All published articles of this journal are available on ScienceDirect.
Factors Influencing Healthcare Workers’ Perception of South African Health System Capability for Managing COVID-19 Pandemic
Abstract
Background:
During the emergence of the COVID-19 pandemic in South Africa in March 2020, there was an urgent mobilization of healthcare workers (HCWs) who had to adapt quickly to a challenging health system. Therefore, this paper examines factors associated with HCWs’ perceptions of the South African health system’s capability for managing COVID-19 during the early stages of the pandemic.
Methods:
Data utilised in this paper were obtained from an online survey conducted among HCWs using a structured questionnaire on a data-free online platform. The study population included all HCWs in South Africa. Bivariate and multivariate logistic regression models were used to examine the factors influencing HCWs’ perceptions of the South African health system capability for managing COVID-19.
Results:
Of the 5,274 respondents, 22.0% indicated that the South African health system would manage the COVID-19 pandemic. Increased odds of perceiving that the South African health system was capable of managing COVID-19 were significantly associated with being male (aOR = 1.55 95%CI [1.22-1.97], p<0.001), being 50-59 years old (aOR = 1.94 [1.31-2.87], p=0.001) and 60 years and older (aOR = 2.27 [1.34-3.84], p=0.002), working in other sector (aOR = 1.42 [1.10-1.84], p=0.007), and having confidence in their overall knowledge about COVID-19 (aOR = 1.92 [1.52-2.41], p<0.001). Decreased odds of perceiving that the South African health system was capable of managing COVID-19 were significantly associated with HCWs being White (aOR = 0.29 [0.22-0.38], p<0.001) and Indian/Asian (aOR = 0.45 [0.33-0.62], p<0.001), being medical practitioner (aOR = 0.55 [0.41-0.73], p<0.001), and having moderate (aOR = 0.70 [0.50-0.99], p=0.042) or high risk perceptions (aOR = 0.55 [0.39-0.77], p<0.001) of contracting COVID-19.
Conclusion:
In the early days of the pandemic, most HCWs felt that the health system would not cope with COVID-19. Healthcare workers’ experience (a proxy for HCWs’ age), work sector, confidence in their knowledge about COVID-19, and their risk perceptions were key factors affecting their perception of the health system’s capability.
1. BACKGROUND
The reports of the novel coronavirus from Wuhan, China, in December 2019 immediately presented health systems around the world with new challenges [1-3]. The challenges brought by the emergence of the COVID-19 pandemic were unprecedented, and most countries’ health systems were stretched beyond capacity, even among the richer nations. It was evident from the onset that health systems would be stretched to capacity due to the rapid number of infected people requiring hospitalization [4]. The impact of this new virus on healthcare delivery can be broadly categorised into two categories; firstly, the impact on the infrastructure of the health systems defined by the structural, contextual material resources, excluding people, and secondly, the impact on the HCWs.
For some of the most affected countries (e.g., USA), the COVID-19 pandemic highlighted significant gaps in their private and public healthcare service provision. In the USA, the demand for increased acute care in some primary centres threatened long-term viability with crippling financial losses. Furthermore, the pandemic disproportionately impacted the Black and Hispanic communities, who had more cases and deaths even though they constituted only 13% and 18% of the total population, respectively [5]. Similar to the USA, in European countries worst hit by the pandemic, such as Italy, France, Spain, and the United Kingdom, inherent gaps in their health systems were exposed by the COVID-19 pandemic. The largely decentralised public health systems of Italy and Spain found it extremely difficult to coordinate activities in certain regions [6, 7]. More than the inability to streamline healthcare provision to those who needed it, several European health systems also suffered a shortage of personal protective equipment (PPE) and intensive care equipment [8, 9]. These challenges hampered HCWs’ ability to provide adequate patient care.
