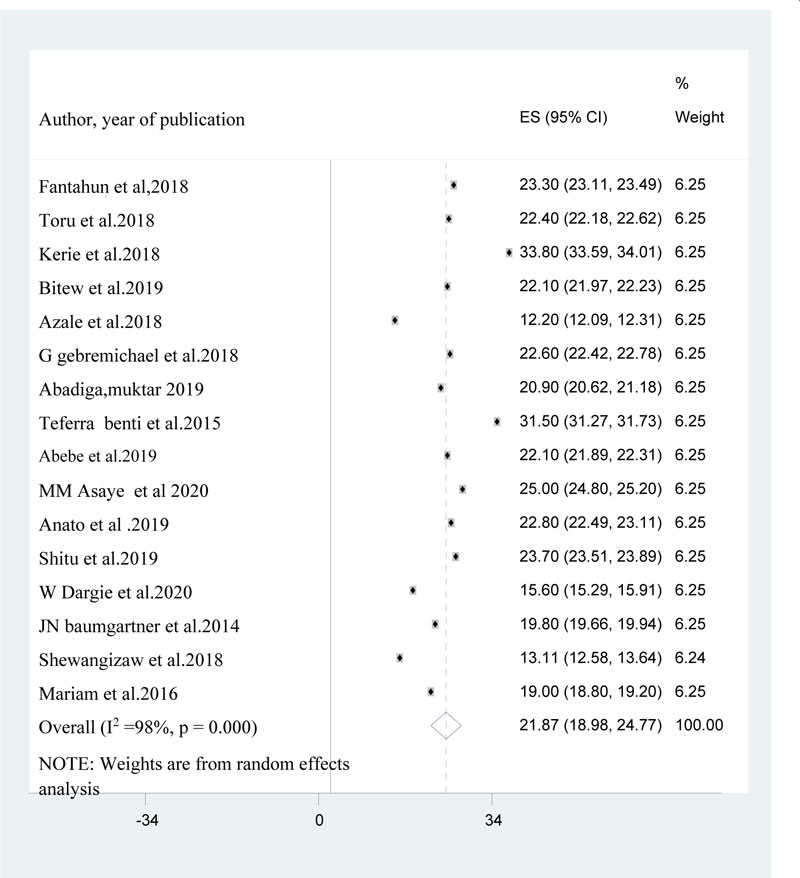
Sixteen studies [21-36] were incorporated to yield the pooled estimated effect size of postpartum depression. The reported magnitude of postpartum depression among the included studies ranged from 12.2%(36) to 33.8% (29). The average estimated prevalence of postpartum depression using the random effect model was 21.9% (95% CI: 18.98, 24.77). This average prevalence of postpartum depression was found to differ(I2 = 98%, p-value =0.000) from the included studies (Fig. 2).
