All published articles of this journal are available on ScienceDirect.
Impact of Social Media Infodemics on Mental Health among Health Colleges’ Students at Saudi Universities during COVID-19 Pandemic
Abstract
Background:
Saudi Arabia has been severely affected by COVID-19 since March 2020. The COVID-19 “infodemic” has spread a plethora of misinformation on social media leading to public panic and serious public health consequences. We aimed to investigate the impact of social media infodemics on mental health status among health colleges’ students, as future healthcare workers, at Saudi universities during the COVID-19 pandemic.
Methods:
We used a cross-sectional web-based survey to collect data from 400 health colleges’ students. We assessed average time spent on social media and used the shortened Pittsburgh sleep quality index, generalized anxiety disorder scale, and Center for Epidemiology scale for depression to measure sleep quality, generalized anxiety disorder, and depressive symptoms. Generalized linear regression was used to determine associations with mental health burdens.
Results:
About 21.5% reported more than 3 hours/day of exposure to social media. Prevalence of poor sleep quality, anxiety, and depression disorders was 16%, 31%, and 24%, respectively. No significant difference was determined between males and females (P>0.05); however, a significant association was detected with time spent on social media (P<0.001).
Conclusion:
We found a significant mental health burden among health colleges’ students during the COVID-19 pandemic. Spending too much time on social media is a potential risk factor. Controlling social media infodemics, early mental health interventions, and continuous monitoring of consequences should become routine as part of preparedness efforts.
1. INTRODUCTION
In recent years, newly recognized or newly evolved emerging zoonotic diseases have caused considerable global health problems. Avian influenza, severe acute respiratory syndrome (SARS), swine flu, Middle East respiratory syndrome, coronavirus (MERS-CoV), and the newly recognized novel coronavirus 2019 (COVID-19) are a few examples of such diseases [1]. On December 31st, 2019, numerous cases of pneumonia of obscure cause were recognized in Wuhan, China, and reported to the WHO Nation Office. Upon investigation, a strain of coronavirus, never seen before, was found. The outbreak then crossed borders and spread around the world and was pronounced a public health emergency of worldwide concern on January 30th, and then as a worldwide pandemic on March 11th. In Saudi Arabia, the first confirmed case was announced on March 2nd, 2020, and the first case of death was announced on March 24th, 2020 [2]. The situation report published by the WHO on September 5th, 2021, confirmed over 218.9 million cases with about 4.5 million deaths globally, with the greatest prevalence reported in the Americas. There were 545,367 cases officially confirmed in Saudi Arabia, with 8,585 deaths reported with a daily increase [3].
Efforts are being made worldwide to reduce the COVID-19 pandemic. Mitigation measures, however, including lockdowns and other efforts to encourage individuals to stay home, may result in more time spent on social media and increased exposure to pandemic news or data. The massive uncontrolled information epidemic on social media has disrupted global efforts to fight against the pandemic and its related psychological consequences [4].
‘Infodemic’ refers to an excessive amount of misinformation that hinders the identification of the solution in an emergency [5]. It is emerging as one of the most virulent phenomena known to humans, able to cross international borders instantly. It was first coined to describe an information epidemic mixed with misinformation, disinformation, fake news, rumors, and conspiracies in the context of the SARS epidemic in 2003. It was defined by the WHO as an “overabundance of information – some accurate and some not – that makes it hard for people to find trustworthy sources and reliable guidance when they need it” [6].
When the demand for information is high, people usually seek information from nonreliable sources present on social media. With the enigmatic nature of COVID-19, there is an abundance of misinformation on social media that leads to public panic and has a serious public health impact. Misinformation travels rapidly across social media through videos, articles, interviews, and pictures providing false claims and repeated exposure causes people to start believing them. With the mission of enhancing reliable information and keeping people informed, authorities are fighting against the ongoing misinformation epidemics [5].
This issue was highlighted by efforts of the WHO, including identifying trusted chains that can be used as amplifiers for correct information. These include healthcare workers (HCWs) and official websites. Moreover, social media firms are working with the WHO to combat the misinformation leading to panic and psychological burden among the masses [7].
