All published articles of this journal are available on ScienceDirect.
Effects of a Continuity of Preterm Infant Care Program on Parenting outcomes and Service Utilization Rates
Abstract
Background:
After transition to home, most preterm infants exhibit higher readmission rates due to lack of readiness for hospital discharge and inadequate discharge preparation. Continuity of care during transitional care is an essential intervention for achieving parental readiness and performance in this group.
Objective:
The study aims to analyze the effects of continuity of care program for parents with preterm infants (CCPI) on parental performances, parental readiness, and service utilization rates post-discharge.
Methods:
A randomized controlled trial evaluated 92 dyads of preterm infants and parents. They were randomly assigned to two groups. The experimental group received the CCPI with routine nursing care, and the control group received only routine nursing care. The parental readiness and parental performance questionnaires were completed by the parents and analyzed using analysis of covariance (ANCOVA). The effectiveness of the CCPI in reducing the service utilization rates post-discharge was demonstrated using RM-ANOVA.
Results:
The parents’ performance who participated in the CCPI was significantly higher, as was their readiness for hospital discharge than the parents of the control group (p< 0.01). In addition, the service utilization rates for the samples significantly decreased (p< 0.01) at the fourth week after discharge. However, there was no significant difference between the first- and second-week post-discharge.
Conclusion:
The study findings may help policymakers deploy the CCPI for parents with preterm infants while suggesting that the CCPI should be used to promote growing preterm infants to reduce post-discharge service utilization rates significantly.
1. INTRODUCTION
The rate of preterm infant births has increased in many countries, especially those considered poor to middle-income level, globally accounted for around 10.6% in 2014, and increased to 16% in 2019 [1, 2]. Approximately 81.1% of preterm births occurred in African and South Asian countries. In Thailand, during 2015-2018, the percentage of preterm infants increased from 10.61% to 11.20% [2, 3]. This makes it apparent that high-risk infants that need special care still exist in Thailand. Preterm infants are more prone to organ dysfunction; they have an increased risk of neonatal morbidity, and require long-term care for growth and development problems [4]. Parents feel frustrated when they think about the preterm infant’s needs [5]. Parents need more time and space to adjust their developmental tasks in terms of living with a preterm infant [6]. The family dynamics for parents that have preterm infants differ from others because they feel an extra burden in being a parent; their child requires more than routine care and more advanced caregiving at home [7, 8]. As a result, parents sometimes require healthcare professionals to support and reassure them during transitions [9] in order to carry out their duties during early child rearing, which are needed in order to promote optimal growth and the development of preterm infants as well as that of the family. In addition, the question becomes how to enhance the family life position, family roles, and transition for the next stage of the family’s development.
According to the Transition Theory of Meleis [10], the transition is the process of movement from one state, condition, or place to another. In terms of the transition for the families of preterm infants, they are defined as multiple types of transition, which include transition from the hospital to home and transition to parenthood. In a previous study [11] among Thai mothers of preterm infants that participated in a transitional care program before discharge, it was revealed that they increased their knowledge and skills for taking their fragile infants. The results demonstrated that the mothers in a transitional care program accepted their role as a mother of a preterm infant, and they experienced a healthier transition than the control group. A transitional care program requires providers to get involved at multiple points before discharge andprovide an effective discharge plan to facilitate a smooth transition to home [12, 13]. Analysis of the interventions from a few studies has shown that dedicated transition providers, facilitated communication with the outpatient, and the creation of a multiple disciplinary team to implement a specific discharge process can reduce the rate of readmission within thirty days [14, 15]. Unfortunately, Thailand also has a limited number of home healthcare teams, a shortage of neonatal nurses and neonatologists for home visits, and inadequate community resources to support the parent of a preterm infant [16]. Furthermore, a successful transition depends on discharge quality and parental readiness. The strategies for improving parental readiness include promoting technical skills and empowering them to continue training until they feel confident and have improved their ability to preterm infant care [17]. The quality of discharge teaching focuses on discharge content and the discharge teaching method [18, 19]. Nowadays, there are many innovations to support discharge teaching materials for preterm infants and families, such as handbooks, multimedia, videos, and web-based learning [20]. Prior studies have found that technology-based and telehealth platform counselling allows the parents to access all discharge materials (discharge guidelines, brochures, videos) after class/discharge teaching, thus improving information transfer from providers to parents [21].
