All published articles of this journal are available on ScienceDirect.
The Content of Breast Milk and the Challenges Experienced by Breastfeeding Mothers during the COVID-19 pandemic: A Systematic Review
Abstract
Introduction:
Every postpartum mother is recommended to breastfeed her baby because breast milk is the main need of newborns. The COVID-19 pandemic has had an impact on life in various aspects, including on the breastfeeding mothers, especially if they suffer from COVID-19 infection.
Aim:
The study aims to provide comprehensive evidence regarding potential virus transmission and antibody transfer through breastmilk and the experiences of mothers related to breastfeeding during the COVID-19 pandemic.
Methods:
A systematic review was conducted following the PRISMA guidelines. The search strategy involved the use of keywords related to COVID-19 and breastfeeding in PubMed and Science Direct databases. Articles were selected according to inclusion and exclusion criteria.
Results:
Breastfeeding has been recommended to be continued during the pandemic due to the benefits associated with it and the absence of sufficient evidence for transmission of COVID-19 infection through breast milk. During the lockdown period, there was a change in breastfeeding patterns, although most mothers believed that breastfeeding should be continued. Anxiety and lack of support affected breastfeeding practices. Breastfeeding mothers reported a dilemmatic situation. They felt protected because of the lockdown policy but also struggled to get support from their social environment. The impact varied in terms of stopping breastfeeding practice altogether, breastfeeding irregularly, and even giving formula milk.
Conclusion:
Adherence to health protocols can reduce the risk of transmission of COVID-19 infection through breastfeeding from mother to baby. Support from the family and the environment is needed to ensure the continuity of breastfeeding practice.
1. INTRODUCTION
The World Health Organization (WHO) declared COVID-19 a global health pandemic in early March 2020. The number of deaths caused by the transmission of the COVID-19 virus continued to increase every day [1]. Various efforts and strategies have been designed, ranging from prevention, such as vaccination, lockdown, health promotion, use of masks, and physical distancing, to the application of curative and alternative medicine [2]. However, the situation was exacerbated by mutation variants that caused the emergence of second wave in several countries. COVID-19 had a wide impact on the health and non-health sectors. One of the health sectors affected was maternal and child health.
There were around 140 million births during the pandemic, and many mothers had difficulty breastfeeding their babies with the increase in positive cases of COVID-19. The fear observed in breastfeeding mothers was that their breast milk might contain the COVID-19 virus pathogen [3]. Pregnant women and newborns were also included in the high-risk group and were vulnerable because of their low immune systems and the capacity to easily get infected [4]. World Health Organization (WHO) provided advice related to breastfeeding during the COVID-19 pandemic. WHO recommended and encouraged women with COVID-19 to continue breastfeeding under strict health protocols. Breast milk is recommended to be given to newborns during the first six months of life and continued until the age of 24 months, accompanied by complementary foods. Breastfeeding can be a source of nutrients for growth during the first few months of life. In addition, passive immune transfer between mother and baby can be done through breastfeeding [5].
The study aimed to provide comprehensive evidence regarding potential virus transmission and antibody transfer through breastmilk and the experiences of mothers related to breastfeeding during the COVID-19 pandemic. The results of this study can support mothers to continue breastfeeding through the available evidence and resolve problems related to breastfeeding during the pandemic.
2. METHODS
2.1. Study Design and Search Strategy
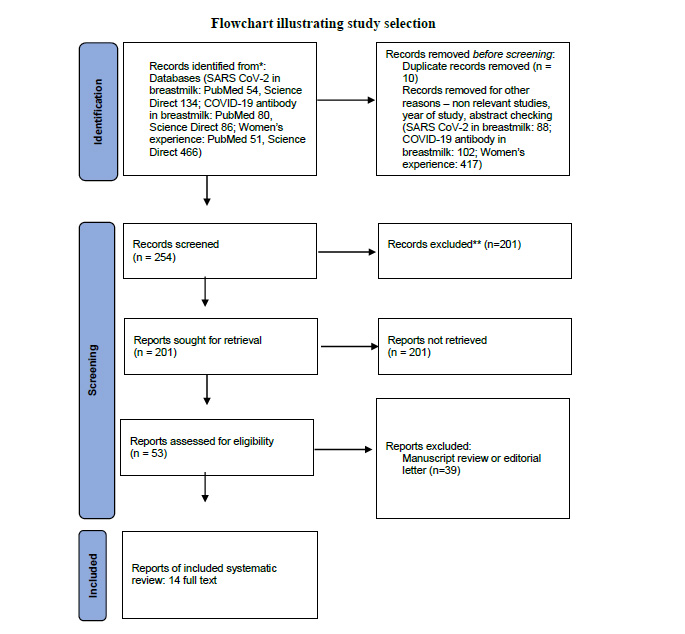
A systematic review was conducted following the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [6] (Fig. 1). The search strategy was carried out through the PubMed and ScienceDirect databases using the Medical Subject Heading (MeSH) keywords and relevant keywords in a different order: “breastfeeding”, “women”, “COVID-19”, and synonyms of these keywords. The list of references found in the selected articles was reviewed to find the articles that were not included in the electronic literature search. Boolean operators were used in the search strategy by using conjunctions, namely AND, OR and NOT.
