All published articles of this journal are available on ScienceDirect.
The Negative Impacts of COVID-19 Containment Measures on South African Families - Overview and Recommendations
Abstract
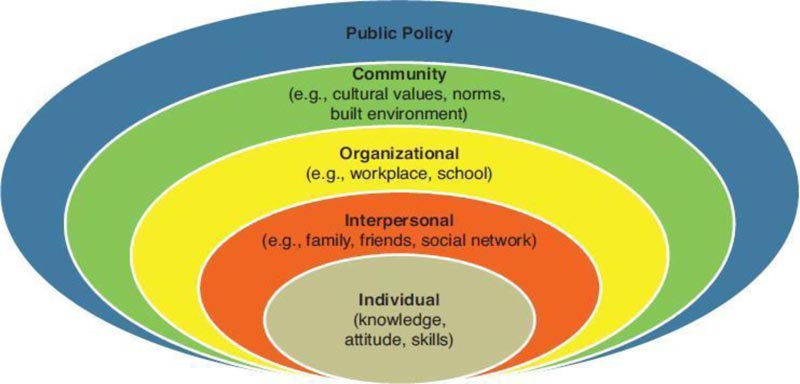
The World Health Organization (WHO) reported various pneumonia cases (‘Coronavirus Disease 2019’ [COVID-19]) on 31 December 2019 in Wuhan City, China, which has spread to many countries, including South Africa. In response to this, the President of South Africa declared a state of national disaster on 15th March 2020, followed by introducing various COVID-19 containment measures to minimize the spread of the virus. This paper examines the negative impacts that COVID-19 containment measures may have had on the family as a unit of society and furthermore provides recommendations to mitigate the impacts of these measures. It can be concluded that COVID-19 containment measures, specifically the lockdown restrictions, would yield both short-term and long-term impacts on proper family functioning. Several families in South Africa have been impacted financially due to the closure of business which led to the temporary/ permanent unemployment of some breadwinners in the families. This also has had a cascading impact on the food security of families and their ability to afford other basic necessities. Distress as a result of financial challenges or failure to provide for the family alongside spending much time locked down together as a family has also led to violence in the family. This was further exacerbated by the fact that the victims were stuck with the abusers and some could not report or find help due to the restricted movements. Furthermore, since most institutions predominantly moved learning online, results indicated that the lockdown restrictions affected the ability of some individuals especially those from poor families to access formal education during the period due to the lack of digital devices and internet facilities. In order to mitigate the impacts of the COVID-19 containment measures on the family, there is a need for collaborative efforts at intrapersonal, interpersonal, institutional, community and policy levels using the ecological framework.
1. INTRODUCTION
On 31st December 2019, the World Health Organization (WHO) reported several pneumonia cases (‘Coronavirus Disease 2019’ [COVID-19]) in Wuhan City, China. Since then, the virus has spread to at least 213 countries and territories, including South Africa [1]. On 5th of March 2020, South Africa recorded its first case of COVID-19 [1] and in less than two weeks, the President declared a state of national disaster to curb the virus. This was later followed by the pronouncement of a series of lockdowns dating from Thursday 26 March, 2020 as part of the effort to fight the outbreak [1]. Measures to contain the virus included but were not limited to the impositions of curfew, closure of schools and businesses, working from home for non-essential workers, restriction on outdoor exercise, large gatherings and inter-province travelling and reduced carrying capacity and operating hours for taxi drivers. Although these measures could not stop the virus, they were significant in slowing down its transmission rate – flatten the curve and allow the preparation of the health system to fight the virus [1].
Though COVID-19 emerged as a health crisis, there is no doubt that it has had a tremendous impact on different aspects of life. This paper discusses the negative theoretical impacts that the COVID-19 containment measure have had and will continue to have on society, particularly the family.
2. THE FAMILY AS A SOCIETAL INDICATOR
The family is a micro-unit of the society. It is a societal group that is not only related by blood, and it equally includes groups related by marriage, civil union, cohabitation and foster care [2]. The family is responsible for maintaining stability in the society through the socialisation function [3] and it is central in the care and well-being of individuals so that they can function properly in society [4, 5]. Therefore, when families are impacted, individuals, as well as societies, are affected. In the case of coronavirus and the containment measures, the negative impacts on the families have been reported to be overwhelming, ranging from short-, to medium- and long-term [6]. The negative impact of coronavirus on one aspect of family life may have a cascade effect. For example, the loss of a job as a result of the lockdown may lead to a situation in which an individual is unable to feed his family (food insecurity), resulting in starvation, malnourishment and nutrient deficiencies [7-10]. As cited by Owusu and Frimpong-Manso [11], many children living in impoverished families depend on the schools for meals provided for them by the Government of Ghana under the school feeding programme. With the lockdown restrictions that they could not get access to these meals. This, coupled with the financial situations of their families, affected their feeding negatively in size, frequency and quality meals taken. The trend in the decreased access to nutrition services for children is similar to those seen during the 2014-16 outbreak of Ebola virus disease in sub-Saharan Africa [12]. On the other hand, the evidence from a study conducted in China indicated that due to economic distress resulting from the lockdown restrictions, violence in the family has increased [13]. This indicates the complexity of the effects of the COVID-19 pandemic on the family.