However, the transition from the hospital to home is only the beginning of a new life cycle for families with preterm infants. Preterm infants need healthcare services and monitoring of proper growth and development throughout the first year of life [22]. Parents still have many doubts and feelings of worry due to the conflict among providers from the NICU, primary healthcare setting, and outpatient unit. Parents receive numerous information before discharge, which represents a poor mechanism for care coordinate [23, 24]. Therefore, the concept of continuity of care proposes to mitigate this problem through the linkage among the subunits with the health care management through continuity of care . According to Haggerty et al. [25], continuity of care is continuously enhanced care, and the continuity of care program facilitates continuing care and collaboration with the healthcare team from various disciplines. This is similar to a previous research [26-28], which found that continuity of care program can reduce the rate of readmission in patients with type 2 diabetes, improve self-care knowledge, and reduce length of hospital stays in high-risk pregnancy. No study however examined the effect of continuity of care for parents with preterm infants. Thus, this study sought to test the effect of continuity of care for parents with preterm infants on parental performances, parental readiness and service utilization rates post discharge. Moreover, it was expected that this program could decrease the service utilization rate within thirty days post-discharge, which would reflect family confidence in child management. Therefore, besides the gap in practice among parents with preterm infants, a continuity of care program for parents with a preterm infant aims to decrease the gap between the healthcare staff and family in order to create a linkage between any two subunits in the healthcare system by using the concept of continuity of care.
2. MATERIALS AND METHODS
2.1. Design and Setting
This randomized controlled trial was conducted on parents with preterm infants at Thammasat University Hospital (TUH), Thailand. Data were collected over a period of ten months, from March to December 2020.
2.2. Sample/ Participants
The participants were recruited from parents that were hospitalized with preterm infants at TUH. The inclusion criteria of the infants were as follows: (1) gestational age (GA) 32 to 36 weeks, assessed using the Ballard score maturation [29]; and (2) stable condition with normal vital signs and not requiring oxygen therapy at home [30]. In addition, the inclusion criteria for the parents were as follows: (1) personally caring for the preterm infant during the first month after hospital discharge; (2) literate parents; and (3) parents and preterm infants living within 50 kilometers of the hospital selected as the study site.
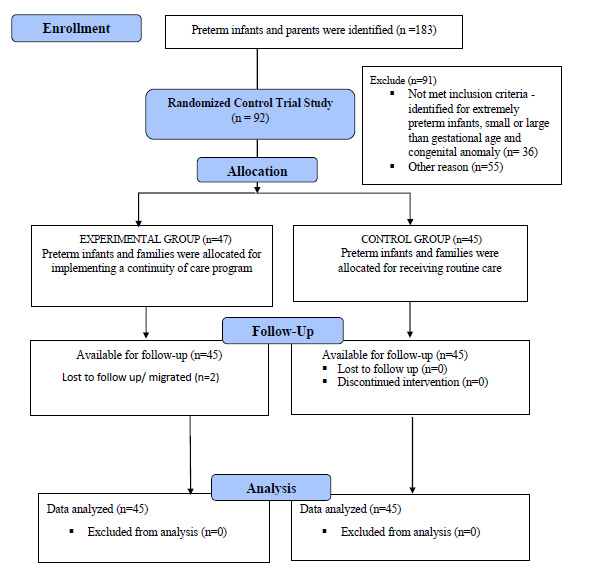
The sample size required to obtain a valid assessment of the effectiveness of the CCPI was determined by power analysis using G*Power version 3.1.9.2 [31]. Then, the researcher calculated the sample size and used the effect size of 0.30 from a previous study related to preterm infants by Chen, Zhang and Bai [32]. A significance level of .05 and a power of 80% were used to calculate the required sample size. The optimal sample size was approximately 45 dyads for the parents and preterm infants in each group. Therefore, the sample size in this study was 90 dyads of parents and preterm infants; the CONSORT flow diagram is displayed in Fig. (1).
