All published articles of this journal are available on ScienceDirect.
Health System Strategies and Adolescent Sexual Health: A Systematic Review of the Literature using Rodgers Concept Analysis Framework
Abstract
Background:
Health Systems Strategies play a key role in determining Adolescent Sexual Health outcomes. This study aims to review the literature on the relationship between Health Systems Strategies and Adolescent Sexual Health issues guided by Rodger's evolutionary concept analysis framework. The study further develops a Conceptual Framework that would guide a study that seeks to “Develop strategies to facilitate safe sexual practices in adolescents through Integrated Health Systems in selected Districts in Zimbabwe.”
Methods:
Adolescents, Health Systems, Sexual Health, and Strategies were used to search for published literature (in English) on Google Scholar, PUBMED, EBSCO, Cochran Library, and Science Direct. A total of 142 Articles and 11 reports were obtained, and the content was screened for relevance. This led to 42 articles and 03 reports being found suitable and relevant, and thus, the content was reviewed. Thematic analysis was done to identify attributes, antecedents, and consequences of Health Systems Strategies on Adolescent Sexual Health. These findings were then used to inform the development of the Conceptual Framework.
Results:
Key attributes, antecedents and consequences of Health System Strategies on Adolescent Sexual Health were identified. Strategies to Improve Adolescent Sexual Health outcomes were also identified.
Conclusions:
Different contextual factors influence policy changes and the consequences are mixed, with both positive and negative outcomes.
1. BACKGROUND
Ensuring safe sexual practices in adolescents is one of the critical challenges that have been faced even up to the 21st century [1, 2]. There have been several factors that have led to negative Sexual Health (SH) outcomes in adolescents. Different authors have noted these as unfriendly sexual health care services for adolescents, inadequate health care financing, to mention a few [2, 3]. Adolescents are the future of tomorrow However, statistics show that there are at a high risk of dying earlier before they realise their full potential because of Sexually Transmitted Infections (STIs) such as Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS) [4, 5]. An adolescent in this study is defined as a young person aged 10 to 19 years and is transitioning into adulthood [6, 7]. Adolescent utilisation of SH care services in low and middle-income countries remains low despite many strategies that have been implemented to create demand for these services [1, 8]. Most countries find it challenging to provide comprehensive and integrated HSs to cater to adolescents' SH issues [9, 10]. The demand and utilisation of modern health care services by adolescents remain low despite this considerable investment in these services [1, 8].
Health Systems (HSs) play a significant role in ensuring access to SH services by adolescents and, in turn, impact their SH outcomes [8]. HSs have been defined as the organisation of people, institutions, and resources to ensure the delivery of SH services to adolescents [6, 11, 12]. It is important to note that this age group is not independent in making their decisions; therefore, they rely on their environments to inform their choices [12].
Several strategies have been implemented worldwide to improve Adolescent Sexual Health (ASH) outcomes [1, 13, 14]. Strategies in this study will be defined as a plan implemented within a HS to impact the SH outcomes of adolescents [15]. Despite implementing some strategies, adolescents remain highly vulnerable, with a high prevalence of Sexually Transmitted Infections (STIs), high incidence of teenage pregnancy, resulting in increased numbers of adolescents dropping out of schools [3, 12, 16]. Dropping out of the formal schooling system subjects adolescents to poverty, particularly in Low and Middle-Income Countries (LMCIs), where employment opportunities are hard to come by, and there is stiff competition for the few available opportunities [2]. Concepts are not well understood when it comes to implementing ASH programs leading to low demand for such programs that are meant to improve their SH outcomes [1, 8]. Therefore, this study aimed to review literature submissions to determine the relationships between HSSs and ASH issues guided by Rodger's evolutionary concept analysis framework. The study further sought to leverage the findings of this literature review to develop a Conceptual framework (CF) that would guide research on “Development of strategies to facilitate safe sexual practices in adolescents through integrated health systems in selected districts of Zimbabwe” [17].
2. METHODS
2.1. Rodgers Concept Analysis Framework
Rodgers' evolutionary concept analysis framework would guide this study. Rodgers argued that to understand the nature of concepts, and there is a need to understand the contextual forces that influence a specific idea at a specific time and point [18, 19]. It should be noted that these concepts are dynamic and evolve with time [18]. Rodgers's CF leverages on three key elements: a) Antecedents- these are classified as events or incidents that must occur before the occurrence of the concept; b) Attributes – that are described as characteristics of that specific concept in terms of addressing its intended issue; c) Consequences under this framework are defined as the outcomes of the concepts as identified from literature [20, 21].
