All published articles of this journal are available on ScienceDirect.
Knowledge, Attitude and Perception of the National Health Insurance Amongst Health Workers in Ugu District, Kwa-Zulu Natal, South Africa in 2017
Abstract
Background:
South Africa aims to progress towards universal health coverage by implementing the National Health Insurance (NHI). The perception and actions of health care workers influence the successful implementation of any intervention.
Aim:
The aim of the study was to establish the knowledge, attitude and perception of National Health Insurance amongst health care workers in Ugu in 2017
Methods:
A descriptive cross-sectional study using self -administered questionnaires were used to gather information from 380 conveniently selected respondents between October 2017 and December 2017 across all health facilities in Ugu Health District. To establish associations between demographic factors and knowledge, attitude and perception on NHI, Chi- Square (X2) test and multivariate logistic regression were analysed.
Results:
Most respondents were aware of National Health Insurance (96.84%). However, only 33% had detailed knowledge of the objectives of National Health Insurance. There was a significant relationship between age less than 45 years and more than 10 years of experience on knowledge of National Health Insurance. The overall perception of National Health Insurance was good (61.92%), despite 60% of respondents believing that there was no proper communication regarding National Health Insurance by the government. Healthcare workers who live in the urban residential area had a better perception of National Health Insurance. The attitude towards NHI was positive, as 77.84% of respondents were willing to comply with the requirements of National Health Insurance.
Conclusion:
A targeted approach for communicating information about the National Health Insurance and an increased investment could improve its credibility and effective application.
1. BACKGROUND
South Africa currently utilises 8.7% of its Gross Domestic Product (GDP) on health services, with 4.2% of the GDP used for covering 84% of the population within the public health sector, and the private sector serving 16% of the population spending 4.5% of the GDP [1]. Despite South Africa’s high healthcare expenditure, the health outcomes are inferior compared to most middle- income countries [2].
South Africa is saddled with a quadruple burden of illness, specifically, the extraordinary prevalence of HIV and Aids, maternal and child morbidity and mortality, non- communicable disease and violence, injury and trauma [3]. Risk factors such as unsafe sex, interpersonal violence as well as alcohol abuse and malnutrition exacerbate the quadruple burden of disease [3]. Compounding the ever-increasing burden of diseases, institutions in the public sector have been prone to poor management, deteriorating infrastructure, insufficient resources, inferior quality of care and a shortage of key medical staff [4].
Universal Health Coverage (UHC) has emerged as a key reform for the health sector in order to provide access to quality and affordable health services for all [5]. The three dimensions of UHC include financial protection (what do people have to pay out of pocket), services (which services are covered) and population (who is covered) [5].
The South African Government has embarked on a number of initiatives to implement UHC. To improve population health coverage and quality of services, the National Department of Health has introduced the ideal clinic model and primary health care re-engineering that aims to move health care closer to the people whilst simultaneously addressing curative and preventative health [6]. To provide financial protection, to reorganize the funding of health care in pursuit of monetary risk shield, safeguarding efficiency in how funds are pooled and used thus eliminating fragmentation, thereby creating a unified health system implementing National Health Insurance (NHI) [7].
The NHI Fund will be the single strategic, publicly owned purchaser that will buy healthcare services [7]. The Office of the Health Standards and Compliance () will approve, certify and hire service providers. Beneficiaries are expected to utilize designated General Practitioners as main health care providers whilst still adhering to a referral pathway [7].
The NHI Bill lays the legal context for the implementation of NHI and recommends the creation of the National Health Insurance Fund as well as its control and advisory organizations. The NHI Bill sets out a three-phase timetable for the implementation of the NHI. Phase one between 2012 and 2017 entailed an analysis of health system and initiation of pilot sites. Phase two, between 2017 and 2022, will see the establishment of institutions, which will be the basis for an entirely efficient fund. The Minister will establish interim committees and there will be introduction of legislative reforms and provisional procuring of personal healthcare services for susceptible people [7]. Phase three, between 2022 and 2026,will involve extension of health system consolidation undertakings, deployment of added resources permitted by Cabinet and choice of commissioning of health services from private suppliers [7].
The envisaged impact of the NHI is that South Africans will receive comprehensive health care in both public and private health services near where they live, without payment at the area of service provision. This will result in households having increased disposable income. Individuals who have private cover will also benefit from the NHI [7].