The pandemic has highlighted the need to enhance health systems' capacity to provide improved and cost-effective healthcare to all sectors of the population. Health systems need to build resilience for future COVID-19 pandemic waves [10]. The South African health system has dealt with a quadruple disease burden for decades [11]. This is likely to be compounded by the COVID-19 pandemic, and maintaining routine healthcare services requires a balance to be struck by a resilient health system. However, in South Africa, there are numerous strains on the health system due to COVID-19, with HCW capacity being overstretched and unable to function effectively [12].
Previous studies report that HCWs are likely to experience increased psychological distress, general anxiety about personally getting infected, and anxiety about the risk of infecting their families and friends [13]. With the progression of the pandemic, burnout became widespread among HCWs as they were unable to take time off due to the overburdened health systems [14]. It became increasingly evident that health facilities and health systems in several countries were unable to cope and adapt. In certain instances, HCWs were redeployed to where they were most needed but did not receive adequate training in their new roles [15]. Perceptions of HCWs about the health system are influenced by these structural and contextual factors as well as the more personal attitudinal motivations [16]. Additionally, factors such as long working hours in the public sector, absence of appraisals of recognition for employees who work hard [17], staff shortages, poor working conditions [18], lack of adequate training, poor communication and hierarchical relationships also have an impact on how HCWs view the health system [16, 19, 20].
The South African experience was similar to the rest of the world, wherein there was an urgent mobilization of HCWs who had to absorb rapidly developing scientific and public health information, adapt and immediately action this information in constrained health facilities [21]. Despite these interventions, South Africa has to date the highest number of COVID-19 cases and deaths in Africa. To maintain essential and optimal health services during a pandemic, it is important that the HCWs’ wellbeing and emotional resilience are not negatively impacted.
Perceiving the health system as being able to manage the pandemic can be viewed as a proxy for optimism and confidence in the collective efficacy of the national health system. The beliefs of a group of people in their collective efficacy impact their function as a whole [22]. The optimism of HCWs is interlinked with resilience and self-efficacy. It is also associated with seeking social support, finding practical solutions, higher performance, and improved patient satisfaction, and during crisis situations, optimism can lead to improved morbidity outcomes [22]. This paper, therefore, examines factors associated with HCWs’ perception of the South African health system’s capability for managing COVID-19 in the early stages of the pandemic.
2. METHODS
2.1. Data
Data utilised in this paper were obtained from a large-scale national online survey conducted among HCWs using a structured questionnaire on a data-free online platform. The survey was conducted from April 11th to May 7th, 2020. The study population was all HCWs aged 18 years and older in South Africa. More details about how the data were collected have been provided elsewhere [23].
2.2. Measures
The primary outcome variable was HCWs’ perception of South African health system's capability for managing COVID-19, which was based on the question, “Do you feel that South African Health System is able to cope with the COVID-19 outbreak?” with response options being 1=yes, 2=no and 3=don’t know. These responses were further dichotomised into 1=yes and 0=no (no and don’t know). Explanatory variables included socio-demographic variables: sex (male or female), age in years (18-29, 30-39, 40-49, 50-59, 60 and older), population group (Black African, Coloured, White, Indian/Asian, Other), education level (diploma(s)/occupational certificate(s), bachelor’s degree, honours/post-graduate diploma, master’s degree, specialist qualification, doctorate), professional category (medical practitioner, nurse practitioner, other healthcare workers), public sector (yes or no), private sector (yes or no), other sectors (yes or no), and locality for work (urban formal areas, urban informal areas, rural areas). Other variables included risk perception for contracting COVID-19, confidence in overall knowledge about COVID-19, and having treated COVID-19 patients. Risk perception of contracting COVID-19 was assessed by the question: “How would you rate your personal risk of contracting COVID-19 in the workplace?” with response options being 1=extremely high risk, 2=high risk, 3=moderate risk, 4=low risk and 5= very low risk. The responses were recoded into 1=low risk (very low risk, and low risk), 2=moderate risk and 3=high risk (extremely high risk and high risk). Confidence in overall knowledge about COVID-19 was assessed by the question, “Do you feel confident in your overall knowledge about COVID-19?” with response options being 1=yes, 2=no and 3=unsure. These were categorised into a dichotomised primary outcome with 1=yes and 0=no (no and unsure). Having treated COVID-19 patients was assessed by the question “Have you treated/provided care for a patient diagnosed with COVID-19?” with binary responses of yes or no. The explanatory variables investigated were informed by the literature on socio-behavioural factors influencing perceptions of health system capability among the general public and healthcare workers [23, 24]. In light of these literature sources, we posited that sociodemographic variables, such as age, education and professional work sector, may be associated with other explanatory variables as well as health system capability. These variables were therefore included in the regression models to adjust for their potential confounding effects.