2.2. Collection and Analysis of Data
2.2.1. Inclusion Criteria
In this systematic review, studies that presented Health System Strategies that targeted Adolescent Sexual Health were considered. Studies and reports published in English up to December 2020 in peer-reviewed journals the world over were targeted. The focus was on original quantitative and qualitative research and reports obtained from Google Scholar, PUBMED, EBSCO, Cochran Library, and Science Direct. The selected articles and reports had to pass the quality assessment criteria described in 2.2.6.
2.2.2. Exclusion Criteria
Studies that focussed on the relationship between Health System Strategies and their impact on other age groups (other than adolescents) were excluded from this study.
2.2.3. Search Strategy
The keywords Adolescents, Health Systems, Sexual Health, and Strategies were used to search for literature from Google Scholar, PUBMED, EBSCO, Cochrane Library, and Science Direct. The obtained literature was screened for content and relevance, as discussed in the sections that follow.
2.2.4. Methods of Review
Titles and abstracts were reviewed independently by the primary researcher and submitted to the promoters for further scrutiny and guidance to identify relevant articles and reports that had to be included in this study. Disagreements were resolved through dialogue between the student and all the three promoters and reaching a consensus based on facts exchanged. Therefore, the first author reviewed the full texts of these articles and reports that met the inclusion criteria and the review outcome discussed with the co-authors.
2.2.5. Data Extraction and Synthesis
A data collection form was developed guided by Rodgers Evolutionary Conceptual Analysis Framework to facilitate uniform data collection on attributes, antecedents, and consequences of Health System Strategies on Adolescent Sexual Health from the articles and reports that met the inclusion criteria. The first author reviewed all articles and reports and extracted data submitted to the co-authors for scrutiny and further guidance. Discrepancies observed on collected data were resolved through dialogue and reaching a consensus. Findings from the articles and reports were coded and thematically analysed to identify and explain antecedents, attributes, and consequences of HSSs on ASH.
2.2.6. Quality Assessment
A quality evaluation tool was adapted and used to assess the selected studies' potential to answer the research questions in line with Rodgers' Evolutionary Concept Analysis Framework [22]. This tool enables one to determine whether original studies adhered to 14 quality criteria for quantitative studies and 10-point quality criteria for qualitative studies [22]. Articles and reports were assessed for clarity in presenting attributes, antecedents, and consequences of HSSs on ASH. Furthermore, the AMSTAR tool for evaluating the methodological quality of systematic reviews was used to assess the quality of the systematic review methods. The AMSTAR tool was developed to assess the methodological quality and rigor of different articles obtained from online databases [23]. A PRISMA checklist was also completed to ensure that the study fulfilled the expectations of review articles. The outcome of the checklist is presented in Table 1.
2.2.7. Timeline
A literature search and quality appraisal, data extraction, synthesis, and writing up were done concurrently between January 2019 and December 2020.
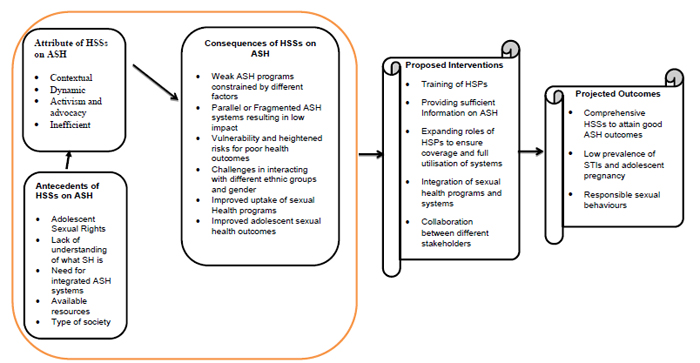
2.2.8. Development of a Conceptual Framework
Findings from this study informed the development of a Conceptual framework that explained the relationship between the identified antecedents and attributes that influence adolescents' sexual outcomes (consequences). The theoretical framework would be presented in a diagram format to understand how these factors relate to adolescent sexual health.