2.3. Sampling Method
A total dyad of 183 preterm infants with parents from TUH, Thailand, who were hospitalized, were screened for this study. A total of 92 dyads met the inclusion criteria and consented to participate in the study. This study is a single-blind design in order to reduce selection bias and confounders. In addition, our study used blocked randomization with Sealed Envelope Software [33] in order to randomly assign a dyad of preterm infants and parents into two groups. Forty-five dyads of preterm infants and parents from the total sample were assigned to each group. Two dyads from the experimental group discontinued intervention due to loss to follow-up and migrated to another city.
2.4. Intervention
The researcher developed the CCPI based on the Transition Theory of Meleis and colleagues [10] and the concept of continuity of care by Haggerty et al. [25]. The CCPI consists of three phases that include: discharge preparation before transition to home; evaluation of the family members for readiness, home environment readiness, neonatal readiness, and screening for community resources for parents with preterm infants; and providing continuity of care post-discharge with telephone follow-ups, home visiting by the healthcare team, and provision for follow-up care. The experimental group intervention included three phases as seen in Fig. (2). Each step was conducted at different time points as follows.
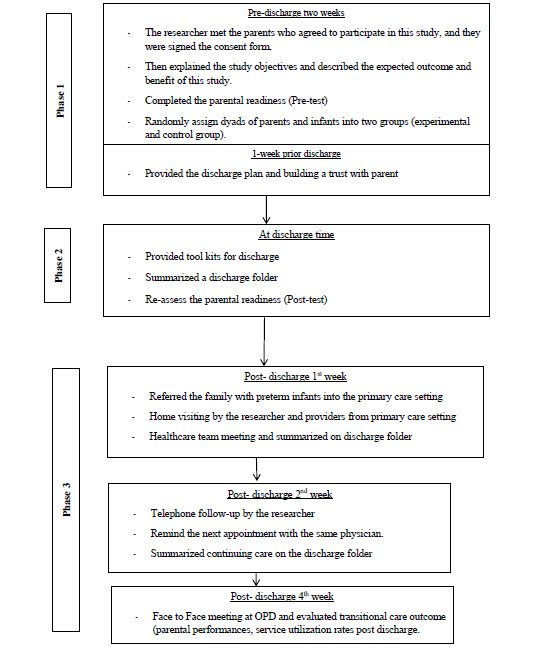
2.4.1. Phase 1: Pre-discharge (Two Weeks before Discharge Day)
Phase 1 was initiated two weeks before discharge. The parents in the experimental group received a discharge tool kit (such as a thermometer, a bulb syringe, and a preterm infant handbook). The researcher explained the learning method and demonstrated how to take care of their preterm infant, including the feeding pattern, maintaining body temperature, maintaining respiratory control, bathing, dressing, and learning about the response of the preterm infant and his or her behavior. Families received an individualized training course in order to gain more hands-on experience with the parents three times a week and this took place 20 minutes/day. The discharge teaching used a preterm infant handbook and a clip video with a flipchart to explain the preterm infant's behavior. Subsequently, the researcher made an appointment to set a schedule to evaluate the parents’ knowledge in the next week. At one week before discharge, the researcher encouraged the parents to use the discharge tool kit to learn about the timetable for adjusting the complex medication at home and home environment preparation, for example the bed and crib using the flipchart. Moreover, crucial data about cardiopulmonary resuscitation were taught using a clip video. The parents in the control group received only routine nursing care. They received discharge teaching in three sessions (such as hygiene care, feeding skills, and first-aid). The duration of each session was 20 minutes. However, the issues of neonatal readiness and content for basic preterm infant care were catered by different healthcare teams that had their duty on the discharge day.
2.4.2. Phase 2: On Discharge Day
On discharge day, the following discharge plan was discussed among the healthcare team and families in order to retain the role of management in the experimental group. First, the researcher completed a checklist in the discharge folder and coordinated with providers to summarize the discharge plan. Parents reviewed the special care for preterm infants, confirmed an initial appointment or follow-up, and evaluated the home care plan. Simultaneously, the parents were given the parental readiness via RHDS-parent form before discharge. In case of unreadiness for hospital discharge, the healthcare team took action to improve readiness (such as reviewing the family discharge folder and requesting the primary healthcare team for support).