3.5. Subgroup Analysis of the Prevalence of Postpartum Depression by the Tools used to Measure Postpartum Depression.
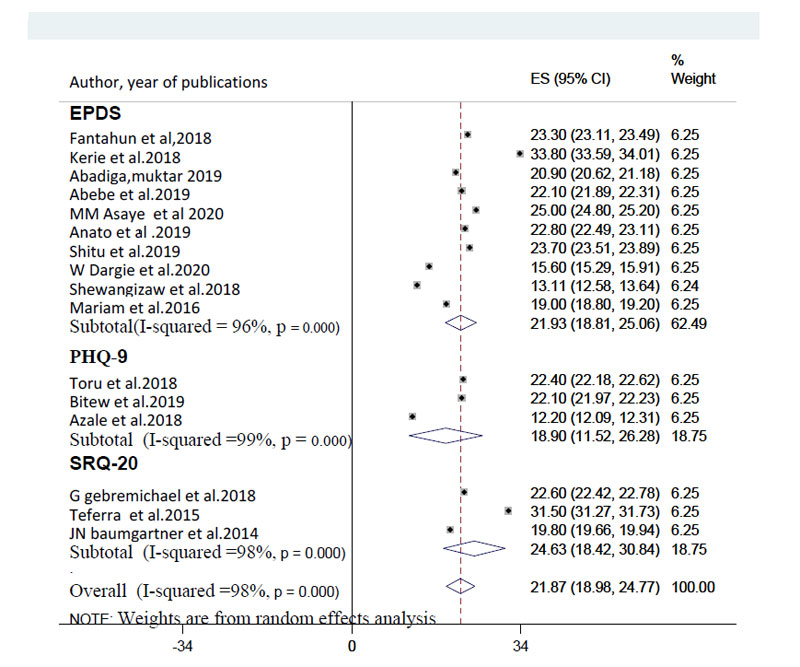
Since the average prevalence of postpartum depression was significantly influenced by the difference between the included studies, it was mandatory to conduct a subgroup analysis. Therefore, we used the measurement tools for postpartum depression to perform subgroup analysis. The subgroup analysis by assessment instrument yields that measurement with SRQ-20 provided significantly higher result, 24.6%% (95% CI: 18.42, 30.84) with (I2 =98%, p < 0.001) than the result with PHQ-9 which was 18.9% (95% CI: 11.52, 26.28) (I2 =99%, p < 0.001) (Fig. 3).
3.6. Sub-group Analysis of the Prevalence of Postpartum Depression taking into Account the Setting of the Study.
Although a subgroup analysis was done based on the setting where the study was done, there was no significant difference in the pooled prevalence of postpartum depression between community-based studies (22%) and institution-based studies (21.7%).
3.7. Sub-group Analysis of the Prevalence of Postpartum Depression with Regard to the Regional Location of the Study.
The pooled prevalence of post-partum depression was slightly higher in studies from the southern part of Ethiopia (22.6%) than the central region (Addis Ababa) (21.2%) and this difference was also significant statistically (p =0.001).
3.8. Sensitivity Analysis
We performed a leave one out sensitivity analysis to detect the source of heterogeneity. However, our result showed that the average prevalence of postpartum depression when each study was left out from the analysis ranged from 21.08% (18.47, 23.68) to 22.52% (20.34, 24.69). Therefore, the result was not outweighed by the influence of a single study (Table 3).
| No | Study Excluded | Prevalence of Postpartum Depression | 95% Confidence Interval |
|---|---|---|---|
| 1 | Fantahun et al.,2018 | 21.77 | 18.69, 24.86 |
| 2 | Toru et al.2018 | 21.83 | 18.77, 24.90 |
| 3 | Kerie et al. 2018 | 21.08 | 18.47, 23.68 |
| 4 | Bitew et al.2019 | 21.85 | 18.66, 25.05 |
| 5 | Azale et al.2018 | 22.52 | 20.34, 24.69 |
| 6 | G gebremichael et al.2018 | 21.82 | 18.72, 24.93 |
| 7 | Abadiga,muktar 2019 | 21.93 | 18.97,24.90 |
| 8 | Teferra benti et al.2015 | 21.23 | 18.41, 24.05 |
| 9 | Abebe et al.2019 | 21.85 | 18.78, 24.93 |
| 10 | MM Asaye et al 2020 | 21.66 | 18.62, 24.70 |