2.3. Statistical Analysis
The “svy” command in Stata version 15.0 [25] was used to incorporate benchmarking weights into the analysis. Other studies have shown that re-weighted online samples can produce response patterns that are statistically similar to population characteristics [23, 26]. Demographic distribution of the weighted analytic sample and the estimated sample frame was undertaken by Manyaapelo et al. [23], and the difference between the two samples was not substantial. The survey data were benchmarked to the distribution of South Africa’s HCWs population by age, sex, population group and province to allow generalizability to the national population of HCWs. The total South African HCWs population across professional categories and demographics was compiled using data sources from the Health Professions Council of South Africa (HPCSA) and the South African Nursing Council (SANC), as there was no pre-existing database of all HCWs in the country. Benchmarking was aimed at both correcting for potential bias that may result due to the online participation and ensuring that the perceptions of overrepresented sectors of the HCWs are scaled downwards and those of less represented are illuminated. Details on benchmarking and sample selection are described elsewhere [23]. Differences in HCWs’ perception of health system capability for managing COVID-19 across the socio-demographic variables were compared using 95% confidence intervals (CIs) and Chi-square tests. Factors influencing HCWs’ perception of health system capability for managing COVID-19 were assessed using bivariate and multivariate logistic regression. All statistically significant variables from the bivariate logistic regression models were entered into the multivariate logistic regression. For statistical significance, p < 0.05 was considered. Statistical literature has often highlighted the shortcomings of stepwise multiple regression, including bias in parameter estimation [27]. The selection criterion of removing variables that are insignificant at 5% is consistent with the literature, and was therefore applied in this article.
3. RESULTS
3.1. Demographics of the Study Sample
The study sample comprised 5274 HCWs (Table 1). After benchmarking, females constituted 76.9% and Black Africans accounted for 57.5% of the HCWs. Around 28% were 30-39 years old, 31.2% had a Bachelor’s degree, and 35.8% were nurse practitioners. About half of HCWs (50.1%) worked in the public sector, and 61.5% worked in urban formal areas.
