RESEARCH ARTICLE
The Effectiveness of Postoperative Antibiotics following Appendectomy in Pediatric Patients: A Cost Minimization Analysis
Rano K. Sinuraya1, 2, *, Aida N. Aini1, Cherry Rahayu3, Nasrul Wathoni4, Rizky Abdulah1, 2
Article Information
Identifiers and Pagination:
Year: 2020Volume: 13
First Page: 80
Last Page: 86
Publisher ID: TOPHJ-13-80
DOI: 10.2174/1874944502013010080
Article History:
Received Date: 22/06/2019Revision Received Date: 19/12/2019
Acceptance Date: 08/1/2020
Electronic publication date: 20/03/2020
Collection year: 2020

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Appendicitis has a high occurrence and is frequently indicated in pediatric abdominal surgery. However, up to 33% of affected children may not present with distinct symptoms, and young children may be a typical or show delayed presentation of symptoms. Appendectomy is one of the most common emergent surgeries to treat appendicitis. After an appendectomy, prophylaxis antibiotics are required to abate infections at the location of surgery and have been shown to reduce postoperative surgical complications significantly.
Objective:
The purpose of this investigation was to determine the most cost-effective prophylactic antibiotic combination between ceftriaxone-metronidazole and cefotaxime-metronidazole following appendectomy.
Methods:
A retrospective observational study was conducted using investigations with a similar design and pediatric medical records from 2011 until 2013 from a referral hospital in Bandung City. All direct medical costs related to pediatric appendectomy were collected and discounted. Independent Student’s t-test and chi-square analysis were used.
Results:
The average total cost of ceftriaxone-metronidazole was USD 393.83/patient and that of cefotaxime-metronidazole was USD 397.89/patient. There were no significant differences in average direct medical costs between treatments with ceftriaxone-metronidazole and cefotaxime-metronidazole (p=0.383). The analysis suggests that both antibiotic combinations have the same effectiveness and cost. For the combinations of ceftriaxone-metronidazole and cefotaxime-metronidazole, approximately USD 1.88 and USD 2.28 were required, respectively, to reduce one day of hospitalization after an appendectomy. Additionally, to increase one percent of cure rate, an amount of USD 19.70 and USD 24.89 was required for ceftriaxone-metronidazole and cefotaxime-metronidazole, respectively.
Conclusion:
Both therapies investigated were effective as a postoperative antibiotic. However, the combination of ceftriaxone and metronidazole may be more cost-efficient.
1. INTRODUCTION
World Health Organization mentioned that the incidence of appendicitis in Asia and Africa in 2004 consisted of 4.8% and 2.6% of the total population [1]. According to data from the Household Health Survey in Indonesia, the incidence of appendicitis is highest when compared to other cases of the abdominal disease [2]. Approximately 80,000 children become afflicted with appendicitis in the United States each year, compared to 4 per 1,000 children under 14 years old in other countries. Perforated appendicitis often occurs in children under the age of 18 years or adults above 50 years old [1, 3].
Appendectomy is the most common surgical procedure for treating appendicitis, and the mortality rate of appendicitis is high despite major advances in modern antibiotics. Although the mortality rate from an appendectomy is low (>1%) in high-, medium-, and low-income countries, the surgical mortality rates for appendectomy are quite high in low-middle-income countries (LMICs) (89/1000 operations). Previous studies have shown multifactorial issues related to the high mortality rate in appendectomy, especially in LMICs, and one of the common problems is the use of prophylactic antibiotics [4, 5].
