All published articles of this journal are available on ScienceDirect.
Report of Aortic Dissection without Risk Factor And Typical Symptoms in a 25-Year Old Man
Abstract
Background:
Acute aortic dissection is a rare but serious and life-threatening disease. The main symptom is chest pain, but in some patients, atypical symptoms are also observed.
Case presentation:
In this report, we reported a patient diagnosed with aortic dissection with atypical symptoms. The patient has been referred with nausea and vomiting. After a thorough examination, the diagnosis of acute aortic dissection was established.
Conclusion:
Aortic dissection may have no typical symptoms and deep examination in all suspected patients, is necessary.
1. INTRODUCTION
Acute aortic syndromes include 1-aortic dissection, 2-penetrating atherosclerotic aorta ulcer, and 3-aortic intramural hematoma [1]. Aortic dissection comprises 80-90% of acute aortic syndromes [2]. The annual incidence of aortic dissection is 2.6-3.5 per 100,000 population [3]. Aortic dissection is a life-threatening condition. The primary event is the tearing of the aortic intima [4]. The major classes of aortic dissection include De Bakey and Stand Ford. Type A Stand Ford dissection involves the ascending aorta (with or without extension to the descending aorta) [5].
Predisposing and risk factors of aortic dissection are hypertension, congenital syndromes (bicuspid aortic valve, coarctation of aorta, and tetralogy of fallot), atherosclerosis, hereditary thoracic aorta disease, trauma, cocaine, inflammatory and infectious diseases, pregnancy, and weightlifting [6].
Aortic dissection can present with a variety of symptoms. The main symptom of the syndrome is severe sharp and ripping or tearing chest pain with a sudden onset. Approximately 80% of patients have experienced chest pain [7]. In some patients, other symptoms and complications may be dominant without pain. Other clinical features at presentation include chronic heart failure, arrhythmia, syncope, stroke, myocardial infarction, paraplegia, cardiac arrest, and sudden death [8].
Aortic dissection is a rare but dangerous disease, and it can be catastrophic if it is not quickly diagnosed and treated [9]. The mortality rate of aortic dissection is more than 50% if it is late diagnosed or inadequately treated [10]. Atypical manifestations of aortic dissection make its diagnosis difficult and may even delay treatment initiation [7]. In this report, a patient diagnosed with aortic dissection with atypical symptoms is described.
2. REPORT
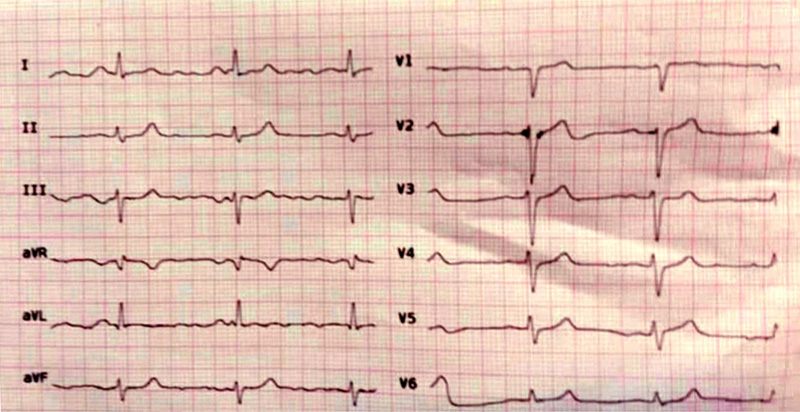
A 25-years old Iranian man has been referred to the emergency department with severe nausea and vomiting. Ultrasounds of the liver, gallbladder, bile ducts and pancreas were normal. The patient had no cardiac symptoms and only presented with nausea and vomiting. Sinus bradycardia was observed in ECG (Fig. 1). Laboratory parameters were within normal range (Table 1).
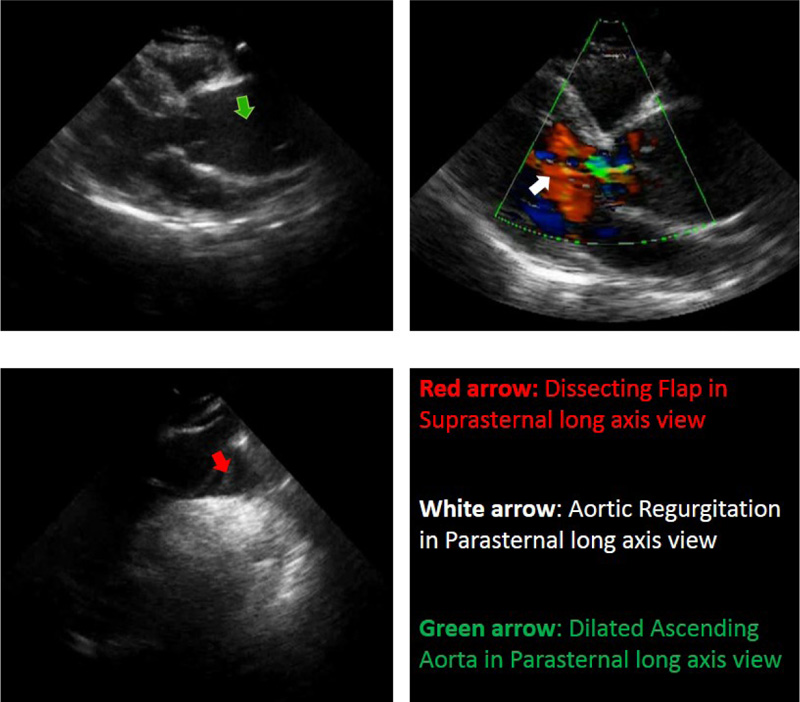
In the emergency department and upon arrival, cardiac counselling was requested due to bradycardia. Based on the cardiac counselling which was provided at once, trans-thoracic echocardiography (TTE) was performed immediately due to diastolic murmur hearing on aortic focus.