| 11 | Anato et al .2019 | 21.81 | 18.78,24.84 |
| 12 | Shitu et al.2019 | 21.75 | 18.67, 24.82 |
| 13 | W Dargie et al.2020 | 22.29 | 19.29,25.29 |
| 14 | JN baumgartner et al.2014 | 21.87 | 18.98, 24.77 |
| 15 | Shewangizaw et al.2018 | 22.45 | 19.47, 25.43 |
| 16 | Mariam et al.2016 | 21.87 | 18.98, 24.77 |
3.9. Publication Bias
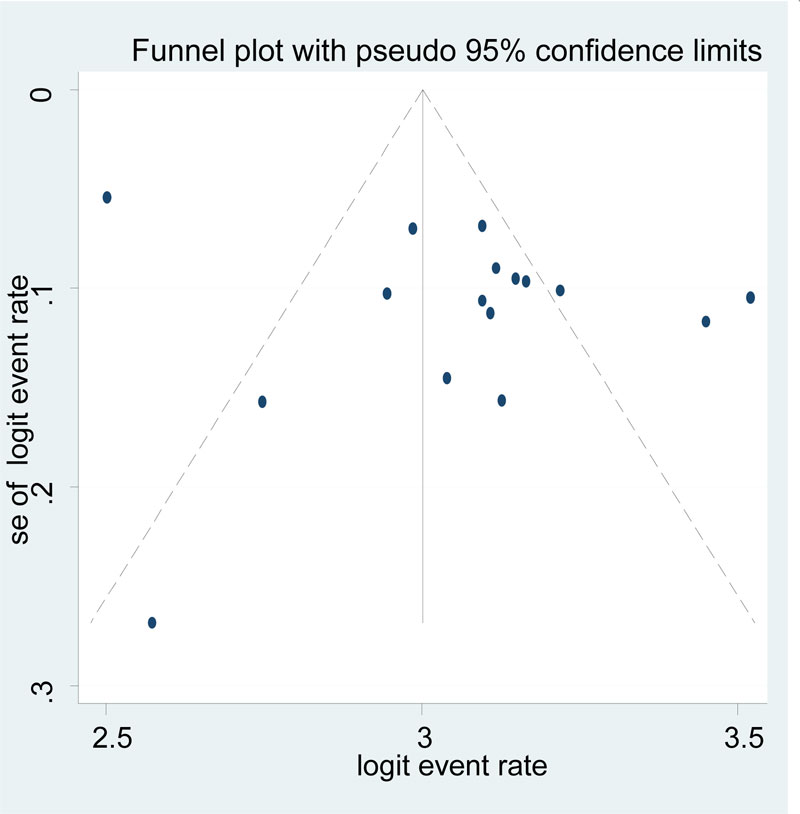
A scatter plot of the logit event rate of postpartum depression on the X-axis and its standard error on the Y-axis was done, which showed that there was a publication bias since the graph was slightly asymmetrical (Fig. 4). However, the eggers publication bias test revealed that there was no significant publication bias (B=71.2, SE = 44 and P-value = 0.13).
3.10. Associated Factors for Postpartum Depression in Ethiopian Women
As stated previously, fourteen studies [21, 22, 24, 26-35, 59] had reported one or more factors related to the development of depression in postnatal women. Our narrative synthesis revealed that poor marital relation [27, 29, 32, 34, 35, 59], unplanned pregnancy [21, 22, 24, 27, 29, 32, 34], previous history of depression [21, 27, 28, 34], domestic violence [21, 22, 27, 34], poor social support [21, 32-35], family history of mental illness [34, 28, 31], use of substance [21, 27, 34] and low income [27, 28, 59] were among the most commonly reported factors contributing to development of postpartum depression in postnatal women (Table 4).
The pooled odds ratio of the poor marital relationship among the above-mentioned studies was 3.56 (95% CI: 2.50, 4.63) (Fig. 5). This implied that women with poor marital relationships were 3.56 times at higher risk of developing PPD than women with good marital relationships. Also, the pooled odds ratio for unplanned pregnancy for the nine studies reported above was found to be 3.48 (95% CI: 2.18, 4.79) (Fig. 6). This showed that women who gave birth from an unplanned pregnancy were 3.5 times more likely to be depressed than women with a planned pregnancy. The previous history of depression was also an associated factor for the development of PPD with a pooled estimate odds ratio of 4.33 (95% CI: 2.26, 6.59); [21, 27, 28, 34]. Besides, domestic violence and poor social support were also found to have a significant association with the development of PPD with the estimated pooled odds ratio of 3.77 (95% CI:2.62, 4.92) [21, 22, 27, 34], 4.5 (95% CI: 3.34, 5.56) [21, 32-35], respectively.