Table 1.
| AMSTAR criteria / Question | Response | Justification |
|---|---|---|
|
1. Was an 'a priori' design provided? The research question and inclusion criteria should be established before the conduct of the review. |
Yes | A review protocol was developed before conducting the literature review |
|
2. Was there a duplicate study selection and data extraction? There should be at least two independent data extractors and a consensus procedure for disagreements should be in place. |
Yes | Three reviewers reviewed the articles and reports, and a clear procedure describe to iron out disagreements and reach a consensus |
|
3. Was a comprehensive literature search performed? At least two electronic sources should be searched. The report must include years and databases used (e.g. Central, EMBASE, and MEDLINE). Keywords and or MESH terms must be stated and where feasible the search strategy should be provided. All searches should be supplemented by consulting current contents, reviews, textbooks, specialised registers, or experts in the particular field of study, and by reviewing the references in the studies found. |
Yes | The review focussed on original quantitative and qualitative research and reports obtained from Google Scholar, PUBMED, EBSCO and Science Direct. |
|
4. Was the status of publication (i.e. grey literature) used as an inclusion criterion? The authors should state that they searched for reports regardless of their publication type. The authors should state whether or not they excluded any reports (from the systematic review), based on their publication status, language, etc. |
Yes | The inclusion and exclusion criteria are fully described and summarised in the PRISMA flow diagram presented in this review as Fig. (1). |
|
5. Was a list of studies (included and excluded) provided? A list of included and excluded studies should be provided. |
No | The list was not provided but can be supplied upon request |
|
6. Were the characteristics of the included studies provided? In an aggregated form, such as a table, data from the original studies should be provided on the participants, interventions and outcomes. The ranges of characteristics in all the studies analysed e.g. age, race, sex, relevant socioeconomic data, disease status, duration, severity, or other diseases, should be reported. |
Yes | These were summarised as Table 1-3 that present an overview of contributions from literature sources according to three Rodgers characteristics: attributes, antecedents, and consequences. |
|
7. Was the scientific quality of the included studies assessed and documented? 'A priori' methods of assessment should be provided (e.g., for effectiveness studies if the author(s) chose to include only randomised, double-blind, placebo-controlled studies, or allocation concealment as inclusion criteria); for other types of studies, alternative items will be relevant. |
Yes | These were assessed using the 14-point quality assessment tool and Rodgers Evolutionary Conceptual Framework. |
|
8. Was the scientific quality of the included studies used appropriately in formulating conclusions? The results of the methodological rigour and scientific quality should be considered in the analysis and the conclusions of the review and explicitly stated in formulating recommendations. |
Yes | Studies that were included were guided and met Rodgers Evolutionary conceptual analysis framework requirements |
|
9. Were the methods used to combine the findings of studies appropriate? For the pooled results, a test should be done to ensure the studies were combinable, to assess their homogeneity (i.e. Chi-squared test for homogeneity, I2). If heterogeneity exists, a random-effects model should be used and or the clinical appropriateness of combining should be taken into consideration (i.e. is it sensible to combine?). |
N/A | The review had a guiding conceptual framework; therefore, the combination of articles was guided by this framework |
|
10. Was the likelihood of publication bias assessed? An assessment of publication bias should include a combination of graphical aids (e.g., funnel plot, other available tests) and or statistical tests (e.g., Egger regression test). |
N/A | The review was guided by Rodgers' Evolutionary Concept Analysis framework. However, limitations of this systematic review are presented. |
|
