All published articles of this journal are available on ScienceDirect.
Knowledge and Attitudes of Pregnant Thai Women Regarding Modes of Birth: A Hospital-Based Study in Southern Thailand
Abstract
Objective:
This study aimed to determine the knowledge and attitudes of pregnant Thai women regarding modes of birth.
Methods:
A cross-sectional study was conducted at Songklanagarind Hospital. A total of 605 women with a singleton pregnancy and gestational age >20 weeks who attended an antenatal clinic from September 2018 to June 2019 were recruited. Women having a history of cesarean section, or any condition associated with indications for cesarean section, having a fetus with an obvious anomaly, could not read or write in the Thai language, or could not complete the questionnaire were excluded. Their knowledge and attitudes regarding modes of birth were evaluated through self-administered questionnaires.
Results:
Most women (69.4%) had poor knowledge scores (<5), with a median score of 3 (range, 0-9). Only 14.5% of women knew about serious complications of cesarean section in future pregnancies(placental adherence). Multivariate logistic regression analysis showed that factors associated with adequate knowledge scores (>5) were high educational levels (OR 2.06; 95% CI 1.23-3.47), high incomes (OR 1.96; 95%CI 1.32-2.90), and multiparity(OR 1.73; 95%CI 1.18-2.52). Most women had positive attitudes towards vaginal birth. Only 10.2% of women had a preference for cesarean birth. Factors associated with the preference for cesarean birth were advanced maternal age (OR 3.10; 95%CI 1.72-5.60), having an underlying disease (OR 3.61; 95% CI 1.79-7.25), and poor knowledge scores (OR 2.43; 95% CI 1.21-4.91).
Conclusion:
Most pregnant Thai women had poor knowledge of the modes of birth. However, the majority of women had positive attitudes towards vaginal birth.
1. INTRODUCTION
Cesarean section rates are increasing worldwide. According to the latest data from 121 countries, the overall cesarean section rates increased from 6.7% in 1990 to 19.1% in 2014 [1]. Based on the data from a World Health Organization (WHO) global survey, the overall cesarean section rate from 2007 to 2008 in Thailand was 34.1% [2]. At our institution in Southern Thailand, the cesarean section rate (retrieved from the database of the Medical Statistics Unit of the Department of Obstetrics and Gynecology) increased from 34.4% in 2001 to 55.3% in 2017, which is higher than the 10-15% rate recommended by the WHO [3]. Cesarean birth without medical indications has adverse maternal and neonatal outcomes, such as the increased risk of maternal death, admission to the intensive care unit, greater blood loss, need for transfusion, hysterectomy, placenta previa, placental adherence in future pregnancies, and neonatal respiratory morbidity [2, 4, 5]. Several factors have contributed to the increased cesarean section rates for both medically and non-medically indicated reasons. Cesarean section on demand is one of these factors.
Knowledge and attitudes about modes of birth have been reported to influence modes of birth chosen by pregnant women [6, 7]. Therefore, it is essential to study these issues. Knowledge and attitudes of pregnant women about modes of birth are different among countries depending on many factors such as educational levels, culture, belief, socioeconomic status as well as health care system. Previous studies have consistently found that pregnant women often have poor knowledge of modes of birth [6, 8, 9]. However, different contents of knowledge were evaluated based on the researchers’ interests.
Attitudes towards modes of birth have varied among countries and are dependent on the population background, study setting, cultural norms, and standards of practice [6, 8-10]. Women who attended public hospitals were more likely to have positive attitudes towards vaginal birth than those who attended private hospitals [6]. Other studies conducted at public hospitals, including one in Thailand, also demonstrated high rates of positive attitudes towards vaginal birth among pregnant women [8, 9]. The information about these issues is limited in our country where cesarean section rates are continually rising. Therefore, we conducted this study to determine the knowledge and attitudes of pregnant Thai women regarding modes of birth and their preferences for modes of birth as well as factors associated with adequate knowledge and cesarean preference.
2. MATERIALS AND METHODS
This study was approved by the Institutional Review Board of the Faculty of Medicine at Prince of Songkla University (code number: REC.61-177-12-4) and was funded by the Faculty of Medicine, Prince of Songkla University.
