All published articles of this journal are available on ScienceDirect.
Treatment and Prevention of Osteoporosis during COVID-19 Outbreak: Management and Adherence to Treatment Guidelines
Abstract
A total of 219 countries, areas, or territories have globally witnessed the existence of a novel Coronavirus (COVID-19) pandemic over the last few months, which posed serious threats to human health. The viral incubation period varies from 2 to 14 days. It has been observed that osteoporosis patients are likely to be at high risk of COVID-19 contracting sequelae. Osteoporosis is a chronic condition that reduces bone strength and increases the risk of fracture. Osteoporosis typically requires sustained therapeutic intervention to reduce the risks of further bone loss, structural integrity impairment and incidence of fractures. In the COVID-19 pandemic, diagnosis of chronic osteoporosis conditions should not become an unwanted casualty. Metabolic bone condition may lead to complications in COVID-19 infected patients. Orthopaedic doctors are being redeployed in different hospitals to treat COVID-19 infected patients. Thus, the orthopaedics community needs compulsory training to understand the symptoms of this condition. Orthopaedics surgery and trauma surgery are challenging in a hospital setup with limited availability of hospital staff and operating facilities. Clinicians must respond to the challenges raised by this crisis and consider ways of continuing to help patients with chronic diseases with their substantive morbidity and mortality.
A total of 219 countries, areas, or territories have been globally witnessing the existence of a novel Coronavirus (COVID-19) pandemic for the last few months, which posed serious threats to human health. In December 2019, a group of patients in Wuhan, China, started reporting symptoms that resembled pneumonia. The causative agent was identified as the 2019 novel Coronavirus (COVID-19). The World Health Organization (WHO) subsequently changed the name of the virus to Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV2). SARS-CoV is a positive-stranded RNA virus of the Coronaviridae family. Severe acute respiratory syndrome coronavirus and Middle East Respiratory Syndrome Coronavirus (MERS-CoV) are the viruses that also belong to the Coronaviridae family. The WHO officially defined the COVID-19 outbreak as a pandemic on 11th March 2020 [1-3]. Until November 9, 2020, a total of 50030121 confirmed cases and 1252072 deaths were recorded worldwide due to the COVID-19 infection [4].
The disease is transmitted through inhalation or contact with infected droplets. The viral incubation period varies from
2 to 14 days. The symptoms typically include nausea, sore throat, cough, breathlessness, malaise, and exhaustion. The mild symptoms can progress to pneumonia, Acute Respiratory Distress Syndrome (ADRS) and multi-organ failure (usually the elderly and those with comorbidities). Several people get the asymptomatic infection. The case-fatality ratio is estimated to be 2.51%. The case fatality ratio is calculated using the below formula [5]:
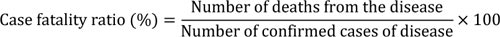 |
The viral infection can be diagnosed by a special molecular examination of the presence of virus in respiratory secretions. Different laboratory findings include normal/low counts of white cells with high C-reactive Protein (CRP). The computerized tomographic chest scans are usually abnormal even in those with no symptoms or minor illnesses. Treatment is generally supportive; antiviral agent function has yet to be identified [6]. Synthesis of better medicines requires proper disease modeling. At present, several research organizations are globally working on the development of vaccines for COVID-19 [7].
Osteoporosis is a chronic condition that reduces bone strength and increases the risk of fracture. Osteoporosis typically requires sustained therapeutic intervention to reduce the risks of further bone loss, structural integrity impairment and incidence of fractures. Osteoporosis patients are likely to be at high risk of COVID-19 contracting sequelae. Telehealth consultations can minimize the risk of infection through social distancing and isolation. In the COVID-19 pandemic, diagnosis of chronic osteoporosis conditions should not become an unwanted casualty. Clinicians must respond to the challenges raised by this crisis and consider ways of continuing to help patients with chronic disease with their substantive morbidity and mortality [8].
Oral bisphosphonate therapy can be initiated via telephone or video visits, and it should not be delayed in patients who are at high risk of fracture. Examination of bone mineral density may need to be postponed if public health guidance recommends that elective procedures be halted. Patients already taking osteoporosis medications should continue to receive these medicines, including oral and intravenous bisphosphonates, estrogen, enosumab, raloxifene, abaloparatide, teriparatide and romosozumab, if safe. There is no evidence that any osteoporosis treatment increases the risk or severity of COVID-19 infection or alters the disease course. However, there are early signals that COVID-19 may be followed by an increased risk for hypercoagulable complications, in which case, caution should be taken for raloxifene and estrogen, both of which can modestly raise the thrombotic risk. Laboratory evaluation is recommended for patients with fluctuating renal function, and those at higher risk of developing hypocalcemia due to malabsorptive disorders, advanced renal dysfunction, hypoparathyroidism, or diuretics with loops [9].
The metabolic bone condition may lead to complications in COVID-19 infected patients. However, no clinical evidence is available, indicating the high risk of viral infection in such patients. The bone disease occurs in hypoparathyroidism due to the deficiency of the parathyroid hormone. Observational studies hypothesized an increased risk of hospitalization in patients with hypoparathyroidism due to the viral infection. However, this relationship is unclear, and no data are available on the risk of COVID-19 infections in patients with hypoparathyroidism. Vitamin D may reduce the risk of respiratory infections through the modulation of inflammatory cytokine profiles and cathelicidins and defense induction. Vitamin D may reduce the risk factor for acute respiratory distress syndrome that can further minimize the life-threatening risk of COVID-19 complications. Metabolic bone disorder management depends on the regulation of vitamin D status [10].
Orthopaedic doctors are being redeployed in different hospitals to treat COVID-19 infected patients. COVID-19 may affect bones and joints. Thus, the orthopaedics community needs compulsory training to understand the symptoms of this condition. Orthopaedics surgery and trauma surgery are challenging in a hospital setup with limited availability of hospital staff and operating facilities. Patients are unable to perform day-to-day functions due to this panic disorder. To avoid the risk of current COVID-19 pandemic and monitor health, it is important to monitor the infectious agent, its disease-causing capacity and community transmission patterns. The risk of COVID-19 can be minimized by: (i) warning for future health problems, (ii) orthopaedics meetings can be held online or through video and audio call, (iii) improvements of orthopaedics surgeon’s experience and work efficiency, (iv) improved support for complex cases, and (v) better protection of hospital staff.
Patient safety and infection management is a major priority. Some precautionary measures need to be taken like cover mouth, avoiding close contacts, regular hand washing, etc. COVID-19 may affect orthopaedic surgeons in their everyday work. Artificial intelligence-based technologies such as wearable sensors and video conferencing tools can be adapted for remote monitoring of patient outcomes such as knee motion range after knee arthroplasty without subjecting patients to cumbersome hospital visits. In addition to ease of monitoring, technology-assisted recovery (such as online education platforms or game-based therapy) has also contributed to substantially enhanced patient satisfaction [11].
To minimize the risk of COVID-19 infection in patients whose life expectancy is less than 3 months, 8 Gy in one fraction (a short-course palliative radiotherapy) can provide effective palliation by reducing the number of hospital visits. The benefits and risks of radiotherapy care need to be discussed with patients to reach a joint decision to ensure patient safety. The radiation room and nearby areas should be sanitized, and protective measures should be taken by to patients and radiotherapy technicians. A short course of stereotactic radiotherapy can be given to oligometastatic or oligoprogressive patients [12].
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


