All published articles of this journal are available on ScienceDirect.
Community-Based Screening for Cardiovascular Disease in the Capricorn District of Limpopo Province, South Africa
Abstract
Background:
The number of people who suffer and die from Cardiovascular Disease (CVD) is increasing at an alarming rate in low-and middle-income countries.
Objective:
The objective of the study was to screen communities using the non-laboratory INTERHEART Risk Score tool (NLIRS) to determine their level of risk for developing CVD.
Methods:
A community-based quantitative study was conducted in the Capricorn District of Limpopo Province. A total of 3315 participants were screened by 63 community health workers (CHWs) using the NLIRS tool. The tool covers the following items which are allocated different scores: Gender:male ≥55 years or female ≥65years=2; being a smoker or having stopped ≤12 months ago = 2; smoking1-5 cigarettes =2; 6-10=4; 11-15=6;16-20 a day and ≥20=11; indirect smoking last 12 months =2; having diabetes=6 and high blood pressure=5; parental history of heart attack=4; having stress and depression=3 each; consumption of salty and fried food, no vegetables or fruits each scored a 1; eating meat twice a day =2; being inactive =2; waist-to-hip ratio ≥.874-0.963=2 and ≥0.964=4. The scores were added and those who scored 0-9 were classified to be at low risk, 10-15 moderate and 16-48 at high risk.
Results:
On average 58% and 33% were found to be at low and moderate risk, respectively for developing CVD and 9% at high risk. The majority consumed salty, fried foods and meat and were inactive. Being hypertensive constituted 67% of being at high risk of developing CVD.
Conclusion:
Envisaged intervention will focus on preventive strategies for risk factors such as diet, exercise and hypertension. More males should be recruited to participate in future research to determine if the same results will be obtained.
1. INTRODUCTION
The World Health Organisation estimated that CVD contributed to 17.5 million deaths worldwide in 2012 with a third of those attributed to CVD [1]. In 2016 the number of CVD deaths increased to 17.9 million, which represented 31% of all global deaths [2]. It is projected that worldwide 24 million people will die from CVD by 2030 [3]. Seventy-five percent (75%) of these people stay in low- and middle-income countries [2, 4]. These estimates suggest that developed countries are experiencing a decline in CVD despite an increase in ageing population which is prone of CVD [5-7]. Another reason for the decline of CVD in developed countries may be due to the improvement in the management of their healthcare systems [5]. On the other hand, the expected increase of CVD in low and middle-income countries is attributed to rapid urbanisation and industrialisation [5, 8].
A report released by the WHO in 2017 indicates that CVD is now the second common cause of death after infectious diseases in Africa [2]. In South Africa, CVD is the second leading cause of death after HIV/AIDS [9] with about 210 people estimated to be dying from CVD every day [10]. It is estimated that the rate of premature death as a result of CVD amongst South African adults is projected to increase by 41% between 2000 and 2030 [11].
It is of concern that people who die from CVD lack awareness regarding the risk factors associated with CVD. Empirical studies have found that major risk factors associated with CVD include high blood pressure (hypertension), smoking, poor eating habits, unhealthy diet, obesity and lack of physical activity [10, 1, 12].
Studies conducted in South Africa by Nojilana et al. and Schutte [13, 14] recommended the prioritisation of the management of CVD in the same way as the aggressive approaches that are needed for the management of Non-Communicable Diseases (NCDs). Amongst strategies recommended for CVD prevention are health promotion and a change of lifestyle [15-17]. Training of nurses on CVD management has also been recommended [13, 14]. Studies show that CVD is preventable through health promotion and a change of lifestyle [15-17]. Epidemiological profiling of communities regarding their level of risk for developing cardiovascular disease, followed by appropriate interventions, may assist in reducing CVD prevalence [18, 19]. In line with the above recommendations, this study aimed to screen semi-urban and rural communities using the non-laboratory INTERHEART Risk Score tool (NLIRS). The results of the study will be used to develop relevant and suitable intervention strategies. This study is part of the bigger intervention study titled: “Scaling-up packages of intervention for cardiovascular disease prevention in selected sites in Europe and Sub-Saharan Africa” (SPICES).
