All published articles of this journal are available on ScienceDirect.
Association between Emergency Department Overcrowding and Mortality at a Teaching Hospital in Saudi Arabia
Abstract
Introduction:
Emergency Departments (ED) are highly important in hospital settings because they offer 24-hour professional assistance to patients in need of healthcare. However, ED overcrowding has started to become a global healthcare crisis, such that the patient capacity of EDs is no longer sufficient to meet patient demand.
Aim:
Thus, this study aimed to determine the relationship between ED overcrowding and the mortality rate of patients to draw the attention of decision makers in Saudi Arabia toward this issue, with the hope of ultimately attaining a solution to this problem.
Methods:
Using patients’ electronic health records that were stored in the Quadra Med system in 2018, we calculated the occupancy rates of the ED of a target teaching hospital at different quarters and associated those figures with the mortality rates for the same quarters.
Results:
Our results showed that there was no significant association between mortality rate and crowding status in the ED. Nonetheless, we recommend increasing public awareness and bed capacity at EDs in Saudi Arabia because overcrowded EDs can lead to adverse patient outcomes.
Conclusion:
The present study showed that the highest percentage (38%) of deaths that occurred during the overcrowded period were mostly of patients between 30 and 44 years of age, while patients between 60 and 74 years of age accounted for 36% of deaths.
The current study also assessed patient triaging, revealing that the highest number of patients was associated with level four (62.7% of the total patients in the overcrowded ED) and level five (33.1% in the overcrowded ED) triaging.
We also discovered higher levels of admission in the critical care unit during the ED overcrowding period compared with other periods.
1. INTRODUCTION
A hospital’s emergency department (ED) plays a key role in saving patients’ lives. EDs that offer 24-hour professional assistance to everyone in need of healthcare serve as vital links between pre-care and in-care medical facilities. However, an increase in the number of visits has been observed in EDs all over the world recently, as shown by the changing demographics worldwide [1].
ED overcrowding occurs when the demand exceeds the supply, i.e., when the number of patients exceeds the bed capacity or when ED patients cannot be moved to inpatient areas [2-4]. This phenomenon results in many organizational problems, such as laboratory and admission delays and staff shortages, leading to a decline in the quality of care. Consequently, these issues can lead to more negative effects, such as delays in care, prolonged patient waiting times especially among non-critical patients, patient dissatisfaction, medical errors, increased mortality rates, and patients leaving without being checked [2, 5-7]. In addition, studies [8,9] on the impact of ED crowding on clinician work process and patient safety perspective found that ED crowding leads to multitasking and interruption of care. They also found that ED crowding is an important factor affecting clinicians’ decision making, resulting in forgetting important details that may be important to patient safety, as well as an increased mortality rate. Moreover, an article published by Moskopet al. [10] reconsidered the problem of crowding in EDs in the US. The researchers gave a review of the origin of the problem, the definitions and measures of crowding, as well as possible causal factors. They also explored studies that examined the adverse moral consequences of ED crowding and its effect on patient outcome and provider morale. The obtained results were unpleasant, indicating that as medical errors increased, patients’ privacy, confidentiality, and communication were compromised.
Previous studies have researched the multiple causes of ED overcrowding. For example, the Center for Disease Control and Prevention claimed that ED overcrowding is mainly caused by patients who do not have medical insurance but have a complicated medical history, as well as the older population (over 65 years of age) who suffer from chronic medical conditions [11-13]. Another reason is inpatient “access block”, which refers to patient delays of more than 8 hours in accessing inpatient beds after getting admitted [14, 15]. These access blocks result in extended lengths of stay in inpatient departments and increased patient mortality [16]. In the Kingdom of Saudi Arabia, Alhussain et al. [17] found that overcrowding was mainly caused by non-urgent visits to EDs due to insufficient community awareness of the ED’s role and lack of access to primary healthcare services.
Many attempts have been made to solve ED overcrowding. For example, one large hospital in the Champagne-Ardenne region in France introduced a fast-track policy that aimed at reducing the duration of stays that last for more than 4 hours; however, they were not able to attain a decrease in access blocks [15]. Another study conducted in the US focused on the role of ED boarding in managing ED crowding [18].The study explored solutions to minimize the boarding time. The researchers found that the implementation of electronic handoffs instead of traditional handoffs resulted in a decrease in the boarding time and, thus, a decrease in ED crowding.