A cross-sectional study was conducted to survey the knowledge and attitudes of pregnant Thai women regarding modes of birth. We invited all pregnant women, who attended the antenatal clinic at Songklanagarind Hospital, a university hospital that serves as a tertiary referral center in Southern Thailand, from September 2018 to June 2019, to participate in this study. Written informed consent was obtained from all participants before enrolment in the study. The questionnaires were answered anonymously.
The inclusion criteria were women with a singleton pregnancy and gestational age greater than or equal to 20 weeks. Women with a history of cesarean birth or any condition associated with indications for cesarean section (placenta previa, malpresentation, obstructive lesions in the lower genital tract, leiomyoma of the lower uterine segment that interferes with the engagement of the fetal head, pelvic abnormality, and so forth), whose fetuses had obvious anomalies, those who could not read or write in the Thai language and those who could not complete the questionnaire were excluded. Cards recording the antenatal visits of pregnant women were marked after the completion of the questionnaire to avoid repeat recruitment during subsequent visits.
Knowledge and attitudes towards modes of birth were evaluated through a self-administered questionnaire that was developed based on a literature review. Three obstetricians, with more than 15 years of experience, evaluated the validity of the questionnaire. A pilot study involving 30 volunteers whose characteristics matched with the inclusion criteria, was conducted to test the reliability of the study using Cronbach’s alpha, which was calculated as 0.7. The questionnaire consisted of four parts: demographic data, knowledge of modes of birth, attitudes towards modes of birth, and birth mode preference.
The section regarding knowledge of modes of birth consisted of 10 questions (answers: true/false/do not know) about the risks and benefits of vaginal and cesarean births, with 1 point given for each correct answer and 0 point given for an incorrect or “do not know” answer. The total knowledge score was 10. We defined an adequate knowledge score as greater than or equal to 5 based on our experts’ opinions. Scores were categorized into two groups as poor knowledge (range, 0-4) and adequate knowledge (range, 5-10).
The section about attitudes towards modes of birth consisted of 11 items with a 5-point rating scale (1-5): 1 point, strongly disagree; 2 points, disagree; 3 points, neither agree nor disagree; 4 points, agree; and 5 points, strongly agree.
The last part of the questionnaire assessed birth mode preference. If women chose cesarean birth, their reasons should be provided.
The sample size was calculated based on the estimated prevalence (P = 0.5, α = 0.05, with d = 0.04) of adequate knowledge scores (>5 out of 10). It was determined that at least 601 participants were required.
EpiData software (version 3.1) was used for data collection. Data were analyzed using SPSS version 17. A multivariate logistic regression analysis was performed to identify factors associated with adequate knowledge scores and preference for cesarean birth. Potential variables were maternal age (<35/> 35 years), educational level (<bachelor/>bachelor degree), income (<30,000/>30,000 baht), occupation (housewife/employee/government employee), parity (nulliparity/multiparity), trimester (second/third),underlying disease (yes/no), previous miscarriage (yes/no), poor obstetric experience (yes/no), previous miscarriage (yes/no), and private health care (yes/no). A p-value of <0.05 was considered significant.
3. RESULTS
A total of 625 pregnant women were recruited; however, only 605 cases (96.8%) completed the questionnaires. Demographic characteristics are given in Table 1. The majority of women were in their second trimester.
Table 2 shows an evaluation of knowledge regarding modes of birth. Most women (69.4%) had poor knowledge scores (<5 points), and the median knowledge score was 3 (range, 0-9). The distribution of knowledge scores is shown in Fig. (1). Of the 10 questions, only two items were answered correctly by more than half of those surveyed. These questions were in regard to the recovery period of vaginal birth (recovery after vaginal birth is faster than that after cesarean birth) and breastfeeding (breastfeeding after vaginal birth can be started sooner than that after cesarean birth). Most participants did not know about the potentially serious complications that can occur with cesarean section.