2.4.3. Phase 3 Post-discharge (1st Week – 4th Week)
The third phase had three sessions to promote management continuity and maintain interpersonal continuity between providers and the families. The first session was conducted from five to seven days after discharge, and the researcher provided home-based continuity of care. The CCPI facilitated the interpersonal continuity among the physician and the healthcare staff from the same team across settings (from the Neonatal intensive care unit; NICU to the Outpatient department; OPD). The researcher sent a family discharge folder to the healthcare staff in the primary care setting in order to establish a team for home visits. Additionally, the researcher interviewed parents regarding the preterm infant's basic care at home and supported the family in managing any adverse event or any health deviation of the preterm infants. If they required a healthcare service, the researcher would coordinate with the healthcare providers and fill out the health information in the discharge folder. Two weeks later (the second session), the researcher had a telephone follow-up and reassured the parent of the next appointment at the OPD. Finally, the researcher met the participants at the OPD in order to evaluate the continuity of care outcome within four weeks post-discharge. On the other hand, the parents with a preterm infant in the control group received routine nursing care from different healthcare staff between the tertiary care setting and primary healthcare setting. The primary healthcare providers were provided with a telephone follow-up and home visits. Four weeks after discharge, the parents brought their preterm infants for follow-up at the tertiary care setting with an unspecified pediatrician (same as the OPD but a different provider for infant care).
Before implementing the CCPI, its content was assessed by five experts. They were neonatologists, an advanced practice nurse (neonatal nurse), and professional academic nurses. The experts agreed on the content of the CCPI and recommended adding an optional vaccine and a breastfeeding technique in the preterm infant handbook. All of the suggestions were accepted. The feasibility and acceptability of the CCPI were tested with five dyads of parents with preterm infants. The results indicated the feasibility and acceptability of the CCPI, and no further change in the CCPI was made.
2.5. Data Collection Tools
The data collection tools included a socio-demographic datasheet record, a service utilization rates post-discharge (SURPD) datasheet record, the Readiness for Hospital Discharge Scale-parent form, and the questionnaire for preterm infant rearing behavior of mothers.
A socio-demographic datasheet record was maintained in two parts. The researcher developed the first part to address the characteristics of the parents with preterm infants. These included family income, parental education level, and age of the parents. In addition, the researcher collected data on the preterm infants regarding sex, gestational age, weight, diagnosis, health insurance, and the history of health conditions/health problems during admission. In addition, a SURPD datasheet record was used to record the frequency of emergency room visits or re-hospitalization for sick newborns at TUH. On the other hand, the SURPD did not include the routine follow-up at the OPD. The parents completed the questionnaires before and after intervening. The questionnaires included the issues of parental readiness and parental performances, and permission was obtained to use all copyright instruments.
The Readiness for Hospital Discharge Scale was designed by Weiss and Piacentine in 2006 [34, 35]. The RHDS is typically used to determine the parents’ perception of the hospitalized child (including premature infants) and measured readiness for hospital discharge. The original version of the RHDS-parent form was comprised of 29 items in two parts: 1) assessing the perceived readiness for hospital discharge; 2) and the part that was divided into five subscales: personal status of parents, preterm infant status, knowledge, coping ability, and expected support. The parental readiness score is a rating scale from 0 to 10. The highest score is 10, which indicates parental perception of greater readiness. After obtaining permission from the designer, the tool was translated into Thai by Inta, Kantaroj, and Dasri [36] with the standard translation guideline. Thai-PedRHDS was checked after forward and backward translation and evaluated for content validity by three experts in neonatal nursing care. The content validity index score was 1.0. Thai-PedRHDS was piloted for internal consistency reliability via 30 parents. Cronbach’s alpha was found to be 0.86. This reliability was acceptable.
The questionnaire for preterm infant rearing behavior of the mother by Tongkammak and Jirapaet in 2010 [37] was used to measure parental performance after discharge. The validity of this questionnaire was determined using the content validity method, where the content validity index was 0.84. The reliability of the questionnaire, with an alpha coefficient of 0.86, was confirmed. There were 25 items with ratings on a Likert scale. The score of each activity was assessed at five levels: 1=Never, 2=Seldom, 3=Sometimes, 4=Frequently, 5=Always. The possible scores ranged from 25 to 125 points. The highest scores referred to a greater frequency of activity used to determine the parental performance for taking the preterm infants home under the principle of newborn care [36]. In our study, the researcher conducted a pilot study on thirty parents of preterm infants and obtained a Cronbach's alpha coefficient of 0.89.
