All published articles of this journal are available on ScienceDirect.
Post-Coronavirus Era: Should We Expect a Surge in Allergic Diseases and Asthma?
Abstract
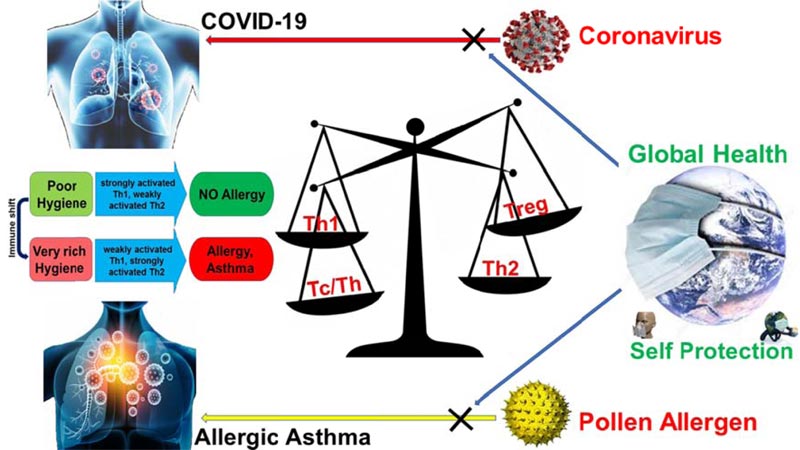
Some infectious agents by priming the immune system promote protection against allergy and asthma. During infections, Th1 immune responses are dominant, while in allergic conditions, Th2 responses are more pronounced. Th1 immune response protects the body against infections, and Th2 response leads to allergy and asthma. For maintaining health, the balance between Th1 and Th2 responses is necessary. The COVID-19 infection augments Th1 and also eosinophilic responses. On the other hand, the main protocols to control the COVID-19 pandemic require adherence to health standards, maintaining personal hygiene, frequent disinfecting of hands, using face masks, etc. In the post-COVID-19 era, this sterile condition may relinquish, and the Th1/Th2 immune imbalance may lead to an increase in the incidence of allergy and asthma. Therefore, focus on the COVID-19 infection should not deter us from foreseeing a surge in asthma and other post-coronavirus problems.
According to the “hygiene hypothesis” and lifestyle changes, infectious diseases have decreased with an increase in the incidence of allergic and autoimmune diseases in industrialized countries. Some infectious agents prime the immune system, protecting against allergy and asthma. Over the last 10 years in industrialized countries, allergic diseases and asthma have turned into epidemics. The decreased rate of infections in the countries have been followed by a surge in the prevalence of allergic diseases, but when people are chronically infected, the prevalence of allergic diseases remains low. During infections, Th1 immune responses are dominant, while in allergic conditions, Th2 immune responses are accentuated. Th1 lymphocytes produce inflammatory cytokines such as IL-2, IFN-γ, IL-12, and TNF-α that are involved in cell-mediated immunity. In contrast, Th2 lymphocytes produce IL-4, IL-5, and IL-13 that contribute to IgE production and allergic responses. So, Th1 protects against infections, and Th2 responses lead to allergy and asthma [1, 2]. For maintaining one’s health and normal immune function, the balance between Th1 and Th2 lymphocytes (and other T cell subsets) is necessary (Fig. 1).
The global community is facing the major crisis of the “COVID-19 pandemic” as the virus, SAR-Cov-2, shows resistance to many therapeutic protocols, with no vaccines applicable on the horizon. The main protocols to control the pandemic include implementing health standards, personal hygiene, disinfecting hands and the living environment, using face masks, etc. Many scientists are currently trying to develop applicable vaccines and treatments for the disease. In the post-COVID-19 era, this sterile condition may lead to a surge in the incidence and prevalence of allergy and asthma [3-5]. Although research evidence does not support asthma as a major COVID-19 risk factor, it is important to consider the underlying hidden causes of asthma amid the pandemic [6]. Depending on the infectious agent (SARS-CoV-2), Th0 cells are polarized towards Th1 response in immunocompetent subjects. Also, eosinophils play a direct role in fighting against RNA viruses (such as the causative agent of COVID-19) [7]. The immune system at the post-COVID-19 period may rearrange itself, which may lead to hypersensitivity. These changes play a fundamental role in reducing COVID-19 severity through alleviating inflammation. Nevertheless, susceptibility to allergies and a possible increase in the incidence and prevalence of asthma need to be validated in future studies [8]. Because of the dysregulated Th1/Th2 balance, after recovery from the COVID-19 pandemic, the epidemics of allergies and asthma may be initiated in many parts of the world due to a decrease in the burden of infectious diseases during the pandemic (Fig. 1).
In a study from January 1st to May 10th, 2020, clinical data analysis showed that out of 71,182 asthmatic patients, 1,006 (1.41%) suffered from COVID-19. Asthmatic patients with COVID-19 were older (55 vs. 42 years) and predominantly female (66 vs. 59%), smoked more frequently, and showed a higher prevalence of hypertension, diabetes, dyslipidemias, and obesity [9]. Confusing data exist regarding asthma and COVID-19 comorbidity. There has been a higher frequency of asthma among COVID-19 patients compared to the general population (2.9 vs. 1.6-2.2%), as well as a higher frequency of COVID-19 infection amongst asthma patients compared to the general population (1.41 vs. 0.86%). In addition, the possibility of contracting COVID-19 is higher in asthma patients than in the general population [10]. On the other hand, numerous patients with asthma are infected with the SARS-CoV-2 virus. Although data is limited, patients with severe asthma seem to have an exaggerated risk of a more severe course of the COVID-19 infection [4]. Uncontrolled severe asthma is a substantial risk factor of developing severe COVID-19 [11]. Angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine 2 (TMPRSS2) are the SARS-Cov2 receptors highly expressed in patients with asthma [12]. Asthma can be harnessed by ACE inhibitors, including lisinopril and enalapril, but patients with asthma must remain alert during the COVID-19 pandemic [13]. Depending on Th response polarization, the role of eosinophils in fighting against the COVID-19 infection is yet to be studied. Also, the interaction between ACE2 and SARS-Cov2 in asthmatic lungs may influence lung immunopathology and shift the immune response towards Th2 response. Also, immune regulation and self-controlling mechanisms after the COVID-19 pandemic, as well as a decrease in infections due to strict hygienic protocols, may force the immune system towards type 2 immune response. Usual recommendations for managing asthma remain valid despite the ongoing epidemic. Furthermore, it is necessary to identify and protect asthmatic patients who are particularly vulnerable to the COVID-19 infection. Asthma treatments should be pursued to ensure the effective management of patients’ problems throughout the epidemic.
CONCLUSION
The notions presented above suggest that after the COVID-19 pandemic, strict protocols and therapeutic perspectives should be considered to prevent a surge in the incidence and prevalence of allergic diseases and asthma. Therefore, a focus on the COVID-19 infection should not deter us from foreseeing a surge in asthma and other post-coronavirus problems.