Furthermore, the pooled odds ratio of family history of mental illness [24, 28, 31], use of substance [21, 27, 34] and low income [27, 28, 59], stressful life event[22, 59] and perinatal complications [28, 59] was 4 (95% CI:1.56, 6.56), 4.67(95% CI:4.00, 5.34), 2.87 (95% CI: 1.59, 4.14), 3.5 (95% CI: 1.39, 5.87) and 3.8 (95% CI: 1.45, 6.15), respectively (Table 5).
| Associated Factors | Odds Ratio (AOR) | 95% CI | Strength of Association | Author, Year of Publication |
|---|---|---|---|---|
| Being unmarried | 2.5 | 1.20, 4.90 | Strong and positive | Fantahun et al,2016 |
| Income difficulty | 2.3 | 1.30, 4.00 | Strong and positive | Fantahun et al,2016 |
| Death of a child | 3.2 | 1.30, 8.00 | Strong and positive | Fantahun et al,2016 |
| Unplanned pregnancy | 2.9 | 1.60, 5.00 | Strong and positive | Fantahun et al,2016 |
| Substance use | 4.9 | 1.10, 21.30 | Strong and positive | Fantahun et al,2016 |
| Previous depression | 4.2 | 2.30, 7.80 | Strong and positive | Fantahun et al,2016 |
| Domestic violence | 3.1 | 1.60, 5.90 | Strong and positive | Fantahun et al,2016 |
| 18 up to 23 years age | 3.9 | 1.53, 9.90 | Strong and negative | Toru et al.2018 |
| Unplanned pregnancy | 3.4 | 1.71, 6.58 | Strong and negative | Toru et al.2018 |
| Sleeping problem of child | 3.7 | 1.79, 7.72 | Strong and negative | Toru et al.2018 |
| Domestic violence | 2.9 | 1.72, 8.79 | Strong and negative | Toru et al.2018 |
| Unsatisfied marital relation | 2.7 | 1.32, 5.62 | Strong and negative | Toru et al.2018 |
| Poor social support | 4.3 | 1.79, 10.60 | Strong and negative | Toru et al.2018 |
| History of depression | 7.4 | 3.12, 17.35 | Strong and negative | Toru et al.2018 |
| Substance use | 5.2 | 2.52, 10.60 | Strong and negative | Toru et al.2018 |
| Unplanned pregnancy | 7.8 | 3.19, 19.26 | Strong and negative | abadiga, 2019 |
| Primi-parity | 4.99 | 1.54,16.09 | Strong and negative | abadiga, 2019 |
| History of depression | 3 | 1.06, 8.82 | Strong and negative | abadiga, 2019 |
| Domestic violence | 5.9 | 2.44, 14.40 | Strong and negative | abadiga, 2019 |
| Substance use | 3.9 | 1.52,10.30 | Strong and negative | abadiga, 2019 |
| Poor social support | 6.6 | 2.25, 19.29 | Strong and negative | abadiga, 2019 |
| Stressful life event | 4.5 | 2.64, 7.54 | Strong and negative | Abebe et al.2019 |
| Domestic decision making | 4.3 | 2.54, 7.14 | Strong and negative | Abebe et al.2019 |
| Unplanned pregnancy | 1.9 | 1.02, 3.41 | Strong and negative | Abebe et al.2019 |
| Partner violence | 3.2 | 1.76, 5.67 | Strong and negative | Abebe et al.2019 |
| Associated factors | Odds ratio(AOR) | 95% confidence interval | Strength of association | Author, year of publication |
| Hospitalization of the baby | 2.2 | 1.17, 4.31 | Strong and positive | Abebe et al.2019 |
| Abortion history | 1.8 | 1,07,2.96 | Strong and positive | MM Asaye et al 2020 |
| Low birth weight of baby | 3.1 | 1.78, 5.48 | Strong and positive | MM Asaye et al 2020 |
| GA of baby< 36 weeks | 2.2 | 1.22, 3.88 | Strong and positive | MM Asaye et al 2020 |
| Unplanned pregnancy | 2 | 1.24, 3.31 | Strong and positive | MM Asaye et al 2020 |
| Relative mental illness | 1.2 | 1.09, 3.05 | weak and positive | MM Asaye et al 2020 |
| Has no ANC visit | 4.05 | 1.81, 9.05 | Strong and positive | MM Asaye et al 2020 |