The patient management for postoperative appendicitis is associated with the antibiotic administration. Although the role of postoperative antibiotics in reducing infection is still debatable, some studies show that antimicrobial prophylaxis should be considered due to reducing the morbidity related to infections (prolonged length of stay, readmission, and reoperation) [6]. Clinical practice guidelines of the American Society of Health-System Pharmacists (ASHP) stated that antimicrobial prophylaxis should be given before and after appendectomy. The antibiotic prophylaxis was identified as an effective intervention to prevent surgical site infections (SSIs) compared with placebo for patients who received appendectomy [7]. Several investigations have showed that preoperative prophylactic antibiotics are recommended for reducing postoperative infections or complications. Furthermore, it is strongly suggested to use broad-spectrum postoperative antibiotics, especially for appendicitis with perforation, for at least 3-5 days to reduce SSIs rate [8]. There are several antibiotics recommended for appendectomy, such as second or third-generation cephalosporins. To prevent the infection related to appendicitis, a third-generation cephalosporin antibiotic (ceftriaxone, cefotaxime) can be administered alone or in combination with metronidazole [6].
Ideally, each hospital has antibiogram guidelines, which should always be updated to determine empiric antibiotic therapy according to the existing germ patterns [6, 9, 10]. However, in the general practice hospital where this study was conducted, the most common antibiotics often used in postoperative pediatric appendectomy were ceftriaxone-metronidazole and cefotaxime-metronidazole. In this study, we assessed which antibiotic would be more cost-efficient as prophylaxis in postoperative appendicitis in pediatric patients.
2. METHODS
This was an observational study using a cross-sectional design in a referral hospital in West Java Province, Indonesia. Inclusion criteria in this study were patients aged 2-13 years, patients who were diagnosed with perforated appendicitis and who had received laparoscopic appendectomy, and patients who received antibiotic therapy ceftriaxone-metronidazole or cefotaxime-metronidazole for at least three days [8, 11]. Patients with incomplete data, referrals from other hospitals, and those exhibiting side effects of these prophylaxes were excluded from the analysis. Data were taken from patient medical records from a period of 2011-2013, and the records covered the diagnosis, length of stay, antibiotics used, and therapy outcomes. In this study, we analyzed the conditions before the implementation of National Health Insurance (NHI) for appendicitis, particularly in the costing system. Due to the changes implemented in the NHI programs in 2014 in Indonesia, the diagnosis, treatments, and costs are based entirely on Indonesian Case-Based Groups (INA-CBGs) or Indonesian Healthcare Insurance.
Cost categories were estimated based on appendectomy protocols in this hospital, and on the total cost, while categories were based on hospital perspective. The currency units that are in Indonesian Rupiah were converted to USD using the Purchasing Power Parity exchange rates and discounted to 2018. Based on economic evaluation protocols [12], all of the costs should be discounted to the present year to adjust the present value of the cost. Then, all of the costs were classified into four groups including the cost of medicines, cost of medical or surgical supplies, cost of laboratory test, and the cost of hospitalization. This study was approved by the Health Research Ethics Committee of this referral hospital. Personal information was kept confidential by providing a numeric code for each medical record. Bivariate analysis was performed using unpaired two-tailed Student’s t-test and chi-square test. Then, a multivariable backward logistic regression analysis was conducted to determine which independent predictors have a significant association with the outcome of the prophylaxis. Probability values less than 0.05 were accepted as statistically significant. All statistical analysis was performed using SPSS 20.
3. RESULTS
There were 717 patients with appendicitis between January 2011 and December 2013 in this hospital. All data were screened, and only 62 patients met the criteria and were included in the analysis (Fig. 1). There were no differences in patient characteristics between the groups. Both the ceftriaxone-metronidazole group and the cefotaxime-metronidazole group showed a higher percentage of male patients by 64.7% and 67.9%, respectively (Table 1).
The patients’ statuses after being administered antibiotics are also reported in Table 1. Chi-square analysis showed that there was no significant difference between both groups in Length Of Stay (LOS) and discharge status. These results suggest that both ceftriaxone-metronidazole and cefotaxime-metronidazole yield similar outcomes.
In order to investigate the variables having a significant association with the outcome, multivariate analysis has been performed (Table 2) with discharge status (cure or recovery) as the outcome. It can be seen that age has the highest odds (2.625), followed by types of prophylaxis and gender.
