All published articles of this journal are available on ScienceDirect.
Development of a Family-Centred Nutrition and Exercise Diabetes Care Programme for Better Diabetes Outcomes in Rural Areas of Limpopo: Practice-Oriented Theory
Abstract
Background:
Cost-effective interventions are required to manage the increasing prevalence of diabetes mellitus and minimize new cases. Family-centred care interventions positively influence patients’ diabetes outcomes and improve health and quality of life. This article aims to describe the development of family-centred nutrition and exercise diabetes care intervention.
Methods:
A mixed method study design was used in the baseline study. The findings from the qualitative interviews and quantitative survey informed the development of the family-centred nutrition and exercise diabetes programme, with the guidance of practice-oriented theory.
Results:
Components of practice-oriented theory guided the study and were applied. The researcher outlined that dietitians and physiotherapists are agents to provide family-centred nutrition and exercise diabetes care to patients and their families. One element of practice-oriented theory involves how the programme is to be implemented, which will be face-to-face in focus groups.
Conclusion:
The study further highlights the need for piloting the implementation of the intervention to determine other dynamics that may obstruct overall implementation.
1. INTRODUCTION AND BACKGROUND
Diabetes Mellitus (DM) is a fast-growing disease. Around 537 million individuals are currently living with diabetes worldwide [1]. Increasing diabetes prevalence leads to complications, increased morbidity, and mortality among patients [2]. Across the globe, a high proposition of poor glycaemic control among diabetes patients was reported [3]. This was attributed to a lack of blood glucose tests, duration of diabetes, presence of complications, poor self-efficacy, and poor self-care behaviours [3]. According to the World Health Organization (WHO) [4], diabetes is expensive to manage and even more costly in the presence of other complications. The cost of managing diabetes is estimated at $1.31 trillion, which accounts for 1.8% of the global gross domestic product of 2015 [5]. Furthermore, the WHO [6] points out that a series of cost-effective interventions are required in diabetes management, irrespective of the type, to improve health outcomes. An expanded burden of Non-Communicable Diseases (NCDs) and communicable diseases were reported in less developed countries without sufficient resources for management [7]. In most developed countries, strategies for the management of NCDs are advanced, with the inclusion of family-centred care [8].
Family-Centred Care (FCC) is an approach to collaborating with patients' families to improve treatment outcomes [9]. Most diabetes care takes place where patients reside, so the use of the FCC approach enables family members to join patients in consultation sessions with healthcare providers for empowerment with the knowledge and skills required in diabetes care [10]. Family members who attend medical consultations with patients have access to more knowledge on how to care for or support them, as this information comes directly from the patient’s healthcare provider [11]. So far, the FCC has been found to positively influence outcomes [12] and improve the health and quality of life of diabetes patients. Inadequate diabetes-related nutrition and exercise knowledge may be liable for poor diabetes outcomes [13]. Behaviours of family members that may be unfavourable include preparing unhealthy meals and promoting inactive lifestyles [14], particularly due to inadequate knowledge. It is essential to assess the diabetes knowledge of non-diabetic family members to reinforce identified knowledge gaps and enable the provision of effective support [11]. In addition to diabetes education to improve knowledge, families should be made aware of the coping skills required for better self-care practices [15].
Before developing a diabetes intervention, a needs assessment should be conducted to identify the immediate needs of the target population [16]. The need for an intervention generally results from a condition of imbalances [17]. The purpose of conducting a needs assessment is also to assess and incorporate the local and cultural needs of the target population. It is imperative to include stakeholders during the development of intervention [18] for acceptance and sustainability [19]. When introducing diabetes interventions, healthcare workers should seek evidence-based approaches that have been found to improve the clinical outcomes and QoL of patients [20].
This article is taken from a larger study titled‘ development and implementation of a family-centred nutrition and exercise diabetes care intervention for patients at Senwabarwana in Limpopo Province, South Africa’. A mixed method approach following convergent parallel design was used during the baseline study to explore patients' quality of life and describe the knowledge, attitudes, and practices of patients and family members related to nutrition and exercise diabetes care. The main aim of this article is to describe the development of family-centred nutrition and exercise diabetes care programme using practice-oriented theory.