| Has no PNV | 1.8 | 1.11, 3.00 | strong and positive | MM Asaye et al 2020 |
| Unplanned pregnancy | 4.5 | 2.31, 8.71 | Strong and positive | Kerie et al.2018 |
| Age 15-24 years | 0.4 | 0.18, 0.98 | Weak and negative | Kerie et al.2018 |
| Chronic illness | 7.7 | 2.34, 25.44 | Strong and positive | Kerie et al.2018 |
| Death of the infant | 4.1 | 1.78, 9.51 | Strong and positive | Kerie et al.2018 |
| Unstable marriage | 6 | 2.79, 12.99 | Strong and positive | Kerie et al.2018 |
| Intimate partner violence | aRR=1.06 | 1.00, 1.12 | Strong and positive | Bitew et al.2019 |
| Depression in pregnancy | aRR=1.3 | 1.15, 1.45 | Strong and positive | Bitew et al.2019 |
| Premature baby | 11.4 | NA | Strong and positive | Shewangizaw et al.2018 |
| Poor satisfaction with care | 8.7 | NA | Strong and positive | Shewangizaw et al.2018 |
| Family hx of mental illness | 7.4 | NA | Strong and positive | Shewangizaw et al.2018 |
| Single/divorced/widowed | 3.5 | 1.35, 8.82 | Strong and positive | Shitu et al.2019 |
| Unwanted pregnancy | 1.9 | 1.14, 3.33 | Strong and positive | Shitu et al.2019 |
| Undesired infant sex | 1.8 | 1.13, 2.86 | Strong and positive | Shitu et al.2019 |
| Infant illness | 2.1 | 1.30, 3.34 | Strong and positive | Shitu et al.2019 |
| Poor social support | 3.2 | 1.55, 6.43 | Strong and positive | Shitu et al.2019 |
| Rural residence | 2.6 | 2.56, 4.19 | Strong and positive | Azale et al.2018 |
| Grand multi-parity | 2.0 | 1.22, 3.26 | Strong and positive | Azale et al.2018 |
| Associated factors | Odds ratio(AOR) | 95% confidence interval | Strength of association | Author, year of publication |
| Perinatal complications | 2.6 | 1.89, 3.44 | Strong and positive | Azale et al.2018 |
| Past history of abortion | 1.5 | 1.07, 2.11 | Moderate and positive | Azale et al.2018 |
| Hunger in past 1 month | 2.4 | 1.75, 3.23 | Strong and positive | Azale et al.2018 |
| Lower perceived wealth | 2.1 | 1.19, 3.76 | Strong and positive | Azale et al.2018 |
| Poor marital relation[12] | 2.5 | 1.79, 3.42 | Strong and positive | Azale et al.2018 |
| stressful event in past | 2.4 | 1.82, 3.06 | Strong and positive | Azale et al.2018 |
| Being widowed | 4.2 | 1.14, 15.20 | Strong and positive | Wubetu et al.2020 |
| Poor social support | 5.1 | 1.00, 26.18 | Strong and positive | Wubetu et al.2020 |
| Hospitalization of a child | 3.3 | 1.39, 7.93 | Strong and positive | Wubetu et al.2020 |
| Death of family member | 2.9 | 1.101, 8.50 | Strong and positive | Wubetu et al.2020 |
| Have no death of one’s child | 0.3 | 0.11,0.86 | Strong and Negative | Teferra et al.2015 |
| Poor support from family | 3.3 | 1.11, 9.52 | Strong and positive | Teferra et al.2015 |
| Low income | 4.2 | 1.90,9.30 | Strong and positive | G Gebremichael et al.2018 |
| Pregnancy complications | 5 | 2.50, 10.40 | Strong and positive | G Gebremichael et al.2018 |
| Smoking in husband | 4.1 | 1.60, 10.60 | Strong and positive | G Gebremichael et al.2018 |
| Previous depression | 2.7 | 1.54, 4.80 | Strong and positive | G Gebremichael et al.2018 |
| Family hx of psychiatry illness | 3.6 | 1.40, 9.10 | Strong and positive | G Gebremichael et al.2018 |

| Associated Factors | Risk Groups | Pooled Effect Size & 95% CI | I2 | Studies Pooled |
|---|---|---|---|---|
| Unplanned pregnancy | Women who have unplanned pregnancy | 3.48 (2.18, 4.79) | 90% | [1-6, 12] |