3. HEALTH IMPACTS AND FAMILY
There are five dimensions of health - physical, mental, social, emotional and spiritual [14]. The restriction placed on outdoor exercise has the potential to affect individuals’ health considering the health benefit of exercise. A few days of inactivity are adequate to induce muscle loss, neuromuscular junction damage and fibre denervation, insulin resistance, decreased aerobic capacity, fat deposition and low-grade systemic inflammation [15, 16].
Also, exercise is a protective factor in many life diseases such as cardiovascular diseases and obesity. There could be an increase in the prevalence of overweight and obesity and their associated consequences, as well as an upsurge in cases of anxiety and depression [17]. Additionally, many family members have become sedentary, working from home and devoting hours to sitting in front of the computer [18-21]. Long hours in front of the computer may lead to a major decline in visual health (visual impairments) and varied adverse health outcomes [18-21]. Furthermore, South Africa has a comparatively high burden of non-communicable diseases with many on chronic medication. Studies have also indicated that about 7% of South African’s GDP was spent in 1995 and currently, the country spends around 89% of its GDP on health [22]. However, there are still apparent challenges and inequalities in terms of affordable health care to all [23, 24]. Unfortunately, measures such as restrictions on movement reduced carrying capacity and operating hours for taxi drivers further hampered patients from collecting medications from the clinic. This consequently may promote non-adherence and affect treatment outcomes.
Age is a crucial risk factor in terms of COVID-19 mortality, as such, it is expected that countries and communities with an increasingly younger generation, would possibly have less mortality than communities that have more of the older age group [25]. It has been suggested that younger populations such as Africa and South Asia may have a reduced mortality rate from the COVID-19 pandemic compared to developed countries like the UK and Italy that have experienced overwhelming deaths among the older generation [25]. Contrariwise, data from the UK has portrayed an increase of COVID-19 deaths among the younger age groups and particularly in black communities [26]. South African data, in particular, suggests that 66% of the first 752 COVID-19 deaths were less than 65 years of age, whilst people between the ages of 40 and 65 years of age were associated with 58% of deaths [27].
4. COVID-19 CONTAINMENT MEASURES AND VIOLENCE IN THE FAMILY
In times of disasters, evidence has shown that violence against women increases [28]. The measures to reduce the transmission of the COVID-19 pandemic have resulted in most people spending most of their time at home with their families, disrupted social and protective networks, reduced access to services and increased stress mainly for breadwinners due to their inability to work and provide for their families. This exacerbates the risk of violence against women and children. According to Taub [29], the pandemic has provided conditions for Sexual and Gender-Based Violence (SGBV) to flourish. The reality is that the pandemic has left many victims of domestic violence trapped with their abusive partners or parents and isolated from people and resources that could provide a means of help or escape.
Evidence from other countries suggests an increase in domestic violence cases since the outbreak of the COVID-19 pandemic [28]. Data from South Africa has shown an increase in the cases linked to domestic violence within the family during the lockdown [30-33]. During the first three weeks after the lockdown started, the Government GBV and femicide centre alone recorded more than 120 000 victims of GBV, which was double the usual number before lockdown [34, 35]. In Tshwane, a city in the Gauteng Province of South Africa alone, the call centre was receiving 500-1000 calls a day and Vodacom’s call centres saw a 65% increase in calls from women confined in their homes and seeking help [35]. The country has become accustomed to the news on the upsurge in incidents of domestic SGBV, including femicide during the lock-down period. Furthermore, the pandemic worsened home-based violence against children since they could not access schools, which are a form of support and protection for many [36].
5. ECONOMIC AND FINANCIAL IMPACTS ON FAMILIES
The COVID-19 restrictions have led to the closure or downsizing of some businesses, which has left millions of people without jobs. Many people work in the informal economy, where they survive from hand to mouth. The lockdown meant many people could not engage in their daily survival strategies. To ease the impact of the lockdown measures on the economic wellbeing of individuals and families, different governments introduced relief measures.
South Africa introduced the UIF (Unemployment Insurance Fund) to help cope with the effects of this pandemic [37]. However, some individuals could not benefit from this fund as a result of not meeting the criteria or their employer not submitting the required documents or lodging the claims [38]. Furthermore, some breadwinners in the families are employed in precarious situations where they have no access to social grants or relief measures. With reduced or no income, it means families will not be able to afford the basic necessities including food.