Little to no information is published regarding the challenges and consequences of infodemics among Arab student communities. In light of the aforementioned challenges and the anticipated consequences of the psychological impact of quarantine, the objective of this research was to investigate the impact of social media infodemics on mental health status (sleep quality, anxiety, and depression disorders) among health colleges’ students at Saudi universities during COVID-19 pandemic.
2. MATERIALS AND METHODS
2.1. Study Design
A cross-sectional web-based survey using snowball sampling was used to investigate the impact of social media infodemics on the mental health status (sleep quality, generalized anxiety disorder, and depressive symptoms) of health colleges’ students at Saudi universities during the COVID-19 pandemic.
2.2. Sample Size
The minimum sample size required for our study was 377 according to an apriori power analysis using the Raosoft sample size calculator based on a 95% confidence level, 5% margin of error, and an anticipated response of 50%.
2.3. Population and Inclusion Criteria
The study included undergraduate students studying at different medical and health-related colleges at Saudi governmental universities who were regular social media users (guided by time spent on social media per day).
2.4. Study Tool
A web-based questionnaire was developed for wide and rapid distribution and to avoid any social contact - while curfew and social distancing measures were being implemented - from April 15th, 2020, to June 20th, 2020. The initial draft was sent to a group of experts chosen according to their experience and expertise in the related fields to reflect on questions in terms of relativity, simplicity, and importance. The questionnaire was piloted prior to the study to identify issues like wording, question clarity, and timing and test its validity or any needed modifications. The questionnaire was finalized after a series of group discussions and the data of the pilot study was removed from the final analysis. The questionnaire included the following:
- Questions on the socio-demographics of participants.
- A question to measure the average time spent daily on social media focusing on COVID-19 pandemic information ‘<1 hour’, ‘1–3 hours’, ‘>3 hours’.
- The validated Shortened Pittsburgh Sleep Quality index (short PSQI) to assess the quality of sleep over the past month [8]. Answer options for the 9 items of the measure were on a four-point Likert scale ranging from 0-3 points ‘not during the past month’, ‘less than once a week’, ‘once or twice a week’, ‘three or more times a week’ with a score ranging from 0-27; increasing score indicates poorer quality of sleep in the last month.
- The validated Generalized Anxiety Disorder scale (GAD-7) to evaluate the frequency of anxiety symptoms over the past 2 weeks [9]. Answer options for the 7 items of the measure were on a four-point Likert scale ranging from 0-3 points ‘not at all’, ‘several days’, ‘over half the days’, ‘nearly every day’ to a score ranging from ‘0-21’; increasing score indicates increasing functional impairment as a result of anxiety over the last 2 weeks.
- The validated Center for Epidemiologic Studies Depression Scale (shortened version) (CESD-10) to assess whether participants had depressive symptoms over the past week [10]. Answer options for the 10 items of the measure were on a four-point Likert scale ranging from 0-3 points ‘rarely or none of the time’, ‘some or little of the time’, ‘occasionally or a moderate amount of time’, ‘most or all of the time’ with a score ranging from 0-30; increasing score indicates greater depressive symptoms during the past week.
The scores were added to find the mean score to measure the severity of each condition. In addition, all scores were categorized into “none, mild, moderate, or severe” based on cut-off points of 0%, 1–50%, 50–75%, or >75% of the full score for each condition, respectively. Those with moderate to severe degrees of sleep disturbance, anxiety disorders, and depression symptoms (>50% of full scores) represented the prevalence of the 3 conditions among participants.
The web-based questionnaire was distributed through the official e-learning deanships of Saudi universities as well as through personal communications between deans, heads of departments, staff, and students of health colleges. All participants were able to see and answer the questionnaire by following the relevant link.
To overcome the possibility of a low response rate, several strategies verified in research studies were implemented, including using a cover letter, clear instructions, follow-up reminders, pre-notification of the intent of the survey, simple formats, and plain design.