Another study [ 19 ] examined a new process (using Alternative Care Area or AltCA beds) for managing crowding at EDs due to the boarding of admitted patients. The researchers explored whether AltCA beds were associated with an increased risk of patient safety and quality outcome. They concluded that patients in AltCA beds did not have an elevated risk of patient safety and quality outcomes. However, AltCA beds decreased the risk of transfer to intensive care units and mitigated hospital-acquired infections compared with standard inpatient beds.
Overcrowding is not an isolated phenomenon, as it has been observed across developed and developing countries. Despite ample research in the field, only a few solutions have been proposed, and none of them have been successful in solving the problem.
1.1. Relationship Between ED Crowding and Mortality Rate
Previous studies have attempted to determine the effects of ED crowding on patient outcomes in terms of mortality. For example, a study in Iran confirmed that overcrowded EDs cause multiple adverse effects, one of them being the increased mortality rate among patients [20].
However, other studies have shown the absence of correlation between ED crowding and an increase in death rates [21, 22]. Furthermore, a retrospective study has shown that during periods of high ED crowding, there are statistically significant increases in patient admissions (e.g., critical and elderly patients), waiting times, length of visits, patient hospitalizations, and associations between ED crowding and seven-day mortality rates [1].
The literature concerning ED crowding indicates that crowding is a risk factor for the poor quality of care and negative events after ED assessment [ 23,24].
Overall, research shows that ED overcrowding results in worsening outcomes for patients.However, most of these studies have been conducted in Western countries. There has been very little research from the Middle Eastern nations, particularly from the Kingdom of Saudi Arabia, on the association between ED overcrowding and patient outcomes. Thus, the relationships between these variables must be evaluated. We expect that if the existence of a relationship between ED crowding and the subsequent high mortality rate is confirmed, decision makers will be motivated to address ED crowding and consider it a top public health priority in Saudi Arabia. Therefore, the main objective of this study was to explore the potential relationships between ED overcrowding and an increase in patients’ mortality rates at a teaching hospital in the Eastern Province of Saudi Arabia. We hypothesized that high ED crowding has negative consequences on patient outcomes in terms of mortality rate. We hope that this study will address the gap in the literature on whether there exists an association between ED overcrowding and mortality rate, produce quality evidence on the topic, and add to the current knowledge on the relationship between ED overcrowding and patient outcomes in Saudi Arabia.
2. MATERIALS AND METHODS
2.1. Data Source and Population
The target teaching hospital has a 440-bed capacity distributed across four floors. The ED has 44 beds for resuscitation, cardiac and trauma, medical, surgical, OB/GYN, and pediatric care. The computerized system Quadra Med (Plano, Texas, USA) is used only in clinical services, while administrative services use a different application developed by the IT department. The target population constitutes all of the patients who visited the ED of the target hospital in 2018.
2.2. Sample Size and Sampling Technique
The data used in this study were retrieved from the patients’ electronic health records in the Quadra Med system in 2018. As shown in Table 1, the entire year was divided into four quarters based on the quarterly statistics sent to the Ministry of Health as per their requirement. The first quarter was from January 1 to March 31, the second from April 1 to June 30, the third from July 1 to September 30, and the fourth from October 1 to December 31. The total number of ED patient visits during the year was distributed among these four quarters.
| 4th Quarter October 1 – December 31 | 3rd Quarter July 1 – September 30 |
2nd Quarter April 1 - June 30 |
1st Quarter January 1 – March 31 |
Characteristics |
|---|---|---|---|---|
| 67441 | 54191 | 54109 | 59202 | ED Visits |
| 44 | 44 | 44 | 44 | ED beds |
| 4048 (44 beds*92 days) |
4048 (44 beds*92 days) |
4004 (44 beds*91 days) |
3960 (44 beds*90 days) |
Available bed-days during the specific period of the calendar year |
| 2361 | 2155 | 2106 | 2169 | Number of patients admitted from the ER |
| 26.8% | 24.5% | 23.9% | 24.6% | Percentage of patients admitted from the ER |
| 3.00 | 2.68 | 2.46 | 2.59 | Occupancy rate |
Table 1 presents the operational characteristics of all four quarters in 2018. The occupancy rates and the number of patient visits were used to measure ED crowding. According to the literature, an ED is considered overcrowded when its occupancy rate is over 100%. The mean occupancy rate of the ED must be ≤ 0.50 and ≤ 1.00 for it to be classified as less crowded and highly crowded, respectively. We used ED occupancy rates to define the crowded categories and standardize the comparisons of crowding states across different ED periods [4]. This measure has been widely accepted as the crowding index [25].