Health care workers are at the centre of the healthcare delivery system. The success of implementing the NHI depends on health care workers understanding the key principles of the NHI [8]. The way health care workers perceive NHI will influence their contribution to the effective application of the NHI [9]. Anecdotal evidence suggested that health workers in general are not familiar with NHI or the content of the NHI Bill. This study aims to determine the knowledge, perceptions and attitudes of healthcare workers in Ugu towards the NHI.
2. MATERIALS AND METHODS
2.1. Study Area and Design
An observational cross-sectional study, with an analytical component, was conducted at the Ugu Health District, South coast of KwaZulu-Natal, expanding to the interior. There are three district hospitals, one regional hospital and one Tuberculosis Hospital in Ugu. There are two community health centres (Gamalakhe and Turton) and 52 clinics.
2.2. Study Population and Sampling
The study population included all healthcare staff from the district office, one regional hospital, three district hospitals, one specialised TB hospital, two Community health centres and 52 clinics within Ugu Health District. The estimated total number of healthcare staff of various categories across the district was 4500. A sample size of 384 respondents was determined based on a projected population fraction of 50%, confidence interval of 95% and a relative precision of 10%. Convenience sampling was used to select the respondents.
2.3. Study Instrument
A self-administered questionnaire that provided primary quantitative data was used. The questionnaire covered closed-ended questions with a room for explanations where it is expected. The questionnaire was based on a pre-existing tool from a study on assessing NHI readiness in the pilot districts of KZN [10, 11] that was modified to suit this study. The questionnaire was divided into four sections: Section A: socio-demographic features entailing 5 items, Section B: Included knowledge of NHI consisting of 7 items, Section C: Included perception of NHI consisting of 4 items and Section D: Included attitude of NHI consisting of 5 items.
A pilot study was performed to pre-test the questionnaire and confirm that the questionnaire was in alignment with the study objectives. The questionnaire was administered twice to a sample of ten respondents within an interval of two weeks. The pilot study respondents were not part of the actual study. The correlation coefficient of the questionnaire was established as 0.82.and found to be acceptable and free of ambiguity for the study.
2.4. Data Collection
Primary data were collected from district office management and staff on 2nd October 2017 at 11:30AM after a District health-planning meeting. An information sheet, consent form, gatekeeper permission and ethics approval were provided to each respondent. The questionnaires were anonymous. A letter of introduction was provided indicating that all information collected was for research purposes only and will be treated as confidential. Respondents were informed by the researcher that name or identity was not required. Instructions were provided to select the response that is most fitting with a tick and offer a reason in simple words where appropriate.
The researcher used Monitoring and Evaluation Managers of each facility as research assistants and trained them before data collection on administering questionnaires to health care workers who met the inclusion and were willing to be involved in the research, within their facilities. Information and cash flow meetings between October 2017 and December 2017, where health care workers from the facility and clinics were present, were used to collect the data.
2.5. Data Management and Analysis
All questionnaires received were distinctively coded with the date and location of data compilation as well as the name of the data gatherer. Data were entered into a database. A password was required for entry into the database. All electronic softwares were stored, archived and a backup was kept in an external hard drive.
Descriptive statistics were utilized to define baseline features such as age, gender, education and marital status. The mean and median were utilised for continuous variables. Proportions were used for categorical variables. Frequency tables were created for categorical variables depicting frequencies and percentages for socio-demographic characteristics.
2.5.1. Knowledge
There were 10 questions and a score of 1 was allocated to each question that was answered correctly. A score of 0-4 was scored as “poor knowledge”, a score of 5-7 was scored as “moderate knowledge” and a score of 8-10 was scored as “exceptional knowledge”.
2.5.2. Perception
Respondents were asked if they will benefit from NHI?. “Yes” was scored as 1 and “no” as 0. Frequency calculations were done to calculate the percentage of participants that answered yes and those that answered no from each group.
2.5.3. Attitude
Respondents were asked a question whether they will adhere to all the requirements of NHI that may be required of them. “Yes” was scored as 1 and “no” as 0. Frequency calculations were made to analyse the percentage of participants that answered yes and no from each group.
The association amongst the knowledge of NHI with independent categorical variables namely age, gender, education, salary level and experience were investigated using chi-squared test. Odds ratios were used as the measures of association and the confidence intervals of these ratios were calculated. Variables found to be significant at the bivariate analysis and variables that had suggested associations in previous research were considered in the multivariate analysis.