2.6. Statistical Analysis
Data related to frequency, percentage, mean, and standard deviation were summarized. ANCOVA was used to compare average parental performances scores and the parental readiness scores between the experimental and control groups. In addition, RM-ANOVA was used to compare the rate of post-discharge service utilization in the experimental group after implementing the continuity of care program within the 1st week, 2nd week, and 4th week. SPSS for Windows, version 26 (Statistical Package for the Social Science, IBM, USA) [38] was applied to analyze the socio-demographic data and to analyze the effect of the CCPI. The degree of significance was approved at 0.05 for all groups.
3. RESULTS
3.1. Socio-demographic Characteristics
No significant differences were found between groups in terms of the characteristics of the preterm infants. The groups had similar demographic characteristics (gestational age, birth weight, mode of delivery, and body weight before discharge) (Table 1).
Regarding the family characteristics, they were for the most part nuclear families (elementary families consisting of a couple and their children) (85.6%), and the parental education level was at least a bachelor’s degree (77.8%). In addition, more than half received adequate income, at least 15,000 baht per month (80%). The exceptions were the parental age and number of siblings, where there was a statistically significant difference between groups (Table 1). Thus, analysis of covariance was utilized to determine parental readiness, parental performances later, and the number of siblings with parental age served as the covariate.
3.2. Variables of Interest
The findings of this study revealed that the parents in the experimental group showed significantly higher readiness than the parents in the control group on discharge day after two weeks of intervention (p < 0.01): the average parental readiness scores are presented in Table 2. Regarding parental readiness at pre-discharge before there was a difference; the mean score of the control group was higher than that of the experimental group at the beginning of the program with a statistical significance (p < 0.01), as shown in Table 2. The results indicated inequality in the baseline regarding parental readiness. Analysis of covariance was utilized to determine parental readiness at discharge day, and the mean score for parental readiness at pre-discharge served as a covariate. The comparison of the mean score of parental readiness between groups is displayed in Table 3, and the results revealed that the direct effect of the continuity of care program on parental readiness on discharge day significantly increased after eliminating the effect of the confounding factors and controlling for the mean of parental readiness scores at pre-discharge, for the number of siblings, and parental ages before intervention (p < 0.01).
The results revealed that the parental performances of the experimental group were significantly higher than the parental performances in the control group (p< 0.01); the average parental performance scores are show in Table 2. The mean scores for the parental performances between groups were compared, and the results from the ANCOVA showed a significant direct effect of the CCPI on parental performances at four weeks post-discharge, significantly higher after controlling for the effects of the number of siblings and parental age (p < 0.01) (Table 4).
| Demographics |
Experimental Group (n = 45) |
Control Group (n = 45) |
p-value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Mode of delivery | 0.327b | ||||
| Caesarean section | 36 | 80 | 32 | 71.1 | |
| Normal labor | 9 | 20 | 13 | 28.9 | |
| Family type | 0.764b | ||||
| Nuclear family | 39 | 86.7 | 38 | 84.4 | |
| Extended family | 6 | 13.3 | 7 | 15.6 | |
| Number of siblings | *0.002c | ||||
| First child | 38 | 84.4 | 25 | 55.6 | |
| ≥ 2 children | 7 | 15.6 | 20 | 44.4 | |
| Parental education level | 0.304b | ||||
| Lower than high school | 7 | 15.6 | 13 | 28.9 | |
| Bachelor degree | 35 | 77.8 | 30 | 72.2 | |
| Master’s degree or higher | 3 | 6.7 | 2 | 4.4 | |
| Income (Baht) | 0.871a | ||||
| ≥ 15,000 | 9 | 20.0 | 9 | 20.0 | |
| 15,001-25,000 | 25 | 55.6 | 27 | 60.0 | |
| ≤ 25,001 | 11 | 24.4 | 9 | 20.0 | |
| M | SD | M | SD | ||
| Average Gestational age (weeks) | 33.60 | 1.30 | 34.49 | 1.37 | 0.557c |
| Average birth weight (grams) | 2202.64 | 555.58 | 2101.49 | 410.64 | 0.329c |