11. Was the conflict of interest stated? Potential sources of support should be clearly acknowledged in both the systematic review and the included studies. |
Yes | All authors declared that they did not have any conflict of interest. |
3. RESULTS
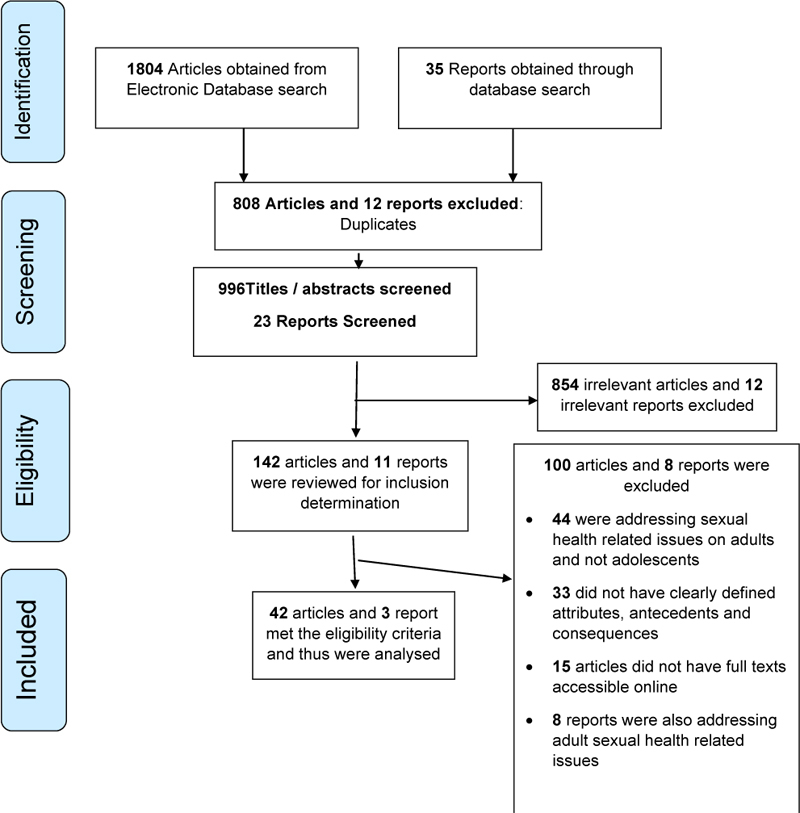
There were 1804 articles and 35 reports that were obtained through an electronic search of databases. After screening for duplicates, 996 articles and 23 reports had their titles and abstracts reviewed by all four authors. Of these reviewed articles and reports, 854 articles and 12 reports were excluded as their content was irrelevant to this study. This sampling procedure meant that 142 articles and 11 reports were reviewed to determine whether they met the inclusion criteria. After reviewing the articles and reports, the three authors resolved those 42 articles and 3 reports met the inclusion criteria and were then analysed. These results are summarised in the PRISMA flow diagram in Fig. (1).
3.1. Outcome of Quality Assessment Tools
All selected articles were subjected to the 14-point quality assessment tool and met the minimum standards required. The AMSTAR tool results on Methodological Quality pointed out that the methods used were sufficient to address this systematic review's research questions. These findings are presented in Table 1.
3.2. Definition of Sexual Health
The definition of sexual health has evolved over the years, leveraging on the 1975 World Health Organization that defined sexual health as “Integration of the somatic, emotional, intellectual and social aspects of sexual being in ways that are positively enriching and that enhance personality, communication, and love” [16, 24, 25]. The change in these definitions has been influenced by political, social, historical events, and human rights considerations [3, 24]. After the sexual revolution in the 1960s, there has been an ongoing struggle over reproductive rights, rights for same-sex relationships, and abortion rights for adolescents [24]. These struggles are influenced by different contextual factors, with some countries rejecting implementing or aligning some of the proposed sexual rights [26, 27]. These have influenced how health systems are structured in different countries with different contextual features resulting in varying adolescent sexual health outcomes [28].
3.3. Attributes, Antecedents and Consequences of HSSs Influencing ASH
3.3.1. Antecedents
Antecedents that influence ASH reported in the literature were: adolescent sexual rights, lack of understanding of what sexual health is, need for integrated ASH systems, available resources, and type of society. Literature sources reporting these attributes are summarised in Table 2.
| Key Antecedent Factors | Supporting Literature |
| Adolescent sexual rights | [2, 16, 28-31] |
| Lack of understanding of what sexual health is | [16, 24, 30, 32, 33] |
| Need for Integrated ASH Systems | [7, 13, 30, 34] |
| Available Resources | [32, 33] |
| Type of society | [16, 32, 35-38] |
3.3.1.1. Adolescent Sexual Rights
One of the antecedent themes that arose from literature was the need to protect adolescents as a human right necessity/requirement [2, 29]. Authors argue that adolescent sexual rights, such as access to sexual health information, are more often violated [2, 29]. There are arguments that sexual education is restricted in schools or religious setups, thereby denying adolescents essential information that would inform their decisions regarding sexual health [16]. Therefore, most strategies have been targeted at improving adolescent access to information, and various health systems have used different techniques to disseminate as much information as possible on sexual health [30]. Some of these strategies have leveraged available technologies (social media, utilisation of sports, to name a few) to ensure that information is disseminated to adolescents [31]. Authors further argue that the current health systems are rigid and violate adolescents' rights [28]. Flicker and Guta (2007) say that there is a need for adolescents to make their own decision in being part of research that is meant to gather data aimed at improving their sexual health outcomes [28]. They argue that involving parents in consenting to adolescents participating in sexual research silences them, which negatively impacts the process of collecting data that answers questions regarding the adolescents' expectations [28].