2.6. Ethical Consideration
There were no direct ethical risks to the study respondents. Questionnaires were administered anonymously to all consenting respondents, thus ensuring and maintaining confidentiality and privacy. The researcher ensured that participation was voluntary and signed agreement was acquired from the participant before continuing with the questionnaire. Ethical approval was obtained from the Biomedical Research Ethics Committee of the University of KwaZulu-Natal, Durban (Reference number BE216/17. Permission to undertake this study was acquired from the University of KwaZulu-Natal’s Postgraduate Research Committee and gatekeeper’s authorisation was also attained from the Ugu District Health Office and the Provincial Health Research and Knowledge Management sub – section.
3. RESULTS
Three hundred and seventy-nine respondents participated in the study. Eighty-three percent of the respondents were hospital-based employees, with the other 17% based at large community health centres. Most of the respondents were nurses (40.9%, 155) with a further quarter of the sample being administrative staff (25..0%, 95). Doctors (3.7%, 14) and pharmacists (6.3%, 24) comprised one-tenth of the sample. Of the sample of respondents, 48% (179) had beyond 10 years of service, 31% (118) had fewer than 5 years of service and 21% (82) had 5 to 10 years of service. A large number of the respondents (60.7%, 230) reside in urban areas as compared to (38.3%, 149) that reside in rural areas. One hundred and eighty-six (65.3%) of the study population were between 20 to 45 years of age, compared to ninety-nine (34.7%) who were between 46 to 65 years of age. There were three times more females (74.9%, 284) as compared to males (25.0%, 95) (Table 1).
| Variable | Study Sample | |
|---|---|---|
| - | Frequency | Percent |
| Category of health worker (n = 379) | ||
| Administrative staff | 95 | 25.0 |
| Manager | 58 | 15.3 |
| Nurse | 155 | 40.9 |
| Doctor | 14 | 3.7 |
| Pharmacist | 24 | 6.3 |
| Allied worker | 33 | 8.7 |
| Years of working experience (n = 379) | ||
| less than 5 years | 118 | 31.1 |
| 5 to 10 years | 82 | 21.6 |
| more than 10 years | 179 | 47.2 |
| Residence (n = 379) | ||
| urban | 230 | 60.7 |
| rural | 149 | 39.3 |
| Age (n = 285) | ||
| 20-45 years | 186 | 65.2 |
| 46-65 years | 99 | 34.7 |
| Gender (n = 379) | ||
| Male | 95 | 25.0 |
| Female | 284 | 74.9 |
| Marital Status (n = 378) | ||
| Single | 180 | 47.6 |
| Married | 156 | 41.3 |
| Separated/divorced | 21 | 5.6 |
| Living with partner (co-habiting) | 8 | 2.1 |
| Widow/widower | 13 | 3.4 |
| Level of Education (n = 379) | ||
| No school | 1 | 0.3 |
| Primary | 6 | 1.6 |
| Secondary | 7 | 1.9 |
| Post Matric | 365 | 96.3 |
3.1. Awareness and Knowledge of NHI
Ninety-seven percent (368) of the respondents indicated that they had heard of the NHI. Of those who had indicated that they had heard of the NHI, 70.0% had learned of this from their health facility, while the remaining 30.0% obtained information from the media (radio, television and / or newspaper).
Two-thirds (66.6%) more participants had basic information on NHI, whereas only one-third (33%) of the participants were familiar with details regarding the objectives of NHI (Table 2).
3.2. Perception of NHI
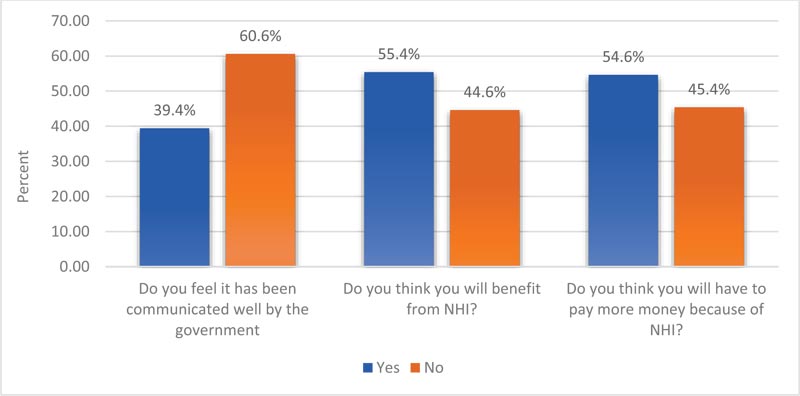
Most respondents (61%; n=231) indicated that the NHI would be helpful, whilst a little more than one third (38%; n=145) indicated that the NHI would not be successful. Sixty percent of respondents (229) believed that the Government did not communicate information about NHI adequately (Fig. 1).