| - |
Total % |
Mean (SD) |
|---|---|---|
| Age (Years) | - | 31.2 (5.3) |
| <35 | 74.2 | - |
| >35 | 25.8 | - |
| Gestational Age (Weeks) | - | 26 (5.8) |
| Second trimester | 62.8 | - |
| Third trimester | 37.2 | - |
| Religions | - | - |
| Buddhism | 71.9 | - |
| Islam and Christianity | 28.1 | - |
| Education | - | - |
| <Bachelor degree | 25.5 | - |
| Bachelor degree or higher | 74.5 | - |
| Occupation | - | - |
| Housewife/unemployed | 21.8 | - |
| Employee/ self-employed | 54.6 | - |
| Government employee | 23.6 | - |
| Monthly Household Income (Baht/Month) | - | - |
| <30,000 | 66.1 | - |
| >30,000 | 33.9 | - |
| Multiparity | 55.2 | - |
| Previous miscarriage | 21.0 | - |
| History of infertility | 13.1 | - |
| Private care | 28.9 | - |
| Previous operative vaginal delivery | 7.7 | - |
| Underlying diseases | 10.9 | - |
| Complications during the current pregnancy | 7.6 | - |
| Poor obstetric experience | 2.8 | - |
| S.No | Statements |
Expected Answer |
Correct % |
Incorrect or Do Not Know % |
|---|---|---|---|---|
| 1 | Blood loss in vaginal birth is greater than in cesarean birth. | False | 33.1 | 66.9 |
| 2 | The infection risk of vaginal birth is higher than that of cesarean birth. | False | 35.0 | 65.0 |
| 3 | Recovery after vaginal birth is faster than that after cesarean birth. | True | 92.7 | 7.3 |
| 4 | Vaginal birth is associated with a lower rate of birth injury. | False | 17.0 | 83.0 |
| 5 | Cesarean birth has a lower rate of respiratory distress in infants than vaginal birth. | False | 34.0 | 66.0 |
| 6 | Cesarean section is a risk factor for placenta previa and placental adherence in future pregnancies. | True | 14.5 | 85.5 |
| 7 | Cesarean birth is associated with greater rates of urinary incontinence and pelvic organ prolapse than vaginal birth. | False | 11.6 | 88.4 |
| 8 | Breastfeeding after vaginal birth can be started sooner than that after cesarean birth. | True | 64.5 | 35.5 |
| 9 | General and regional anesthesia in cesarean birth are not dangerous to both mother and infant. | False | 18.3 | 81.7 |
| 10 | Potential complications of the cesarean section include adjacent organ injuries such as to the bowel, bladder, or ureter. | True | 24.0 | 76.0 |
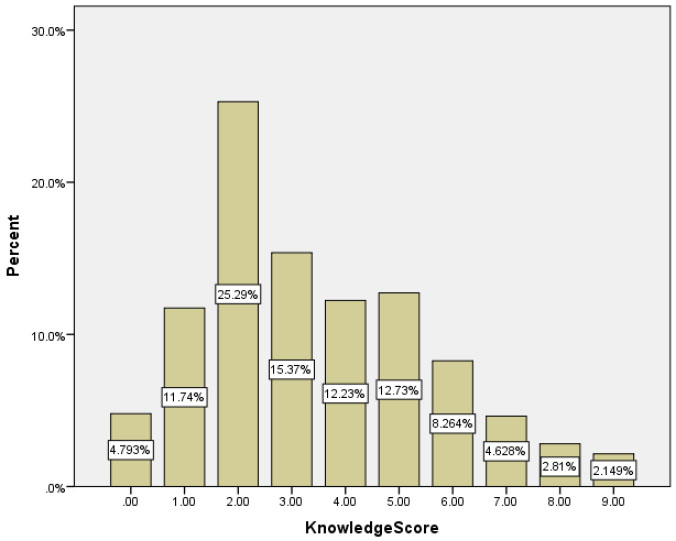
Table 3 shows details of the questionnaire related to attitudes towards modes of birth. The three most common items related to positive attitudes towards vaginal birth (those that participants mostly answered as “agree” and “strongly agree”) were the following:1) vaginal birth is a natural and acceptable method (80.1%), 2) vaginal birth is safe for the mother (70.6%), and 3) vaginal birth is safe for the baby (63%). The most common item related to a positive attitude towards cesarean birth (agree/strongly agree) was: “I prefer a cesarean birth because it is less painful than vaginal birth”(49.2%). The three items related to the benefits of cesarean birth (item number 6,7,8) were rated agree/strongly agree for approximately 20-35%. The percentages of items indicating positive attitudes towards vaginal and cesarean births are shown in Fig. (2).