2.5. Statistical Analysis
Statistical analyses were carried out using SPSS version 25.0 (IBM SPSS, Armonk, NY: IBM Corp., USA). For descriptive statistics, the mean ± SD was calculated for quantitative variables, while counts and percentage were calculated for qualitative variables. In analytical statistics: Chi-square or Fisher’s exact tests were used to assess differences in frequency of qualitative variables, while Mann-Whitney or Kruskal-Wallis tests were applied for nonparametric data to assess differences in means of quantitative variables. The associations between sleep quality, anxiety, and depressive disorders with study variables were explored. Additionally, univariate & multivariate analyses were done using a generalized linear model. Statistical methods were verified, assuming a significant level of p< 0.05 and a highly significant level of p< 0.001.
3. RESULTS
The study included 400 completed questionnaires fulfilling the inclusion criteria. Participants’ ages ranged from 19-26 with a mean age of 21.56 ± 1.53 years; 45.8% were males and 54.2% were females. About one-third of the participants were living in the Makkah region (34.25%), while a minority were living in the Northern Border region (2.25%). Students of Public Health/Health Sciences constituted 43.25% of the sample. All participants were social media users. Most participants (42%) reported spending less than an hour each day seeking/reading/following information regarding the COVID-19 pandemic on social media (Table 1).
| Variables | N= 400 | % | |
|---|---|---|---|
| Age (Years) | Mean ± SD Min – Max |
21.56 ± 1.53 19 – 26 |
|
| Gender | Male | 183 | 45.8 |
| Female | 217 | 54.2 | |
| Province | Makkah | 137 | 34.25 |
| Riyadh | 74 | 18.5 | |
| Jizan | 46 | 11.5 | |
| Medina | 18 | 4.5 | |
| Tabuk | 18 | 4.5 | |
| Asir | 16 | 4.0 | |
| Ha'il | 16 | 4.0 | |
| Najran | 15 | 3.75 | |
| Eastern | 14 | 3.5 | |
| Al Jawf | 13 | 3.25 | |
| Al Qassim | 13 | 3.25 | |
| Al Baha | 11 | 2.75 | |
| Northern Border | 9 | 2.25 | |
| Faculty | Medicine | 61 | 15.25 |
| Dentistry | 34 | 8.5 | |
| Pharmacy | 52 | 13.0 | |
| Applied Medical Sciences | 41 | 10.25 | |
| Public Health / Health Sciences | 173 | 43.25 | |
| Nursing | 39 | 9.75 | |
| Time spent on social media focusing on COVID-19 pandemic every day | Less than 1 hour | 168 | 42.0 |
| 1 – 3 hours | 146 | 36.5 | |
| More than 3 hours | 86 | 21.5 | |
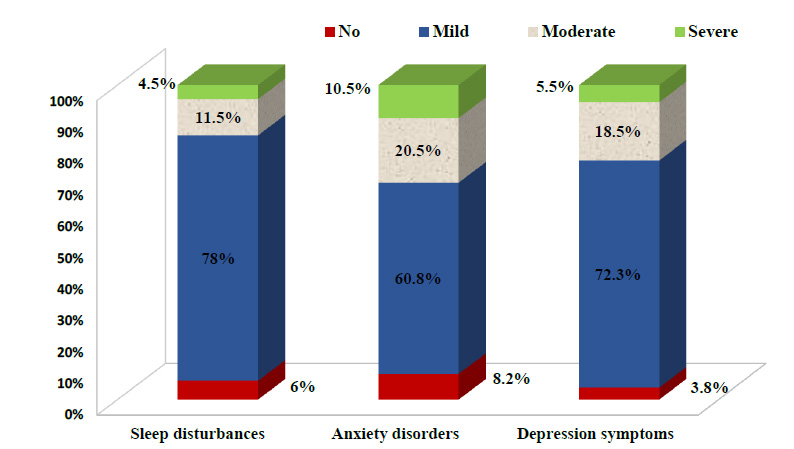
The overall mean PSQI, GAD-7, and CESD-10 scores of the sample were 8.42±5.87, 8.06±5.77, and 11.75±6.74, respectively. Only 6%, 8.2%, and 3.8% of the participants had no sleep, anxiety, or depression disorders, respectively. Prevalence of the 3 conditions were 16% (95% CI: 14.7%–17.4%), 31% (95% CI: 29.6%–32.5%), and 24% (95% CI: 22.8%–25.3%), respectively. Rates of mild, moderate, and severe degrees of sleep, anxiety, and depression disorders are illustrated in Fig. (1).