| Body weight at before discharge(grams) | 2349.27 | 431.00 | 2406.11 | 434.80 | 0.535 c |
| Average of parental age | 36.42 | 4.91 | 34.40 | 3.71 | *0.030c |
| Parenteral Readiness | Analysis of Covariance | ||||
|---|---|---|---|---|---|
| SS | df | MS | F | p | |
| Parental readiness (Pre-discharge) | 460.887 | 1 | 460.887 | 1.155 | .286 |
| Parental ages | 129.065 | 1 | 129.065 | .323 | .571 |
| Number of siblings | 106.932 | 1 | 106.932 | .268 | .606 |
| group | 2835.279 | 1 | 2835.279 | 7.104 | .009* |
| Error | 33922.838 | 85 | 399.092 | ||
| Parental Performances | Analysis of Covariance | ||||
|---|---|---|---|---|---|
| SS | df | MS | F | p | |
| Number of siblings | 101.870 | 1 | 101.870 | 1.060 | .306 |
| Parental ages | 48.594 | 1 | 48.594 | .506 | .479 |
| Group | 4146.984 | 1 | 4146.984 | 43.163 | .000* |
| Error | 8262.574 | 86 | 96.076 | ||
| Service Utilization Rates Post Discharge | Analysis of Variance | ||||
|---|---|---|---|---|---|
| SS | df | MS | Fr | p | |
| Time | 4.104 | 2 | 2.052 | 6.322 | 0.003* |
| Error | 28.563 | 88 | .325 | ||
| Time | Experimental Group (n=45) | ||
|---|---|---|---|
| Mdiff | SE | p-value | |
| Service utilization rates post discharge | |||
| Post-discharge 1st week - 2nd week | 0.16 | 0.13 | 0.723 |
| Post-discharge 2nd week - 4th week | 0.27 | 0.10 | 0.038** |
| Post-discharge 1st week - 4th week | 0.42 | 0.12 | 0.005* |
**significance at level 0.05.
In order to test the effects of the CCPI, the analysis of RM-ANOVA showed a significant difference in the CCPI in terms of the change in the mean scores of service utilization rates post-discharge over time between groups (p < 0.01), as shown in Table 5. A post hoc analysis of SURPD revealed that the CCPI elicited a slight reduction in SURPD from the first week to the second week after discharge, which was not significant (p = 0.723) (Table 6). However, service utilization rates at the fourth week post-discharge were reduced, which were significantly different from the first week after discharge (p< 0.01) and the second week after discharge (p < 0.05). Therefore, we can summarize that the continuity of care program before release elicits a significant reduction in the service utilization rates, not only during the first week after discharge.
4. DISCUSSION
The study aimed to examine the effects of the CCPI. The results revealed that combining discharge preparation and home-based continuing care by the same healthcare team effectively improved parental readiness and parental performances post-discharge. The parents of the preterm infants in the experimental group were significantly more ready for discharge than those in the control group. The parental readiness in the experimental group increased than before receiving the program because the continuity of care program enhanced their participation in their preparation for discharge. Before hospital release, a skill-based training program is significant for the transition and for its influence on parental readiness [40, 41]. Previous studies have confirmed these results. According to Gupta, Pursley, and Smith [42], discharge readiness increased following quality improvement in the discharge-preparation process. Adequate discharge preparation for the parents was accomplished by maintaining information continuity and by promoting hands-on experience, all of which enhanced their parental readiness [43, 44]. Parents have also acknowledged the need for appropriate content for use in rearing their preterm infants. The CCPI also influenced the parents in terms of performing their tasks regularly, especially in the area of preterm infant care, such as feeding skills, temperature measurement, observing the preterm infant’s behavior cues, and first-aid with continuing care post-discharge in case of emergency. The parents were interested in practicing their roles, using the preterm infant handbook in the discharge tool kit, and raised some questions to discuss with the team in order to clarify any misunderstandings they had. Once the parents felt ready to perform their duties confidently, they were more motivated to overcome obstacles and fulfill their responsibilities in meeting their infants' needs. During the transition period of a family with a preterm infant, the goal is to establish their parenthood after returning home, and to enjoy a period of progressive growth and development [45].