2. MATERIALS AND METHODS
2.1. Study Design
A quantitative research approach applying the household-based cross-sectional descriptive design was used to conduct this study. Once-off data collection was done from the participants, using the NLIRS tool at their homes.
2.2. Study Setting
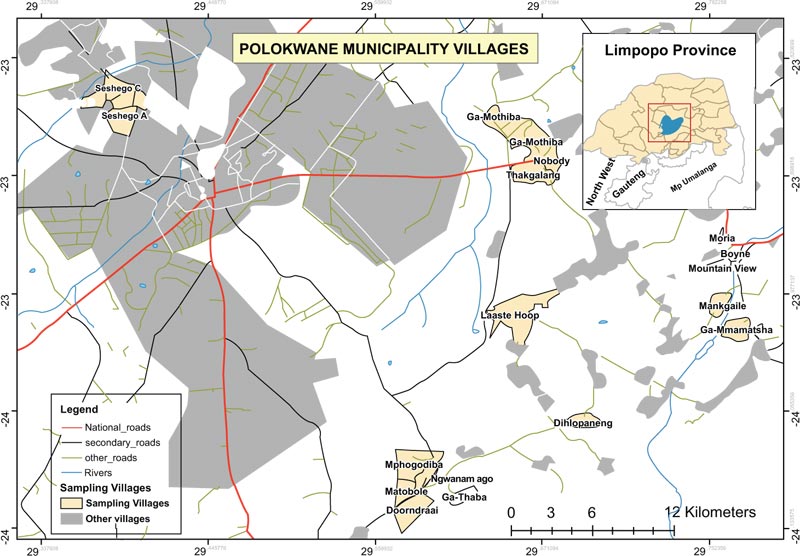
The study was conducted in two study sites of the Polokwane Municipality in Limpopo province, Capricorn district namely, Seshego semi-urban township located in the west and Ga-Molepo villages located in the eastern part of Polokwane city. The semi-urban township was serviced by 4 public Primary Health Care (PHC) clinics whereas, the rural villages were serviced by 7 public PHC clinics. The two sites were selected based on the findings and recommendations of research studies that reported a high prevalence of chronic diseases and an increase in the risk factors associated with the development of CVD [20-25]. These previous studies also recommended the development and implementation of health interventions to control the risk factors associated with NCDs and CVD (Fig. 1) [15-24].
2.3. Population and Sampling
The total number of households was 3,930 for Seshego semi-urban township and 11,854 for Ga-Molepo rural villages. Yamane’s mathematical formula with an error of 5% and a confidence coefficient of 95% [26] was used to obtain a sample size for the selected sites (Seshego and Ga-Molepo) of 1,111 and 2,082 households, respectively. Furthermore, to obtain the exact number of the sample as proposed by Yamane’s mathematical formula [26] per village, proportional sampling was used where the researchers divided the population sample size per site into sub-villages and then applied proportionalsampling techniques to each sub-population. The total number of participants screened on both sites was 3315 (1390 Seshego and 1925 Ga-Molepo)due to their availability and willingness to participate in the study at the time of data collection.
2.4. Ethical Considerations
In preparation for data collection, ethical clearance was obtained from the University of Limpopo Turfloop Research and Ethics Committee (TREC/381/2017). Permission to conduct the study was obtained from the Limpopo Department of Health Research Committee. All the screened participants were briefed by trained CHWs about the data collection procedure before consenting to participate. Participants were further informed that their participation in the study was voluntary and that they were free to withdraw from the study at any time. A consent form was signed by those who agreed to participate in the study. Anonymity was ensured and all data was kept secure. No animals or plants were used in this study.
2.5. Data Collection
Data were collected over 8 months from June 2018 to January 2019 by 63 trained CHWs attached to the 11 clinics, 14 CHWs were from Seshego semi-urban township, whereas 49 were from Ga-Moleporural villages. The 63 CHWs were selected from a total of 143 CHWs due to their level of education. On average, each CHW was allocated between 280 and 242 households, which are under his/her care at the clinic in Seshego and Ga-Molepo, respectively. The CHWs are also well known to the communities because they reside in those areas. Each community health worker screened all members of a household who were at home on the day the data were collected, from 18 years and above, using the non-laboratory INTERHEART Risk Score tool.