There were no significant differences in cost (Table 3). The higher costs were associated with surgical supplies, hospitalization, and laboratory test. The difference in total cost averages between both groups was only USD 4.06.
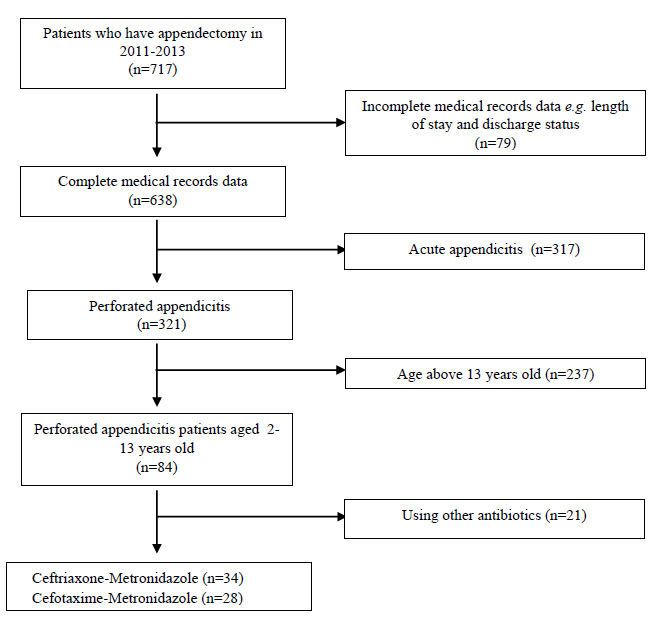 |
Fig. (1). Medical records selection process. |
| Characteristics | Combination Ceftriaxone-Metronidazole (n=34) | Combination Cefotaxime-Metronidazole (n=28) | p-value |
|
Age (years) Mean (SD) Range |
9.76 (2.35) 4-13 |
8.14 (2.98) 3-13 |
0.048* |
|
Gender, n (%) Male Female |
22 (64.7) 12 (35.3) |
19 (67.9) 9 (32.1) |
0.451 |
|
Length of Stay (day) ≤ 6 > 7 |
20 (58.8) 14 (41.2) |
16 (57.1) 12 (42.9) |
0.447 |
|
Discharged status, n (%) Cure Recovery |
20 (58.8) 14 (41.2) |
16 (57.1) 12 (42.9) |
0.165 |
| – | Coefficient (B) | S.E | Wald | p-value | OR | 95% CI | |
| Min | Max | ||||||
| Type of prophylaxis | 0.216 | 0.580 | 0.139 | 0.709 | 1.242 | 0.398 | 3.871 |
| Age | 0.965 | 0.584 | 2.728 | 0.099 | 2.625 | 0.835 | 8.251 |
| Gender | -0.871 | 0.544 | 2.565 | 0.109 | 0.419 | 0.144 | 1.215 |
| Constant | 0.173 | 0.552 | 0.098 | 0.754 | 1.189 | ||
There were no significant differences between each category of cost for both the combination groups (p > 0.05). The cost of medical or surgical supplies has the highest value, followed by the cost of hospitalization and laboratory test. The analysis was performed by comparing the total cost from each combination with LOS and discharge status as the outcome. In this condition, a cost-effectiveness analysis could not be conducted because the total cost and patients’ status (LOS and discharge) did not show a significant difference or quite similar. The cost analysis across patient status is reported in Table 4. Both combinations of antibiotics yielded the same cost and effectiveness. It was found that the average cost and effectiveness ratio for combination ceftriaxone-metronidazole or cefotaxime-metronidazole were USD 1.88/LOS and USD 2.28/LOS, respectively.