6. EDUCATIONAL IMPACTS ON FAMILIES
Early learning and play formed part of early childhood development. Research has shown that a child with early and proper physical, social, emotional, language and cognitive development has better health and educational outcomes in childhood and employment outcomes in adulthood [39]. The school closure has negatively impacted learners and their families in several ways. Due to the closure, learners, especially young learners can no longer learn and play. Many South African families live in environments that are not conducive to learning – connectivity problems, limited data access, power blackouts, small space and lack of learning facilities [40]. Although some of the schools have started online and remote learning, many South African families cannot afford the equipment that is needed for effective online learning [41, 42]. For the schools that have resumed teaching; only a few selected grades were asked to return, and many of the learners and teachers have to go to school in fear as some of their colleagues had tested positive to COVID-19 [43].
7. RECOMMENDATIONS
We proffer recommendations that might help reduce the negative impacts of the COVID-19 containment measures using the ecological framework - a theory-based framework for understanding the multifaceted and interactive effects of personal (family) and its environment [44]. The framework consists of the intrapersonal/individual, interpersonal, institutional, community and policy levels as depicted in Fig. (1).
8. INTRAPERSONAL AND INTERPERSONAL LEVELS
Herein, we recommend:
- Indigent families can be assisted with equipment that is essential for effective homeschooling, for example, televisions and radios (this has also been recommended in a rapid review on how to mitigate the impacts of physical distancing in Africa [45]). This can be done through the cooperation of both Government and private organisations as part of their corporate social responsibility. According to UNESCO, a collaboration between different actors was the main factor of success in implementing radio and television based educational programs in Lithuania, Georgia and Australia during the COVID-19 pandemic [46].
- Individuals should be encouraged to engage in indoor exercises that are age and health fitness appropriate. These may include yoga, dancing, barre, High-Intensity Interval Training (HIIT), using weight plates, planking, couch workouts, squats, lunges, kickboxing workouts and walking up and down a staircase. Physical activities have been reported to be beneficial in ameliorating respiratory difficulties and preventing weight gain, depression and psychological distress [17].
9. INSTITUTIONAL LEVEL
Herein, we recommend that:
- Schools should also use cheaper platforms such as the radio to educate learners so that learners in poor communities with limited connectivity and technological resources can benefit. This has been recommended in a previous review [45]. The Government should assist in supplying radios and batteries to cater to learners who cannot afford other technologies for online learning as evidence from the Ebola pandemic showed that some learners did not have access to radios or batteries [47].
- The use of telemedicine can be promoted where possible to increase access to medical consultation and treatment during this period to patients that may be afraid to visit the clinic. Telemedicine can be used to maintain social distancing during COVID-19 and other pandemics [48, 49]. There is evidence of the successful use of telemedicine during global emergencies, for example, the SARS epidemic in 2003 in China [49].
- There should be increased efforts by government officials, majors, judges and other officials in responding to and combating domestic violence as well as providing a safe outlet for victims to report abuse [50]. Programmes on various platforms showing campaigns against domestic violence should also be aired. National free toll numbers should be provided so that victims can call for help [51].
- Banks in collaboration with the government should provide loan payment relief for medium and small-scale businesses to prevent more businesses from closing down – thereby preventing job loss. Lessons can be learned from Switzerland which was accredited for successfully avoiding income losses by workers and damage to the economy by supporting independent workers and small business owners through wage compensations, income support and loans [52].
10. COMMUNITY LEVEL
At this level, we recommend that:
- Medication collection points can be open in areas close to people or home deliveries of medicine can be encouraged so that those on chronic medication easily access their drugs to promote adherence [53]. Community workers can be utilised to spread information about these collection points and other health related information as well as assist in the distribution of drugs in the community [45].
- A conducive shelter should be provided to accommodate victims of gender-based violence as many of them are living with their perpetrators. This could be achieved through the support of all stakeholders (individual, community, civil society and government). Shelters should be opened as priority services, raising awareness on the existence of such shelters and toll-free numbers for victims to report abuse and seek assistance should be prioritised. Safe spaces can be established for girls and women to be protected, for example, in the context of Ebola, countries such as Sierra Leone established safe spaces where girls could go during school closure, and this was successful in minimising adverse outcomes for girls [54]. Furthermore, Campbel [36] suggests that many postal workers, garbage collectors, food delivery workers, and public works; officials who have access to the community during the pandemic should take part in identifying violence in the homes and reporting it to the relevant authorities.
- Parents and teachers should be trained on how best to assist learners as online learning may be new to them. Teachers should be asked to register for courses on online teaching as part of continuing professional development (CPD). Also, online workshops can be organised to teach teachers about online teaching [55]. The community forum in the community can be used as an avenue to teach parents about online learning.
11. POLICY LEVEL
- The government should enact and amend laws and policies that will facilitate the implementation of interventions to mitigate the negative impacts of COVID-19 containment measures on the family. For example, policies such as reducing or removing administrative barriers that could be seen as unnecessarily burdensome or needless will expedite the implementation of the much-needed interventions. This step has been seen to be effective in [56].
- There is a need for the development of policy measures to properly monitor COVID-19 relief interventions (such as unemployment grants and food packages) so that they can reach those in need [57].
AUTHORS' CONTRIBUTIONS
All authors contributed equally to this work.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGMENTS
Declared none.