2.5.1. The Interheart Risk Score Tool
The NLIRS tool covered the following items and was each allocated a score: Being male ≥55 years and female ≥65years=2; being a smoker or having stopped 12 months ago orless= 2; smoking 1-5 cigarettes=2; 6-10=4; 11-15 cigarettes=6;16-20 and 20+ per day=11; inhaling smoke from other people in the last 12 months =2; having diabetes=6and high blood pressure=5; a parental history of heart attack=4; psychological factors: experience of several periods of permanent work or home life stress in the past year and feeling depressed for two weeks or more in a row in the past 12 months=3 each; diet: consumption of: salty food or snacks one or more times a day and deep fried foods, snacks or fast foods 3 or more times a week=1 each, no vegetables or fruits a day=1, eating chicken or red meat twice a day=2; inactive or performing mild physical exercise during leisure=2; and measurement of waist-to-hip ratio (WHR) ≥.874-0.963=2 and ≥0.964=4 [26, 27]. At the end, the scores were added and those who scored 0-9 were deemed to be at low risk, 10-15 were at moderate risk and 16-48 were at high risk. The English version of the NLIRS tool was translated by a language expert to Northern Sotho after conducting the pilot study. Northern Sotho is an indigenous language spoken by the majority of respondents in the Capricorn district of Limpopo Province [28]. The NLIRS tool was chosen because it can be used in settings with limited resources [19, 29].
2.5.2. Measurements
The waist-to-height ratio circumference was measured using a tape measure. The waist circumference was measured at the approximate midpoint between the lower margin of the last palpable rib and the top of the iliac crest and the hip circumference was measured around the widest portion of the buttocks [30]. The blood pressure (BP) of those who did not know if they were hypertensive, was measured on the left arm using the MEDIC Pharmacists Choice Devices Blood Pressure Monitor Classic (MPCDBPMC). TheBP Monitor used has been clinically validated according to the European Society of Hypertension (ESH) protocol [31]. Being hypertensive included those who answered yes when asked if they had high blood pressure and those who did not know that they are hypertensive, but were found to have a systolic BP score of
2.5.3. Validity and Reliability
To ensure validity and reliability, the CHWs were first trained by the research team on risk factors associated with CVD, prevention of CVD and how to screen the participants using the NLIRS tool for a week followed by a one-day refresher course before commencing with the pilot study. Training of the CHWs at their respective clinics continued after the pilot study. The NLIRS tool has been validated by 52 countries [25-27]. The CHWs were supervised by registered nurses and the research team during data collection.
2.6. Statistical Analysis
The participants who scored
3. RESULTS
The risk levels of developing CVD per residential site are presented in Table 1 below. Of the 3 315 participants who were screened, 1 390 were from Seshego and 1 925 from Ga-Molepo. On average 58% were at low and 9% at high risk.Whereas 33% were at moderate risk of developing CVD for both sites. Using a t-test it was found that there were no statistical differences between the risk score mean of the two sites. The number of female participants was almost triple that of males (females 75% vs 25%).
The mean NLIRS for the males was higher as compared to that of the females (10.59 vs 9.10, p< 0.001) (Table 2). Eighty-nine percent (89%) of the participants were non-smokers, with the majority (75%) consuming salty food/snacks (
The differences between gender with behavioural, biological, dietary and physical factors are also presented. The mean age of men and women was 49.34 and 48.79 years, respectively, with no major gender differences. There is a statistical difference between the numbers of the inactive participants/ those who performed mild exercises in the women sample as compared to the men sample (p < 0.001) with a higher number of women being inactive or performing mild exercises. There was no statistical difference in gender (p>0.05) regarding other factors, such as being diabetic and stressed, low fruit and vegetable intake, consumption of salty/deep-fried foods and red /poultry meat twice per day. Males exhibited an elevated ≥0.964 WHR as compared to females [64 males vs. 36, p < 0.001].