4. DISCUSSION
Perforated appendicitis is a well-described complication of acute appendicitis. Acute appendicitis is commonly undiagnosed and has no precisely defined signs or symptoms. Perforated appendicitis is characterized by a high fever and severe pain covering the entire abdomen, which typically makes the abdominal muscles tense. Acute appendicitis can become perforated appendicitis within 24–36 h, and the risk of perforation increases by 15% after 36 h. The prevalence of perforated appendicitis is higher than acute appendicitis, especially in children [13]. In this particular hospital, in 2011–2013, the number of perforated appendicitis in pediatric patients increased by 74.19%, 87.50% and 90.48%, respectively. There was no clear enlightenment related to this issue. However, previous investigations [14, 15] suggest that there are many factors related to perforated appendicitis occurrence. For example, family history of appendicitis, the timing of care (immediately or delayed), history of abdominal pain episodes, and childhood body mass index all play critical roles in the development of this condition.
There was a significant difference in age of the patients (p=0.048) for both prophylaxis agents. This may be because the average age of the ceftriaxone-metronidazole group was 9.76 years old, compared to the 8.14 years for a group of cefotaxime-metronidazole (Table 1). Both therapies showed a higher percentage of male patients. The previous study states that male has a higher prevalence in appendicitis (8.6%) than in female (6.7%) [16]. Patients’ LOS and discharge status percentage are nearly similar for both groups.
This hospital does not have official guideline for antimicrobial prophylaxis. Therefore, the physicians used many antibiotics (single or combination) as prophylaxis following a postoperative appendectomy based on literatures and experience. For instance, cefotaxime, ceftriaxone, gentamycin, cefotaxime-metronidazole-ceftazidime, cefotaxime-metronidazole-ampicillin, cefotaxime-erythromycin-ampicillin, cefo taxime-metronidazole and ceftriaxone-metronidazole. However, the most commonly prescribed antibiotic combination for pediatric patients with perforated appendicitis are cefotaxime-metronidazole and ceftriaxone-metronidazole. In this study, other prophylactic antibiotics are excluded since their costs were not comparable because of less prescription. Several RCT studies performed by Andersen [17] and Helmer [18] have evaluated antibiotic prophylaxis for appendicitis. Most commonly used antibiotics were cephalosporins, particularly third-generation cephalosporins, such as cefotaxime and ceftriaxone, which effectively reduce postoperative SSI rates by <5%. However, when cefotaxime or ceftriaxone was combined with metronidazole, the postoperative SSI rates were reduced to 3%. Previous studies also found that these combinations are effective against most aerobic and anaerobic organisms, reduce the rate of sepsis after appendectomy, and are more cost-effective compared with other regimens [8, 19]. A study about interchange program of ceftriaxone/cefotaxime showed that both ceftriaxone and cefotaxime have equal microbiological and clinical efficacy. It was also found that ceftriaxone appeared to be cost-effective alternative to cefotaxime in this hospital. However, despite their efficacy, both of these antibiotics have considerably different pharmacokinetic properties (half-life and elimination routes).
All antibiotics in this investigation were administered intravenously. Prophylaxis antibiotic administration is typically provided no more than 24 h after surgery. However, in cases of poor sanitation and an unsupportive environment, generally, antibiotic administration is prolonged for at least three days or until clinical symptoms abate. This advice is also suggested by previous studies conducted by Bratzler [7] and Solomkin [20].
The doses of antibiotics utilized in the present investigation were based on the clinical guideline of the hospital. Commonly, the antibiotics were given every 12-24 h for 3-5 days. The patient selection was assessed based on the clinical status of the patients (e.g., fever, pain, and infection status) [10, 21]. Generally, patients’ LOS after appendectomy was six days, and patients were sent home with status cure or recovery (Table 1). The cure status means that the patient can fully go home and there are no problems with their clinical status. Conversely, patients with a recovery status suggest that they can go home but should be followed-up after a few days or a week to make sure their medications are well tolerated.