| Sample | % | [95% CI] | |
|---|---|---|---|
| Total | 5 274 | 100.0 | |
| Sex | |||
| Female | 3 696 | 76.9 | [75.4-78.4] |
| Male | 1 554 | 23.1 | [21.6-24.6] |
| Population group | |||
| Black African | 1 108 | 57.5 | [55.7-59.4] |
| White | 2 710 | 23.2 | [22.1-24.4] |
| Coloured | 507 | 12.6 | [11.4-13.8] |
| Indian/Asian | 628 | 5.6 | [5.1-6.1] |
| Other | 321 | 1.1 | [0.9-1.2] |
| Age group | |||
| 18-29 | 862 | 17.8 | [16.3-19.5] |
| 30-39 | 1 568 | 28.2 | [26.5-30.0] |
| 40-49 | 1 363 | 24.2 | [22.5-25.9] |
| 50-59 | 893 | 17.9 | [16.3-19.6] |
| 60+ | 588 | 11.9 | [10.5-13.5] |
| Education level | |||
| Diploma(s)/Occupational certificate(s) | 920 | 22.8 | [21.1-24.5] |
| Bachelor's degree | 1 567 | 31.2 | [29.3-33.2] |
| Honours /Post Graduate Diploma | 958 | 16.8 | [15.4-18.4] |
| Master's degree | 787 | 13.1 | [11.8-14.6] |
| Specialist qualification | 825 | 12.4 | [11.2-13.7] |
| Doctorate | 217 | 3.7 | [2.9-4.6] |
| Professional category | |||
| Nurse practitioner | 1 170 | 35.8 | [33.8-37.9] |
| Medical practitioner | 2 124 | 30.6 | [28.8-32.4] |
| Other healthcare worker | 1 980 | 33.6 | [31.8-35.5] |
| Public sector1 | |||
| No | 3 250 | 49.9 | [47.9-52.0] |
| Yes | 2 022 | 50.1 | [48.0-52.1] |
| Private sector1 | |||
| No | 2 934 | 68.0 | [66.2-69.7] |
| Yes | 2 338 | 32.0 | [30.3-33.8] |
| Other sector1 | |||
| No | 3 719 | 71.0 | [69.1-72.8] |
| Yes | 1 553 | 29.0 | [27.2-30.9] |
| Locality for work | |||
| Urban formal areas | 3 872 | 61.5 | [59.4-63.6] |
| Urban informal areas | 852 | 22.3 | [20.6-24.2] |
| Rural areas | 523 | 16.2 | [14.5-18.0] |
1. Groups are not mutually exclusive. An HCW could work in multiple sectors.
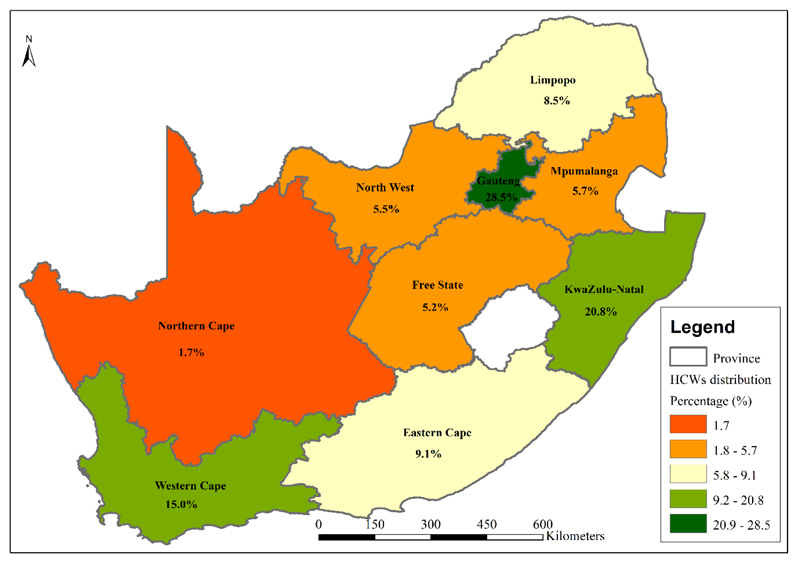
Gauteng and KwaZulu-Natal provinces contributed the largest proportions of HCWs who participated in the survey (28.5% and 20.8%) (Fig. 1).
3.2. Healthcare Workers’ Perception of Health System Capability for Managing COVID-19
About a fifth (22.0%) of HCWs indicated the South African health system to have the ability to manage the COVID-19 pandemic (Table 2). This perception was higher among male HCWs (27.3%), HCWs identified as Black African (26.1%), those aged 50-59 years old (27.4%), those with doctorate degrees (32.3%), and HCWs who had confidence in their knowledge about COVID-19 (59.2%) than their relevant counterparts. The perception that the health system was capable of managing COVID-19 was significantly lower among HCWs who treated COVID-19 patients (17.5%) than those who did not (Fig. 2).