2. METHODOLOGY
Based on the baseline study results and the use of a conceptual framework, this study employed a developmental design to establish family-centered nutrition and exercise diabetes care.
2.1. Baseline Study
A baseline study was conducted prior to the development of the programme to gain insights and determine factors impacting diabetes management. The literature review indicated that family support is crucial in diabetes outcomes [4]. In addition, it was discovered that most diabetes care happens in patients’ places of residence [8, 9], hence the inclusion of family members in this study. The following components were assessed: (1) knowledge, (2) attitudes, (3) practices related to nutrition and exercise diabetes care, (4) anthropometric status (Body Mass Index and Waist Circumference) of patients and family members, and (5) quality of life of patients diagnosed with diabetes.
The findings from the quantitative survey highlighted the prevalence of obesity among diabetes patients and their non-diabetic family members. Furthermore, the quantitative findings establish a need to improve participants’ knowledge, attitudes, and practice related to family-centred nutrition and exercise diabetes care programme. Unhealthy habits, including overeating, skipping breakfast, eating unhealthy meals, lack of physical activity, as well as the high prevalence of obesity, all influence behaviour change. On the other hand, diabetes patients in the qualitative strand of the situational analysis phase indicated that the family culture of consuming large portions once a day without any physical activity, influenced the need for family-centred care and behaviour change. Furthermore, the qualitative data revealed diabetes patients' lived experiences, which included little or no sexual intercourse, stress, non-disclosure, inappropriate food consumption, and inability to work prior to diagnosis. These challenges were found to affect patients’ Quality of Life (QoL).
2.2. Conceptual Framework
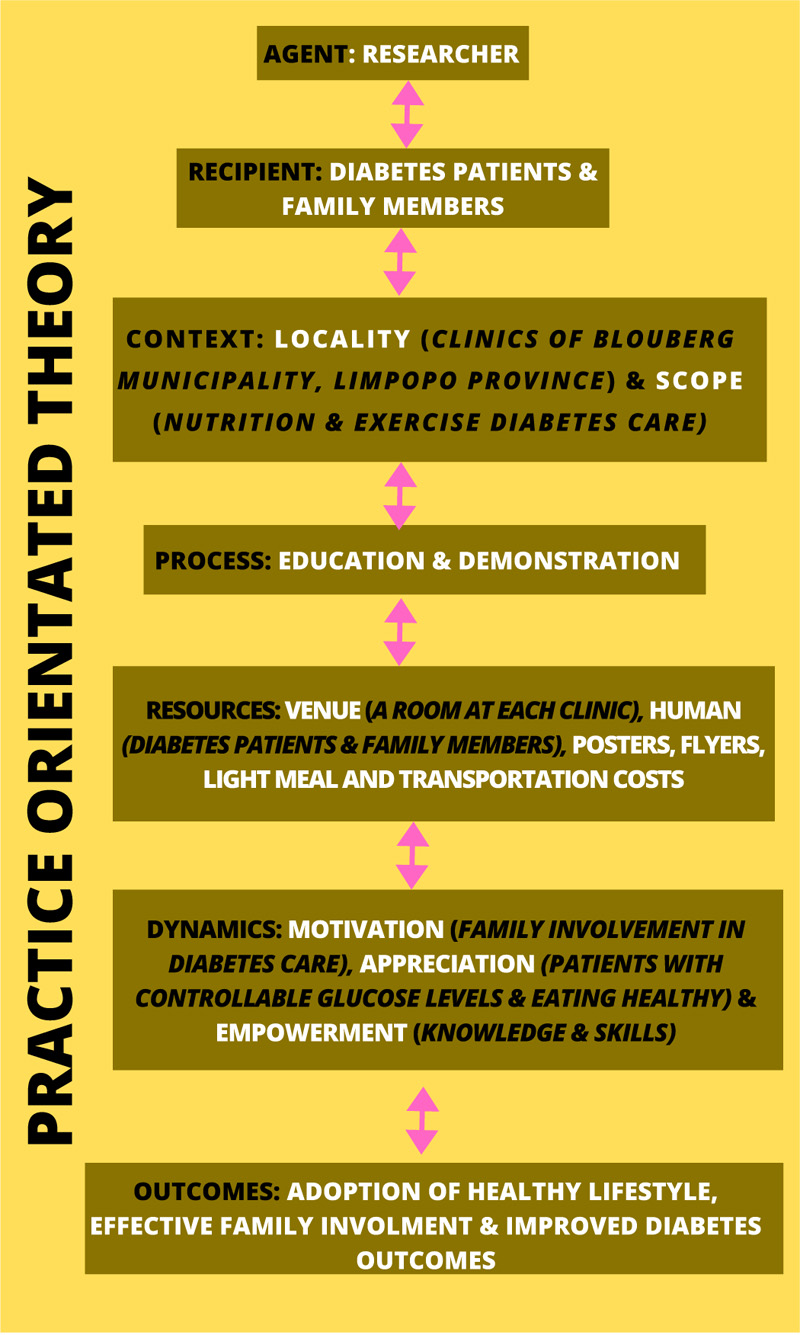
The conceptual framework which guided the overall study was based on the Practice-Oriented Theory (POT) by Dickhoff [21]. It explains concepts and examines activities aimed at achieving programme objectives. The POT has seven elements: Agents, Recipients, Context, Process, Resources, Dynamics, and Outcomes. However, in this study, only five components of POT were used in the development of the programme and are explained as follows:
2.3. Agent
The agent is the element of POT concerned with identifying the providers of the intervention. The agent is the person responsible for planning, coordinating, and developing a programme [21]. The researcher was in charge of organising and coordinating the development of the intervention based on the findings of the baseline study, which identified knowledge gaps and the need for behavioural change. The researcher identified the need for a dietitian and physiotherapist to offer education on nutrition and exercise diabetes care.