Details of different items of the PSQI, GAD-7, and CESD-10 scores are summarized in Table 2.
| Short PSQI | Not During Past Month | Less than once a Week |
1–2 Times a Week |
> 3 Times a Week |
|---|---|---|---|---|
| Cannot get to sleep within 30 minutes | 73 (18.25) | 110 (27.5) | 90 (22.5) | 127 (31.75) |
| Wake up in the middle of the night or early morning | 92 (23.0) | 75 (18.75) | 89 (22.25) | 144 (36.0) |
| Cannot breathe comfortably | 242 (60.5) | 80 (20.0) | 48 (12.0) | 30 (7.5) |
| Cough or snore loudly | 274 (68.5) | 70 (17.5) | 27 (6.75) | 29 (7.25) |
| Feel too hot | 280 (70.0) | 61 (15.25) | 38 (9.5) | 21 (5.25) |
| Have bad dreams | 205 (51.25) | 121 (30.25) | 47 (11.75) | 27 (6.75) |
| Have pain | 225 (56.25) | 95 (23.75) | 49 (12.25) | 31 (7.75) |
| Trouble staying awake | 224 (56.0) | 92 (23.0) | 45 (11.25) | 39 (9.75) |
| Problem affects enthusiasm to get things done | 150 (37.5) | 110 (27.5) | 76 (19.0) | 64 (16.0) |
| GAD-7 | Not at all | Several Days | Over Half the Days |
Nearly Every Day |
| Feeling nervous, anxious, or on edge | 75 (18.75) | 166 (41.5) | 91 (22.75) | 68 (17.0) |
| Not being able to stop or control worrying | 139 (34.75) | 158 (39.5) | 60 (15.0) | 43 (10.75) |
| Worrying too much about different things | 104 (26.0) | 139 (34.75) | 76 (19.0) | 81 (20.25) |
| Trouble relaxing | 99 (24.75) | 167 (41.75) | 72 (18.0) | 62 (15.5) |
| Being so restless that it's hard to sit still | 200 (50.0) | 129 (32.25) | 42 (10.5) | 29 (7.25) |
| Becoming easily annoyed or irritable | 71 (17.75) | 168 (42.0) | 75 (18.75) | 86 (21.5) |
| Feeling afraid as if something awful might happen | 174 (43.5) | 133 (33.25) | 53 (13.25) | 40 (10.0) |
| CESD-10 | < 1 Day | 1–2 Days | 3–4 Days | 5–7 Days |
| I was bothered by things that usually don’t bother me | 174 (43.5) | 133 (33.25) | 57 (14.25) | 36 (9.0) |
| I had trouble keeping my mind on what I was doing | 173 (43.25) | 116 (29.0) | 67 (16.75) | 44 (11.0) |
| I felt depressed | 143 (35.75) | 138 (34.5) | 75 (18.75) | 44 (11.0) |
| I felt that everything I did was an effort | 135 (33.75) | 133 (33.25) | 68 (17.0) | 64 (16.0) |
| I felt hopeful about future | 66 (16.5) | 119 (29.75) | 88 (22.0) | 127 (31.75) |
| I felt fearful | 141 (35.25) | 161 (40.25) | 49 (12.25) | 49 (12.25) |
| My sleep was restless | 128 (32.0) | 141 (35.25) | 71 (17.75) | 60 (15.0) |
| I was happy | 39 (9.75) | 164 (41.0) | 121 (30.25) | 76 (19.0) |
| I felt lonely | 157 (39.25) | 113 (28.25) | 66 (16.5) | 64 (16.0) |
| I could not “get going” | 134 (33.5) | 134 (33.5) | 64 (16.0) | 68 (17.0) |
| Variables |
Short PSQI Score (max.=27) |