In TTE findings, evidence was in favour of type A acute thoracic aortic dissection (Fig. 2). Dilated aortic root and ascending aorta were noticed. The dissecting flap was extended from the large curvature of ascending aorta to the right brachiocephalic artery. Malcoapted AV and diastolic flow reversal in the descending aorta suggest moderate AI. The patient was immediately transferred to the CCU, and cardiac monitoring and emergency therapy were initiated. The patient was finally referred to the cardiac surgery department.
| Clinical examination | Heart rate: 58 |
| blood pressure: 110/60 | |
| Respiratory rate: 15 | |
| Laboratory examination | Hb: 15.7 |
| WBC: 10.5 | |
| PLT: 235000 | |
| Cr: 1 | |
| Na: 142 | |
| K: 3.7 | |
| Total Bilirubin: 0.9 | |
| AST: 9 | |
| ALT: 18 | |
| ALKP: 258 | |
| Troponin T: negative |
3. DISCUSSION
This was a report of type A Stand Ford aortic dissection with atypical manifestations in a 25-year-old Iranian patient. The patient had no risk factors or a past history of any special cardiac disease. Atypical manifestations of aortic dissection make the diagnosis of the condition difficult and delay treatment initiation. These atypical manifestations include pulse deficit, syncope, shock, tamponade, hypotension, heart failure, focal neurological deficits, and pericardial effusion [11, 12]. In accordance, such atypical symptoms were misleading in our patient as well. In a similar study by Solhjoo et al. (2019), they described a patient with aortic dissection presenting with nausea and gastrointestinal symptoms. In addition, this patient also had neurological symptoms that led to the final diagnosis [12]. The difference between our patient and the one introduced in the study of Solhjoo et al. is that our patient had only nausea and vomiting with no other symptoms. In fact, less than 5% of these patients present with gastrointestinal symptoms [13]. In our patient, however, there were only nausea and vomiting without any neurological or another symptom. We also identified no risk factors for cardiac diseases. While our patient was 25-years old, but the one reported by Solhjoo et al. aged 48 years old and had hypertension. This is noteworthy as the incidence of this condition in individuals less than 40 years of age is rare. As well, hypertension is one of the main risk factor for aortic dissection. Nevertheless, our patient did not have hypertension.
The diagnosis of aortic dissection may be missed in up to 38% of patients, especially those with atypical manifestations, in whom the missing rate is higher [14]. After diagnosis, if the case is not immediately treated, the mortality rate increases with the rate of about 1-3% per hour and reaches 20-30% within the first 24 hours [15]. In patients with atypical symptoms, the probability of a missed diagnosis is high. Due to the high mortality rate of aortic dissection, misdiagnosis can be very dangerous. The diagnostic key in our patient was diastolic murmur, which is a sign of acute aortic regurgitation. This was successfully detected by our cardiologist. Otherwise, the patient’s clinical history and symptoms did not provide any diagnostic clue for us. So, it seems that a thorough cardiac examination is necessary to accurately and timely diagnose this condition.
Aortic dissection is associated with different types of arrhythmias such as premature ventricular contraction, supraventricular tachycardia, atrioventricular block, and atrial fibrillation [16-19]. In our patient, no evidence of arrhythmia or ischemia were noticed on ECG, and only sinus bradycardia was seen in this test.
According to the IRAD study, only 7% of patients with aortic dissection are under 40 years old. These patients usually have bicuspid aortic valve, marfan syndrome, and aortic valve replacement or are in the peripartum period [20]. Our patient (a 25-year-old man); however, did not mention any of the noted problems and disorders. Indeed, he had no obvious symptoms and risk factors favoring aortic dissection. Therefore, the patient’s age and clinical history were misleading, increasing the possibility of misdiagnosis. Nevertheless, a thorough examination, paying attention to all signs and symptoms, and looking into all possible diagnoses led to an immediate and correct diagnosis.
CONCLUSION
The educational point of this case report is to be careful to examine all the body organs and have a wide clinical view while assessing these patients.
Learning Points
- The aortic dissection was diagnosed with atypical symptoms.
- The main problem in a patient with aortic dissection was nausea and vomiting.
- Aortic dissection may have no typical symptoms and needs deep examination.
- Malcoapted AV and diastolic flow reversal in the descending aorta showed moderate AI.
AUTHORS' CONTRIBUTIONS
AB, MK, EMN, and SSA participated in the diagnosing, laboratory testing, and drafting the manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patient.
STANDARDS OF REPORTING
CARE checklist was followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in this article.
FUNDING
None.
ACKNOWLEDGEMENTS
Declared none.