2.4. Recipients
The recipients of the intervention receive the prescription of the activity from the agents so as to achieve desired outcomes [21]. Recipients are the primary beneficiaries of the intervention. The primary recipients of this programme are diabetes patients and their family members. Only diabetes patients and family members who participated in the baseline study participated in the intervention. Therefore, purposive sampling was used to sample both patients and their non-diabetic family members.
2.5. Context
Context is defined as an environment or setting that not only considers the physical aspects or locality but policies governing or directing the activity at hand [22]. All factors affecting the engagement of the agent with recipients towards yielding desirable outcomes could be included in the context [23]. The context of this intervention consists of the locality and scope. Locality refers to where the programme or intervention is to be implemented. In this case, the intervention was implemented in the clinics of Blouberg Municipality in the Senwabarwana area. Blouberg Municipality is a rural-based municipality with a population of 162 297 people [24]. There are 22 clinics, 2 health centres, 4 mobile clinics, and one hospital in the Blouberg Municipality. As indicated, context is not only limited to the physical location but also directs the activity at hand [22]. The scope of the programme or educational guidelines, as well as behavioural change processes, are directing the activity in this case. A needs assessment is required to design an educational program that deals with the local needs of the target population [25]. The scope of the intervention or programme is based on the results of the baseline study, which identified the need to improve knowledge in the following areas:
- Importance and benefits of nutrition in diabetes care
- Food preparation
- Food intake and medication
- Food intake and exercise
- Importance and benefits of exercise in diabetes care
- Types of exercises
- Glucose monitoring and exercise
2.6. Process
The process emphasises the activity's course, steps, or patterns. According to Meleis [23], processes are steps taken by the agent so as to realize the desired goal. In this study, the process is defined as procedures of programme development inclusive of actions taken to ensure that the programme is validated before its implementation [26]. Professionals or experts in programme validation from institutes of higher learning examined the proposed programme and provided scholarly assistance [26].The experts reviewed programme content and gave feedback. The process also included how the programme would be executed, which included face-to-face instructional discussions in focus groups of up to 10 people (5 diabetes patients and 5 family members) in the local language.