3.3.1.2. Lack of Understanding of What Sexual Health is
Sexual health definitions have evolved over the years and have been contextualised to suit specific environmental contexts [16, 24]. Different settings have created varied illustrations that are sometimes contradictory and create confusion, with other countries contextualising the meanings to suit their way of living [24]. The universal understanding of what sexual health entails is therefore influenced by cultural, social, political, and environmental contexts and might differ from country to country or continent to continent [16, 24]. Therefore, HSs have been designed to lack comprehensiveness as there are varied expectations that commonly undermine international expectations and recommendations regarding the management of ASH issues [16, 24]. Some authors argue that most health service providers do not speak about sexual health issues as often as they are expected to address the sexual health concerns of adolescents [32] proactively. Lack of such interaction has created huge gaps in knowledge in adolescents [32, 33]. It is also presented that most studies evaluating the impact of different HSSs on promoting sexual health in young people often lack methodological rigour leading to uncomprehensive conclusions and recommendations. These then do not adequately inform policymakers on the direction they should take with their strategies to promote safe sexual practices in young people [30].
3.3.1.3. Need for Integrated ASH Systems
Adolescents need to be exposed to programmes that enhance their negotiating skills for safe sexual behaviours [34]. The approaches or strategies used should be comprehensive in providing them with skills that improve their ability to make beneficial relationships (with their parents, guardians, and adults in general) that are supportive and offer them guidance towards economically sound career prospects [7, 34]. ASH strategies should, therefore, go beyond sexual issues to provide an integrated platform to ensure healthy development in these adolescents [7]. Thus, strategies targeting these groups should be driven by the need to facilitate growth and enhance skills beyond sexual health issues and offer equal opportunities for girls and boys [34]. There is a gap that ASH programs are not integrated into main HS structures, leading to less time and resources being dedicated to this cause [13, 30].
3.3.1.4. Available Resources
HSSs are crafted based on available resources to fund and sustain specific sexual health programs [32]. Health service providers in resource-poor settings avoid “opening a can of worms,” asking questions or following up on adolescent sexual health issues that would require more resources and time than the HS can offer at that specific time and point [32]. Lack of resources leads to non-prioritisation of adolescent sexual health issues and avoidance of asking or following up on matters that might have a bearing on ASH issues [32, 33].
3.3.1.5. Type of Society
HSSs are influenced by different ethnic values [32, 35]. Most people identify with different cultural norms that could be for or against certain HSSs [35]. Strategies that clash with specific societal beliefs are bound not to work. Adolescents from poor settings, such as those from rural areas, are more at risk of suffering adverse sexual health outcomes than those in urban areas with easy access to information and health facilities [36, 37]. Adolescents utilising Indigenous Health Systems (IHSs) often have poor health outcomes as compared to using Modernised Health Systems (MHSs) [38]. Therefore, crafting and implementing HSSs to address ASH issues are leveraged on specific societal characteristics to generate demand for ASH services [16, 35-41].
3.3.2. Attributes
Sexual health attributes obtained from literature were: contextual, dynamic, activism, advocacy, and inefficient. Literature sources reporting these attributes are summarised in Table 3 below.
3.3.2.1. Contextual
There is no consensus on how sexual health is defined, interpreted, and infused into HSs within different communities in different countries [24, 25]. HSSs implanted in various communities in different countries are influenced by contextual factors such as political environment, culture, religion, technological developments, and many more that will prevail at that specific time and point [16, 24, 25, 42, 43]. There is also a need for the HSSs to align and observe different societal values and expectations and conform to the leadership structures in charge then [35, 44].
3.3.2.2. Dynamic
Different HSSs are implemented to address ASH issues in response to ever-changing environments [37, 39-42, 45]. It is presented that strategies to address sexual health issues have evolved in line with the ever-changing environmental and contextual factors leading to the utilisation of different technological platforms to ensure the relevance of the strategies in addressing ASH issues [16, 24, 25, 39, 41, 43].