| Previous history of depression | Women having history of depression | 4.33 (2.26, 6.59) | 94% | [1-3, 15] |
| Poor social support | Women with poor social support | 4.5 (3.34, 5.56) | 96% | [2, 3, 12-14] |
| Domestic violence | Women who faced domestic violence | 3.77 (2.62, 4.92) | 94.6% | [1-4] |
| Poor marital relation | Single/divorced/widowed& dissatisfied marriage | 3.74 (2.47, 5.00) | 92% | [1, 2, 6, 12, 13, 17] |
| Substance use | Those women who are using substances | 4.67(4.00, 5.34) | 90.6% | [1-3] |
| Low income | Women with insufficient income | 2.87(1.59, 4.14) | 84% | [1, 15, 17] |
| Family history of mental illness | Women with history of mental illness in the family | 4 (1.56, 6.56) | 92.6% | [5, 10, 15] |
| Stressful life-event | Women who faced stressful event | 3.5 (1.39, 5.87) | 97% | [4, 17] |
| Perinatal complications | Women with perinatal complications | 3.8 ( 1.45, 6.15) | 98% | [15, 17] |
4. DISCUSSION
To date, this review and meta-analysis on depression and the related factors in women in the postnatal period are the first of its kind in the context of Ethiopia. Therefore, the pooled effect size of postpartum depression and related factors would be an added advantage for the scientific community and other diverse stakeholders who intend to intervene in this significant public health issue. We gathered data from a total of 11400 postpartum women and a total of sixteen studies from both institutional and community settings and the estimated pooled prevalence of postpartum depression was found to be 21.9% (95% CI: 18.98, 24.77).
The result of the pooled estimated prevalence of postpartum depression in this study (21.9%) was in line with a systematic review and meta-analysis on depression in the postpartum period in India (22%) which analyzed 38 studies and 20043 women [10]. It was also consistent with the result of a systematic review and meta-analysis study on women from low and middle-income countries which assessed 34 studies and 19.8% of them were found to have a postpartum common mental disorder [9]. Furthermore, another study that incorporated 38412 women and 23 studies from low and middle-income countries [6] reported 19.2% of women as having postpartum depression, which was also supportive of the current finding.
However, the result of the pooled estimated prevalence of postpartum depression in Ethiopia exceeds the worldwide estimated prevalence of postpartum depression, such as 17% reported in 2018 by S Shorey et al. [8]. The possible reason for the higher estimated prevalence in the earlier study as compared to our study could be due to the inclusion of a larger number of studies and participants in the analysis (26 cross-sectional, 30 prospective cohort and 2 case-control studies with an overall 58 studies and 37294 participants); however, only 16 studies were included in our study. Moreover, women in the previous study were healthy subjects having no history of depression previously but our study found that a previous history of depression was among the factors responsible for the increased prevalence of postpartum depression. Moreover, the rate of prevalence in our study was higher than the result of a systematic review and meta-analysis in 11 high-income countries reported in 2005, in which the pooled estimated prevalence of postpartum depression was 12.9% [72].