In Table 1, both LOS and discharge status were not significantly correlated (p>0.05) with the preference of therapy. This suggests that the combination of ceftriaxone-metronidazole and cefotaxime-metronidazole is just as effective at preventing infection after an appendectomy, at least in pediatric patients. A previous study conducted by Daskalakis [8] showed similar findings. Both combinations showed similar strength and had the lowest wound infection rate, thereby further substantiating their recommendations in pediatric patients.
A multivariate analysis was conducted to investigate which independent variables have a significant correlation with the prophylaxis outcome. Type of prophylaxis, age, and gender as the predictors while discharge status (cure or recovery) as the response (Table 2). It can be seen that age has the highest OR (2.625), although not statistically significant (p=0.099). These results have similar findings with the previous study conducted by Singh [22], it stated that in general, the significant factors that affect the recovery process in bacterial infection especially pediatric patients are nutritional status and body weight.
As a type of prophylaxis, we want to investigate which combination shows a better cure rate for the patients. Therefore, in the multivariate analysis, combination ceftriaxone-metronidazole is placed as the baseline and cefotaxime-metronidazole as the comparator. The results showed that there was no significant association between type of prophylaxis towards the patient’ cure rate, thus, it can be seen that both combinations have similar strengths in clinical aspects (OR 1.242 (95%CI 0.398-3.871). However, some previous studies recommend using a combination of ceftriaxone-metronidazole as surgical prophylaxis and treatment for infections because of its effectivity in reducing the risk of postoperative anaerobic infection and good clinical results [23, 24].
Regarding the cost analysis assessment, only a direct medical cost assessment related to the appendectomy protocol of the hospital was utilized. In 2011-2013, the NHI was not conducted comprehensively in Indonesia, so that most of the patients used the out-of-pocket system for their hospital bills. Therefore, we used the hospital perspective to standardize all of the costs in this study.
The highest cost was on medical or surgical supplies, which accounted for 55% of the total cost for appendectomy treatment in both groups (Table 3). The antibiotic cost of the cefotaxime-metronidazole group was slightly more (USD 0.33) than the ceftriaxone-metronidazole group, although the unit cost of ceftriaxone was more expensive than cefotaxime. The higher cost may be because the administration of cefotaxime was throughout 12 h, two times a day, whereas ceftriaxone was given every 24 h or once daily. This has similar results with a previous study conducted by Minotolo [25] and Aiello [26] showing that an appendectomy, in order, the highest cost for an appendectomy is for surgery, antibiotics, and laboratory test.
The cost and effectiveness ratio was conducted using an average of the direct medical cost with LOS and discharge status as the outcome (Table 4). From this study, it can be concluded that there is no difference in effectiveness for both combinations. Both groups showed the same effectiveness and the same cost. To reduce the one day of hospitalization after an appendectomy, USD 1.88 is needed if we use a combination of ceftriaxone-metronidazole as a postoperative antibiotic after an appendectomy. Otherwise, a combination of cefotaxime-metronidazole at the cost of USD 2.28 is suggested to reduce one day of hospitalization. On the other hand, it can be said that to increase one percent cure rate, we have to spend USD 19.70 and USD 24.89 for ceftriaxone-metronidazole and cefotaxime-metronidazole, respectively. These results suggest that a combination of ceftriaxone-metronidazole is more efficient than cefotaxime-metronidazole.
Regarding total cost (Table 3), there was a difference in the treatment cost of USD 4.06 but it was not significant. It means that the saving for postoperative treatment after appendectomy was approximately USD 4.06 by using combination ceftriaxone-metronidazole as prophylaxis after an appendectomy. Furthermore, since it is no cost-effectiveness study, the incremental cost-effectiveness ratio was not performed because both of the combinations have the same cost and effectiveness. A previous study shows that the same generation of antibiotics is not significantly different [19].