3.3.2.3. Activism and Advocacy
Most HSSs, as identified in the literature, leverage activism and advocacy to create demand for ASH programs [31, 46, 47]. Different strategies are demonstrated as health service providers utilise various methods to involve adolescents and lure them into programs that target their knowledge, attitudes, and behaviours to promote safe sexual practices [48-50].
3.3.2.4. Inefficient
Due to differences in adolescents' age groups, social status, ethnic beliefs, and expectations, designed HSSs are never comprehensive enough [16, 24]. Therefore, it is noted that most HSSs have their strengths and weaknesses, thus putting some adolescent populations at risk while, on the other hand giving advantages to other adolescent populations [32, 33, 35-37].
3.3.3. Consequences
Consequences of these attributes and antecedents were: Weak adolescent programs constrained by different factors, parallel or fragmented systems resulting in low impact, vulnerability, and heightened risks for poor health outcomes and challenges in interacting with various ethnic groups and gender. Literature sources reporting these consequences are summarised in Table 4.
| Key Consequences Factors | Supporting Literature |
|---|---|
| Weak adolescent programs constrained by different factors | [2, 7] |
| Parallel or Fragmented ASH Systems resulting in low impact | [13] |
| Vulnerability and heightened risks for poor health outcomes | [3, 7, 34, 39-41] |
| Challenges in interacting with different ethnic groups and gender | [26, 27, 32, 33] |
| Improved uptake of sexual health programs | [41, 42, 51, 52] |
| Improved adolescent sexual health outcomes | [3, 8, 9, 16, 29, 39, 41, 42, 51, 52] |
3.3.3.1. Weak Adolescent Programs Constrained by Different Factors
Adolescent sexual health programs usually fail to achieve desired health outcomes. There are stigma and controversial attitudes that undermine these adolescent sexual health programs rendering them ineffective [7]. These factors expose adolescents to fragmented programs that exacerbate their vulnerability, mainly fuelling confusion in how adolescents are expected to conduct themselves regarding sexual health issues [7]. Therefore, adolescents become victims of sexual violence, early pregnancies, unsafe abortions, and STIs [2, 7].
3.3.3.2. Parallel or Fragmented Systems Resulting in Low Impact
It was revealed that several ASH programs are delivered as specific fragments addressing specific programs [13]. Sexual health programs such as those addressing STIs, HIV, and AIDS and family planning are generally funded by different organisations leading to a fragmented approach in addressing ASH issues [13]. Most HSSs, therefore, lack comprehensiveness and run parallel to each other though delivered to the same recipients leading to conflicts, duplication, confusion, and inefficient utilisation of resources [13].
3.3.3.3. Vulnerability and Heightened Risks for Poor Health Outcomes
Adolescents are placed at heightened risks for poor sexual health outcomes due to the non-compatibility of HSSs considering the developmental needs of their specific age groups [3, 34, 41]. There is a need to contextualise strategies to consider the different developmental stages and the requirements of these adolescents, thereby ensuring that the approach used is appropriate to attain desired goals [7, 39-41].
3.3.3.4. Challenges in Interacting with Different Ethnic Groups and Gender
Authors point out that no matter how accommodating some HSs are to adolescents, some ethnic groups were born from less liberal communities and are not forthcoming in discussing sexual health-related issues [32]. It is also presented that gender plays a vital role as some health service providers prefer talking about sexually related matters with service recipients of the same sex [32, 33]. This disadvantages some service recipients as they are denied the chance to be given information that they could pass on to their children in adults' cases, thereby disturbing sexual health information dissemination [33]. There are also challenges where most health service providers find it challenging to discuss sexual health issues with individuals in same-sex relationships [32]. These challenges create barriers in HS functions regarding information dissemination expected to foster safe sexual practices in adolescents [26, 27, 32].
3.3.3.5. Improved Uptake of Sexual Health Programs
Some strategies in some settings have centred on behaviour change communication, life skills and livelihoods, youth-friendly service delivery, policy advocacy, and coordination [51, 52]. Furthermore, implementing a multi-sectorial approach to ASH package delivery and all this, in turn, enhanced uptake of services in different country settings [41, 42, 52].