2.7. Resources
Resources are key factors in programme implementation. In this context, resources refer to the equipment and financial and human resources needed to carry out the intervention or provide political support [27].Therefore, the following resources are needed for the implementation of this programme:
- Facility at the clinic for programme to take place.
- Educational materials (flyers and wall posters) to assist in active learning and behaviour modification. Transportation fees to and from the clinic for patients and family members.
- Light meals for the period of implementation.
- Nurses to help in securing participants and venue.
- Diabetes patients and families as participants or recipients.
2.8. Ethical considerations
This study is part of a bigger study approved by Turfloop Research and Ethics Committee with reference number TREC/35/2019:PG and permission was given by Limpopo Department of Health with ref: LP 201903-007. All participants provided written informed consent. Participation was voluntary and participants were informed of their freedom to withdraw from the study at any stage without penalty. Privacy and confidentiality of the participants’ data were also maintained.
3. RESULTS
The conceptual framework applied in this study was based on the practice-oriented theory. However, only five components of POT guided the development process, namely: Agent, Recipients, Context, Resources, and Process. The findings of the baseline study guided the outlining of results via a practice-oriented theory component. The development of family-centred nutrition and exercise diabetes care intervention was to empower diabetes patients and their family members with the knowledge and skills necessary to help achieve better glucose outcomes and minimize prevalence, respectively.
Fig. (1) presents the elements or activities adapted from the Practice-Oriented Theory to describe the development of family centred nutrition and exercise diabetes care programme.
3.1. Agent
The main agent in this study was the researcher who developed the family-centred nutrition and exercise diabetes care programme for better diabetes outcomes. Furthermore, the intervention was provided by dietitians and physiotherapists, who provided advice on nutrition and exercise diabetes care, respectively.
3.2. Recipients
The recipients were diabetes patients and their non-diabetic family members. Diabetes patients, as the primary recipients, were expected to participate in order to improve their self care practices.Family members were expected to participate in the study as to gain knowledge on how to best assist diabetic family members and minimize the prevalence of diabetes.
3.3. Context
The context refers to both the place where the programme is to be implemented and the scope of the intervention. The specific context of this programme includes the clinics of Blouberg Municipalities in Senwabarwana of Capricorn District in Limpopo Province, South Africa. The context also includes the scope of the intervention, informed by the outcomes of quantitative surveys and qualitative interviews in the baseline study.
Table 1 shows the learning guides that include the importance of nutrition, food preparation, food intake and medication, food intake and exercise, benefits of exercise, types of exercise, and glucose monitoring during exercise.
| Learning Outcomes | Beneficiaries Must be Able To: |
|---|---|
| Importance and benefits of nutrition | Adopt healthy eating habits |
| Increased intake of breakfast | |
| Consumption of small frequent meals | |
| Knowledge of what to eat and what not to eat | |
| Food preparation | Avoidance of fried food |
| Less use of sugar and salt during food preparation | |
| Food hygiene | |
| Not overcooking food | |
| Food intake and medication | Consuming food before or after taking medication as per the prescription |
| Use of reminders for medication/insulin injection | |
| Food intake and exercise | Food intake before or after exercises |
| Intake of high carbohydrate drinks during exercise | |
| Importance and benefits of exercise | Knowledge of exercise prescription |
| Understanding the consequences of no physical exercise | |
| Types of exercise | How to make exercise a daily part of life |
| Engage in enjoyable exercises | |
| Ability to listen to their bodies while exercising and stopping once startfeeling dizzy | |
| Engage in exercises as a family | |
| Choose low-risk exercises | |
| Glucose monitoring and exercise | Checking of blood glucose before or after exercise |
| Those without glucometers should avoid engaging in prolonged exercises and also eat before and after exercise | |
| Glucose levels |
3.4. Process
Process involves the actions to be taken in the implementation of the intervention. In this study, the process was the family-centred nutrition and exercise diabetes care programme for patients in clinics of Senwabarwana to empower both patients and family members with knowledge, skills, and abilities for better outcomes and to minimize new diabetic cases, respectively. Guidelines are considered essential foundations for healthcare policy, planning, delivery, evaluation, and quality improvement by clinicians, managers, and policy-makers [28].