Table 2.
| Total | Sample | % | [95% CI] | p-value |
|---|---|---|---|---|
| 5 274 | 22.0 | [20.3-23.9] | ||
| Sex | ||||
| Female | 3 696 | 20.4 | [18.4-22.6] | <0.001 |
| Male | 1 554 | 27.3 | [24.2-30.7] | |
| Population group | ||||
| Black African | 1 108 | 26.1 | [23.3-29.1] | <0.001 |
| White | 2 710 | 13.3 | [11.9-14.8] | |
| Coloured | 507 | 23.4 | [19.6-27.6] | |
| Indian/Asian | 628 | 14.3 | [11.6-17.6] | |
| Other | 321 | 15.5 | [11.2-21.1] | |
| Age group | ||||
| 18-29 | 862 | 17.8 | [14.3-21.9] | 0.007 |
| 30-39 | 1 568 | 19.7 | [17.1-22.7] | |
| 40-49 | 1 363 | 21.5 | [18.4-25.0] | |
| 50-59 | 893 | 27.4 | [22.9-32.5] | |
| 60+ | 588 | 26.7 | [20.4-34.0] | |
| Education level | ||||
| Diploma(s)/Occupational certificate(s) | 920 | 22.9 | [19.6-26.7] | 0.003 |
| Bachelor's degree | 1 567 | 19.4 | [16.4-22.8] | |
| Honours /Post Graduate Diploma | 958 | 23.5 | [19.4-28.3] | |
| Master's degree | 787 | 27.6 | [22.5-33.3] | |
| Specialist qualification | 825 | 15.8 | [12.4-20.0] | |
| Doctorate | 217 | 32.3 | [21.7-45.2] | |
| Professional category | ||||
| Nurse practitioner | 1 170 | 24.7 | [21.4-28.4] | <0.001 |
| Medical practitioner | 2 124 | 15.6 | [13.3-18.1] | |
| Other healthcare worker | 1 980 | 25.0 | [22.1-28.1] | |
| Public sector | ||||
| No | 3 250 | 23.5 | [21.1-26.2] | 0.098 |
| Yes | 2 022 | 20.5 | [18.1-23.1] | |
| Private sector | ||||
| No | 2 934 | 24.1 | [21.9-26.5] | <0.001 |
| Yes | 2 338 | 17.6 | [15.2-20.3] | |
| Other sector | ||||
| No | 3 719 | 19 | [17.1-21.1] | <0.001 |
| Yes | 1 553 | 29.4 | [25.8-33.3] | |
| Locality for work | ||||
| Urban formal areas | 3 872 | 22.8 | [20.7-25.1] | 0.44 |
| Urban informal areas | 852 | 19.9 | [16.2-24.1] | |
| Rural areas | 523 | 21.2 | [16.8-26.4] | |
| Risk perception for contracting COVID-19 | ||||
| Low | 798 | 30.4 | [25.2-36.2] | 0.001 |
| Moderate | 1 741 | 23.1 | [20.0-26.4] | |
| High | 2 735 | 20.0 | [17.8-22.4] | |
| Confidence in knowledge about COVID-19 | ||||
| No | 2 378 | 17.5 | [15.1-20.1] | <0.001 |
| Yes | 2 855 | 27.0 | [24.5-29.6] | |
| Treated COVID-19 patient | ||||
| No | 4 480 | 22.8 | [20.9-24.8] | 0.031 |
| Yes | 772 | 17.5 | [13.8-21.9] |
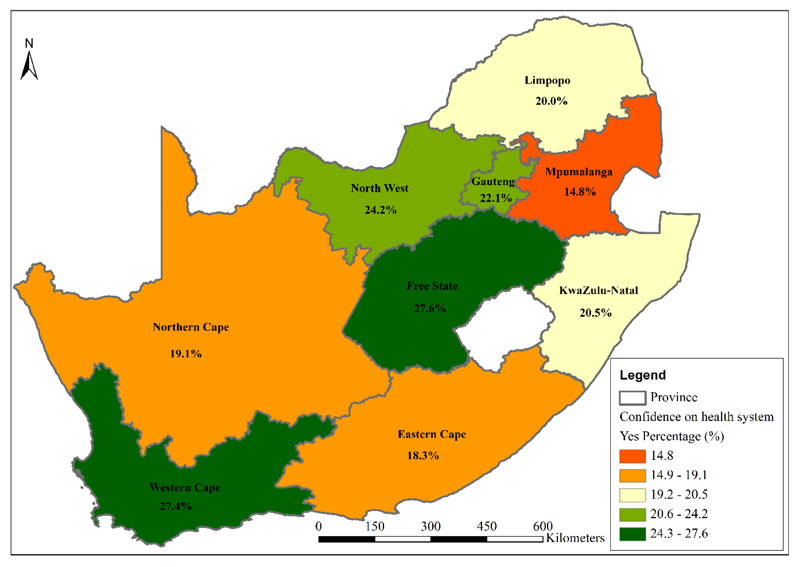
The perception that the health system would manage COVID-19 was highest in the Free State (27.6%) and Western Cape (27.4%) and lowest in Mpumalanga (14.8%).