Although in this study, we have verified all the data from the clinicians, nurses and pharmacists to avoid missing data related to side effects and patients’ medical histories, our study has limitations. These include the limitations to collect patient's data on clinical outcomes for cost analysis, such as time taken for symptoms, the incidence of generalized peritonitis, the incidence of hypotension, the incidence of fever, admission to high-dependency or critical care unit, and comorbid illnesses. Furthermore, other patient outcomes should be considered, such as blood tests, the rate of infections following surgery, and several other clinical parameters.
| Type of Costs |
Combination Ceftriaxone-Metronidazole (SD) (n=34) |
Combination Cefotaxime-Metronidazole (SD) (n=28) |
p-value | 95% CI |
| Cost of antibiotics | 35.80 (10.7) | 36.14 (19.3) | 0.467 | -0.33 (-8.07-7.42) |
| Cost of medical or surgical supplies | 212.94 (19.3) | 211.26 (22.1) | 0.375 | 1.68 (-8.83-12.02) |
| Cost of Laboratory Test | 66.92 (27) | 75.74 (22.9) | 0.088 | -8.82 (-21.71-4.07) |
| Cost of Hospitalization | 76 (19.9) | 74.75 (18.5) | 0.400 | 1.25 (-8.59-11.09) |
| Total cost | 393.83 (48.6) | 397.89 (57.9) | 0.383 | -4.06 (-31.12-23.0) |
| Variable |
Combination Ceftriaxone-Metronidazole (SD) (n=34) |
Combination Cefotaxime-Metronidazole (SD) (n=28) |
| Average total cost (USD) | 11.58 | 14.21 |
| The average length of stay (days) | 6.15 | 6.21 |
| Cure rate (%) | 58.8 | 57.1 |
| Cost/LOS (USD/day) | 1.88 | 2.28 |
| Cost/cure rate (USD/cure rate) | 19.70 | 24.89 |
CONCLUSION
Both antibiotic therapies studied herein showed the same cost and effectiveness and prophylactic capabilities, but the cost of ceftriaxone-metronidazole may be lower in certain circumstances.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Health Research Ethics Committee of Dr. Hasan Sadikin General Hospitals, Indonesia with ethical approval number: LB.02.01/C02/14920/XII/2013.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
REFERENCES
| [1] | Gardikis S, Giatromanolaki A, Kambouri K, Tripsianis G, Sivridis E, Vaos G. Acute appendicitis in preschoolers: A study of two different populations of children. Ital J Pediatr 2011; 37(1): 35. |
| [2] | Indonesian basic health researh Indonesia MoHo, editor Indonesia: Ministry of Health of Indonesia 2013. Available from: https://apps.who.int/iris/bitstream/handle/10665/259685/9789241513340-eng.pdf;jsessionid=1FEED738EE9F75ADB3DCE326B66E5680? sequence=1 |
| [3] | Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993-2008. J Surg Res 2012; 175(2): 185-90. |
| [4] | Ng-Kamstra JS, Arya S, Greenberg SLM, Kotagal M, Arsenault C, Ljungman D. Perioperative mortality rates in low-income and middle-income countries: A systematic review and meta-analysis. BMJ Glob Health 2018; 3(3): e000810-e. |
| [5] | Uribe-Leitz T, Jaramillo J, Maurer L, et al. Variability in mortality following caesarean delivery, appendectomy and groin hernia repair in low-income and middle-income countries: a systematic review and analysis of published data. Lancet Glob Health 2016; 4(3): e165-74. |
| [6] | Sadraei-Moosavi S-M, Nikhbakhsh N, Darzi AA. Postoperative antibiotic therapy after appendectomy in patients with non-perforated appendicitis. Caspian J Intern Med 2017; 8(2): 104-7. |
| [7] | Bratzler DW, Dellinger EP, Olsen KM, et al. American Society of Health-System Pharmacists; Infectious Disease Society of America; Surgical Infection Society; Society for Healthcare Epidemiology of America. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm 2013; 70(3): 195-283. |