In this study, the occupancy rate was calculated based on the following occupancy rate formula suggested by the World Health Organization [26]: utilized bed-days x 100/available bed-days during the calendar year. Therefore, the occupancy rate for the first, second, third, and fourth quarters was 259%, 246%, 268%, and 300%, respectively. Since all of the occupancy rates in our study were greater than 1.00 (>100%), all four quarter periods were evaluated to be crowded.
However, based on the number of patient visits during the individual quarters of 2018, it seems that the lowest number of patient visits was seen in the second quarter, while the highest was noted in the fourth quarter. Accordingly, we considered the second and fourth quarters as crowded and overcrowded periods for the comparison analysis. The inclusion criterion for this study was patient attendance at the target hospital’s ED during crowded and overcrowded times between January 1 and December 31, 2018, whereas the exclusion criterion was attendance in quarters other than the second and fourth quarters.
2.3. Ethical Consideration
Ethical approval was obtained from Imam Abdurrahman Bin Faisal University’s research ethical review board.
2.4. Statistical Analysis
We used IBM SPSS software for Mac for the statistical analysis. Mean and standard deviation were used to report continuous variables. Frequencies and percentages were used to report categorical variables. The variables of age, gender, nationality, and triage level were retrieved from the patients’ electronic records. In addition, variables such as ED bed number, admission number, and occupancy rate were retrieved from Quadra Med, as well as from the IT and quality departments. A p-value of 0.05 was used as the cut-off value. This study also used univariate descriptive statistics and bivariate statistics to differentiate between overcrowded and crowded EDs, followed by multilinear regression to identify the predictors of mortality.
2.5. Confounding Factors
The literature [ 27 ] highlights that studies on the relationship between ED overcrowding and hospital mortality must consider confounding factors, such as the long-term trends, for example, where ED occupancy seems to increase over time possibly due to the access block ( i.e ., delay in obtaining inpatient beds). In the present study, according to the target hospital’s regulations, long-term patients were excluded from the bed occupancy count in the next shift (shifts last for 8 hours).
3. RESULTS
Table 2 reports the demographic characteristics of the participants. Statistically significant relationships (p< 0.001) were found between ED crowding status and all of the demographic variables, except for participant nationality.
| Crowded n (%) |
Overcrowded n (%) |
p-value | |
|---|---|---|---|
|
Gender Male Female |
28016 (52.6%) 25247 (47.4%) |
30812 (53.8%) 26478 (46.0%) |
<0.001 |
|
Age Less than 15Y 15Y – 29Y 30Y – 44Y 45Y – 59Y 60Y – 74Y More than 75Y |
9546 (18.6%) 19538 (38.1%) 12906 (25.2%) 5959 (11.6%) 2533 (4.9%) 810 (1.6%) |
12282 (22.4%) 20335 (37.1%) 13012 (23.7%) 5858 (10.7%) 2594 (4.7%) 793 (1.4%) |
<0.001 |
|
Adult Yes No |
40180 (75.4%) 13083 (24.6%) |
40560 (70.8%) 16729 (29.2%) |
<0.001 |
|
Nationality Saudi Non-Saudi |
45325 (85.1%) 7938 (14.9%) |
48557 (84.8%) 8733 (15.2% |
0.114 |
Table 3 presents the distribution of patients at the triage levels, admission to the critical care unit, and the mortality rates. The mortality rates were calculated using the following formula: number of deaths x 100/number of people during crowding [11]. Thus, the mortality rate in the crowded period was calculated as 25 (deaths) x 100/53309 (number of patient visits during the crowded period) = 0.047. Meanwhile, the mortality rate in the overcrowded period was calculated as 25 (deaths) x 100/57290 (number of patient visits during the overcrowded period) = 0.044. Table 3 demonstrates that there are significant associations between crowding status and triage levels (p< 0.001). A greater percentage of patients with non-urgent cases attended the ED during the overcrowded period than during the crowded period. A nearly similar percentage of death was observed during the crowded and overcrowded periods. However, no statistically significant associations were found between the crowding status and both mortality rate and admission to the critical care unit (p = 0.888 and 0.802, respectively).