2.2. Study Selection and Outcome Measures
Articles were selected through inclusion and exclusion criteria. The selected articles were researches conducted during the COVID-19 pandemic in 2020-2021, written in English, and provided full text. The author has evaluated the chances of viral transmission and antibody transfer in the first part of the discussion and then described the experience of breastfeeding during the pandemic in the second part. The exclusion criteria for this study included animal studies, letters to editors, study reviews, and abstracts without full text.
2.3. Data Extraction
All authors performed title and/or abstract screening independently of the included articles using standard Microsoft Excel forms. A third external collaborator was consulted to address disagreements in consensus. The formal assessment of the article quality was carried out with the criteria of having clear objectives, explaining the type of research carried out, writing down the appropriate research methodology according to the objectives, and drawing the right results.
2.4. Data Abstraction and Synthesis
The analysis was based on the results and conclusions of each study. Parameters examined in (Tables 1 and 2) include author, year, purpose, research method, population/sample, and findings. (Table 1) summarizes the presence of virus pathogens and antibodies in breast milk. (Table 2) summarizes the factors influencing the breastfeeding experience during the pandemic.
| Author, Year | Purpose | Research Method | Population/ Sample Setting | Finding |
|---|---|---|---|---|
| Virus transmission | ||||
| Liu et al., 2021 [7] | This research studies the potential spread of SARS-CoV-2 to 3-month-old infants through exclusive breastfeeding | Case report | A 33 years-old woman | Mothers can exclusively breastfeed their babies since they are confirmed to be infected with SARS-CoV-2. A breast milk sample was taken, and the nucleic acid test result for COVID-19 was negative. The baby is asymptomatic and remains negative for the virus. |
| Kunjumon et al., 2021 [8] | The study determines if SARS-CoV-2 was present in the breast milk of lactating mothers who had a positive SARS-CoV-2 nasopharyngeal swab test before delivery and the clinical outcomes for their newborns. | Prospective cohort study | A total of 19 mothers and their babies who were breastfed | Breast milk samples from 18 mothers were tested negative for SARS CoV-2, but 1 sample was positive for SARS-CoV-2 RNA. Infants, who ingested breast milk from a mother who was tested positive for COVID-19, had a negative nasopharyngeal test for SARS-CoV-2 and had a benign clinical course. |
| Thanigainathan et al., 2021 [9] | The study was done to check the possible transmission of the virus through breastfeeding in the Indian context. | Descriptive study | Breast milk samples were collected from 30 COVID-positive mothers | All breast milk samples were negative for SARS-CoV-2 except for one, but they were negative the next day when re-checked. No clinical manifestations or infectious status of COVID-19 were recorded among the neonates. |
| Talat Kilic et al., 2021 [10] | The study investigated the presence of SARS-CoV-2 RNA in human milk samples of 15 mothers with coronavirus disease 19 (COVID-19) and their infants' throat swab samples. | Prospective observational study | Breast milk samples were collected from 15 mothers with COVID-19 | SARS-CoV-2 RNA was detected in milk samples from 4 of 15 mothers with COVID-19. A throat swab sample from the baby was found to be positive for SARS-CoV-2 RNA. The results of the SARS-CoV-2 RNA test on throat swab samples were found to be negative in 6 of the 12 infants who were breastfed. Six infants with mild COVID-19 symptoms tested positive for SARS-CoV-2 RNA. |
| Shlomai et al., 2021 [11] | The study assessed infection rates predischarge and post-discharge in breast milk-fed newborns with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-positive mothers who were separated postdelivery from their mothers and discharged from the hospital. Also, the study aimed to evaluate breastfeeding rates predischarge and post-discharge. | Prospective cohort study | A total of 55 newborns of SARS-CoV-2-positive mothers were born in Israel during the three months under study. | No viral infection was identified in neonates born and separated from their mothers who were positive for SARS-CoV-2 at birth and subsequently fed unpasteurized breast milk. All babies who were breastfed at home remained SARS-CoV-2 negative. |
| García et al., 2021 [12] | The research addresses the prevalence of SARS-CoV-2 and the evolutionary profile of immune compounds in breastmilk of positive mothers according to time and disease state. | Prospective cohort study | Forty-five women with term pregnancies with confirmed non-severe SARS-CoV-2 infection (case group) and 96 SARS-CoV-2 negative women in identical conditions (control group) were approached using consecutive samples. | There was no viral RNA and different immunological profiles in breast milk according to the SARS-CoV-2 status of the mother. |
| Antibody in breastmilk | ||||
| Juncker et al., 2021 [13] | To determine (1) the prevalence and (2) the dynamics of immunoglobulin A (IgA) antibodies against SARS-CoV-2 in human milk amongst lactating mothers in the Netherlands. | Prospective cohort study | Lactating mothers (N = 2312) were included between 12 October 2020 and 24 February 2021. | The prevalence of IgA antibodies against SARS-CoV-2 in human milk was 23.1% in our cohort. This high prevalence of antibodies in human milk might lead to passive immunity in many breastfed infants and may serve as protection against COVID-19. |