3.3. Attitude Towards NHI
Seventy-eight percent (296) of respondents were willing to adhere to the requirements of NHI. There were nearly as many respondents who believed that the responsibility lay with health facilities (47.76%) as there were those who believed that the responsibility lay with the individual (52.24%) (Table 3).
| - | Frequency (Correct response) | Percent |
|---|---|---|
| a) NHI stands for National Insurance System | 245 | 66.6 |
| b) NHI is a government initiation | ||
| c) The government wants to provide an equitable health care for every South African citizen through NHI | ||
| d) All South African have to contribute towards NHI depending on how much they earn | ||
| e) NHI means that I don’t have to pay when I am cared for in a private facility | 123 | 33.4 |
| f) NHI has not started in public health facilities | ||
| g) NHI will expand public clinics and General Practitioner's clinics so that everyone has a health provider next to them | ||
| h) NHI will ensure that people get treatment before they get very sick and hence get treated at a clinic level effectively | ||
| i) NHI is now at a pilot phase being piloted at Umzinyathi, Amajuba and Umgungundlovu | ||
| j) Private health sector and medical aids are an important part of NHI |
| Number | Frequency | |
|---|---|---|
| Are you going to adhere to all the requirements of NHI that may be required from you? | 296 | 78.1% |
| Responsibility of NHI | ||
| Health facility | 181 | 47.8% |
| Individuals | 198 | 52.2% |
3.4. Association between Respondents Demographics and Knowledge, Attitude and Perceptions Towards NHI
3.4.1. Knowledge
Good knowledge was equated to a respondent’s score of ≥75 percent Bivariate analysis showed: nurses (Odds ratio (OR):1,36; 95% CI,08-22;); females (OR:138;95% CI,08-23;) and respondents with post matric education (OR:133;95% CI,03-45;) showed an increased but not significant odds of having a better knowledge of NHI Respondents less than 45 years (OR: 193; 95% CI, 10-37;) and respondents who had beyond 10 years of experience (OR: 166 95% CI, 10-26;) showed a statistically significant increased odds of having better knowledge on NHI After multivariate analysis, age (OR: 136; 95% CI, 06-29;) and respondents who had more than 10 years of experience (OR: 152; 95% C1, 07-30;) showed increased odds of having better knowledge on NHI, this was not statistically significant.
3.4.2. Perceptions
Respondents who lived in urban residential area (Odds ratio (OR) 211; 95% CI. 10-449;) showed a statistically significant increased odds of better perception of NHI. After multivariate analysis, respondents from urban residential area (OR 089; 95% CI. 023 – 043;) and females (OR 086; (95% CI 025-05; P=061) were less likely to have a better perception of the NHI. Age less than 45 years (OR 196; 95% CI. 064-206;) was a statistically significant factor for better perception of NHI.
3.4.3. Attitudes
Nurses (OR 05; 95% CI 03-08) showed a statistically significant but less likely odds of better attitude towards NHI, whilst those under 45 years (OR 19; 95% CI. 103-37)) displayed a statistically significant increased odds of better attitude towards NHI Nurses with more than 10 years of experience (OR: 1.08; 95% CI.06-18). Females (OR: 1.38; 95% CI.08-23) and those with post matric (OR: 1.3; 95%CI.03-45) showed an increased but non-significant odds of having better attitudes towards NHI After multivariate analysis. Nurses less than 45 years (OR 13; 95% CI. 05 – 08;) and those with post-matric (OR 19; 95% CI. 17 – 07;) showed increased but non-significant odds for better attitude towards NHI Nurses (OR 04; 95% CI 01-28;) showed a statistically significant but less likely odds of better attitude towards NHI .
4. DISCUSSION
The profile of respondents in the current study of a majority of nurses (409%, 155) having more than 10 years of service (48%; 179), more females (7493%, 284) and the majority being between 20 to 45 years of age (186; 653%) is reflective of the profile of the health workforce of in the public health sector of South Africa (Table 4).