| Crowded n (%) |
Overcrowded n (%) |
p-value | |
|---|---|---|---|
| Triage levels * I. Immediate II. Highly urgent (10 min.) III. Urgent (30 min.) IV. Standard (60 min.) V. Non- urgent (120 min.) |
21 (0.1%) 57 (0.2%) 2629 (7.2%) 23399 (64.2%) 10342 (28.4%) |
17 (0.0%) 26 (0.1%) 1518 (4.1%) 23006 (62.7%) 12134(33.1%) |
<0.000 |
| Admission to Critical Care Unit | 169 | 196 | 0.802 |
| Expired (Death) Yes No |
25 (0.047) 53238 (99.9) |
25 (0.044) 57262 (99.9) |
0.888 |
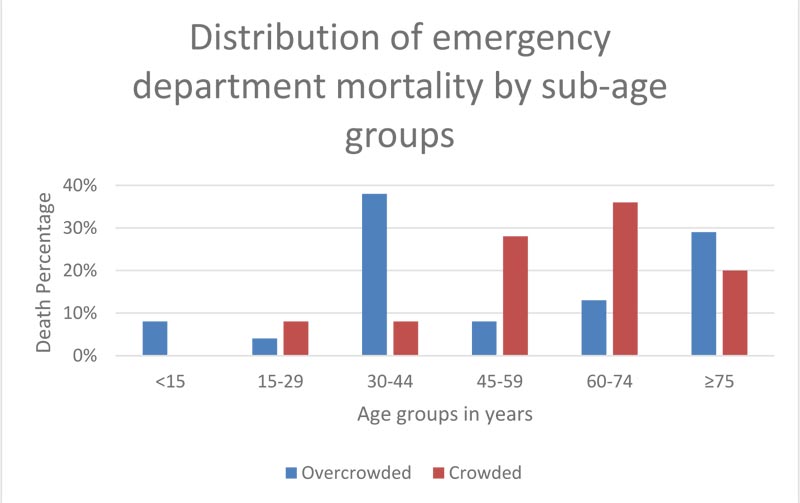
Fig. (1) shows the distribution of ED mortality by sub-age groups. There were statistically significant age differences in mortality for the two levels of crowding (p< 0.000). The mortality rate in the overcrowded period for patients between 30 and 44 years of age was higher than that for patients in other age groups. However, in the crowded period, those between 60 and 74 years of age accounted for 36% of the mortality, the highest among all age groups.
With regards to the gender variable, although the mortality rate in males was higher than that in females in both crowding options, there were no statistically significant gender differences in mortality for the crowded and overcrowded periods ( p = 0.123 and 0.154, respectively).
4. DISCUSSION
The aim of this study was to identify the possible association between ED crowding status and patient outcomes. ED high crowding and patient outcomes are related in multiple ways, as demonstrated by previous studies that have been conducted across the globe. Based on a large sample of 110,553 patients (48.2% in a crowded ED and 51.8% in an overcrowded ED in 2018), our findings revealed an occupancy rate of 2.46 for a crowded ED and 3 for an overcrowded ED. During the ED overcrowding period, there was an increase in the number of patient admissions (26.8% out of the total percentage during 2018), while the share of admissions during the ED crowding period was 23.9%.
In addition, we found that the highest percentage of patients at the ED comprised the age groups of 15–29 and 30–44, respectively, at both crowding periods. This result is in agreement with the findings presented earlier [ 17 ], which showed that the largest percentage of patients visiting ED comprised middle-aged individuals.
Furthermore, our study found that the percentage of Saudi patients present at the target government hospital was the highest in both crowding statuses. This result might be partly explained by the availability of medical insurance for the majority of non-Saudi people, which might have enabled them to utilize private hospitals.
Our study found no significant association between mortality rate and crowding status in ED. Our finding is in line with the findings reported earlier [21, 22], which demonstrated the absence of correlation between ED crowding and increase in death rates. However, our result contradicts the findings of two retrospective cohort studies conducted in Sweden and Italy that revealed a high mortality rate within 10 and seven days during overcrowding [4, 28]. This is more or less similar to the evidence obtained in other parts of the world, such as a retrospective study in Australia showing that when patients came in during high ED occupancy, in-hospital mortality rate increased within 10 days. Another study that analyzed the relationship between high ED occupancy and patient mortality showed that the relative risk of death between overcrowded shifts and non-overcrowded shifts for 10 days was 0.09% [29]. Although differences in mortality have been observed in various studies, we did not find this difference between the crowded and overcrowded periods at the EDs covered in our study.