| [8] | Daskalakis K, Juhlin C, Påhlman L. The use of pre- or postoperative antibiotics in surgery for appendicitis: a systematic review. Scand J Surg 2014; 103(1): 14-20. |
| [9] | Hughes MJ, Harrison E, Paterson-Brown S. Post-operative antibiotics after appendectomy and post-operative abscess development: a retrospective analysis. Surg Infect (Larchmt) 2013; 14(1): 56-61. |
| [10] | Abdulah R, Kumamba RD, Sinuraya RK, Rahayu C, Barliana MI. Cost Minimization Analysis of the Use of Meropenem and Ceftazidime in Febrile Neutropenia Therapy. Indonesian Journal of Clinical Pharmacy 2016; 5(2): 132-7. |
| [11] | Hopkins JA, Wilson SE, Bobey DG. Adjunctive antimicrobial therapy for complicated appendicitis: bacterial overkill by combination therapy. World J Surg 1994; 18(6): 933-8. |
| [12] | Severens JL, Milne RJ. Discounting health outcomes in economic evaluation: the ongoing debate. Value Health 2004; 7(4): 397-401. |
| [13] | Drake FT, Mottey NE, Farrokhi ET, et al. Time to appendectomy and risk of perforation in acute appendicitis. JAMA Surg 2014; 149(8): 837-44. |
| [14] | Chen C-L, Chao H-C, Kong M-S, Chen S-Y. Risk factors for prolonged hospitalization in pediatric appendicitis patients with medical treatment. Pediatr Neonatol 2017; 58(3): 223-8. |
| [15] | Blanco FC, Sandler AD, Nadler EP. Increased incidence of perforated appendicitis in children with obesity. Clin Pediatr (Phila) 2012; 51(10): 928-32. |
| [16] | Humes DJ, Simpson J. Acute appendicitis. BMJ 2006; 333(7567): 530-4. |
| [17] | For prevention of postoperative infection after appendicectomy. Cochrane Database of Systematic Reviews 2003; (2): CD001439 |
| [18] | Helmer KS, Robinson EK, Lally KP, et al. Standardized patient care guidelines reduce infectious morbidity in appendectomy patients. Am J Surg 2002; 183(6): 608-13. |
| [19] | St Peter SD, Tsao K, Spilde TL, et al. Single daily dosing ceftriaxone and metronidazole vs standard triple antibiotic regimen for perforated appendicitis in children: A prospective randomized trial J Pediatr Surg 2008; 43(6): 981-5. |
| [20] | Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: Guidelines by the surgical infection society and the infectious diseases society of america. Clin Infect Dis 2010; 50(2): 133-64. |
| [21] | Ruterlin V, Sinuraya RK, Halimah E, Barliana MI, Hartini S. Economic Evaluation of the Use of Cefotaxime and Ceftazidime in the Treatment of Pneumonia in Pediatric Patients. Pharmacol CL Pharm Res 2017; 2(1): 17-21. |
| [22] | Singh P, Wadhwa N, Lodha R, Sommerfelt H, Aneja S, Natchu UCM. Predictors of time to recovery in infants with probable serious bacterial infection PLoS One 2015; 10(4): e0124594-. |
| [23] | Löfmark S, Edlund C, Nord CE. Metronidazole is still the drug of choice for treatment of anaerobic infections. Clin Infect Dis 2010; (Supplement_1): S16-23. |
| [24] | Navarro NS Jr, Campos MI, Alvarado R, et al. Oasis II Study Team. Ertapenem versus ceftriaxone and metronidazole as treatment for complicated intra-abdominal infections Int J Surg 2005; 3(1): 25-34. |
| [25] | Minutolo V, Licciardello A, Di Stefano B, Arena M, Arena G, Antonacci V. Outcomes and cost analysis of laparoscopic versus open appendectomy for treatment of acute appendicitis: 4-years experience in a district hospital BMC Surg 2014; 14: 14. |
| [26] | Aiello FA, Gross ER, Krajewski A, et al. Post-appendectomy visits to the emergency department within the global period: a target for cost containment. Am J Surg 2010; 200(3): 357-62. |