3.3.3.6. Improved Adolescent Sexual Health Outcomes
Different contextual strategies that have been implemented in other countries led to improved health outcomes [52]. The result of these strategies has been an increase in proportions of adolescents who seek ASH information utilisation of the reproductive health services and products, voluntary testing as well as the adoption of safe sexual practices [3, 8, 9, 16, 29, 39, 41, 42, 52].
3.4. Overcoming Barriers to Safe Sexual Practices in Adolescents
Sources found in the literature suggested that training, providing sufficient information to adolescents, and expanding roles of Health Service providers would improve adolescent sexual Health Outcomes. These findings are summarised in Table 5 and further expanded on in the sections that follow.
3.4.1. Training
It is evident from the findings of this study that most HSs are very unfriendly to adolescents. Those manning the HSs are often judgemental, less tolerant, and hostile towards adolescents [9, 53]. Generally, proposals from the literature suggest that for HSSs to address ASH issues effectively, there is a need to train HSPs to be accommodative, sensitive, and tolerant to adolescents [32, 54]. Considering the above proposals will enable these ASH systems to be accessible to adolescents through the generation of demand for services offered, thereby improving coverage of ASH programs and thus minimising barriers associated with poor relations between adolescents and HSPs.
3.4.2. Providing Sufficient Information on SH
Findings in this study suggest that SH is misunderstood, and the definitions are not internationalised. Different contextual factors influence SH's interpretations, and diverse communities have a varied understanding of what sexual health is. Different strategies, therefore, are used in specific population groups and are hard to adapt or adopt in other populations. There are proposals that SH issues should be infused into the curriculum at schools to ensure that all adolescents get relevant information on SH [3, 39, 55]. Some conservative communities might not permit SH information sharing between parents and adolescents outside the school setup [56, 57]. Using contextualised strategies for different adolescent age groups would enable effective information sharing and promote safe sexual practices in adolescents [7, 32, 33, 39, 41, 58-60]. There is also a need to encourage dialogue between adolescents and their parents to facilitate information sharing and responsible parenting and guidance regarding SH issues [58].
3.4.3. Expanding the Roles of HSPs to Ensure Coverage and Full Utilisation of Systems
It is presented in the findings that HSPs do not address SH issues proactively with adolescents, thus making the services rendered ineffective and disjointed [32]. HSPs should take a leading role in disseminating and marketing ASH programs to the extent that their services could be extended to schools [32, 39]. The availability of useful information would ensure demand generation for ASH programs, trust-building between HSPs and adolescents and the general community. Such a scenario would reduce conflicts between different HSs and foster an inclusive and integrated approach to the management of ASH issues.
3.5. The Conceptual Framework Resulting from the Findings
A conceptual framework was developed based on the findings of this study and presented in Fig. (2). The model also included proposed strategies found in the literature that aimed to improve ASH outcomes and the desired outcomes that would, therefore, be achieved.
4. DISCUSSION
It was noted that different contextual settings have different definitions for Adolescent Sexual health, thus influencing the packages available to adolescents, thereby justifying the success and failure of programs in different countries. These countries have various service providers with varying competencies and ideologies and the working conditions (contextual factors) as informed by the interpretation and prioritisation of ASH issues [61, 63]. Understanding different issues relating to ASH has a bearing on the systems' efficiency and effectiveness that would be conceptualised and implemented in response to the adolescents' needs [44, 61, 63, 64].
Generally, it emerged that the key antecedents that influence the nature of programs to be implemented are varied. This included observing sexual rights, misconceptions, understanding what sexual health entails, and integrating different programs. Most programs are implemented due to strides made in human rights issues; there is a need that the rights of adolescents must be protected. There have been reports on the abuse of adolescents' sexual rights through forced marriages in some countries [65]. The need for integrating different systems to ensure efficiency in utilisation of resources and minimisation of duplications in adolescent sexual health programs is being implemented [65]. It has also been reported that the available resources for sustaining ASH programs and the nature of society these programs are implemented play a significant role as an antecedent that influences the formulation, implementation, and sustenance of ASH programs. It is reported that resources influence activities that must be engaged with and the nature of the programs that can be sustained. Furthermore, there is a need to consider the society that these programs are to be implemented in, as this has a bearing on the success or failure of programs in achieving intended targets [65].