The results demonstrated that discharge preparation is vital for preterm infants' families, and that the program may help parents believe that they can handle the preterm infant’s needs [45]. Furthermore, home-based care and continuing care post-discharge appeared to serve as a support mechanism that influences the developmental tasks of families of preterm infants [44, 46], as well as increases parental performances for preterm infant rearing post-discharge. The findings supported that the continuity of care guides intervention for improving the parental performances at four weeks post-discharge. Previous studies support this finding [44], the parents involved in the CCPI were educated and followed up from weeks 1-4 with the same healthcare team. Initially, interpersonal continuity was carried out, and valid information continuity was promoted with the handbook and tool kits, such as a bulb and a thermometer used as teaching materials. According to the literature review, other techniques can include education sessions and continuing care, such as follow-ups, home visits, and telephone calls in order to encourage and develop the parental role and to increase their ability to care for the infant at home.
Service utilization rates post-discharge were monitored in order to confirm the program’s effect. The CCPI provided information continuity with a package of discharge planning during transition to the home, and by coordinating with the same healthcare team across settings in order to retain continuity of care post-discharge. All of the families in the CCPI received a home visit during the first week. The findings revealed that the number of SURPDs showed a significant decrease after implementing the CCPI at the fourth-week post-discharge, but the SURPD were not significant during the first week. It is interesting to note that the parents in the experiment group indicated to providers, during the telephone follow-up in the second week, that they had to fill a birth certificate in their hometown (different from the study site). The parents had to register a birth report, choose the healthcare scheme properly, and wait until the electronic health system approved it. This is a limitation of management continuity because we have several platforms of recording the health-related information. Most of the health information is not linked between the local administration and healthcare services in Thailand [47]. This process is relevant to the study of Silva, Zilly, Nononse, Fonseca, and Mello [48], who stated that poor management continuity from an inactive department in primary care interrupted the continuity of care for vulnerable people. The healthcare provision system requires more strategies to optimize the use of the available tools and to encourage the healthcare teams to maintain a good standard of care by promoting the continuity of care concept. Finally, an essential strategy for maintaining the continuity of care in the family for preterm infants was implemented. As a result, essential information continuity for the tailored care of preterm infants was provided, promoting interpersonal continuity among providers, peers, and parents .
4.1. Limitations
This study has a number of limitations, including the use of several kinds of platforms for recording the client’s health information, and the participants used a variety of a healthcare plans. Therefore, all of these barriers disrupted the consistency of information continuity and interrupted the process of management continuity between the families and the healthcare providers. Future studies need to consider a variety of healthcare schemes and new Internet-based/digital technology at each level of healthcare in order to collaborate with teams across settings.
CONCLUSION
The findings of this study confirmed the effectiveness of the CCPI in reducing service utilization rates at four weeks post-discharge and improving parental performances after going home. Additionally, the parental readiness before hospital discharge was higher than parents who received routine nursing care. This result indicated that individualized discharge teaching and utilizing discharge tool kits could achieve a state of technical readiness and emotional readiness for the parents. The CCPI was implemented at two weeks before discharge and following until four weeks post-discharge, which is the critical transition period for families with preterm infants. The CCPI helped the parents adapt to their phase of being a parent of a preterm infant.
LIST OF ABBREVIATIONS
| SURPD | = Service Utilization Rates Post Disharge |
| OPD | = Out Patient Department |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Human Research Ethics Committee of Thammasat University (Science), (HREC-TUSC) #COA No. 091/2563.
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. All the humans procedure were conducted in accordance with the principle of Declaration of Helsinki.
CONSENT FOR PUBLICATION
During recruitment, the researcher verbally explained the objective and significance of this study. Then, if they agreed to participate in this study, the participants signed a consent form.
STANDARDS OF REPORTING
CONSORT guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
This study was supported by a research grant from the National Research Council of Thailand (Grant no. 1244412/ 2020).
CONFLICT OF INTEREST
The authors declare no conflicts of interest or otherwise.
ACKNOWLEDGEMENTS
The author would like to sincerely acknowledge the National Research Council of Thailand (Grant no. 1244412/ 2020) for the financial support to this research. The author would also like to express her deepest gratitude to all of the participants and thank all of the nurses in Pathum Thani Province, Thailand, for their kind co-operation. Finally, the author extends special thanks to Professor Emerita Dr. Marianne Weiss, who gave permission to use the readiness for hospital discharge scale and to translate the Ped-RHDS into the Thai version.