The following guidelines assisted the implementation of the intervention:
- Face-to-face group.
- Use of educational tools such as posters and pamphlets to facilitate knowledge and behavioural change.
- Submission of implementation schedule to the clinic 5 days prior to implementation.
- Arrange for a clinic location.
- Recruitment of participants.
3.5. Resources
Resources and their effective use are essential elements of practice-oriented theory and are significant for the successful implementation of family-centred nutrition and exercise diabetes care intervention. The resources required include (1) Humans, (2) Materials or Educational tools, (3) Finances, (4) Equipment, (5) Transportation, (6) Consultation rooms, (7) Light Meal or Lunch, and (8) Stipend. The human resources needed are shown in Table 2 with defined roles.
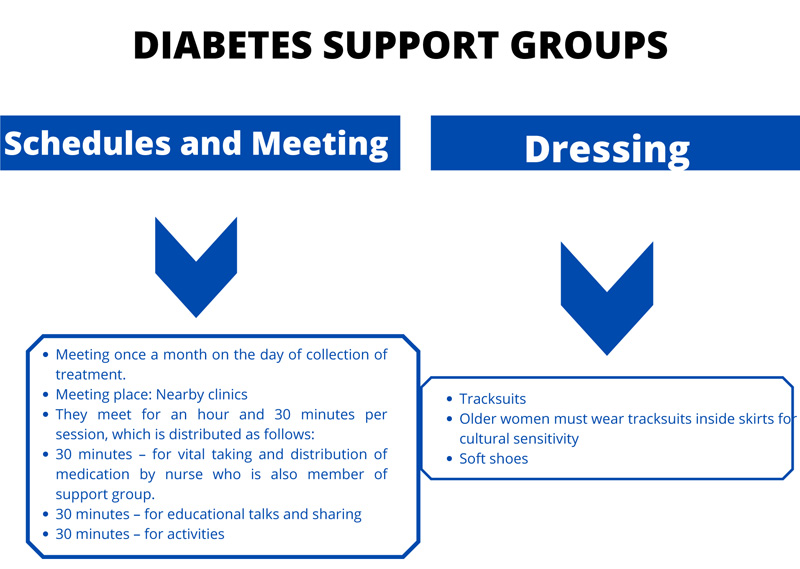
Diabetes support groups are essential resources to support adopting a healthy lifestyle for better diabetes outcomes. The schedule of diabetes support groups is described, as shown in Fig. (2).
Fig. (2) depicts the meeting schedule for diabetes support groups, which is once a month at nearby clinics and the division of sessions into educational and physical activities.The dress code is also prescribed.
Table 2.
| - | Responsibilities |
|---|---|
| General Practitioners | Perform their professional duties and also refer to other healthcare providers. |
| Dietitians | Educate about nutritional diabetes care management and also treat. |
| Physiotherapists | Educate about exercise diabetes care management and also treat. |
| Psychologists | Perform their professional duties and also promote mental health. |
| Social Workers | Perform their professional duties and make sure patients are well looked after through social relief programmes. |
| Nurses | Establish and facilitate support groups; identify patients and family members who may need the attention of other multidisciplinary teams such as dietitians and physiotherapists. Take vital signs of patients. |
| Patient | Be part of support groups, encourage each other on how to best manage diabetes, and take charge of their health |
| Family members | Be part of support groups and provide support to patients at home, where most of the care takes place. |
4. DISCUSSION
The overall aim of this study was to develop family-centred nutrition and exercise diabetes care for better glycemic outcomes among outpatients in rural areas of Senwabarwana in the Capricorn District of Limpopo Province, South Africa. The Practice-Oriented Theory was used to guide the intervention's development process. This is the first programme developed for diabetes patients and their families at the Senwabarwana area in Blouberg Municipality. The newly developed intervention is the first step toward improving diabetes care and preventing new cases among the most vulnerable persons [29].The non-diabetic family members of diabetes patients are already at risk of developing Diabetes Mellitus due to family history [8]. Individuals with a family history of diabetes are 3 times more likely to develop diabetes than those without a family history [30]. It has been reported that poor diabetes control led to complications, increased morbidity, and mortality among patients [3]. The POT guided the development of the intervention for better diabetes outcomes and to minimize the associated risks.