3.3. Factors Influencing HCWs’ Perception of Health System’s Capability for Managing COVID-19
Increased odds of perceiving that the South African health system would manage COVID-19 were found among HCWs who were male (aOR = 1.55 95%CI [1.22-1.97], p<0.001), aged 50-59 years old and 60 years and older (aOR = 1.94 [1.31-2.87], p=0.001; aOR = 2.27 [1.34-3.84], p=0.002 relative to 18-29 years), working in a sector other than private or public (aOR = 1.42 [1.10-1.84], p=0.007), and those who had confidence in their overall knowledge about COVID-19 (aOR = 1.92 [1.52-2.41], p<0.001). Decreased odds of perceiving that the health system would manage COVID-19 were found among HCWs who were White and Indian/Asian (aOR = 0.29 [0.22-0.38], p<0.001; aOR = 0.45 [0.33-0.62], p<0.001, respectively, relative to Black African), were medical practitioners (aOR = 0.55 [0.41-0.73], p<0.001), and had moderate (aOR = 0.70 [0.50-0.99], p=0.042) or high risk perceptions of contracting COVID-19 (aOR = 0.55 [0.39-0.77], p<0.001, respectively, relative to low risk perceptions (Table 3).
| aOR | [95% CI] | p value | |
|---|---|---|---|
| Sex | |||
| Female (Ref) | |||
| Male | 1.55 | [1.22-1.97] | <0.001 |
| Population group | |||
| Black African (Ref) | |||
| White | 0.29 | [0.22-0.38] | <0.001 |
| Coloured | 0.80 | [0.60-1.07] | 0.127 |
| Indian/Asian | 0.45 | [0.33-0.62] | <0.001 |
| Other | 0.41 | [0.26-0.66] | <0.001 |
| Age group | |||
| 18-29 (Ref) | |||
| 30-39 | 1.15 | [0.82-1.60] | 0.418 |
| 40-49 | 1.31 | [0.92-1.86] | 0.132 |
| 50-59 | 1.94 | [1.31-2.87] | 0.001 |
| 60+ | 2.27 | [1.34-3.84] | 0.002 |
| Professional category | |||
| Nurse practitioner (Ref) | |||
| Medical practitioner | 0.55 | [0.41-0.73] | <0.001 |
| Other healthcare worker | 1.13 | [0.84-1.50] | 0.417 |
| Private sector | |||
| No (Ref) | |||
| Yes | 0.88 | [0.68-1.14] | 0.329 |
| Other sector | |||
| No (Ref) | |||
| Yes | 1.42 | [1.10-1.84] | 0.007 |
| Risk perception | |||
| Low (Ref) | |||
| Moderate | 0.70 | [0.50-0.99] | 0.042 |
| High | 0.55 | [0.39-0.77] | 0.001 |
| Confidence in overall knowledge about COVID-19 | |||
| No (Ref) | |||
| Yes | 1.92 | [1.52-2.41] | <0.001 |
| Treated COVID-19 patient | |||
| No (Ref) | |||
| Yes | 0.83 | [0.60-1.14] | 0.247 |
4. DISCUSSION
This study found that approximately one-fifth (22.0%) of HCWs believed that the South African health system has the ability to manage the COVID-19 pandemic. When the same question was asked to South African residents in another study, two in five (40.7%) indicated that the country’s health system was able to manage the COVID-19 pandemic [24]. Healthcare workers’ positive views of the health system’s capability can reflect optimism or confidence in the collective efficacy of the national health system.