Only 10.2% of women preferred cesarean birth. The most frequent reason for this preference was fear of labor pain (61.2%), followed by safety concerns for the baby (38.7%).
| S.No | Statements |
Strongly disagree (1) % |
Disagree (2) % |
Neither Agree Nor Disagree (3) % |
Agree (4) % |
Strongly Agree (5) % |
|---|---|---|---|---|---|---|
| 1 | Vaginal birth is safe for the mother. | 0.3 | 2.3 | 26.8 | 57.4 | 13.2 |
| 2 | Vaginal birth is safe for the baby. | 0.3 | 3.3 | 33.4 | 52.9 | 10.1 |
| 3 | Vaginal birth is a natural and acceptable method. | 0.3 | 1.5 | 18.0 | 56.1 | 24.1 |
| 4 | Women who deliver by cesarean section miss an opportunity to have a natural birth. | 2.5 | 18.3 | 22.7 | 39.8 | 16.7 |
| 5 | I prefer a cesarean birth because it is less painful than vaginal birth. | 5.1 | 19.7 | 26.1 | 42.0 | 7.1 |
| 6 | Cesarean birth is convenient and safe. | 3.0 | 21.0 | 47.1 | 25.9 | 3.0 |
| 7 | Cesarean birth by scheduling birth date and time is great for the baby. | 10.9 | 37.0 | 30.3 | 18.0 | 3.8 |
| 8 | If there is an intention for tubal ligation, cesarean birth is much better. | 2.6 | 18.3 | 45.0 | 30.1 | 4.0 |
| 9 | Vaginal birth environment makes me stressed and anxious. | 0.7 | 7.7 | 22.0 | 53.4 | 16.2 |
| 10 | I am afraid of frequent and painful vaginal exams during labor. | 5.0 | 28.9 | 23.3 | 36.7 | 6.1 |
| 11 | I am worried about decreased sexual satisfaction following vaginal birth. | 9.1 | 39.0 | 28.1 | 20.2 | 3.6 |
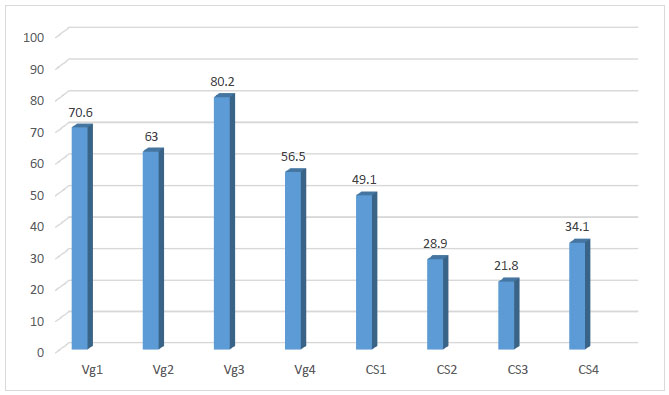
Vg1: Vaginal birth is safe for the mother.
Vg2: Vaginal birth is safe for the baby.
Vg3: Vaginal birth is a natural and acceptable method.
Vg4: Women who deliver by cesarean section miss an opportunity to have a natural birth.
CS1: I prefer a cesarean birth because it is less painful than vaginal birth.
CS2: Cesarean birth is convenient and safe.
CS3: Cesarean birth by scheduling birth date and time is great for the baby.
CS4: If there is an intention for tubal ligation, cesarean birth is much better.
The authors performed a multivariate logistic regression analysis to identify factors associated with adequate knowledge scores. Five factors (retrieved from the univariate analysis) were included in the final model: educational level, income, parity, occupation, and previous miscarriage. Only three factors, high educational level, high income, and multiparity, were statistically significant (Table 4).
Significant factors associated with the preference for cesarean birth in the final model of multivariate logistic regression analysis were advanced maternal age, having an underlying disease, and poor knowledge scores. These were adjusted for parity, income, poor obstetric experience, previous miscarriage, trimester, and private health care (Table 5).