| - | Total | Low | Moderate | High | P-value |
|---|---|---|---|---|---|
| Seshego | n (%) | n (%) | n (%) | n (%) | 0.077 |
| Female | 1035 (75) | 646 (78,30) | 317 (69,82) | 72 (64,86) | |
| Male | 355 (25) | 179 (21,70) | 137 (30,18) | 39 (35,14) | |
| Total | - | 825 (59) | 454 (33) | 111 (8) | |
| Ga-Molepo | - | - | - | - | |
| Female | 1440 (75) | 872 (79,34) | 448 (71,34) | 120 (60,61) | |
| Male | 485 (25) | 227 (20,66) | 180 (28,66) | 78 (39,39) | |
| Total | - | 1099 (57) | 628 (33) | 198 (10) | - |
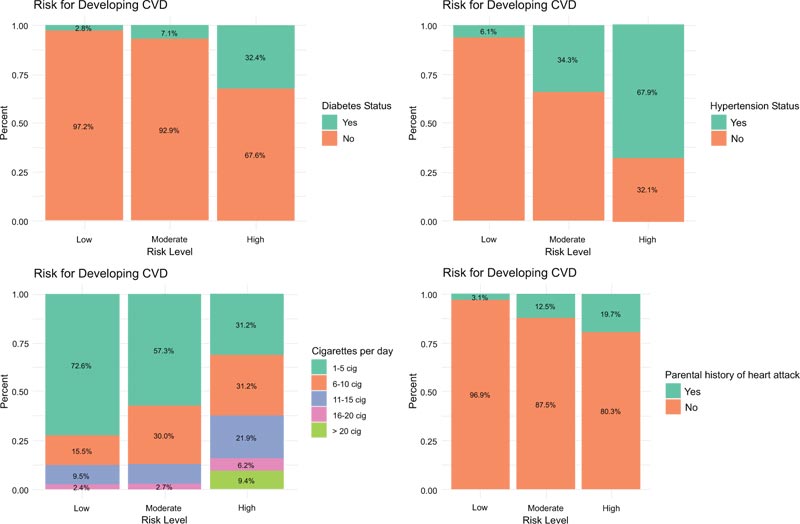
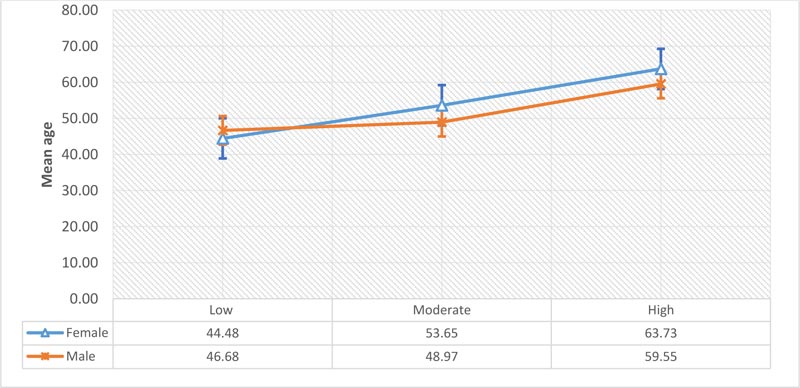
Fig. (2) illustrates the percentage distribution by diabetes, hypertension, number of cigarettes and parental history of heart attack among all the categories of risk levels. It can be seen from the plot that participants who reported being hypertensive hold a high proportion (67.9%) of being at a high-risk level of developing CVD. The proportion of being diabetic, having a parent who has a history of heart disease, smoking more than 6 cigarettes per day increases as you move from low to moderate, to high risk. Only the high-risk level had participants that smoked more than 20 cigarettes per day. The mean age for both genders increased as you moved from low to high risk (Fig. 3) suggesting that the level of risk for developing CVD increases with age for both males and females. More females were at moderate and high risk for developing CVD than males.