A study in Romania Sava [28] found low HCWs’ confidence (24.0%) in the health system to manage the pandemic, while Finland, Norway and Denmark reported high HCWs’ confidence (78.0%; 56% and 86.0%, respectively) in their health systems [29-31], thereby indicative of the disparate viewpoints between countries with different health systems and economies. In this study, low confidence in the health system’s response to the epidemic might be due to low trust in HCWs themselves or in their peers or possibly a lack of resilience to face workplace challenges or epidemic response in general [32]. Resilience, self-efficacy and coping strategies, therefore, need to be enhanced in HCWs, particularly in the subgroups whose confidence in the health system is lower.
Male HCWs reported greater confidence that the health system could manage the COVID-19 pandemic than female HCWs, which could be linked to males’ tendency to downplay risk [33]. Furthermore, the job roles, patient experiences, coping, mental health risks and personal commitments of HCWs differ by gender [34], and are linked to optimism and self-efficacy during health crises. There is a disproportionate distribution of race/population groups in the South African health worker force by professional category, years of experience, and job roles. However, after adjustment for professional category, sex, and age, perceptions of the health system’s capability were higher among Black African HCWs compared to other race groups. The factors associated with these differences need to be further understood.
Older HCWs and those who were confident in their knowledge about COVID-19 reported greater confidence in the national health system’s capability. Literature shows that older HCWs have more experience, which contributes to their higher confidence [35]. Experience in one’s job role in the healthcare sector contributes to an enhanced understanding of the health system, its capabilities and limitations. Furthermore, HCWs who are older, more experienced and working in senior roles might be less prone to panic in crisis situations, thereby explaining their optimistic perceptions of the health system’s capability.
Medical practitioners were less confident of the health system management in the pandemic than nurses, which should be interpreted by considering their different roles and experiences during the pandemic. It is likely that medical practitioners were already under pressure when consulting patients due to the existing quadruple burden of disease in South Africa [12] and were seeing challenges within the health system, thereby explaining their limited confidence in the health system’s management of COVID-19. Healthcare workers in other sectors, i.e., not in public and or private sectors, reported higher confidence in the health system’s capability. These HCWs included researchers and academics who were less frequently patient-facing. Therefore, they may not directly encounter or see the challenges in individual health facilities and may have a broader aggregated perspective of the national COVID-19 health response. South Africans with higher risk perceptions were less confident that their communities complied with the country’s lockdown regulations [36]. Healthcare workers who perceived themselves as being vulnerable to contracting COVID-19 may have lower self-efficacy and perceive the threat of the pandemic as very large.
The Western Cape and Free State provinces had the highest proportions of HCWs reporting the health system would manage the COVID-19 pandemic, while Mpumalanga province had the lowest. During the initial phase of the pandemic, higher infection rates were recorded in the Western Cape than other provinces. It is likely that HCWs in the Western Cape had higher confidence and self-efficacy in managing the epidemic from having dealt with more cases daily than the other provinces [23].
Despite immense improvements in the health system since 1994, there are still several service delivery challenges. These include unequal (human) resource distribution between the public/private sector and urban/rural localities [37], slow progress in health system restructuring [38], the ongoing disease burden [11], and poor goal setting, leadership and management. It is vital to address the structural challenges in the health system to improve the working conditions for HCWs.
While HCWs face exhaustion from longer working shifts, risk of infection and transmission to families, anxiety and stress, and limited resources including PPE, HCWs continue to provide patient care. As the greatest assets of our health systems, effective support for HCWs is essential, especially during a pandemic. Their challenges, needs and concerns must be understood, so that despite the ongoing COVID-19 pandemic, the fragile health system can still cope [12].