Generally, they were four key attributes that were obtained from literature and found to be impacting ASH programs in different settings. It was reported that the context in which adolescents live in influences the nature of progs that must be implemented. It should also be noted that if the context is ignored, such programs are bound to fail as they will not relate or address the needs of adolescents leading to low uptake. It was also noted that the environment that we live in is dynamic. This means that there are a lot of advances in HSs, as well as different challenges that re-encountered. Therefore, interventions/programming must be a manner that is dynamic as well in response to the ever-changing needs. Thirdly, it emerged that activism and advocacy were key attributes that also influenced the nature of programs implemented. Generally, through advocacy and activism, demand is created. This then means the programs implemented must respond to the needs that would have been lobbied. This then determines the nature of programs that must respond to the identified issues. Lastly, the inefficiency of implemented programs, influences the development of other programs that were meant to cover the gap. These new programs tend to leverage the ones already implemented to come up with improved versions that then address the identified gaps.
A significant number of consequences that had resulted from the implemented programs were identified. The consequences were both positive and negative in different country settings. These were influenced by the different contextual settings that vary in different contextual settings that vary in different countries. Some of the countries, particularly those that have adequately financed HSs the outcomes were positive, while for those with weak and poorly financed HSs the outcomes were negative as this led to weak and fragmented systems being implemented. This highlighted that the impact of having sound HSs on the ASH outcomes. It was also noted that several issues drive different health systems and the resultant programs they offer to adolescents. This scenario means that not all strategies would get the desired policy changes to influence desired outcomes across different countries [44, 61, 63, 64]. Consequently, similar techniques could have further consequences (good or bad) in managing ASH issues as influenced by matters contextual to that specific population [66].
The full utilisation of Health systems depends on and is influenced by access to information. Access to helpful information ensures improved collaborative work, behaviour change, learning, knowledge management, and adaptation to local contexts [55, 66]. Arguments have erupted that discourage the safety of Indigenous Health Systems though they play an essential role in improving adolescent sexual health issues [17, 55]. Different strategies have been used in the past to aid effectiveness in Health Systems. In some health systems, electronic systems such as emails have been used as a platform for making appointments and general consultations for health system users, including adolescents [43, 67]. As a result, records management is efficient, and health care users could make an appointment or consult through electronic platforms. Adolescents are usually shy to consult on matters that relate to sexual behaviours/issues. Therefore, this electronic platform could provide a platform for information sharing as far as adolescents are concerned [42, 68].
5. LIMITATIONS OF THIS STUDY
Findings from the different articles and reports reviewed were not presented independently but collectively according to themes. This scenario could have led to biases towards themes and not the in-depth and rich findings of the reviewed articles and report study.
CONCLUSION
Adolescents are very vulnerable and need to be protected at all costs. Different contextual factors influence various policy changes, and the consequences are mixed, both positive and negative. There is a need to have comprehensive HSSs that would positively impact ASH through proposed comprehensive and integrated systems. Comprehensive HSSs would reduce their vulnerability and ensure they access HSs and utilise them in a manner that would improve their SH outcomes. Providing training, information sharing, and integrating ASH systems is critical in achieving and enhancing desired ASH outcomes.
AUTHORS' CONTRIBUTIONS
WNN was a PhD in Public Health student at the University of Venda when this research was conducted. The author conceptualised the protocol as partial fulfillment of the requirements of the PhD requirements. LM is the Supervisor of these PhD studies, while JTM and RTL are Core Supervisors. The three contributed by guiding the PhD student in conceptualising the research idea, carrying out the research, and preparing the manuscript. All authors read and approved the final manuscript.
IMPLICATIONS AND CONTRIBUTIONS
Health Systems Strategies have been vital in determining Adolescent Sexual Health outcomes. Adolescents are very vulnerable and need to be protected at all costs. There is a need to have comprehensive Health Systems Strategies that would positively impact Adolescent Sexual Health through proposed comprehensive and integrated systems.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
The research was funded by the National University of Science and Technology under the Staff Development Programme. The funder paid for tuition fees related to these PhD studies. The funder also provided resources to cover data collection, analysis and remuneration of two data collectors who assisted the principal investigator WNN. Researchers wrote and submitted six-monthly reports to appraise the funder of progress. The funder's role was to provide resources to carry out this research successfully.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