This result might be attributed to the low number of deaths reported by the hospital staff during these two periods, coupled with incomplete medical records. Notably, incomplete medical records might also have had a major effect on our results.
The present study showed that the highest percentage (38%) of deaths that occurred during the overcrowded period was realted to patients between 30 and 44 years of age, while patients between 60 and 74 years of age accounted for 36%. This is inconsistent with the findings of Richardson [27] which showed that mortality was concentrated around the elderly age group.
The mortality rate based on demographic valuables in our study showed no statistically significant results for gender. However, it was noted that the percentage of mortality in men (68%) was twofold higher than in women (32%). Similar results were obtained in two studies conducted in Sao Paulo [ 30 ] and Nigeria [31], respectively, wherein the males had higher hospitalization and mortality rate than the females.
The current study also assessed patient triaging, revealing that the largest number of patients was associated with level four (62.7% of the total patients in the overcrowded ED) and level five (33.1% in the overcrowded ED) triaging, being in line with the findings of Berg et al. [29] and Alyasin and Douglas [32]. While our study utilized nurse triage data, evidence from other studies suggests that the physician-led triage process elicits better outcomes, quality, and efficiency [33]. This is also an area of concern, as more evidence on physician-led triage is emerging in recent years.
Further, we discovered higher levels of admissions in the critical care unit during the ED overcrowding period compared with other periods, which is also in line with the trends observed in previous researches around the world [34]. In general, our study showed no association between ED crowding status and mortality rate.
5. LIMITATIONS
Our study has some limitations. First, it was performed in a single tertiary hospital, so generalization to other medical institutions should be done with caution. Second, our data were retrieved from an electronic health data record system with incomplete data entries, so it is recommended that future studies focus on the aspects of completeness and quality of electronic health record data. Third, while this study highlighted patient outcomes in terms of mortality, future studies are recommended to consider other important patient outcomes, such as patients leaving without being seen, against medical advice, or before consultation due to high crowding conditions. Fourth, while our study explored traditional ED practices such as nurse triaging, other methods such as ED physician triaging should be taken into consideration in future research. Fifth, the occupancy rate in this study exceeded for all quarters, indicating that all quarters were crowded periods. For this reason, we used the number of patient visits in the individual quarters of 2018 to classify the quarters as less crowded and overcrowded. Therefore, methods other than using both the occupancy rate equation and the number of patient visits for quantifying quarters as low and high should be considered in future studies.
Finally, as the nature of the current study was retrospective, there might be other confounding factors influencing mortality that were not apparent in the patients’ medical records.
6. RECOMMENDATIONS
We recommend that public awareness be increased regarding the services provided at public health centers, particularly in the ED.
Furthermore, we suggest increasing the bed occupancy in EDs and enhancing the soft skills of electronic health record personnel in order to train them to promptly enter complete and accurate patient data in the electronic medical record system. Additionally, we suggest looking at process improvements to reduce the length of stay in EDs and, ultimately, to mitigate overcrowding, through strategies such as incorporating a fast-track system with appropriate physician or physician assistant staffing. In addition, we highly recommend conducting further research to explore the impact of crowding on patients’ healthcare in teaching hospitals versus other hospitals.
CONCLUSION
Although we did not find significant associations between ED overcrowding and increase in mortality rate in our study, we suggest that productive measures to decrease crowding in EDs be deliberated upon and implemented based on previous literature showing that overcrowded EDs can lead to adverse patient outcomes.
Factors such as triage priority, shift time, and demographic considerations constitute some of the basic elements of studies of this nature, but they have not been considered as major factors in previous studies. Thus, future research should focus on these factors to further explore this topic.
AUTHORS’ CONTRIBUTIONS
Conceptualization, F.Y.K. and M.F.Q.; methodology, F.Y.K. and M.F.Q.; formal analysis, F.Y.K.; investigation, F.Y.K.; writing and original draft preparation, F.Y.K.; writing, review and editing, M.F.Q.; supervision, M.F.Q. All authors have read and agreed to the published version of the manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from research ethical review board of Imam Abdurrahman Bin Faisal University, Saudi Arabia (Approval No. IRB-PGS-2019-03-399).
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data that supports the findings of this article is available from the corresponding author [M.F.Q], upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