| Pace et al., 2021 [14] | Whether mother to-infant SARS-CoV-2 transmission can occur during breastfeeding and, if so, whether the benefits of breastfeeding outweigh this risk during maternal COVID-19 illness remain essential questions. | Prospective cohort study | Eighteen women following the COVID-19 diagnosis with a recent diagnosis of laboratory-confirmed COVID-19 participated in the study. | 76% of the milk samples collected from women with COVID-19 contained SARS-CoV-2-specific IgA, and 80% had SARS-CoV-2-specific IgG. In addition, 62% of the milk samples could neutralize SARS-CoV-2 infectivity in vitro, whereas milk samples collected before the COVID-19 pandemic could not do so. |
| Favara et al., 2020 [15] | Perform detection of breastmilk antibodies targeting SARS-CoV-2 nucleocapsid, spike and receptor-binding-domain antigens | Case report | A 40-year-old breastfeeding mother | A 40-year-old female was found to have strongly neutralizing SARS-CoV-2 breastmilk IgA and IgG antibodies reactive against multiple SARS-CoV-2 antigens at 2.5 months after documented infection with SARS-CoV-2. At 6.5 months following the infection, she remained positive for breastmilk and serum SARS-CoV-2 neutralizing antibodies. |
| Valvacre et al., 2021 [16] | The purpose of the study is to determine whether SARS-CoV-2-specific immunoglobulins are found in human milk after the COVID-19 vaccination and to characterize the types of immunoglobulins present. | Prospective observational study | Twenty-two lactating health care workers who received the SARS-CoV-2 mRNA vaccine (Pfizer/BioNTech or Moderna) made up the sample group. | There is a significant SARS-CoV-2-specific IgA and IgG secretion in human milk and plasma after SARS-CoV-2 vaccination. |
| Author, Year | Research Method | Population Setting | Finding |
|---|---|---|---|
| Costantini C et al., 2021 [17] | Cross-sectional study | Mothers of children aged 0–36 months (N = 4018) took part in an online survey. | Participants strongly agreed with the importance of breastfeeding, even if a mother shows symptoms of COVID-19. Differences of opinion regarding breastfeeding practices (e.g., use of donor breast milk and relactation), were found between participants regarding the duration of breastfeeding and the number of children. Participants with more than one child showed higher negative emotional states, namely anxiety symptoms. Except for internet use, participants indicated a decrease in all sources of advice and support for breastfeeding during the COVID-19 lockdown. |
| Brown et al., 2021 [18] | Cross-sectional study | 1219 breastfeeding mothers in the United Kingdom with a baby 0–12 months old | The results highlight two very different experiences: 41.8% of mothers felt that breastfeeding was protected because of the lockdown, but 27.0% of mothers struggled for support and had many barriers stemming from the lockdown, with some stopping breastfeeding before they were ready. Mothers with lower education, more challenging living circumstances, and black and minority ethnic backgrounds were more likely to find the impact of lockdown challenging and cessation of breastfeeding. |
| Chanodom et al., 2021 [19] | Cross-sectional study | Data were collected from 903 mothers with infants aged 0–12 months | Mothers changed breastfeeding practices during the lockdown period, including having changed from exclusive breastfeeding to combined breastfeeding with formula, and having reduced the frequency compared to before the pandemic. Factors associated with changing breastfeeding practices were contact with health services, infant feeding support from health workers and lack of family support and assistance in infant feeding after lockdown. |
| Latorre et al., 2021 [20] | Prospective cohort study | 204 mother-baby dyads during lockdown (9 March to 8 May 2020) compared to previously studied 306 mother-baby dyads admitted in 2018. | Lockdown and confinement at home led to a decrease in exclusive breastfeeding in the population studied. When it came to the transition from exclusive to non-exclusive breastfeeding, the differences between the study groups were concentrated during the hospital stay and from 30 to 90 days of newborn life, confirming that hospital stay is critical in continuing exclusive breastfeeding at least for baby in the first 30 days, but no longer relevant at 90 days of life. |
3. RESULTS
The systematic review was carried out in several stages. 54 articles on the PubMed database and 134 articles on the ScienceDirect database discuss the presence of the SARS-CoV-2 virus in breast milk. 80 articles on the PubMed database and 86 articles on the ScienceDirect database discuss the presence of antibodies against COVID-19 in breast milk. 51 articles on the PubMed database and 466 articles on the ScienceDirect database discuss the experience of breastfeeding mothers. A total of 14 articles were included in the inclusion criteria covering three main topics from the 254 articles that were screened. The articles were analyzed and examined qualitatively for quality assessment. The types of articles included 2 case reports, 4 cross-sectional studies and 8 prospective cohort studies. The articles have been thoroughly reviewed, and their summary has been presented in (Tables 1 and 2).