The study described five components of the Practice-Oriented Theory that helped develop the family-centred nutrition and exercise diabetes care programme. The components of the POT that guided the development of the family-centred nutrition and exercise diabetes care are Agent, Recipients, Context, Resources, and Process. The agents were dietitians and physiotherapists who provided nutrition and exercised diabetes care education to both patients and their non-diabetic family members, respectively. As one of the aspects of POT, the education was provided based on the context, which established the scope of the intervention and was guided by the baseline study's findings.Appropriate awareness is necessary in diabetes management to empower beneficiaries with knowledge on how to best manage the condition. The family-centred nutrition and exercise diabetes care intervention indicated that the program shall be offered face-to-face to a group of diabetes patients and their families. Various studies about self-management education programmes have shown that most diabetes educational interventions were offered through face-to-face education [31, 32] and that the interventions have been effective in improving the knowledge of beneficiaries.
The practice-oriented theory developed the intervention, which provided a practical component for organizing family-centered nutrition and exercise diabetes care intervention. According to Mothiba [32], the practice-oriented theory describes components that should be followed to design and develop an intervention. The Agents, Recipients, Context, Process, and Resources were the only five components used in the development of the intervention. The use of the theory was helpful because it followed well-defined basic and easy-to-follow elements [33, 34]. The baseline study results enabled defining agents and their scope within the context component of practice-oriented theory. The scope of the intervention was informed by major knowledge gaps, which were determined in the baseline study findings. Knowledge gaps revealed during the baseline study, according to Bopape [35], provided the basis for learning outcomes, content and activities, instructional and assessment strategies, as well as training topics. Furthermore, a study by Tsolekile, Schneider, and Puoane [36] reported poor diabetes knowledge among healthcare providers and the need for training and education for better diabetes outcomes.
CONCLUSION
The Practice-Oriented Theory as a conceptual framework guided the development of the family-centred nutrition and exercise diabetes care programme. The use of the practice-oriented theory helped in defining the agents who are to offer the intervention to patients and their family members as recipients. The study further highlighted the need for piloting the implementation of the intervention to identifyidentify other dynamics that may obstruct the successful implementation of the intervention.
LIMITATIONS OF THE STUDY
The programme has not been implemented yet, so some of the dynamics or challenges that may obstruct the successful implementation may be identified during the implementation and evaluation of the programme.
RECOMMENDATIONS
To demonstrate awareness of the recent conceptual developments in practice-oriented theory and related fields: Pilot the implementation of the developed family-centred nutrition and exercise diabetes care programme, while keeping an eye on the rapid conceptual development in practice-oriented theory and related fields [37-45].
AUTHORS’ CONTRIBUTION
Mphasha was a project leader, responsible for data collection and interpretation, Skaal supervised data collection and interpretation, and Mothiba co-supervised data collection and interpretation, The contributions of the authors in writing this article were 50%, 30%, and 20%, respectively. The final manuscript was approved by all three authors.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical clearance for this study was obtained from the Turfloop Research Ethics Committee (TREC) at the University of Limpopo (TREC/35/2019: PG). Permission to conduct the study was obtained from the Limpopo Province Department of Health (LP 201903-007) and operational managers in clinics.
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from participants prior to data collection.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
This article is based on the data collected from diabetes patients in Blouberg Municipality, Senwabarwana area of Limpopo Province, South Africa. The data generated or analysed during the current study is not publicly available. However, the data sets used during this study are available on request for readers from corresponding authors.
FUNDING
None.
CONFLICT OF INTEREST
he authors declare no conflict of interest, neither financial nor otherwise.
ACKNOWLEDGEMENTS
The authors acknowledge male diabetes patients with erectile dysfunction for participation.