Possible grounds for the difference could be due to a long time gap between the previous study and the present study. The difference in the time point for the assessment of postpartum depression could also be a reason. The previous study included studies that screened PPD only in the three months of the postpartum period but in the present study, assessment period was far beyond this. Moreover, a socio-economic and cultural difference between high-income study subjects of the earlier study and low-income study subjects of the present study could be a root cause for the variation.
Contrary to the subgroup analysis result of a worldwide meta-analysis study [8] that observed the pooled estimated prevalence of postpartum depression to be similar across the different measurement tools for PPD, the present study revealed that pooled prevalence of postpartum depression was higher in studies as measured with SRQ-20 (24.6%%) (95% CI: 18.42, 30.84) than the result with PHQ-9 (18.9%) (95% CI: 11.52, 26.28). This could be because most studies that utilized SRQ-20 delineated a lower cut-off point (SRQ-20 score ≥ 6), which might result in an overestimation of postpartum depression.
In line with the result of an earlier meta-analysis study [8], the pooled estimated size of postpartum depression showed a geographical difference. The pooled estimated post-partum depression was slightly higher in studies from the southern part of Ethiopia (22.6%) than the central region (Addis Ababa) (21.2%), which could be due to the relatively improved socio-economic and cultural advances in the central region of Ethiopia. This was, however, in contrast to the result of a meta-analysis conducted in India [10].
However, no significant variation in the magnitude of PPD was noticed between the community and institutional settings of the studies. This was consistent with a review and meta-analysis study in India [10] in which little but insignificant variation was observed across the community and institutional setting studies. Even though heterogeneity was a problem in the present study, the 95% confidence interval of the average prevalence of postpartum depression was narrow. This might be due to the small standard error in the included studies, a large number of included studies with a large number of participants.
Regarding the associated factors of postpartum depression, fourteen studies [21, 22, 24, 26-35, 59] had reported different factors and poor marital relation [27, 29, 32, 34, 35, 59], unplanned pregnancy [21, 22, 24, 27, 29, 32, 34], previous history of depression [21, 27, 28, 34], domestic violence [21, 22, 27, 34], poor social support [21, 32-35], family history of mental illness [24, 28, 31], use of substance [21, 27, 34] and low income [27, 28, 59] were among the most commonly reported factors.
The pooled odds ratio of the poor marital relationship among the above-mentioned studies was 3.56 that implies women with poor marital relationships were 3.56 times at higher risk of developing PPD than women with good marital relationships. A meta-analysis study in India showed a similar conclusion supporting this [10]. The possible reason for this could be poor marital relationship increasing the burden of psychosocial responsibility of child care and other household responsibility in the postpartum period as compared to the shared psychosocial responsibility of women with good marital relation.
Besides, the pooled odds ratio for unplanned pregnancy for the nine studies reported above was found to be 3.48. This showed that women who gave birth from an unplanned pregnancy were 3.5 times more likely to be depressed than women with a planned pregnancy. A consistent finding was reported in studies conducted in Turkey [17], Qatar [14], northwestern Brazil [73], and Iran [74]. This might be due to the common factor involved in the development of PPD in Ethiopia too.
Another additional possible reason for this could be the absence of psychological readiness in mothers with unplanned pregnancy predisposing them to be vulnerable to physiological, psychosocial challenges of pregnancy and the postpartum period.