GAD-7 Score (max.=21) | CESD-10 Score (max.=30) | |
|---|---|---|---|---|
| Gender | Male | 7.89±4.5 | 7.63±6.31 | 11.67±8.12 |
| Female | 9.04±7.12 | 8.43±5.26 | 11.82±5.32 | |
| P-value1 | 0.107 | 0.268 | 0.832 | |
| Time Spent on Social Media | <1 hour | 6.51±4.14 | 6.73±5.23 | 10.33±5.95 |
| 1-3 hours | 8.11±4.21 | 7.79±4.67 | 9.99±4.59 | |
| >3 hours | 10.98±7.31 | 9.88±6.42 | 14.38±7.7 | |
| P-value2 | < 0.001* | < 0.001* | < 0.001* | |
| Variables | Short PSQI | GAD-7 | CESD-10 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Prev. % |
OR (95%CI) |
AOR (95%CI) |
Prev. % |
OR (95%CI) |
AOR (95%CI) |
Prev. % |
OR (95%CI) |
AOR (95%CI) |
||
| Gender1 | Male | 14.0 | 1.0 (ref) | 1.0 (ref) | 28.4 | 1.0 (ref) | 1.0 (ref) | 22.1 | 1.0 (ref) | 1.0 (ref) |
| Female | 18.8 | 1.28 (0.92-1.64) |
1.22 (0.84-1.60) |
33.2 | 1.30 (0.81-1.95) |
1.25 (0.79-2.01) |
26.2 | 0.94 (0.56-1.48) |
0.85 (0.52-1.31) |
|
| Time Spent on Social Media2 * | <1 hour | 6.5 | 1.0 (ref) | 1.0 (ref) | 22.8 | 1.0 (ref) | 1.0 (ref) | 20.7 | 1.0 (ref) | 1.0 (ref) |
| 1-3 hours | 8.6 | 1.14 (0.74-1.46) |
1.09 (0.69-1.38) |
27.1 | 1.26 (0.94-1.67) |
1.19 (0.81-1.56) |
7.1 | 1.75 # (1.38-2.09) |
1.60 # (1.28-1.98) |
|
| >3 hours | 31.5 | 2.27 * (1.74-2.81) |
2.06 * (1.80-2.76) |
43.2 | 2.41 * (1.99-2.83) |
2.26 * (1.83-2.75) |
36.3 | 2.01 * (1.71-2.55) |
1.88 * (1.54-2.26) |
|
CI: Confidence interval. 1: Fisher’s exact test. 2: Chi-square test.
*: Significant (P-value <0.001). #: Significant (P-value <0.05).
The prevalence of the 3 measured disorders was stratified by gender and social media exposure, and their relations are described in Tables 3 and 4. No gender differences were detected (P>0.05); however, all 3 scores were found to be significantly associated with time spent on social media (P<0.001), where higher scores were found among those who spent >3 hours reading about COVID on social media. Multivariate analyses found that the adjusted odds of the 3 conditions were greater among those who spent >3 hours on social media compared with <1 hour after controlling for all covariates (P<0.001).
4. DISCUSSION
The announcement of COVID-19 as a pandemic and its rapid global spread leads many countries, including Saudi Arabia, to activate strict measures to prevent its further spread. These measures led to panic among the population and contributed to mental stress and worry. This was exacerbated by misinformation and myths that were rampant on social media [11]. To the best of our knowledge, this is the examining social media-related mental and psychological burden during the COVID-19 pandemic among future HCWs in Saudi universities.