Based on various studies that examined the presence of SARS-COV-2 in breastmilk, it was found that most breastmilk samples did not contain the virus. Samples in small quantities were found to contain the virus, but did not permanently harm the baby. Infants, who had ingested breast milk from mothers positive for COVID-19, revealed a negative nasopharyngeal test for SARS-CoV-2 and had a benign clinical course. There was no significant evidence obtained for mother-infant transmission through breast milk, but transmission during breastfeeding needs to be understood, especially with respect to the skin of the breast. Potential antibodies against COVID-19 infection have been found to be present in breastmilk, namely IgA and IgG.
There was a change in breastfeeding patterns during the lockdown observed in breastfeeding mothers. Although most mothers agreed to the importance of breastfeeding, there were differences in opinion regarding breastfeeding practices, such as the use of donor breast milk and relactation, the duration of breastfeeding, and the challenges with respect to a number of children. Anxiety affected mothers in giving breastmilk to their babies. The support required during breastfeeding was also reduced, including the availavility of health workers and families. Mothers had different experiences, such as feeling protected by a lockdown but struggling to find support. The visible impact was that they decided to stop breastfeeding, breastfed irregularly, or used formula milk. Mothers who lived in hospitals had a better chance of exclusively breastfeeding for the first 30 days. After 90 days, they were not affected by the hospital support anymore but may have been influenced in other aspects, such as family support.
4. DISCUSSION
4.1. Viral Transmission and Antibody Transmission During Breastfeeding
Based on various studies that examined the content of SARS COV-2 in breastmilk, it was found that most of the breastmilk samples did not contain the virus, and there was potential for antibodies against COVID-19 in the mother's breastmilk. Newborns of mothers infected by SARS-CoV-2 are more likely to receive intensive care that limits direct contact for breastfeeding initiation [21, 22]. So far, breastfeeding is the best feeding for infants and has countless benefits for both mother and infant, including a protective effect on morbidity and mortality [23]. Breast milk protects the infant against several infectious diseases through the transfer of antibodies and stimulates the development of the immune system. In newborns with immature immunity, breast milk is required to protect infants through bioactive factors and secretory IgA antibodies [24]. Breast milk is also rich in immunoglobulin, lactoferrin, and lysozyme, stimulating the innate and adaptive immune response to protect against microorganisms [25]. Previous studies show that preterm birth incidence (12.9%) is higher in women with SARS-CoV-2 infection [26]. Premature infants are much more susceptible to infection, so they need more protection and stimulants for the development of the immune system [27].
Skin-to-skin contact in breastfeeding between mother and infant immediately after the birth provides exposure to the mother's normal flora and stimulates the development of the baby's microbiome. Skin-to-skin contact also increases blood glucose, stabilizes the respiratory system, prevents neurodevelopmental disorders, and also reduces stress for both mother and infant [28, 29]. It has been reported that scaling up breastfeeding to a near-universal level could stop around 823,000 child deaths annually [30]. Breastfeeding also reduces morbidity and mortality in diarrhea by up to 64% and the severity of respiratory syncytial virus (RSV) up to 72% [25]. Therefore, continuing to breastfeed during the COVID-19 pandemic must be considered, especially for women with SARS-CoV-2 infection [31].