This study has some limitations. Healthcare workers with no access to the internet and technology as well as HCWs from health facilities with a high number of COVID-19 patients had a limited chance of participating in the online survey. To correct this bias, the survey data were benchmarked to the distribution of South Africa’s HCWs population by age, sex, population group, and province. This may allow generalizability of the findings of this study to the national population of HCWs in South Africa. Despite these limitations, the sample size for this study was relatively large, and it represented all major health professional categories in the country.
CONCLUSION
In the early days of the epidemic, most HCWs felt that the health system would not cope with COVID-19. Healthcare workers’ experience (a proxy for HCW’s age), work sector, professional category, confidence in knowledge about COVID, and risk perception were key factors affecting HCWs' perception of the health system's capability. It is important to build resilience and foster hope and optimism among HCWs while minimizing ongoing personal or workplace risks. Health systems strengthening and continuous professional development will contribute to improving collective efficacy among HCWs.
RECOMMENDATIONS
Experience Counts: Peer Support Initiatives and Access to Training for HCWs
Given that older age and higher education levels are attributes associated with being more confident in the health system response, we recommend peer support initiatives and mentorship to boost HCW confidence, and enhance psychological abilities, such as self-efficacy, resilience, coping abilities, perceived control, and mental health and wellbeing. Shung-king et al. [39] highlighted that mentorship and inter-generational role modeling can impact positively in the workplace. Perhaps much of what has been learnt in the one year since the epidemic hit South Africa was “on-the-job” training rather than formal training, given the speed at which the epidemic spread. Training content can be built on the experience gained. Healthcare workers need to have access to regularly updated education resources, including peer support learning. Strategies to build coping skills, such as ways to think optimistically and approach adversities, are needed.
Ongoing Engagement with HCWs in the Workplace to Contain Health Facility Outbreaks
After the fourth wave and emergence of variants, the risk of health facility outbreaks is ever present. Therefore, there remains the need for information sharing, making information easily accessible through multi-disciplinary collaboration and continued use of personal protection.
Research to Improve the HCW-patient Experience
Further research is needed to determine how HCWs’ lack of confidence in the health systems’ management translates into the patient experience during the pandemic in South Africa. Studies suggest that practitioners with confident standpoints toward their duties can effectively convey health promotion messages to patients [22]. Factors that hinder health service delivery in South Africa include poor infection control and hygiene, lack of resources such as medications and equipment, long patient waiting times due to HCW shortages, adverse events, litigation due to avoidable errors, and poor record-keeping [37].
Research Needed on Gender Issues Among the Health Workforce
The finding that male HCWs were more confident in the health system response warrants further exploration to understand the drivers for the gender differential. As the majority of HCWs are female, and they occupy high-risk positions in the health sector, there is an urgent need for gender responsiveness in the health workforce [40], including mental health support structures. Research exploring gender inequalities among HCWs in South Africa is limited [39]. Qualitative work is required to understand these inequalities. A recent report on the demographic and clinical characteristics of HCWs admitted with COVID-19 from March 5th, 2020, to September 18th, 2021, showed approximately 67% to be females [41]. A total of 12.8% of HCWs had been reported to pass away [41].
AUTHORS’ CONTRIBUTIONS
TM conceptualised the paper, conducted the analysis, and interpreted the results. TM, TMa, SS, ND, RS, and IN drafted the manuscript. TM, TMa, SS, ND, RS, IN, MM, MMo, and PR contributed to interpreting the results and editing the manuscript. All authors read and approved the final manuscript before submission.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethics approval was received from the Human Sciences Research Council (HSRC) Research Ethics Committee (REC); (REC 5/03/20).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All participants provided electronic informed consent.
STANDARDS OF REPORTING
STROBE guidelines and methodologies were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analysed during this study are available on request from the corresponding author [T.M.].
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors thank all healthcare workers who participated in the HSRC COVID-19 Online Survey. They also thank the HSRC COVID-19 Research Team. Health Professions Council of South Africa (HPCSA) and the South African Nursing Council (SANC) are credited for sharing data used for benchmarking.


