All published articles of this journal are available on ScienceDirect.
COVID-19 Pandemic: Addressing Vaccine Hesitancy Based on Gender
Dear Editor,
One of the best cost-effective ways to prevent diseases is vaccination. The World Health Organization (WHO) has estimated that immunization currently prevents two to three million deaths annually and its widespread coverage could prevent an additional one and a half million deaths [1]. Although the epidemiological and socioeconomic benefits of immunization programs are familiar, the discussion on vaccine hesitancy has grown worldwide. Hesitancy poses a universal risk to the development made in combating vaccine-preventable diseases, becoming a central issue for immunization programs [2-4]. Vaccine hesitancy is described as a delay in acceptance or refusal of vaccination despite the availability of vaccination services [5]. In 2019, vaccine hesitancy was graded as one of the WHO's top ten threats to global health [1]. Vaccines around the world are facing hesitance for different reasons. In 2003, polio vaccine hesitancy was reported in Nigeria [6], measles vaccine hesitancy in Europe and North America [7, 8], and in 2009, the hesitancy of influenza vaccine was reported [9]. Mostly, government mistrust, fear of side effects, and misinformation are the factors responsible for vaccine hesitancy [10]. Vaccine hesitancy is an obstacle to achieving high vaccination coverage against contagious diseases. Hence, understanding its determinants is essential to help acceptability and tackle vaccine hesitancy [11].
The novel coronavirus is responsible for causing an infectious disease known as coronavirus disease 2019 (COVID-19) [12-16]. A COVID-19 vaccine is intended to provide acquired immunity against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus causing COVID-19. Unfortunately, COVID-19 vaccination programs face an extreme level of vaccine hesitancy worldwide [17, 18]. Thus, notwithstanding great efforts to achieve successful results of COVID-19 vaccines, there may be a significant obstacle to vaccine hesitation regarding approved and potential COVID-19 vaccinations [19].
A recent study has reported that the female gender has a high percentage of vaccine hesitancy, i.e., 21.0%, compared to 14.7% of the male gender [20]. Similarly, another study established that hesitancy was 19.8% and 13.2% among females and males, respectively [21]. Likewise, the mean (±SD) hesitancy was higher among women (5.08 ± 2.70) than men (4.80 ± 2.66); this was reported in a study conducted in Bangladesh [22]. Females were found six times less likely than males to get a COVID-19 vaccine. However, females were more concerned about becoming sick with coronavirus than males [23]. Women would be more likely than men to wear a mask but less likely to get a COVID-19 vaccine [23]. Nearly 7000 reports processed through the CDC's Vaccine Adverse Event Reporting System revealed that women were accounted for more than 79.0% of all reported adverse events. The most frequent side effects, such as headache, fatigue, and dizziness, were reported [24]. A study said that more side effects from a stronger reaction might contribute to vaccine hesitancy [24]. A survey revealed that women were found to be more likely than men to turn down the shots. They were incredibly anxious about long-term side effects, with nearly three-quarters being extremely or slightly concerned [25].
Signs of vaccine hesitancy among pregnant women plus those wanting to become pregnant in the future are found by doctors [26]. Pregnant people have additional concerns about how the vaccine might affect their developing fetus. Vaccine acceptance was found to be lower among pregnant women and mothers of young children in the US, Russia, and Australia [27]. Factors unique to reproductive age center on future fertility, current pregnancy, and breastfeeding [25]. Another survey found that about one-fifth (21.0%) of mothers with a dependent kid aged ≤4 admitted were scared of injection due to the possible effects of the jab on their fertility [28]. In December 2020, the first widely shared wrong report about the COVID-19 vaccines and fertility began appearing on social media. Widespread rumors, myths, and misconceptions have been circulated widely on social media, like WhatsApp, Twitter, and Facebook, that SARS-CoV-2 vaccines will result in infertility [25].
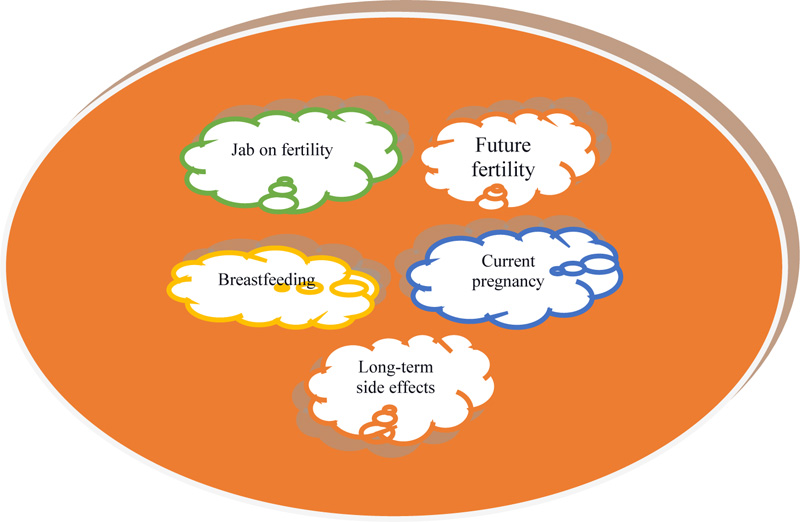
There is no evidence that COVID-19 vaccines affect women's fertility. Based on the current information, the COVID-19 vaccine is safe for pregnant women and breastfeeding mothers [28, 29]. The COVID-19 vaccines do not affect fertility, and there is no evidence reporting that getting vaccinated will injure a mother's baby or disturb someone's ability to conceive [26]. Indeed, the study revealed that COVID-19 antibodies found in mothers' breast milk could be another added advantage to protect the baby [26]. Research on historical data on vaccines revealed that there is never been an instance where a vaccine was responsible for infertility [26]. However, COVID-19 vaccine hesitancy is more common in women than men. Rumors, myths, and misconceptions on infertility are the major causes of COVID19 vaccine hesitancy among women, which implies that public health messaging needs to be informed by the growing feminist literature on the positionality, subjectivity, and situated knowledge of women in the context of personal and social change [30-33]. More studies on COVID-19 vaccination are needed to make women more confident about receiving the vaccine (Fig. 1).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