4.2. Experiences of Breastfeeding Mothers During the Pandemic Situation
During the pandemic, there was a change observed in breastfeeding patterns even though most mothers supported and believed that breastfeeding should be continued during the lockdown. Anxiety and lack of support affect mothers in giving breastmilk to their babies. Mothers reported different experiences, such as feeling protected by the lockdown. Still, mothers had to struggle to get support and experienced many related obstacles, so they decided to stop breastfeeding or breastfeed irregularly. Some even changed it to a combination with formula milk. Apart from mothers, it turned out that most of the staff who participated in providing lactation support to women affected by COVID-19 reported increased stress. Ensuring written or verbal guidance could reduce staff's stressful experience. Efforts to optimize lactation support during COVID-19 involved reduced distraction, physical separation, and logistical challenges [32].
The UNICEF's latest information still recommends exclusive breastfeeding while using necessary precautions for infection prevention and control, even in mothers with suspected or confirmed COVID-19 [33]. CDC indicates that breastfeeding is up to the mother, family members, and health professionals [34]. This recommendation is based on the health benefits of breastfeeding for both the mother and the child. The risk of COVID-19 infection in an infant can be prevented when the mother obeys universal protocols. For a mother with asymptomatic or mildly symptomatic COVID-19, it is highly recommended to wash hands for 20 seconds using running water and soap or hand sanitizer before breastfeeding, touching any pump or bottle parts, and before expressing breast milk. It is also recommended to wear a mask while breastfeeding, expressing breast milk, and whenever within 6 feet distance from the baby [5]. The mother should maintain the breast hygiene with soap and water before breastfeeding the baby. These precautions should be continued until afebrile, the improvement of symptoms, and having two negative tests for SARS-CoV-2 at least 24 hours apart. If there is no source for testing, the mother should continue these precautions until she symptomatically improves and becomes afebrile for at least three days since the onset of symptoms. For moderate to severely symptomatic mothers with COVID-19, the mother must wear a mask, wash her hands, and wash her breast with soap and water. If the mother expresses milk (with a hospital-grade electric breast pump if available), then a healthy family member/nurse shall feed the expressed milk to the baby in a separate room. Breast pump tubing and container should be cleaned after each use. The outside surface of containers must be disinfected after milk expression and before storage [35].
Breastfeeding support is also provided through a private room, which ensures the mother's privacy. Mothers must feel comfortable during breastfeeding, such as the room must have a comfortable chair, electrical outlets, appropriate lighting, and must be kept at a comfortable temperature. There should be a flat surface, such as a table, to place the breast pump and its accessories. Room sanitation must be kept clean. There should be access to hand washing as well as pump supplies. In addition, there must be safe access to breast milk storage and breast pump storage [36].
Various problems have been encountered in terms of breastfeeding during the pandemic, such as the premature termination of the baby. Mothers in this setting have expressed high stress and anxiety levels during their premature infant's NICU admission [37]. It is because postpartum mothers often have unstable emotions, so they have difficulty adapting to changes during the perinatal period that cannot be resolved fundamentally [38]. Support from family and the environment is vital in ensuring that mothers breastfeed well, especially during a pandemic. Mothers with a positive COVID-19 status need to pay attention to the existing symptoms in breastfeeding. Mothers with severe symptoms of COVID-19 can be advised to get a breast milk donor, while mothers with moderate symptoms, if possible, can give expressed breast milk. Mothers who receive proper support will continue breastfeeding well, even during a pandemic.
CONCLUSION
Considering the benefits of breastfeeding and no adequate evidence for transmission of COVID-19 via breast milk, there is no indication to stop breastfeeding. Nonetheless, the experience of mothers reported during the pandemic demonstrate a change in breastfeeding patterns even though most mothers supported and believed that breastfeeding should be continued during the lockdown. Anxiety and lack of support affected mothers in giving breastmilk to their babies. Mothers had reported different experiences, such as feeling protected by the lockdown. However, mothers had to struggle to get support and still encountered many related obstacles, so they decided to stop breastfeeding or breastfed irregularly. Some even shifted to a combination with formula milk. However, adherence to universal protocols can reduce the risk of mother-to-child transmission of COVID-19.
LIST OF ABBREVIATIONS
| MeSH | = Medical Subject Heading |
| PRISMA | = Preferred Reporting Items for Systematic Reviews and Meta-analyses |
| PRISMA | = Preferred Reporting Items for Systematic Reviews and Meta-analyses |
| RSV | = Respiratory Syncytial Virus |
| SARS-CoV2 | = Severe Acute Respiratory Syndrome Coronavirus 2 |
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS FOR REPORTING
PRISMA guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.