Our study revealed that the prevalence of poor sleep quality was 16% among participants. This is lower than that reported during the COVID-19 pandemic among HCWs in China (23.6%) [12] but much higher than that reported by Anzar et al. in Pakistan (6.9%). Students exhibited poorer symptoms compared to HCWs and other professions, which may be attributed to more panic due to young age and less experience [13].
The prevalence of anxiety disorders in our study was 31%, similar to that reported during the COVID-19 pandemic in Pakistan [13]. This rate, however, is higher than among the public in Iran (19.1%) [14] and China (23.8%) [15], as well as among HCWs in China (21.1%) [15] and in India (8.7%) [16]. The prevalence of anxiety disorders in our study was lower than that reported among the general population in Saudi Arabia (24%) [17], Iraqi Kurdistan (38.7%) [18], and among HCWs in Riyadh, Saudi Arabia (41.4%) [19].
The prevalence of depression among Saudi medical students has been documented to be high (28.3%–67.4%), representing a hidden problem [20]. Nearly one in four participants in our study had depression symptoms (24%). Our results were higher than that reported during the COVID-19 pandemic among the public in Spain [21] and Pakistan [13] (9.9% and 13.9%, respectively) and among Chinese HCWs in Wuhan (19.2%) [15], but lower than the general population in Saudi Arabia (28.3%) [17].
The differences in prevalence may be explained by the differences in status and progression of the pandemic in each country. Additionally, strict governmental measures may induce a higher prevalence of mental health challenges that may exacerbate isolation, panic, and associated consequences. Our participants, as students, may be more prone to panic due to their young age and less experience in life compared to other demographics [12]. In addition, given our sample was comprised of future HCWs, the pandemic may have highlighted the potential for high working intensity and not enough time to rest, making them susceptible to chronic stress and a more pronounced psychological burden [22].
There was no significant difference between male and female participants regarding the 3 mental health issues measured. This finding was in line with those of Huang and Zhao in their study among the Chinese population during the COVID-19 epidemic [12]. Other studies, however, found more mental health problems among females in Saudi Arabia [17], Pakistan [13], and China [23]. This may be attributed to the fact that females, compared to males, tend to be more anxious towards emergencies and have emotional responses. Saudi females, compared to males, experience less interaction and socialization. Educational policies separate campuses for male and female students with relatively poorer learning environments, educational facilities, and recreational opportunities for females, increasing their stress and depression [24]. The different lived experiences between males and females in Saudi Arabia during the pandemic require further investigation.
The literature confirms our findings that public mental health problems are linked to exposure to public health emergencies, in particular major infectious diseases and major population events. Reports from previous research highlight the mental and psychological burden among HCWs and/or the public during the SARS outbreaks [25], Swine flu (influenza A H1N1) outbreak [26], Ebola outbreak [27], MERS-CoV epidemic [28], and current COVID-19 pandemic [11, 17, 19].
Numerous studies have examined the psychology behind the responses to and consequences of disasters and devastation. The psychological typhoon eye effect, for example, is a paradoxical phenomenon in which respondents closer to the center of the pandemic appear to have lower levels of concern about imminent risk [29]. This, however, is not consistent with our findings among students affiliated with health colleges. This may be attributed to the uncertainty regarding educational processes after closing campuses as well as the unpredictability of the course and progression of the COVID-19 pandemic. Furthermore, increased psychological load and mental health strain on the population, particularly future HCWs, which may be connected to “hypochondriac worries,” fear of contamination, and fear/anticipation regarding the containment of the pandemic [30].
Social media is one of the main sources updating the public on COVID-19 information. It is also used in mobilizing the community, providing telemedicine, and online psychological counseling [11]. Social media platforms, however, may also amplify the perception of risk, spread negative emotions, “emotional contagion”, rumors, and fake news during a pandemic [31]. We found that participants who spent more time (>3 hours) on social media each day focusing on the COVID-19 pandemic were more likely to suffer mental problems. This may be related to the body’s normal defensive reaction to stress caused by the pandemic and the assumption that individual perceptual bias could lead to insufficient or excessive information seeking, resulting in collective perceptual biases [32]. In addition, many people express their feelings towards the pandemic on social media, and many netizens, as a result, are exposed to unfounded fears from the flow of misinformation on social media [31].