4. DISCUSSION
The study aimed to screen communities for their level of risk for developing CVD using the NLIRS tool. The results from the study showed that ageing for both males and females could increase a person's risk of developing CVD. This was not surprising, because age is a well-known independent risk factor for developing CVD [33]. However, the lowering of blood pressure, cholesterol, blood glucose, smoking abstinence, being female and having a higher education increased the survival rate up to the age of 85 years [34].
The number of females screened was almost triple that of males in this study. The reason for the high number of females as compared to males in this study could be attributed to the fact that most men were not at home at the time of screening, as they could probably have been at work [35].
There was a higher number of hypertensive females compared to males in this study. This differs from other findings, where there were more males with hypertension as compared to females [36-39]. Studies that have investigated gender differences in hypertension reported that the reason why there were more men than women with hypertension is that women are protected by biological factors such as the sex hormones oestrogen and progesterone before they reach menopause [40, 41] and chromosomes [42-44]. These biological factors become evident during adolescence and persist through adulthood and disappear when women reach menopause and at that point, the differences in hypertension become smaller or non-existent [40, 41, 45-47].
More males in this study had a WHR of
In this study, more females were consuming more red meat/poultry ≥2 times/day than males. A study conducted amongst college students found that males consumed more red meat than females [58]. Consumption of red meat is a risk factor for developing CVD, type 2 diabetes and colon cancer [59-63]. But consumption of more than one portion per day and regular consumption of processed meat rather than fresh red meat put people at greater risk of developing type 2 diabetes, coronary heart diseases and CVD [64].
More females perform mild exercises than males, who tend to lead a sedentary life. In most cases, women do not have the time to exercise because of the housework, taking care of children, care for the elderly or disabled family members [65]. In some places, there are no sidewalks and women are an easy target for criminals so they are afraid to go to parks.
The majority, 89%, of the participants in this study were non-smokers. The prevalence of smoking in South Africa based on the national survey conducted in 2012 was 17.6% [66]. However, the participants who smoked 20 and more cigarette per day in this study were all found to be at high risk of developing CVD. Cigarette smoking is a major risk factor for the development of CVD [67, 68]. Many researchers reported that cigarette smoking poses a double risk of developing CVD, including cerebrovascular diseases and heart failure, irrespective of the number of cigarettes smoked a day [69-74].
Most participants who were hypertensive were classified to be at high risk of developing CVD. Hypertension has been reported by many researchers as the strongest risk factor for developing almost all different cardiovascular heart diseases, cardiac arrhythmias, including arterial fibrillation, cerebral stroke and renal failure [75-80].
CONCLUSION
Communities were successfully screened to determine their level of risk for developing CVD by trained CHWs. Those at high risk for developing CVD were referred for further management to their respective Primary Health Care clinics. Those who were found to be at moderate risk will be enrolled in an intervention programme focusing on the prevention of hypertension, reduction in the consumption of salty foods/snacks, deep-fried foods/fast foods and red meat/poultry applying self-management strategies. More than half of the participants who reported being mainly inactive, or performing mild exercises, will be advised/taught individual exercises at their homes or group exercises at their respective Primary Health Care clinics and those who can afford to will be advised to enrol at the available Gyms in their communities. Ageing was also found to be a contributing risk factor for developing CVD. Rolling-out of intervention programmes at schools will be beneficial. Very few males participated in the study as compared to females. More males should be recruited to participate in future research studies to determine if the same results will be obtained.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical clearance was obtained from the University of Limpopo Turfloop Research and Ethics Committee, South Africa (TREC/381/2017).
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all the participants.
AVAILABILITY OF DATA AND MATERIALS
Derived data supporting the findings of this study are available from the corresponding author [R.N] on request.
FUNDING
This research is funded by the European Commission through the Horizon 2020 Research and Innovation Action Grant Agreement No. 733356.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGMENTS
The authors would like to thank all the participants, CHWs, professional nurses at the clinics, members of the SPICES research, the University of Limpopo and the Limpopo Provincial Department of Health. Lastly, to thank the European Commission for funding this project.