The previous history of depression [21, 27, 28, 34] and stressful life events [22, 59] was also an associated factor for the development of PPD with a pooled estimate odds ratio of 4.33 and 3.5, respectively. A consistent finding was observed in an Indian meta-analysis study[10]. Furthermore, other several studies [6, 75, 76] reported the presence of depression during pregnancy, facing stressful life events during pregnancy, and prior history of depression as related to postpartum depression, which was also in line with the current study.
Besides domestic violence was also found to have a significant association with the development of PPD with the estimated pooled odds ratio of 3.77 [21, 22, 27, 34]. A report by the World Health Organization in 2013 [77] suggested a similar conclusion in terms of intimate partner violence in women predisposed to various mental health problems in the postpartum period.
Poor social support with a pooled odds ratio of 4.5 [21, 32-35] also increases the vulnerability to postpartum depression. This also supports the findings of the Indian review study [10]. Multiple earlier studies have also reported that good interpersonal relationships across the social support networks increase flexibility to stress and subsidize enormously women from developing postpartum depression [78-81], hence decreasing the risk of postpartum depression. A study in Ghana on interventions for women with postpartum depression revealed that psychosocial support interventions are the most effective treatments implying an underling psychosocial deficit in this target population[82].
Furthermore, the pooled odds ratio of family history of mental illness [24, 28, 31], use of a substance [21, 27, 34] and low income [27, 28, 59] and perinatal complications [28, 59] was 4, 4.67, 2.87, 3.5 and 3.8, respectively. A systematic review and meta-analysis study in which 17 articles were reviewed and postpartum depression between 3 and 52 weeks postpartum periods was assessed [83] reported substance use as a contributing factor for postpartum depression, being in line with the current study.
5. STRENGTHS AND LIMITATIONS
Regarding strength, this study utilized a pre-specified search strategy through the mentioned libraries that are intended to reduce the assessor's bias. The subsequent strength was that the independent extraction of data and quality assessment of the included studies by two autonomous reviewers also lessened the reviewer's bias. Furthermore, the employment of subgroup analysis and sensitivity analysis to distinguish the foundation of heterogeneity was also a strength. On the contrary, the limits of this meta-analysis study emanate from the presence of a high difference between the included studies that might disrupt the deduction of the study results. Besides, the use of two or three studies in the sub-group analysis might diminish the accuracy of the estimates.
CONCLUSION
This review and meta-analysis study obtained a high pooled estimated prevalence of postpartum depression (21.9%), suggesting that more than one in five women experience postpartum depression. The pooled estimate of postpartum depression was higher in studies that used SRQ-20 (24.6%) than studies that used PHQ-9 (18.9%. Moreover, the pooled prevalence of postpartum depression was slightly higher in the southern part of Ethiopia (22.6%) than Addis Ababa (21.2%). However, no significant difference in pooled prevalence was noticed across study settings (community versus institutional). Poor marital relations, unplanned pregnancy, previous history of depression, poor social support, domestic violence, family history of mental illness, use of the substance, low income, stressful life event, and perinatal complications were among the associated factors for postpartum depression. Therefore, postnatal antenatal care services should consider this significant mental health problem of women and its associated factors basically by delivering integrated postnatal care services for women.
LIST OF ABBREVIATIONS
| AOR | = Adjusted Odds Ratio |
| CI | = Confidence Interval |
| CS | = Cross-Sectional |
| EPDS | = Edinburgh Postnatal Depression Scale |
| OR | = Odds Ratio |
| PHQ-9 | = Patient Health Questionnaire-9 |
| PPD | = Postpartum depression |
| PRISMA-P | = Preferred Reporting Items for Systematic Reviews and Meta-analysis |
| SRQ-20 | = Self Reporting Questionnaire-20 |
CONSENT FOR PUBLICATION
Not applicable
FUNDING
None.
CONFLICT OF INTEREST
We authors have no competing interests regarding this meta-analysis study.
ACKNOWLEDGEMENTS
We acknowledge the authors of the included studies for their original contribution.