Neria and Sullivan found that mental health effects may result from indirect exposure to mass trauma through the media [33]. Disaster coverage through social media is found to be associated with adverse psychological outcomes [34]. Chao et al. suggested bidirectional links between mental health outcomes and social media exposure that possibly increases subsequent negative mental outcomes, which in turn advances expanded social media utilization as the spread of the pandemic proceeds [35]. Recent studies found that time spent cantered on COVID-19 on social media may be potentially hazardous for the psychological and mental health of the public [12, 13, 15, 18, 35]. Other studies, however, did not confirm a significant association [20].
In Saudi Arabia, the government has taken strict orchestrated national measures to mitigate the further spread of COVID-19. Health authorities launched a positivist initiative to relieve psychological burdens and mental stress among current HCWs. There is still a lack of similar interventions, however, targeting the general population, including future HCWs, as a potentially vulnerable group. Harnessing social media and combating infodemics through promoting trusted official information to neutralize the possible adverse impacts of other shapes of media sharing and filtering out false information may be relevant interventions as part of COVID-19 pandemic preparedness efforts.
5. LIMITATIONS
It is imperative to decipher our results in the context of potential study limitations. The cross-sectional nature of the study does not allow the interpretation of causality. The use of web-based surveys may lead to selection bias and limits the generalizability of the results of our study. Additionally, the previous mental and psychological status of participants could not be assessed before the outbreak, so we cannot exclude the preexisting effect. There was also an oversampling of particular regions (e.g., Makkah province), and participation from other provinces was low. In addition, future HCWs in private colleges were not included. We also relied on self-reported data, which may have resulted in recall bias or social desirability bias. Possible exposure to COVID-19 cases or close contact may have exacerbated levels of anxiety, and we did not control this potential variable. We also did not control mental wellbeing conditions and social media utilized behaviors before the outbreak, and we were unable to monitor potential mental health changes over time. Finally, the possibility of residual confounding caused by unmeasured covariates can not be excluded. We intend to reevaluate our participants if the present pandemic persists in the country, as well as after it is subsided, in order to acquire reliable explanations investigating the association between mental health conditions and social media infodemics.Despite the limitations, our results are consistent with previous studies illustrating the association between infodemics and mental health, highlighting potential areas of intervention.
CONCLUSION
The mental health burden among future HCWs during the COVID-19 pandemic is a major concern. Spending too much time on social media focusing on consuming COVID-19 pandemic information is a potential risk factor. We recommend early targeted psychological support, mental health interventions, and controlling social media infodemics. Subsequently, continuous surveillance and monitoring of the mental health burden of pandemics and similar catastrophes should become routine as an integral component of preparedness. In addition, universities should include designed courses to help students search for and evaluate health information.
AUTHORS’ CONTRIBUTION
M.O.N.: Conceptualization, methodology, software, data curation, project administration, original draft preparation, validation, visualization, supervision, reviewing, and editing. T.H.S.: Conception and design of the study, software, interpretation of data, validation, drafting the article, reviewing, and editing. H.A.N.: Conception and study design, visualization, interpretation of data, reviewing, and editing. All authors have read and approved the final version to be submitted.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Local Committee for Bioethics and Medical Ethics at Umm Al-Qura University (No.# PBIM010520). Electronic informed consent from anonymous participants was obtained on the initial page before beginning the online survey with emphasis on their voluntary participation and permission to withdraw at any time without justification.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from the participants.
STANDARDS OF REPORTING
STROBE guidelines and methodologies were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available from the corresponding author upon reasonable request. In addition, the questionnaire can be found at the following link:
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We would like to thank the official e-learning deanship of Saudi universities as well as the deans, heads of departments, staff, and students at health colleges at Umm Al-Qura University and other Saudi universities for their help and cooperation.