| Knowledge | Perception | Attitudes | |||||||||||||||||
| Bivariate Analysis | Multivariate Analysis | Bivariate Analysis | Multivariate Analysis | Bivariate Analysis | Multivariate Analysis | ||||||||||||||
| Variable | Categories | Unadjusted OR | 95% CI | - | Adjusted OR | 95% CI | p-value | Unadjusted OR | 95% CI | - | Adjusted OR | 95% CI | p-value | Unadjusted OR | (95% CI) | - | Adjusted OR | 95% CI | - |
| Category of healthcare worker | Nurses versus other | 1.36 | 0.8-2.2 | - | 1.44 | 0.8-2.5 | - | 0,83 | 0,54-1,28 | - | 0.91 | 0.23-0.35 | - | 0.5* | 0,30-0,84 | - | 0.4* | 0.1-2.82 | - |
| Years of experience | > 10 years versus < 10 years | 1.66 * | 1.0 – 2.6 | - | 1.52 | 0.7-3.0 | - | 1,15 | 0,74-1,77 | - | 0.95 | 0.30 –1.3 | - | 1.08 | 0,64-1,81 | - | 0.72 | 0.26-0.88 | - |
| Area of residence | Urban versus rural | 0.57 * | 0.3-0.9 | - | 0.58 | 0.3-1.05 | - | 2.11* | 1.00 – 4.49 | - | 0.89 | 0.23—0.43 | - | 6.0 | 0.36 – 1.1 | - | 0.9 | 0.28-0.33 | - |
| Age | < 45 years versus > 45 years | 1.93 ** | 1.0-3.7 | - | 1.36 | 0.6-2.9 | - | 1.44 | 0.85 – 2.44 | - | 1.96* | 0.64 – 2.06 | - | 1.9* | 1.03-3.7 | - | 1.3 | 0.55-0.85 | - |
| Gender | Female versu males | 1.38 | 0.8-2.3 | - | 1.38 | 0.7-2.5 | - | 0.99 | 0.60 – 1.62 | - | 0.86 | 0.25 – -0.5 | - | 1.38 | 0.81 -2.3 | - | 0.7 | 0.26-0.9 | - |
| Marital status | Single versus married | 0.86 | 0.5-1.3 | - | 1.28 | 0.7-2.3 | - | 1,46 | 0,95-2,26 | - | 1.66 | 0.45 – 1.88 | - | 0.86 | 0.5-1.3 | - | 0.5 | 0.18-1.73 | - |
| Education | Post matric versus less than matric | 1.33 | 0.3-4.5 | - | 0.50 | 0.05-4.4 | - | 0,49 | 0,11-1,74 | - | 1.07 | .0.85 – 0.9 | - | 1.3 | 0.3-4.5 | - | 1.9 | 0.7-1.7- | - |
The findings of this study indicate that most health care workers in Ugu (968%) are familiar with the basic concept of NHI, of which 70% heard about NHI from their health facility and 85% were aware of NHI services to be offered at the health facility. This potentially implies that basic training or seminars on NHI in the facilities have yielded positive results of creating awareness on NHI. The high level of awareness is consistent with previous studies conducted amongst healthcare professionals in Mthatha General Hospital), OR Tambo district, that showed 90 of the 100 respondents surveyed were aware of NHI [10]. A previous study from EThekwini Metro and Ugu districts in Kwazulu-Natal province documented 91% level of awareness among health professionals [11].
Two-thirds (666%) more participants had basic information on NHI, whereas only one-third (33%) of the participants were familiar with details regarding the objectives of NHI. This may be attributed to the lack of detail of the training program. Concurring with these results a cross - sectional study (n=253) conducted of health care staff in a tertiary hospital in Limpopo showed that although 64% of respondents knew what NHI is about, 48% did not know about policy content [12]. It is worth noting that both these studies were at non-NHI pilot sites. Corroborating with the results of poor knowledge on objectives of NHI by health care staff, was a cross-sectional survey regarding awareness of health care workers on NHI in Tshwane (n-480), where 58% of respondents were not familiar with the objectives of NHI [13] In contrast to these findings, a study conducted in the three KZN NHI pilot districts showed that 93% of health workers had good knowledge of the NHI, whilst in Mtata General Hospital 81% of the respondents knew the objectives of NHI
The statistically significant relationship between younger ages (< 45 years) and better knowledge and attitudes towards NHI could be because of younger health workers having more opportunities for exposure to seminars and training programs. In addition, younger age groups are more technologically savvy and have internet access and engage on social media platforms. In contrast to these findings, a study of private Doctors in Ethekwini indicated that older people are more inclined to favour redistribution and hence have a positive attitude towards NHI, as one of the key objectives of NHI is redistribution and sharing of resources [11].