Table 4.
| - | Adjusted Odds Ratio | 95% Confidence Interval | P-value |
|---|---|---|---|
| High educational level (bachelor degree or higher) | 2.06 | 1.23-3.47 | .006 |
| Occupation | - | - | - |
| Housewife/ unemployed | 1 [Reference] | - | - |
| Employee/self-employed | 1.24 | 0.74-2.10 | .41 |
| Government employee | 1.79 | 0.97-3.29 | .06 |
| High income (> 30,000baht/month) | 1.96 | 1.32-2.90 | .001 |
| Multiparity | 1.73 | 1.18-2.52 | .005 |
| Previous miscarriage | 0.66 | 0.42-1.06 | .08 |
| - | Adjusted odds ratio | 95%confidence interval | P-value |
|---|---|---|---|
| Age>35 years | 3.10 | 1.72-5.60 | < .001 |
| Underlying diseases | 3.61 | 1.79-7.25 | .001 |
| Poor knowledge scores | 2.43 | 1.21-4.91 | .01 |
| Multiparity | 1.27 | 0.69-2.33 | .45 |
| Income >30,000 baht | 1.64 | 0.89-3.02 | .11 |
| Poor obstetric experience | 1.80 | 0.51-6.39 | .37 |
| Previous miscarriage | 1.03 | 0.54-1.98 | .93 |
| Private care | 1.66 | 0.89-3.08 | .11 |
| Third trimester | 0.72 | 0.39-1.34 | .30 |
4. DISCUSSION
This study demonstrated that most pregnant women had poor knowledge of modes of birth, especially regarding the serious complications of cesarean section. However, most women had a positive attitude towards vaginal birth and chose this birth mode. Factors associated with adequate knowledge were high education, high income, and multiparity, while those associated with cesarean preference were advanced maternal age, having an underlying disease, and poor knowledge scores.
We found that most women had poor knowledge of modes of birth, similar to other studies [6, 9, 11]. However, details of knowledge evaluation were different and dependent on researchers’ interests. Yamasmit and Chaithongwongwatthana conducted the study in Thailand and found that only 3.1% of participants provided correct answers to questions about modes of birth [9]. When we focused on the details of knowledge, the majority of women did not recognize the serious risks of cesarean section for future pregnancies, especially placenta previa and placental adherence. This information is useful for establishing an educational program during antenatal visits focusing on improving poor knowledge of the benefits and risks of different modes of birth, especially serious risks of cesarean section.
There have been limited studies on factors associated with knowledge of modes of birth with inconsistent results. It is likely due to differences in knowledge backgrounds, cultures, or beliefs. Ghotbi et al. demonstrated that Iranian women of advanced maternal age (>35 years) had higher knowledge scores than younger women [6]. Aali and Motamedi reported that the educational levels of Iranian women were not associated with knowledge of modes of birth [8]. On the contrary, we found that higher educational levels, higher incomes, and multiparity were significantly associated with adequate knowledge scores. Advanced maternal age was not a significant factor in this study. Multiparous women had previously experienced childbirth, and therefore, had better knowledge of the modes of birth than nulliparous women. High income was usually related to a high educational level.
Regarding attitudes towards modes of birth, similar to previous studies performed at public hospitals, the majority of women had positive attitudes towards vaginal birth [8, 9, 12]. However, a lower proportion of women in studies at private hospitals had a positive attitude towards vaginal birth [6]. Maternal request for a cesarean birth is not permitted at our hospital, so recruitment bias could have occurred, because women who attended our hospital may be more likely to prefer vaginal birth. On the contrary, women who prefer cesarean birth would most likely attend a private hospital.
Regarding attitudes towards cesarean birth, less than half of the women agreed with the following item: “I prefer cesarean birth because it is less painful than vaginal birth.” Furthermore, only 20-35% of women agreed or strongly agreed with the benefits of cesarean birth such as convenience, scheduling birth date, and intention for tubal ligation. In addition, women were not as concerned with the disadvantages of vaginal birth, such as frequent pelvic exams during labor and sexual dissatisfaction following vaginal birth. These data indicated that most women had positive attitudes towards vaginal birth.