More than half (606%) of the respondents believed that NHI was not well communicated by the government and 546% believed they will have to pay more money because of NHI. Nevertheless more than half of the respondents (619%) still believed that NHI will help them a lot and they will benefit from NHI (554%). Similar findings of support for NHI were established in Mthatha General Hospital on the awareness, knowledge and perception of health care staff on NHI, where 79% supported the implementation of NHI, although more than half of the respondents believed that they would be taxed more to fund the program [10]. Ambivalent perceptions were reported from a study of private doctors in KwaZulu-Natal where only 21% of doctors had a good perception of NHI. The poor perception was attributed to the lack of clarity and control mechanisms regarding risks [14]. This is further exasperated by the constant reports of fraud and corruption in the media by South African Government Departments, politicians and Parastatals. This suggests that the NHI Policy and NHI Bill is not clear in terms of risk mitigation strategies and requires further clarity during stakeholder engagements.
A study on the three pilot districts in KwaZulu-Natal found that more than 50% of health care workers were optimistic about NHI [11]. However, the inference is that the balance of the health care workers in the said study had a poor perception of NHI and believed NHI will not help them. Similarly, a study of health care workers in Limpopo revealed that only 40 percent of respondents had the perception that their facility was ready to implement NHI due to lack of sufficient resources [12]. Some of these health care workers are under the impression that there is a serious lack of resources within public health. This insinuates the need to increase resources in order to improve credibility in the effective application of NHI.
Although only a handful of studies have documented the perceptions on NHI, it is evident that the responses of health care staff on their perception of NHI are varied. However, negative perceptions can hinder success. On the other hand, a good knowledge of the objectives of NHI could inspire an optimistic perception and, therefore successful implementation.
The study found that most (778%) of the respondents were willing to adhere to the requirements of NHI and more than half of the respondents believed that NHI will help them a lot. Similarly, a cross sectional study in Nigeria regarding knowledge and attitude of health professionals towards the National health insurance scheme indicated that health workers had a positive attitude towards the NHI [15]. On the contrary, in the study of private doctors in Ethekwini and Ugu, less than 50% of the respondents indicated that they are ready to implement NHI, citing lack of resources as a challenge [11]. Similarly, lack of staffing and infrastructure were cited as challenges to implementation of NHI [16].
4.1. Study Limitations
The study is limited by an overall relatively small sample size. It would have been preferable to select a larger number of respondents. The small sample size resulted in the study being underpowered to detect associations of socio-demographic variables with outcome. As a result of the cross-sectional study design, causality could not be determined. Furthermore, owing to time, budget and resource shortages, a bigger overall sample size was not feasible. Perceptual studies are predisposed to subjective experiences and social desirability bias. Therefore, it may not be possible to establish if respondents were honest. Options were provided for the questions, which could have swayed the respondents towards the choices provided. The respondent’s attitudes on NHI could have negatively prejudiced their answers, for instance, an adverse attitude on the objectives of NHI could have been understood as absence of knowledge. The study was conducted in 2017 after the release of the NHI white paper. However, the NHI Bill and the Medical Schemes Amendment Bill were subsequently released in 2018. The publicity around the said Bills in the media, may have improved the knowledge of health care workers on NHI and changed their perception and attitude towards NHI.
CONCLUSION
This study has revealed that majority of the respondents know about NHI but they are not familiar with the details regarding the implementation of NHI. In addition, the lack of clarity and control mechanism regarding risk have served to perpetuate the negative perceptions toward the NHI. The impression of a serious lack of resources within public health sector continues to perpetuate a negative perception and attitude towards the NHI. In order to improve knowledge, attitudes and perceptions towards the NHI, it is imperative that a modified approach is adopted for communicating and training about the NHI and an increased investment could improve credibility in the effective application of NHI
LIST OF ABBREVIATIONS
| GDP | = Gross Domestic Product (GDP) |
| KZN | = KwaZulu Natal |
| NHI | = National Health Insurance |
| OR | = Odds Ratio |
| UHC | = Universal Health Coverage |
AUTHORS’ CONTRIBUTIONS
All authors gave intellectual inputs to the study protocol and drafting of the manuscript. NG conducted data collection and analysis. All authors approved the final draft of the manuscript for submission.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Biomedical Research Ethics Committee of the University of KwaZulu- Natal, South Africa (Reference number BE216/17). The management of uGu district and the Provincial Knowledge Unit gave permission for the implementation of the study.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Each participant signed an informed consent for the voluntary participation in the study.
STANDARDS OF REPORTING
STROBE guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available on request from the corresponding author [N.G].
FUNDING
The study was self-funded by the researcher. No external funding was received.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors are grateful for the support of the staff of the facilities in Ugu district.