Rates of preference for cesarean birth varied among studies from 6% to 38.9% [6, 9, 13-17]. One international meta-analysis found that 15% of women preferred cesarean birth [17]. Researchers from a public hospital in Thailand found that only 12.5% of participants preferred cesarean birth [9]. We found a lower percentage of women preferred cesarean birth (10.2%); with the two most common reasons being fear of labor pain and safety concerns for the baby, this was similar to previous studies [6, 15, 16, 18-20]. This finding implies that during the antepartum period, we need to provide more knowledge in regards to pain control options during labor, such as narcotic drugs, epidural analgesia, and nitrous oxide.
Significant factors associated with the preference for cesarean birth in our study are as follows: advanced maternal age, having an underlying disease, and poor knowledge scores. Advanced maternal age and having an underlying disease were self-perceived risk factors and could not be modified. These women probably felt they were not fit enough for vaginal delivery and were worried about the safety of their babies. Most women with poor knowledge scores did not know about the serious complications associated with a cesarean birth. They probably believed that undergoing cesarean section was safe and were more likely to have positive attitudes towards it. Researchers from Norway revealed that predictors of the preference for cesarean birth were previous cesarean section, negative delivery experience, and fear of birth [15]. We excluded women with previous cesarean births because repeating cesarean section for subsequent pregnancies is our standard practice. The poor obstetric experience was not a significant factor in multivariate analysis. Anxiety and fear of birth were significant predictors of preferring cesarean birth in other studies [6, 15, 16, 18-20].
Parity was not a significant factor for cesarean birth preference in this study, whereas some researchers found that multiparous women preferred cesarean birth more often than nulliparous women [21, 22]. However, researchers from Norway showed that the strong preference for cesarean birth by multiparous women was attributable to other factors, such as previous cesarean birth or fear of birth, but not to parity itself [15]. This study demonstrated that having an underlying disease was significantly associated with the preference for cesarean birth, which had not been reported previously.
The strengths of our study were the good reliability of the questionnaire and the large sample size. In addition, it was conducted in Thailand, a country in Southeast Asia, where data have not been extensively published. To our knowledge, having an underlying disease as a significant factor associated with cesarean preference has not previously been reported. Interestingly, we demonstrated that most women had poor knowledge concerning the serious consequences of cesarean-section being associated with high morbidity and mortality in future pregnancies. This information is useful for obstetricians or health care providers as there is a need to pay attention to the counseling of pregnant women and their couples during antenatal visits to address this point. Women who prefer cesarean birth may change their minds if they realize its detrimental risk. One semi-experimental study revealed that a group consultation is an appropriate approach to improve knowledge and attitudes towards the mode of birth as well as the mothers’ decisions to choose a vaginal birth mode [23].
Limitations of this study must also be addressed. The participants may not be representative of pregnant women in other settings, such as those attending private hospitals, where the cesarean section rate is much higher due to the availability of cesarean section upon request. In addition, participants were recruited with a wide range of gestational ages (20-40 weeks), and delivery mode preference may change as gestational age advances. However, multivariate logistic regression analysis showed no significant difference in birth mode preference between second and third trimesters.
Based on our findings, we recommend educating women and their families about the risks and benefits of different modes of birth, especially the serious risks and consequences associated with cesarean birth, and modalities of pain control during labor. Education can be undertaken through available data sources such as social media, television, radio, pamphlets, antenatal clinic counseling programs, and secondary school curricula, to help women improve their knowledge and change their attitudes towards modes of birth. This approach might decrease the demand for cesarean birth, especially at private hospitals.
CONCLUSION
Most pregnant women had poor knowledge of the modes of birth, especially the serious risks of cesarean birth. However, the majority of women had positive attitudes towards vaginal birth and chose this birth mode. Implementation of antenatal educational program regarding risks and benefits of vaginal and cesarean births, serious consequences of cesarean birth as well as pain control during labor is recommended.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The ethical approval was obtained from the Institutional Review Board of the Faculty of Medicine, Prince of Songkla University, Thailand with approval no. REC.61-177-12-4..
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All participants were provided information sheets about the study and all the women signed written informed consent before answering the self-administered questionnaires.
STANDARDS OF REPORTING
STROBE guidelines and methodologies were followed.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated and/or analysed during the current study are available from the corresponding author upon reasonable request.
FUNDING
This research was funded by the Faculty of Medicine, Prince of Songkla University.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors wish to thank Andrew Tait for language editing.


